Abstract
Objective
To study the relationship between neighborhood demographic characteristics (disadvantage, racial concentration) and the birthweight of infants born to adolescent mothers, potentially as mediated by smoking, prenatal care use, or perceptions of neighborhood safety.
Methods
Data from Waves I and IV of the National Longitudinal Survey of Adolescent Health were analyzed. Birthweight (continuous) and low birthweight (<2.5 kg) of singleton infants born to non-Hispanic Black and non-Hispanic White adolescent mothers (<20 years) after Wave I were examined as outcomes. Neighborhood demographic characteristics included Census Block Group socioeconomic disadvantage and Black racial concentration. Possible mediators (smoking during pregnancy, early initiation of prenatal care, and perceptions of safety) were also examined. Controls for adolescent baseline age, age at pregnancy, body mass index (BMI) and parental education were included. Analyses were run stratified on race.
Results
Baseline continuous birthweight, BMI and neighborhood demographics varied significantly between non-Hispanic Black and White adolescent mothers, with Black adolescent mothers evidencing lower birthweight and higher BMI, neighborhood disadvantage and Black racial concentration. In multivariable analyses among Black adolescent mothers, Black racial concentration was positively associated with birthweight, and negatively associated with low birthweight; no mediators were supported. Neighborhood disadvantage and Black racial concentration were unassociated with birthweight outcomes among White adolescent mothers.
Conclusions
Infants born to Black adolescent mothers evidenced higher birthweight with increasing Black neighborhood concentration. Further exploration of mechanisms by which Black racial concentration may positively impact birthweight is warranted.
Keywords: adolescent, birthweight, neighborhood
INTRODUCTION
In 2010, there were 372,252 live births to mothers age 10–19 in the U.S. (1). Giving birth before age 20 is associated with increased risk for a number of pregnancy complications, including infant mortality, stillbirth, congenital anomalies, preterm birth, and low birthweight (2–7). Black adolescents and very young adolescents (<15 years old) appear to be at even greater increased risk (8–11). Adverse birth outcomes among adolescents appear to be the result of both the high risk psychosocial context in which most adolescent pregnancies occur, as well as biological immaturity and other risk factors (2, 12, 13).
Although some studies have examined individual and interpersonal risk factors for adverse birth outcomes among adolescents, little is known about contextual contributors to birth outcomes in this group (10, 14–17). Neighborhood demographic characteristics (especially socioeconomic disadvantage and racial concentration) have been linked with adolescent behaviors including early sexual initiation, substance use, and delinquency (18–20). Neighborhood demographic characteristics could influence birth outcomes through such behavioral pathways, or by shaping access to health services, exposing adolescents to environmental stressors (i.e., crime), or affecting social sanctions against adolescent pregnancy (21–23).
Studies among regional and local samples combining adolescent and adult mothers have linked neighborhood disadvantage and Black racial concentration to increased risk of preterm birth and low birthweight, although findings have not been consistent across geographic areas, and sometimes varied by race of the mother (24–30). Recent research with a national sample of mothers suggests biobehavioral risk factors for adverse birth outcomes differ between adult and adolescent mothers (17). Due to adolescents’ relatively lesser mobility compared to adults, neighborhoods may be even more influential in adolescents’ versus adult women’s birth outcomes (31). The purpose of this study was twofold: (1) to examine how neighborhood disadvantage and racial concentration are related to the birthweight of infants born to adolescent mothers; and (2) if associations are found, to test potential mediators of this relationship, namely smoking during pregnancy, prenatal care use, and perceptions of neighborhood safety. Results can be used to identify pregnant adolescents who may be at increased risk of adverse birth outcomes.
METHODS
Data
Data from the National Longitudinal Study of Adolescent Health (Add Health) dataset were utilized (32). Add Health is a prospective cohort study of a nationally-representative sample of youth enrolled in grades 7–12 in the 1994–95 school year (Wave I) (33). Follow-up interviews were conducted in 1996 (Wave II), 2001 (Wave III), and 2007–08 (Wave IV). At Wave I, a multistage probability clustered sampling design was used. The first stage was a stratified, random sample of all public and private high schools in the U.S. A feeder school (i.e., a middle or junior high school whose graduates attend the selected high school) was also recruited from each participating community. In-school surveys were attempted with all students attending participating schools; a total of 90,118 were completed. In the second Wave I sampling stage, a sample of adolescents was drawn for in-depth in-home interviews, consisting of a random core sample plus selected special oversamples; a total of 20,745 interviews were conducted at this stage. At Wave II, most students (except Wave I seniors) were eligible for re-interview; at Waves III and IV, all respondents to the Wave I in-home interview were eligible for re-interview. A total of 15,701 interviews were conducted at Wave IV (80.3% response rate). Sampling weights adjusted for both unequal probabilities of selection into the original sample and for loss to follow-up. The present analysis was deemed exempt by the Institutional Review Board at Tulane University.
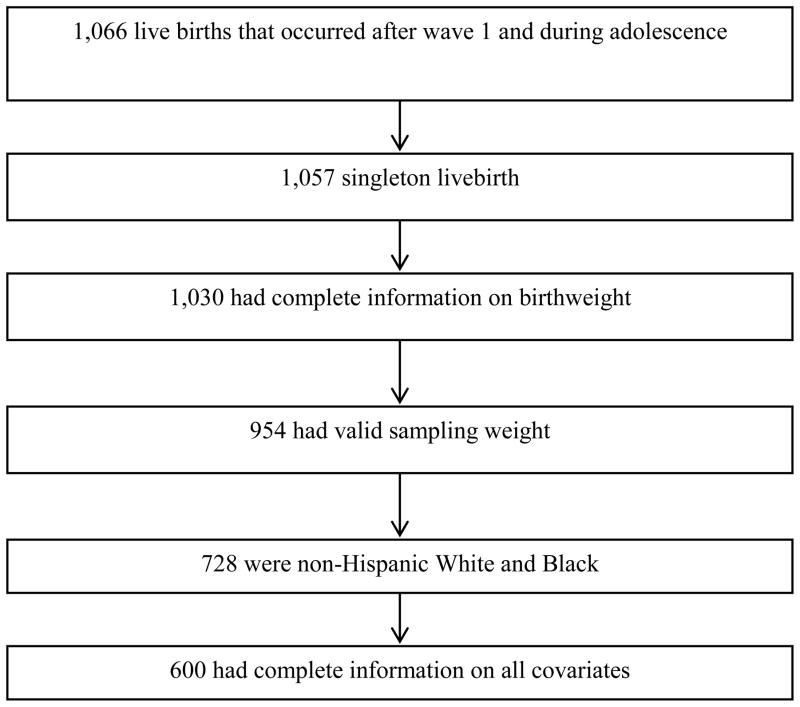
We applied a number of sample inclusion criteria (Figure 1). First we limited to females who participated in Wave IV, as that was the Wave when all respondents had completed their teenage years and had complete adolescent birth data. Second, we limited to females whose first births occurred during adolescence and after Wave I to ensure the temporal ordering of predictors and outcomes (n=1,066). Third, we limited to singleton live births with complete information on birthweight (n=1,030). Fourth, we limited to female participants with valid sampling weights in order to make generalizations to the U.S. population, and to adjust for loss to follow-up (n=954). Fifth, we limited to non-Hispanic White and Black females (n=728) because of the small number of adolescent mothers in other racial/ethnic groups. Finally, we limited to respondents with complete information on all analysis covariates. This left us with an analysis sample of 600 adolescent births.
Figure 1.
Sample inclusion criteria
Measures
Outcomes
At Wave IV girls were asked about previous pregnancies and their outcomes. If they had gotten pregnant, they were asked “How did this pregnancy end?”, with options of abortion, ectopic/tubal, miscarriage, stillbirth, and live birth. If they indicated they had given birth, they were asked “How much did the baby weigh at birth?”, and reported birthweight in pounds and ounces. We transformed birthweight into kilograms, and examined birthweight both in its continuous form and dichotomized to low birthweight (<2.5 kg vs. >2.5 kg) in order to capture a clinically problematic outcome.
Neighborhood Predictors
Two demographic aspects of neighborhood environments which have been linked with birth outcomes in past studies were examined as the main predictors. These were based on adolescents’ neighborhoods at the Wave most closely preceding the pregnancy (Wave I or II). First, neighborhood disadvantage was based on Census Block Group characteristics: proportion of households headed by a female, percent of people below poverty level, median household income (reverse coded), proportion of households with public assistance, proportion aged 25+ with no high school diploma or equivalency and unemployment rate. We ran a principal components analysis of these variables and applied factor loadings on the first principal component as item weights to generate a summary score. Second, Black racial concentration was measured as the Block Group percentage of residents who were Black. For bivariate and multivariable analyses we divided the percentage by 10, so that effect estimates could be interpreted as change in the outcome per 10% change in neighborhood percent Black.
Mediators
Three possible mediators of the relationship between neighborhood demographic characteristics and adolescent birthweight were examined. First, cigarette smoking during pregnancy was assessed at Wave IV for each pregnancy reported. Respondents were asked to report on an ordinal scale how many cigarettes they smoked during their pregnancy (none/a few cigarettes but not every week/a few cigarettes a week but not every day/10 or fewer a day/11–20 a day/21–30 a day/31 or more a day). We combined responses into three levels (none/less than daily/daily), due to sparseness across smoker frequencies in the sample. Adolescent cigarette smoking is more common in lower SES neighborhoods, but less common in neighborhoods with a high percentage of Black residents (34). Cigarette smoking is a known risk factor for adverse birth outcomes (35). Second, the timing of prenatal care initiation was based on two questions asked about each pregnancy reported at Wave IV: “During this pregnancy with [partner] did you ever visit a doctor, nurse-midwife or other health care provider for prenatal care, that is, for one or more pregnancy check-ups?” and “How many weeks pregnant were you at the time of your first prenatal care visit?” Responses to these two questions were combined and recoded to reflect prenatal care initiation in the first trimester versus no use or late initiation of prenatal care. Late entry into prenatal care has been linked with living in a socioeconomically deprived neighborhood, and also has been linked to adverse birth outcomes (36, 37). Third, the adolescent’s perception of neighborhood safety at the interview most closely preceding the pregnancy was based on the question: “Do you usually feel safe in your neighborhood?” Response options were yes or no. Neighborhood crime is more common in socioeconomically deprived neighborhoods, and has been associated with adverse birth outcomes in past studies (22, 38).
Controls and Modifiers
We drew upon our previous analysis of predictors of birth outcomes in this cohort to determine potential confounders (17). This analysis indicated effects of race, age at pregnancy, age at Wave I, parental education, and BMI. Individual race, parental education, and BMI are also likely to be correlated with neighborhood disadvantage and Black racial concentration, and thus potentially be confounders. Race/ethnicity was self-reported by the adolescent at Wave I, when they were asked two separate questions: “Which one category best describes your racial background?” (White/Black or African American/American Indian or Native American/Asian or Pacific Islander/Other), and “Are you of Hispanic or Latino origin?” (yes/no). We limited our sample to adolescents who reported non-Hispanic ethnicity and either Black or White race. Parental education was measured as the higher of either co-residential mother or father: less than high school diploma, high school diploma/General Equivalency Degree [GED], some postsecondary, college degree. BMI was based on self-reported weight and height, and was categorized as underweight, normal weight, overweight, and obese. All control and modifier variables except age at pregnancy were measured at Wave I.
Analyses
All analyses were conducted in SAS (SAS Institute, Cary, North Carolina) using survey procedures, which apply population weights and adjust standard errors for non-independence between observations due to school-based sampling. Analyses were run stratified on race (non-Hispanic Black/non-Hispanic White), given past analyses indicating racial differences in the predictors of birth outcomes among adolescent mothers (17), and studies in other samples indicating neighborhood effects on birth outcomes may vary by race (24, 28). We began with descriptive statistics (means and percentages) for all analysis variables, statistically comparing their distributions in non-Hispanic Black versus non-Hispanic White adolescent mothers using Chi-square or t-test analyses. We also conducted bivariate analyses (ordinary least squares [OLS] and logistic regression) to test the crude relationships between individual characteristics, neighborhood demographic characteristics and birthweight (continuous and low birthweight). To examine the adjusted relationship between neighborhood demographic characteristics and birthweight after controlling for individual characteristics, we implemented OLS and logistic regression models including neighborhood demographic characteristics and control variables. To test mediation, we added potential mediators (chosen based on significant bivariate relationships) in a subsequent step. Mediation was only assessed for the continuous birthweight outcome, because cell sizes were too small for mediation analyses to be supported with the dichotomized low birthweight outcome. Mediation was assessed based on change in effect estimates for neighborhood demographic features after inclusion of the mediating variable(s) (39). All models were run on a single level given 311 of the 416 neighborhoods included in the analysis included only one participant. Significance testing was conducted at α<0.05.
RESULTS
Descriptive Characteristics
Descriptive characteristics of the study sample by maternal race are presented in Table 1. Among both non-Hispanic Black and non-Hispanic White adolescent mothers, mean age at Wave I interview was around 15.5 years, while average age at pregnancy was nearly 18 years. Significantly more Black compared to White adolescent mothers were overweight or obese at baseline (27.60% vs. 12.62%). Approximately 18% of adolescent mothers’ parents had less than a high school education. Black adolescent mothers lived in significantly more disadvantaged and Black concentrated neighborhoods compared to White adolescent mothers. Although Black adolescent mothers were significantly more likely than White adolescent mothers to feel unsafe in their neighborhoods (22.5% vs. 9.3%), White mothers were significantly more likely to smoke during pregnancy (35.7% vs. 7.5%). No significant differences between groups were observed in timing of prenatal care initiation.
Table 1.
Singleton Live births from women whose first pregnancy occurred after wave 1 at the Add
| Non-Hispanic Black | Non-Hispanic White | P-value | |
|---|---|---|---|
|
|
|||
| Baseline age (mean[se]) | 15.61(0.23) | 15.49(0.16) | 0.65 |
| Age at pregnancy (mean[se]) | 17.73(0.09) | 17.93(0.09) | 0.12 |
| Baseline BMI category (n [%]) | <0.01 | ||
| Underweight | 23(9.64) | 61(17.92) | |
| Normal weight | 149(62.76) | 251(69.46) | |
| Over weight | 48(20.46) | 38(9.41) | |
| Obese | 16(7.14) | 14(3.21) | |
| Parental education (n [%]) | 0.99 | ||
| ≥HS | 201(82.00) | 297(81.97) | |
| less than HS | 35(18.00) | 67(18.03) | |
| Neighborhood disadvantage (mean[se]) | 0.98(0.14) | 0.17(0.11) | <0.01 |
| Proportion Black (mean[se]) | 0.59(0.05) | 0.06(0.02) | <0.01 |
| Neighborhood safety before conception (n | <0.01 | ||
| No | 53(22.45) | 33(9.27) | |
| Yes | 183(77.55) | 331(90.73) | |
| Cigarette smoking during pregnancy (n [%]) | <0.01 | ||
| None | 220(92.53) | 239(64.28) | |
| Less than daily | 8(3.75) | 56(15.39) | |
| Daily | 8(3.72) | 69(20.33) | |
| Initiation of prenatal care (n [%]) | 0.82 | ||
| None/late initiation | 47(17.14) | 54(18.03) | |
| Early initiation | 189(82.86) | 310(81.97) | |
| Birthweight (kg) | 3.04(0.05) | 3.28(0.03) | <0.01 |
| Low Birthweight (n [%]) | 22(10.74) | 30(7.20) | 0.26 |
Non-Hispanic Black adolescent mothers evidenced significantly lower birthweight compared to non-Hispanic White adolescent mothers (3.04kg vs. 3.28kg, Table 1). Birthweight was approximately normally distributed. Almost 9% of adolescent mothers gave birth to a low birthweight infant (10.74% among Black adolescent mothers, 7.20% among White adolescent mothers).
Bivariate Analyses
A number of individual and neighborhood characteristics were associated with continuous birthweight and low birthweight in bivariate analyses (Table 2). Among Black adolescent mothers, lower parental education was associated with greater continuous birthweight, as was neighborhood disadvantage and percent Black. Black racial concentration was also negatively associated with Black adolescent mothers’ likelihood of having a low birthweight baby. Although perceived neighborhood safety and early prenatal care use initiation were unassociated with continuous birthweight and low birthweight among Black mothers, smoking during pregnancy was positively associated with these outcomes. Among White adolescent mothers, none of the factors investigated were significantly associated with continuous birthweight in crude analyses, although low parent education appeared positively associated with White mothers’ likelihood of having a low birthweight baby.
Table 2.
Bivariate Analysis: Individual and neighborhood characteristics and Birthweight in Add
| Birthweight | Low Birthweight | |||
|---|---|---|---|---|
| Non-Hispanic Black (n=236) | Non-Hispanic White (n=364) | Non-Hispanic Black (n=236) | Non-Hispanic White (n=364) | |
|
|
|
|||
| Est. β (95%CI) | Est. β (95%CI) | OR (95%CI) | OR (95%CI) | |
| Baseline age | 0.00(−0.06,0.07) | 0.00(- | 1.00(0.75,1.34) | 0.94(0.67,1.32) |
| Age at pregnancy | 0.01(−0.05,0.06) | −0.02(- | 0.8(0.62,1.04) | 0.92(0.64,1.34) |
| Baseline BMI | 0.01(−0.01,0.03) | 0.02(- | 1.03(0.92,1.15) | 0.88(0.77,1.01) |
| Parental education | ||||
| ≥HS | ref * | ref | ref | ref * |
| less than HS | 0.22(0.03,0.41) | 0.05(- | 0.28(0.05,1.41) | 3.67(1.23, |
| Neighborhood | 0.09(0.01,0.17)* | 0.00(- | 0.63(0.29,1.37) | 1.00(0.46,2.18) 10.88) |
| Proportion Black¶ | 0.04(0.02,0.07) ** | −0.02(- | 0.78(0.67,0.92)** | 0.94(0.58,1.50) |
| Cigarette smoking | ||||
| No | ref * | ref | -- | -- |
| Less than daily | 0.27(−0.06,0.60) | 0.04(- | ||
| Daily | 0.31(0.04,0.57) | −0.15(- | ||
| Initiation of prenatal | ||||
| None/late initiation | 0.03(−0.11,0.18) | 0.11(- | -- | -- |
| Early initiation | ref | ref | ||
| Neighborhood safety before conception | ||||
| No | 0.05(−0.14,0.24) | 0.11(- | -- | -- |
| Yes | ref | ref | ||
P<0.05
P<0.01
Regression coefficients and odds ratios represent increases in birth weight per 10% increase in Percent Black
Multivariable Analyses – Continuous Birthweight
The relationship between neighborhood demographic characteristics and continuous birthweight after controlling for individual factors is presented in Table 3. Among non-Hispanic Black adolescent mothers, a 10% increase in neighborhood percent Black was associated with 0.04 kg greater birthweight (β̂ = 0.04, 95% CI 0.01–0.07 [Model 1]). Neighborhood disadvantage was no longer significantly associated with birthweight among Black adolescent mothers after controlling for other factors at the individual and neighborhood level. After adding cigarette smoking during pregnancy (Model 2), the association between neighborhood percent Black and birthweight remained largely the same (β̂ = 0.05, 95% CI 0.01–0.08), suggesting no mediation. However, cigarette smoking during pregnancy (both less than daily and daily) was significantly positively associated with birthweight. Similar to bivariate analyses, no factors at the individual or neighborhood level were significantly associated with birthweight among non-Hispanic White adolescent mothers.
Table 3.
Multivariable Analysis of neighborhood variables and birthweight (n=600)
| Non-Hispanic Black (n=236)
|
Non-Hispanic White (n=364)
|
||
|---|---|---|---|
| Model 1 Est. β (95%CI) | Model 2 Est. β (95%CI) | Model 1 Est. β (95%CI) | |
| Baseline age | −0.02(- | −0.03(- | 0.00(−0.05,0.05) |
| Age at pregnancy | 0.01(−0.05,0.06) | 0.00(−0.05,0.06) | −0.02(−0.08,0.05) |
| Baseline BMI | 0.01(−0.02,0.03) | 0.00(−0.02,0.02) | 0.01(−0.01,0.04) |
| Parental education | |||
| ≥HS | ref | ref | ref |
| less than HS | 0.17(−0.02,0.36) | 0.19(−0.01,0.39) | 0.02(−0.24,0.29) |
| Neighborhood disadvantage | 0.03(−0.06,0.12) | 0.02(−0.07,0.10) | 0.00(−0.07,0.08) |
| Proportion Black¶ | 0.04(0.01,0.07)* | 0.05(0.01,0.08)** | −0.02(−0.07,0.03) |
| Cigarette smoking during | |||
| No | ref* | ||
| Less than daily | 0.42(0.06,0.79) | ||
| Daily | 0.43(0.03,0.83) | ||
P<0.05
P<0.01
Regression coefficients represent increases in birth weight per 10% increase in proportion Black
Multivariable Analyses – Low Birthweight
Associations between neighborhood demographic characteristics and low birthweight controlling for individual factors are presented in Table 4. For Black adolescent mothers, a 10% increase in the proportion of neighborhood residents who are Black was associated with a 22% lower likelihood of giving birth to a low birthweight infant (AOR 0.78, 95% CI 0.61–0.99). For non-Hispanic White adolescent mothers, the only factor that was associated with giving birth to a low birthweight infant was low parent education (AOR 5.68, 95% CI 1.99,16.20).
Table 4.
Multivariable Analysis of neighborhood variables and low birthweight (n=600)
| Non-Hispanic Black (n=236) AOR (95% CI) |
Non-Hispanic White (n=364) AOR (95% CI) |
|
|---|---|---|
| Baseline age | 1.16(0.84,1.60) | 1.05(0.75,1.47) |
| Age at pregnancy | 0.75(0.55,1.01) | 0.97(0.63,1.48) |
| Baseline BMI | 1.05(0.95,1.17) | 0.82(0.69,0.97)* |
| Parental education | ||
| ≥HS | ref | ref |
| less than HS | 0.31(0.07,1.39) | 5.68(1.99,16.20)** |
| Neighborhood disadvantage | 0.95(0.41,2.20) | 0.85(0.42,1.69) |
| Proportion Black¶ | 0.78(0.61,0.99)* | 0.91(0.60,1.38) |
P<0.05
P<0.01
Odds ratios represent increases in low birthweight per 10% increase in proportion Black
DISCUSSION
Despite growing appreciation for the influence of contexts on health, relatively little is known about contextual contributors to birth outcomes among adolescent mothers. Past research has suggested factors such as neighborhood disadvantage and racial concentration could influence birth outcomes through their effects on prenatal care access, health behaviors affecting pregnancy, and stresses associated with high crime environments (40). The purpose of this study was to explore how neighborhood disadvantage and racial concentration are related to the birthweight of infants born to adolescent mothers.
After controlling for individual and other neighborhood characteristics, Black racial concentration was associated with improved birthweight among non-Hispanic Black adolescent mothers, and also reduced likelihood of an infant born with low birthweight. This is consistent with findings from some past studies that included both adult and adolescent mothers, but contrary to others (29, 30, 41). Given a minority of births included in past studies were to adolescent mothers, and age differences in estimated effects of racial concentration were not tested, it is possible that findings from this and prior studies do not conflict because racial concentration could affect adult and adolescent mothers differently. Studies examining neighborhood effects on birth outcomes have used a variety of racial concentration measures (i.e., dissimilarity index, index of isolation, percentage of Black residents), different analytic methods (i.e., single-level vs. multilevel), and have used data from a variety of samples (i.e., from multiple counties vs. a single state vs. national). Given the varying methodology across studies, it is difficult to pinpoint the sources of difference in findings.
There are a variety of reasons why Black racial concentration may be positively related to birthweight among Black adolescent mothers. Black women are more likely to give birth as adolescents than white women, so neighborhoods with a higher proportion of Black residents may have better caregiving and support for some pregnant adolescents (42). Racial concentration may also reduce adolescent mothers’ exposure to racism (43), which has been linked with adverse birth outcomes (44). It is also possible racially concentrated neighborhoods enable the development of Black political power, which in turn can affect birth outcomes and infant mortality (45). Further research on the mechanisms by which racial concentration affects Black adolescent mothers’ birth outcomes is warranted.
Neighborhood disadvantage and Black racial concentration were unrelated to birthweight outcomes among non-Hispanic White women in both crude and adjusted analyses. These findings suggest that the neighborhood factors we studied were not particularly influential for birthweight of the infants born to White adolescent mothers. It is possible that other aspects of neighborhood social environments, such as social support for adolescent mothers, may be more important in this group.
Surprisingly, we found that smoking during pregnancy was significantly positively related to Black adolescent mothers’ self-reported birthweight. Such smoking did not appear to mediate the association between neighborhood percent Black and birthweight outcomes. This finding runs counter to extensive literature documenting increased risk of adverse birth outcomes with smoking during pregnancy (35). We speculate that this unexpected result may be due to the very small number of Black adolescent mothers who reported any smoking during pregnancy (n=16), which may lead to spurious results. It is possible that smoking during pregnancy is correlated with another unmeasured factor that is positively related to birthweight. Sample selection biases are also possible, since our sample was limited to mothers who experienced a birth as an adolescent. In past analyses with this same cohort, comparing women who gave birth before versus after age 20, we found adolescent mothers were less likely to live with both biologic parents during adolescence and to be married at the time of the birth, but they were more likely to have low parent education (less than high school diploma), an unemployed parent, to smoke during pregnancy, and to have late or no prenatal care (17). Reporting biases may also have influenced results, since smoking during pregnancy is a highly stigmatized behavior. There also were weaknesses in the way smoking during pregnancy was measured. We don’t know, for example, whether smoking was restricted to the first trimester before the mother knew about her pregnancy, or whether smoking heaviness changed during pregnancy. Given all these potential issues with the ascertainment of smoking during pregnancy, results should be interpreted with caution.
Despite the strengths of the study, including the use of a large, national dataset and measurement of exposures prior to health outcomes, results should be interpreted with knowledge of the study limitations. First, we reduced sample size by requiring complete covariate data, which could bias our study results. Analyses comparing included versus excluded adolescents indicated no significant difference in birthweight (p=0.89), baseline age (p=0.39), age at pregnancy (p=0.17), parental education (p=0.48), or neighborhood disadvantage score (p=0. 68). However, adolescents who were included evidenced significantly lower BMI compared to those excluded (p<0.01). Second, neighborhood exposures were measured on average three years before adolescent births, and may not represent the neighborhood experiences of adolescents at the time of the pregnancy or birth if the adolescent moved in the interim. Despite this concern, research indicates that there may be relatively few demographic differences between neighborhoods when an individual moves, which may diminish this concern (46). Third, the analysis makes use of data from a school-based study, so students who dropped out of school before the first Wave are not included. This could possibly bias our sample toward more advantaged adolescent mothers – those who were able to stay in school. Fourth, this study relies on self-report of birthweight. Although maternal report of these outcomes is generally reliable (47–50) and these pregnancies had occurred fairly recently, this is a potential source of error. Although maternal age has not been related to accuracy of reporting in past studies (49, 51), ethnicity and SES have been found to predict errors (52). We did not include an examination of gestational age because it is ideally assessed with early ultrasound (53), especially for adolescents, who have more irregular menstrual cycles (54).
In summary, we found that neighborhood Black racial concentration was significantly associated with improved birthweight and lower likelihood of having an infant born with low birthweight among Black adolescent mothers. Although past studies are suggestive of potential pathways by which racial concentration may affect birth outcomes (i.e., through reduced exposure to racism or greater political power), further studies are needed to test these pathways among Black adolescent mothers. Such studies could inform intervention efforts to improve birth outcomes among Black adolescent mothers, especially those living outside racially concentrated neighborhoods.
References
- 1.Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary Data for 2010. National Vital Statistics Reports. 2011;60(2):1–25. [PubMed] [Google Scholar]
- 2.Chen XK, Wen SW, Fleming N, et al. Increased risks of neonatal and postneonatal mortality associated with teenage pregnancy had different explanations. J Clin Epidemiol. 2008;61(7):688–94. doi: 10.1016/j.jclinepi.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Alexander MR, Salihu HM, Rouse DJ. Survival of triplets who are born to teen mothers in the United States. Am J Obstet Gynecol. 2004;191(6):2097–102. doi: 10.1016/j.ajog.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 4.Phipps MG, Blume JD, DeMonner SM. Young maternal age associated with increased risk of postneonatal death. Obstet Gynecol. 2002;100(3):481–6. doi: 10.1016/s0029-7844(02)02172-5. [DOI] [PubMed] [Google Scholar]
- 5.Salihu HM, Sharma PP, Ekundayo OJ, et al. Childhood pregnancy (10–14 years old) and risk of stillbirth in singletons and twins. J Pediatr. 2006;148(4):522–6. doi: 10.1016/j.jpeds.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 6.Chen XK, Wen SW, Fleming N, et al. Teenage pregnancy and congenital anomalies: which system is vulnerable? Hum Reprod. 2007;22(6):1730–5. doi: 10.1093/humrep/dem043. [DOI] [PubMed] [Google Scholar]
- 7.Koniak-Griffin D, Turner-Pluta C. Health risks and psychosocial outcomes of early childbearing: a review of the literature. J Perinat Neonatal Nurs. 2001;15(2):1–17. doi: 10.1097/00005237-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ayoola AB, Brewer J, Nettleman M. Epidemiology and prevention of unintended pregnancy in adolescents. Prim Care. 2006;33(2):391–403. doi: 10.1016/j.pop.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Chandra PC, Schiavello HJ, Ravi B, et al. Pregnancy outcomes in urban teenagers. Int J Gynaecol Obstet. 2002;79(2):117–22. doi: 10.1016/s0020-7292(02)00240-0. [DOI] [PubMed] [Google Scholar]
- 10.Phipps MG, Sowers M, DeMonner SM. The risk for infant mortality among adolescent childbearing groups. J Womens Health (Larchmt) 2002;11(10):889–97. doi: 10.1089/154099902762203722. [DOI] [PubMed] [Google Scholar]
- 11.Martin JA, Hamilton BE, Sutton PD, et al. Births: Final Data for 2005. National Vital Statistics Reports. 2007;56(6):65. [PubMed] [Google Scholar]
- 12.Ekwo EE, Moawad A. Maternal age and preterm births in a black population. Paediatr Perinat Epidemiol. 2000;14(2):145–51. doi: 10.1046/j.1365-3016.2000.00234.x. [DOI] [PubMed] [Google Scholar]
- 13.Markovitz BP, Cook R, Flick LH, et al. Socioeconomic factors and adolescent pregnancy outcomes: distinctions between neonatal and post-neonatal deaths? BMC Public Health. 2005;5:79. doi: 10.1186/1471-2458-5-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robson S, Cameron CA, Roberts CL. Birth outcomes for teenage women in New South Wales, 1998–2003. Aust N Z J Obstet Gynaecol. 2006;46(4):305–10. doi: 10.1111/j.1479-828X.2006.00597.x. [DOI] [PubMed] [Google Scholar]
- 15.Reime B, Schucking BA, Wenzlaff P. Reproductive outcomes in adolescents who had a previous birth or an induced abortion compared to adolescents’ first pregnancies. BMC Pregnancy Childbirth. 2008;8:4. doi: 10.1186/1471-2393-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haeri S, Guichard I, Baker AM, et al. The effect of teenage maternal obesity on perinatal outcomes. Obstet Gynecol. 2009;113(2 Pt 1):300–4. doi: 10.1097/AOG.0b013e3181945b8a. [DOI] [PubMed] [Google Scholar]
- 17.Harville EW, Madkour AS, Xie Y. Predictors of birthweight and gestational age among adolescents. American Journal of Epidemiology. 2012;176(supplement 7):S164–S74. doi: 10.1093/aje/kws231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Browning C, Leventhal T, Brooks-Gunn J. Neighborhood context and racial differences in early adolescent sexual activity. Demography. 2004;41(4):697–720. doi: 10.1353/dem.2004.0029. [DOI] [PubMed] [Google Scholar]
- 19.Fite PJ, Wynn P, Lochman JE, et al. The influence of neighborhood disadvantage and perceived disapproval on early substance use initiation. Addict Behav. 2009;34(9):769–71. doi: 10.1016/j.addbeh.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sampson RJ. Collective Regulation of Adolescent Misbehavior. Journal of Adolescent Research. 1997;12(2):227–44. doi: 10.1177/0743554897122005. [DOI] [Google Scholar]
- 21.Charreire H, Combier E. Poor prenatal care in an urban area: A geographic analysis. Health Place. 2009;15(2):412–9. doi: 10.1016/j.healthplace.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277(5328):918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 23.Mollborn S. Norms about nonmarital pregnancy and willingness to provide resources to unwed parents. Journal of Marriage and Family. 2009;71(1):122–34. doi: 10.1111/j.1741-3737.2008.00584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Campo P, Burke JG, Culhane J, et al. Neighborhood Deprivation and Preterm Birth among Non-Hispanic Black and White Women in Eight Geographic Areas in the United States. American Journal of Epidemiology. 2008;167(2):155–63. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- 25.Elo IT, Culhane JF, Kohler IV, et al. Neighbourhood deprivation and small-for-gestational-age term births in the United States. Paediatric and Perinatal Epidemiology. 2009;23(1):87–96. doi: 10.1111/j.1365-3016.2008.00991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. American journal of public health. 2001;91(11):1808–14. doi: 10.2105/ajph.91.11.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farley TA, Mason K, Rice J, et al. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatric and Perinatal Epidemiology. 2006;20(3):188–200. doi: 10.1111/j.1365-3016.2006.00719.x. [DOI] [PubMed] [Google Scholar]
- 28.Buka SL, Brennan RT, Rich-Edwards JW, et al. Neighborhood Support and the Birth Weight of Urban Infants. American Journal of Epidemiology. 2003;157(1):1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- 29.Bell JF, Zimmerman FJ, Almgren GR, et al. Birth outcomes among urban African-American women: A multilevel analysis of the role of racial residential segregation. Social Science & Medicine. 2006;63(12):3030–45. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 30.Mason SM, Messer LC, Laraia BA, et al. Segregation and preterm birth: The effects of neighborhood racial composition in North Carolina. Health & Place. 2009;15(1):1–9. doi: 10.1016/j.healthplace.2008.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leventhal T, Brooks-Gunn J. Diversity in developmental trajectories across adolescence: Neighborhood influences. In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology. 2. Hoboken, NJ: John Wiley & Sons, Inc; 2004. pp. 451–86. [Google Scholar]
- 32.Harris KM. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [machine-readable data file and documentation] Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2009. [Google Scholar]
- 33.Harris KH. Design Features of Add Health. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2011. [Google Scholar]
- 34.Xue Y, Zimmerman MA, Caldwell CH. Neighborhood residence and cigarette smoking among urban youths: the protective role of prosocial activities. American journal of public health. 2007;97(10):1865–72. doi: 10.2105/AJPH.2005.081307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Floyd RL, Rimer BK, Giovino GA, et al. A review of smoking in pregnancy: effects on pregnancy outcomes and cessation efforts. Annual review of public health. 1993;14:379–411. doi: 10.1146/annurev.pu.14.050193.002115. [DOI] [PubMed] [Google Scholar]
- 36.Perloff JD, Jaffee KD. Late Entry into Prenatal Care: The Neighborhood Context. Social Work. 1999;44(2):116–28. doi: 10.1093/sw/44.2.116. [DOI] [PubMed] [Google Scholar]
- 37.Debiec KE, Paul KJ, Mitchell CM, et al. Inadequate prenatal care and risk of preterm delivery among adolescents: a retrospective study over 10 years. American Journal of Obstetrics and Gynecology. 2010;203(2):122.e1–.e6. doi: 10.1016/j.ajog.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 38.Messer LC, Kaufman JS, Dole N, et al. Neighborhood Crime, Deprivation, and Preterm Birth. Annals of Epidemiology. 2006;16(6):455–62. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 39.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 40.Schempf A, Strobino D, O’Campo P. Neighborhood effects on birthweight: An exploration of psychosocial and behavioral pathways in Baltimore, 1995–1996. Social Science & Medicine. 2009;68(1):100–10. doi: 10.1016/j.socscimed.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Debbink MP, Bader MD. Racial residential segregation and low birth weight in Michigan’s metropolitan areas. Am J Public Health. 2011;101(9):1714–20. doi: 10.2105/ajph.2011.300152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kost K, Henshaw S. US Teenage Pregnancies, Births and Abortions, 2008: National Trends by Age, Race and Ethnicity. New York: Guttmacher Institute; 2012. [Google Scholar]
- 43.Pickett KE, Collins JW, Jr, Masi CM, et al. The effects of racial density and income incongruity on pregnancy outcomes. Social Science & Medicine. 2005;60(10):2229–38. doi: 10.1016/j.socscimed.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 44.Collins JWJ, David RJ, Symons R, et al. Low-Income African-American Mothers’ Perception of Exposure to Racial Discrimination and Infant Birth Weight. Epidemiology. 2000;11(3):337–9. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 45.LaVeist TA. Segregation, Poverty, and Empowerment: Health Consequences for African Americans. The Milbank Quarterly. 1993;71(1):41–64. doi: 10.2307/3350274. [DOI] [PubMed] [Google Scholar]
- 46.Sampson Robert J. Moving to Inequality: Neighborhood Effects and Experiments Meet Social Structure. American Journal of Sociology. 2008;114(1):189–231. doi: 10.1086/589843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sou SC, Chen WJ, Hsieh WS, et al. Severe obstetric complications and birth characteristics in preterm or term delivery were accurately recalled by mothers. J Clin Epidemiol. 2006;59(4):429–35. doi: 10.1016/j.jclinepi.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 48.Jaspers M, de Meer G, Verhulst FC, et al. Limited validity of parental recall on pregnancy, birth, and early childhood at child age 10 years. Journal of Clinical Epidemiology. 2010;63(2):185–91. doi: 10.1016/j.jclinepi.2009.05.003. S0895-4356(09)00151-6 [pii] [DOI] [PubMed] [Google Scholar]
- 49.Adegboye AR, Heitmann B. Accuracy and correlates of maternal recall of birthweight and gestational age. BJOG. 2008;115(7):886–93. doi: 10.1111/j.1471-0528.2008.01717.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hakim RB, Tielsch JM, See LC. Agreement between maternal interview- and medical record-based gestational age. Am J Epidemiol. 1992;136(5):566–73. doi: 10.1093/oxfordjournals.aje.a116534. [DOI] [PubMed] [Google Scholar]
- 51.Seidman DS, Slater PE, Ever-Hadani P, et al. Accuracy of mothers’ recall of birthweight and gestational age. Br J Obstet Gynaecol. 1987;94(8):731–5. doi: 10.1111/j.1471-0528.1987.tb03717.x. [DOI] [PubMed] [Google Scholar]
- 52.Tate AR, Dezateux C, Cole TJ, et al. Factors affecting a mother’s recall of her baby’s birth weight. Int J Epidemiol. 2005;34(3):688–95. doi: 10.1093/ije/dyi029. [DOI] [PubMed] [Google Scholar]
- 53.Lynch CD, Zhang J. The research implications of the selection of a gestational age estimation method. Paediatr Perinat Epidemiol. 2007;21(S2):86–96. doi: 10.1111/j.1365-3016.2007.00865.x. [DOI] [PubMed] [Google Scholar]
- 54.Sanfilippo JS, Lara-Torre E. Adolescent gynecology. Obstet Gynecol. 2009;113(4):935–47. doi: 10.1097/AOG.0b013e31819b6303. [DOI] [PubMed] [Google Scholar]