Abstract
The authors aimed to determine the economic value of providing on-site group cognitive behavioral therapy (CBT) for depression to clients receiving residential substance use disorder (SUD) treatment. Using a quasi-experimental design and an intention-to-treat analysis, the incremental cost-effectiveness and cost-utility ratio of the intervention were estimated relative to usual care residential treatment. The average cost of a treatment episode was $908, compared to $180 for usual care. The incremental cost effectiveness ratio was $131 for each point improvement of the BDI-II and $49 for each additional depression-free day. The incremental cost-utility ratio ranged from $9,249 to $17,834 for each additional quality adjusted life year. Although the intervention costs substantially more than usual care, the cost effectiveness and cost-utility ratios compare favorably to other depression interventions. Health care reform should promote dissemination of group CBT to individuals with depression in residential SUD treatment.
INTRODUCTION
Most Americans with depressive disorders do not receive evidence-based treatment, and among individuals with co-occurring substance use disorders (SUD), rates of evidence-based depression treatment are even lower (Gonzalez et al., 2010; Wang et al., 2005; Watkins et al., 2011). This unmet need has serious consequences. Individuals with co-occurring depression and SUDs experience greater impairment and worse outcomes than persons with only a single disorder. By 2030 depressive disorders are expected to be the leading cause of disability in the United States (Mathers & Loncar, 2006) and, in substance users, depressed mood is associated with relapse to substance use (Kelly, Stout, Magill, Tonigan, & Pagano, 2010; Witkiewitz & Villarroel, 2009) and suicide. Although effective depression treatments exist, few publicly-funded substance use providers have the capacity to deliver these treatments, and limited resources in the public sector constrain access to mental health treatment for depression.
Policy decisions about coverage and reimbursement need to take into account the cost-effectiveness of different health care interventions and balance potential costs against benefits (“Patient Protection and Affordable Care Act,” March 23, 2010). Earlier results from the Building Recovery by Improving Goals, Habits and Thoughts (BRIGHT) (“Building Recovery by Improving Goals, Habits, & Thoughts,” 2011) study indicated that group cognitive behavioral therapy improved both depression and substance use outcomes in individuals receiving residential substance use treatment when compared to residential substance use treatment alone (Watkins, et al., 2011). Because the treatment is delivered in a group format and can be provided by trained substance use counselors, it may increase the availability of evidence-based depression treatment at a lower cost and be more feasible than either pharmacotherapy or individual psychotherapy.
The purpose of the present analysis is to determine, based on the findings from BRIGHT, the economic value of providing on-site group cognitive behavioral therapy for depression to clients receiving residential substance abuse treatment. The cost-effectiveness of depression treatment for individuals in substance use treatment has not yet been evaluated. Our hypothesis was that the total direct medical costs would be higher in the intervention condition when compared to usual care for at least two reasons. First, the intervention uses more resources (e.g. client and provider manuals), than usual care. Second, the intervention was jointly delivered by two substance abuse treatment counselors, whereas usual-care groups are typically led by a single counselor. We also hypothesized that the cost-effectiveness of BRIGHT (“Building Recovery by Improving Goals, Habits, & Thoughts,” 2011) would be similar to, or lower than, other existing depression interventions because of the reliance on bachelor-level counselors to deliver the intervention.
We report on the cost of the BRIGHT intervention, the cost-effectiveness of BRIGHT on depression and substance use outcomes, and the cost-utility of the intervention. Effectiveness results have been reported previously (Watkins, et al., 2011).
MATERIALS AND METHODS
BRIGHT was a quasi-experimental clinical trial in which cohorts of clients at four study sites were alternately assigned to receive either residential treatment as usual (UC) or residential treatment enhanced with the BRIGHT intervention (BRIGHT) (“Building Recovery by Improving Goals, Habits, & Thoughts,” 2011) provided by trained substance abuse counselors. The assignment pattern alternated every four months and continued for a two-and-a-half-year enrollment period. Study sites were the four residential sites operated by Behavioral Health Services, one of the largest publicly-funded substance abuse treatment providers in Los Angeles County. In 2009, 26% of SUD treatment facilities offered residential treatment outside of a hospital (Substance Abuse and Mental Health Administration, 2012). The RAND human subjects protection committee approved the study protocol.
BRIGHT (“Building Recovery by Improving Goals, Habits, & Thoughts,” 2011) consisted of 16 two-hour sessions of group cognitive behavioral therapy; clients who were assigned to BRIGHT attended a mean of 10.5 sessions (SD=5.5) and 69% attended at least half of the 16 sessions. While participating in the BRIGHT(“Building Recovery by Improving Goals, Habits, & Thoughts,” 2011) group, other group commitments were reduced accordingly (i.e., BRIGHT participation counted as 2 groups per week), suggesting that all clients should have received the same number of group sessions per week. Usual care treatment was standardized across all four sites and consisted of individual substance use treatment counseling, group therapy, vocational skills training, AA/NA/CA, recreational therapy and family services. To prevent usual care clients from being inadvertently exposed to the intervention, outpatient counselors employed by the same parent organization and with similar qualifications and experience to residential treatment counselors travelled to the residential sites to deliver the intervention. Outpatient counselors had no contact with usual care clients. Five outpatient counselors were trained.
We screened 1,262 clients, and 299 clients with persistent depressive symptoms were enrolled. We defined persistent depressive symptoms as symptoms that were measured on two separate occasions after at least two weeks of sobriety. Eligible clients scored five or greater on the Patient Health Questionnaire-8 and 18 or greater on the Beck Depression Inventory II (BDI-II). The current analysis includes all 256 clients who had 6-month outcome data out of the initial sample of 299 clients, as outcome data from only the six-month time period was used to estimate QALYs. We conducted analyses to confirm that responders do not significantly differ from non-responders at either follow-up with respect to baseline characteristics.
Costs
We account for the costs from the perspective of the health care provider. Our cost estimates include service-level direct medical and non-medical costs (Gold, Siegel, Russell, & Weinstein, 1996).
The primary component of service-level costs is that associated with the time and labor costs of the counselors, trainers and supervisors. We collected the time spent in training and supervision, and the counselors kept logs for the first eleven months of the intervention that documented the time spent preparing, delivering, documenting and travelling to and from group sessions. We applied the average counselor wage rate ($17.30 including fringe benefits) across the sites to the number of hours worked. Separately, we calculated the service-level costs for contracted trainers and supervisors, using their reported hours and wages ($62 per hour) and including travel-time costs. In addition, for the didactic training we included direct non-service costs, such as manuals and workbooks, audio-visual equipment, and meals. Costs were adjusted for the consumer price index and are presented in 2009 dollars. All service-level costs were divided into training and implementation phases and exclude costs associated with research activities.
For the usual care residential counselors, we calculated training costs as time spent in continuing education training (8 hours) multiplied by wages. We assumed zero non-labor costs to the agency associated with the continuing education. Time for the two usual care counselors was estimated at two hourly sessions per week. The total number of sessions for both the intervention and usual care was 246 sessions across the intervention period. In our per client cost calculations we standardize the number of clients, using the average number of clients in each study arm or 149.5 clients.
Time costs associated with screening and identifying clients with depression and orienting them to the intervention, as well the cost of materials and office space, are included in the cost analysis. These costs are included through the estimated indirect labor and nonlabor cost rates, which are the same for the intervention and usual care conditions.
We used a modified SASCAP data collection instrument to capture cost of benefits associated direct labor, indirect labor and nonlabor costs in a manner consistent with economic rather than accounting definitions of these concepts (Zarkin, Dunlap, & Homsi, 2004). SASCAP was designed for methadone clinics and we modified the instrument to reflect the residential treatment setting. We collected information on indirect labor resources (e.g., costs for administrative duties) that are not linked to specific services, and nonlabor resources (e.g., costs for building space, contracted services, supplies and materials) over three years. These indirect resources were calculated as percentages of direct client services costs and applied to the direct counselor labor cost estimates. The indirect and nonlabor cost rates are the same across the two treatment conditions so that variation in costs across treatments is driven completely by the differences in labor costs.
Follow-up costs associated with subject tracking were considered research costs and were excluded from the analysis. We excluded the value of clients’ time spent receiving treatment because the clients are in a residential treatment facility and as such do not have the opportunity to work. Therefore, their wage (or potential wage rate) is not a very good approximation to the value (or opportunity cost) of their time in treatment.
We conducted sensitivity analyses by projecting the costs of the intervention if it were implemented under non-research conditions. We assumed lower estimated training costs because of lower material costs, three counselors trained instead of five, and one trainer instead of two. In addition, we assumed there would be less preparation time, as prepared materials are now available, and no travel time for counselors to go from the outpatient to the residential setting. Our projection further assumes delivering the intervention for one year with 6 cohorts of clients treated twice weekly for 8 weeks, i.e., a total of 96 sessions. We assumed each cohort contained 10 clients (the maximum recommended number of clients per group), for a total of 60 clients treated in a one-year period. This compares to 149.5 average clients across the treatment and intervention groups which ran for two and one-half years and for a total of 245 sessions.
The projected costs are hypothetical and intended to inform program implementation and provide sensitivity analyses. We present these results using a range of wages that take into account staffing with typical addiction counselors (as was the case in the BRIGHT trial), as well as potential staffing with doctoral-level therapists. The doctoral level wage rate was obtained from the Los Angeles County Department of Mental Health.
Outcomes
Our primary mental health outcomes were depression symptoms, as measured by the BDI-II, and health status, as measured by the Short- Form-12 (SF-12). Decreases in the BDI-II reflect mental health improvements while the opposite is the case for the SF-12. These outcomes were collected at three and six months after study enrollment. The primary substance use outcome was days of self-reported use of problem substance on days available for use (i.e., when client was not institutionalized) during past 30 days, collected at six months after study enrollment. Thirty-day use was converted to 90-day use by multiplying by 3. We assumed no substance use during the first three months, as most clients were still in treatment the first three months. Previous studies suggest the validity of self-reported mental health and substance use outcomes, and the measures we used are based on previously-validated scales (Brown, Kranzler, & Del Boca, 1992; Fals-Stewart, O'Farrell, Freitas, McFarlin, & Rutigliano, 2000; Rush et al., 2006; Sobell, Maisto, Sobell, & Cooper, 1979; Sobell & Sobell, 1978; Weiss et al., 1998; Zimmerman, Coryell, Wilson, & Corenthal, 1986).
Quality adjusted life years (QALYs) are a measure of health outcome reflecting patient preferences over both length and quality of life, combined into a single metric. QALYs facilitate comparison across disease states and interventions. QALYs are measured on a scale that ranges from 0 to 1, where 0 corresponds to death and 1 corresponds to perfect health (Gold, et al., 1996). We obtain 6-month QALYs from the SF-12 using a preference-based scoring algorithm, which offers strong methodological and theoretical properties (Brazier & Roberts, 2004; Pickard, Wang, Walton, & Lee, 2005). The use of the SF-12 as a measure of longitudinal preference-weighted health-related quality of life in both substance using populations and depressed populations has been previously validated (Lenert, Sherbourne, Sugar, & Wells, 2000; Mann, Gilbody, & Richards, 2009; Pyne, Tripathi, Williams, & Fortney, 2007).
A selection of health states was derived from combinations of the SF-12 items. Model-based coefficient weights for these combinations were then applied to individual SF-12 responses in order to calculate QALYs. For each participant, a QALY is calculated using baseline, 3-month and 6-month SF-12 responses. We estimate the differential mean QALY between BRIGHT and usual care, controlling for the baseline QALY score (Manca, Hawkins, & Sculpher, 2005). Given the time horizon of the analysis, QALYs were not discounted.
We also estimated 6-month QALYs based on changes in depression-free days and converted our measure of disease-specific symptom severity to utility-weighted scores (Chouinard & Albright, 1997; Katon et al., 2006; Lave, Frank, Schulberg, & Kamlet, 1998). One advantage of converting disease specific scores to utility weights is that disease-specific scores are more sensitive to disease-specific symptom change. The conversion formula assumes that a nondepressed person has a utility score of 1.0 and a severely depressed person has a utility score of 0.6 (Pyne, et al., 2007). We calculated the number of depression-free days based on a cut-off for minimal depression, which on the BDI-II is 13 and below, and a cut-off for severe depression which is 29 or above (Beck, Steer, Ball, & Ranieri, 1996). Those with BDI between 14 and 29 were assigned a value that was weighted proportionately. As an additional sensitivity analysis, we assumed a utility score of 0.7 instead of 0.6 for a severely depressed person.
Analyses
The effect of BRIGHT on BDI-II and SF-12 scores, days of problem substance use and QALYs was examined at 3- and 6-months. The differences in outcomes are measured from multivariate models that regress the 6-month outcome on the baseline value and the intervention indicator (Manca, et al., 2005). Each outcome was modeled using mixed effects regression modeling, in which the centered baseline value of the outcome was included as a covariate. Random client effects accounted for the non-independence, or intra-cluster correlation (ICC), of outcomes repeatedly observed for clients at 3- and 6-months. A multiple membership modeling approach was used to account for the ICC of outcomes among those who attended group CBT sessions together, which involved including random CBT session effects in the model and estimating the client-specific session effect as an average of the random session effects for those sessions attended by the client (Paddock & Savitsky, 2013). An indicator variable of intervention assignment, follow-up wave (3 or 6 months), and an interaction of these two measures were included as predictor variables. Intervention effects on BDI-II, days of problem substance use, QALYs and SF-12 at 3 and 6 months were estimated from these coefficients and tested using two-sided t-tests.
The incremental cost effectiveness ratio (ICER) between the intervention and control groups is calculated by dividing the difference in costs between BRIGHT and usual care by the difference in outcomes between BRIGHT and usual care. When the outcome is expressed in QALYs, it yields the incremental cost utility ratio (ICUR).
RESULTS
Table 1 summarizes the costs of the BRIGHT intervention as implemented, by training and intervention phases. The average cost per BRIGHT client was $908, 25 percent of which was for training, compared to $180 for usual care, for which 14 percent was for training.
Table 1.
BRIGHT Intervention and Usual Care Costs, in 2009 Dollars
| BRIGHT Intervention | Usual Care | |
|---|---|---|
| Training Phase | ||
| Nonlabor1 | $ 2,059 | $ - |
| Labor2 | $20,559 | $ 2,449 |
| Indirect | $ 8,779 | $ 968 |
| Total | $31,396 | $ 3,417 |
| Intervention Phase | ||
| Nonlabor1 | $ 5,887 | $ - |
| Labor2 | $57,481 | $12,759 |
| Indirect | $32,817 | $ 9,116 |
| Total | $96,184 | $21,875 |
| # clients | 149.50 | 149.50 |
| Training per client | $ 223 | $ 24 |
| Intervention per client | $ 685 | $ 156 |
| Total per client | $ 908 | $ 180 |
includes manuals and workbooks, audio-visual equipment, and other supplies
includes direct labor costs (wages and fringe benefits) associated with training, preparation, and travel for group sessions on the part of counselors and trainers
3 includes labor that is not tied to specific treatment services (e.g., depression screening and administrative duties) and nonlabor resources (e.g., costs for building space, contracted services, supplies and materials)
Table 2 presents the projected costs of BRIGHT which rely on fewer trainers and fewer counselors trained. If counselors are at the bachelor-level (A) then the projected average cost per client is $746 of which 29 percent represents training costs, a slightly higher fraction than in the intervention as implemented. If counselors are clinical psychologists, (B) rather than bachelor-level counselors, then the projected cost per client rises to $1,896.
Table 2.
Sensitivity Analyses to Project BRIGHT Costs Using Bachelor and Doctoral-Level Therapists, in 2009 Dollars
| Bachelora | Doctoralb | |
|---|---|---|
| Training Phase | ||
| Nonlabor | $ 1,040 | $ 1,040 |
| Labor | $ 7,808 | $17,036 |
| Indirect | $ 3,267 | $10,420 |
| Total | $12,115 | $28,496 |
| Intervention Phase | ||
| Nonlabor | $ 3,300 | $ 3,300 |
| Labor | $17,402 | $45,656 |
| Indirect | $ 9,227 | $29,433 |
| Total | $29,930 | $78,389 |
| # clientsc | 60 | 60 |
| Training per client | $ 215 | $ 505 |
| Intervention per client | $ 531 | $ 1,390 |
| Total per client | $ 746 | $ 1,896 |
Counselors at bachelors level. Trainers are doctoral level.
Counselors and trainers at doctoral level.
6 rounds with 10 patients per round over one year.
Table 3 presents incremental cost-effectiveness and cost-utility ratios. The first column reflects BRIGHT as implemented, and the next column reflects the sensitivity analysis using our assumptions about how BRIGHT would be implemented under non-research settings. The changes in outcomes are based on 6-month estimates previously reported. The ICER for the intervention as implemented is $131 for each point decrement of the BDI and $41 for each additional depression-free day. The intervention improved self-reported mental health, as measured by the SF-12 mental component scale (MCS), and the cost per unit improvement in the SF-12 MCS is estimated to be $157. However, reflecting the fact that there was a reduction in the physical component scale (PCS), albeit not statistically significant, the ICER for this small decline is substantially higher ($3,033). The differential cost of decreasing the number of problem substance use days is $237.
Table 3.
Cost Effectiveness/Cost Utility Ratios, Associated With BRIGHT vs. Usual Care, as Implemented and Projected.
| Change in Outcomes BRIGHT vs. Usual Care | BRIGHT Intervention | Projected | |
|---|---|---|---|
| Mean | Incremental Cost Effectiveness Ratioa (Confidence Interval) | ||
| BDIb | −5.56 | −$131 (−$303, −$83) | −$102 (−$236, −$65) |
| Depression-free days | 17.70 | $41 (−$100, $17) | $32 (−$78, $13) |
| SF-12 PCSc | −0.24 | −$3,033 (−$315, $400) | −$2,358 (−$245, $311) |
| SF-12 MCSd | 4.63 | $157 ($499, $93) | $122 ($388, $73) |
| Problem substance use days | −9.21 | −$237 (−$1,820, −$127) | −$184 (−$1,415, −$98) |
| Incremental Cost Utility Ratioe | |||
| $ per QALYf gained, SF-12g (at 6 months) | .04 | $17,834 ($10,224, $69,782) | $13,866 ($7,949, $54,253) |
| $ per QALY gained, depression-free daysh (at 6 months) | .06 | $12,332 ($8,394, $23,226) | $9,588 ($6,526, $18,058) |
| $ per QALY gained, depression-free daysi (at 6 months) | 0.08 | $9,249 ($6,337, $17,109) | $7,190 ($4,927, $13,301) |
ICER: calculated as (cost of BRIGHT – Cost of UC)/(Change in Outcome for BRIGHT– Change in Outcome for UC)
BDI = Beck Depression Inventory
PCS = Physical Component Score
MCS = Mental Component Score
ICUR: calculated as (cost of BRIGHT – Cost of UC)/(Change in QALY for BRIGHT– Change in QALY for UC)
QALY = Quality Adjusted Life Year
Based on preference based weights applied to the SF-12 ((Brazier & Roberts, 2004)).
Assumes a 0.40 gain of quality-adjusted day when one moves from being fully depressed to being symptom free.
Assumes a 0.30 gain of a quality-adjusted day when one moves from being fully depressed to being symptom free.
The ICUR estimates vary depending on whether they are derived from the SF-12 or from the utility gains that arise from depression free days. The estimates for BRIGHT, as implemented in the trial, range from $17,834 based on the SF-12 and $9,249 to $12,332 based on depression free days. For the sensitivity analyses the SF-12-based ICUR is $13,866.
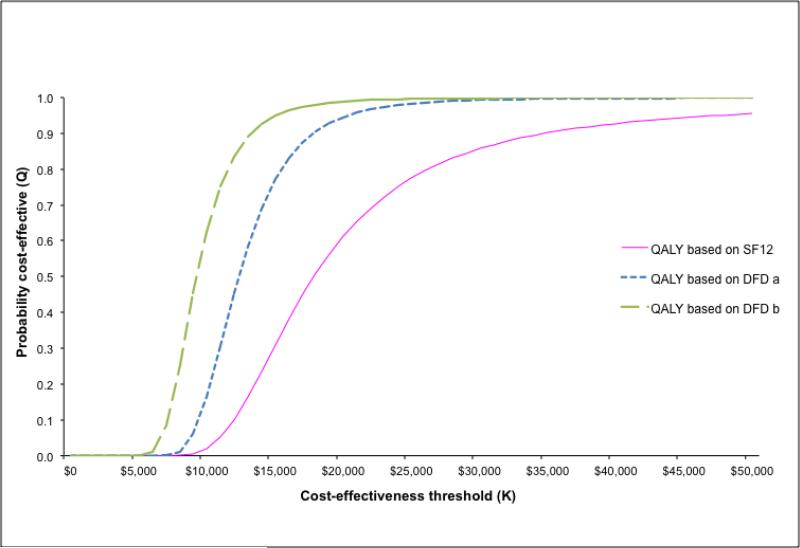
Figure 1 presents cost effectiveness acceptability curves based on QALYs attained derived from the SF-12 and DFD measures. The figure shows that if society places a $20,000 value on a QALY then there is a 90% chance that BRIGHT is more cost-effective than usual care if DFDs are associated with the lower utility differential and a 99% chance that BRIGHT is more cost-effective if DFDs are associated with the higher utility differential. When QALYs are measured using the SF12, the figure shows that there is a 90% chance that BRIGHT is more cost-effective at $35,000.
Figure 1. Cost-Effectiveness Acceptability Curve for BRIGHT Intervention vs Usual Care.
US Dollars per Increase in quality-adjusted life years
a Assumes a 0.30 gain of a quality-adjusted day when one moves from being fully depressed to being symptom free.
b Assumes a 0.40 gain of a quality-adjusted day when one moves from being fully depressed to being symptom free.
DISCUSSION
This is the first trial to evaluate the cost-effectiveness of depression treatment for individuals in substance abuse treatment and adds to the literature on the cost-effectiveness of depression treatment. We show that it costs $908 per client to provide an evidence-based depression treatment to individuals in residential substance use treatment, which is an increase of $728 over usual care. The increased costs are primarily labor costs and are primarily a function of using two co-therapists to deliver the BRIGHT intervention. Under non-research conditions, we estimate that it would cost $746 to deliver BRIGHT if bachelor-level counselors were used and $1,896 using doctoral-level therapists.
Although BRIGHT costs substantially more than the cost of usual residential care, the ICER and ICUR of the mental health outcomes compare favorably to other depression interventions in the literature. Under non-research conditions and using bachelor-level counselors, we show depression ICURs that range from $8,576 to $11,440 per QALY. We compared BRIGHT to other therapy and pharmacologic interventions for depression that do not include a screening component and which did not target individuals with co-occurring disorders. Adjusting these prior estimates for inflation, Pyne et al.(Pyne et al., 2003) report an ICUR of $7,500 per QALY, Revicki et al. (Revicki et al., 2005) report $13,500 per QALY for therapy and for medication; while Lave et al. estimate $22,900 to $29,700 per QALY for therapy and $9,100 to $11,800 per QALY for medication (Lave, et al., 1998). Finally, Stevenson et al. (Stevenson, Scope, & Sutcliffe, 2010) report incremental costs per QALY of $57,300 to $103,300. The range reported for the BRIGHT intervention is substantially less than the reported range for therapy, and similar to the range reported for medication. However, BRIGHT has higher incremental costs per QALY than has been found in computer-delivered therapy; (McCrone et al., 2004) McCrone, et al (2004) for instance, report incremental costs per QALY that are approximately $2,000.
We note that the training costs are a substantial “start-up” cost. However, they are being pro-rated over only the length of the trial. In practice, these start-up costs would be pro-rated over a much longer timeframe (assuming the training effects stick), and so their contribution to the per participant cost of BRIGHT would go down over time.
The utility estimates derived either from the SF-12 or from depression-free days were similar, despite their different methodologies, which is consistent with other studies (Pyne, et al., 2007). The high cost associated with improvements in the SF-12 reflects the fact that much of the gain in the SF-12 was due to improvements in mental health, rather than physical health. At relatively modest valuations of QALYs at $35,000 or more, BRIGHT is cost-effective with a high degree of certainty (>= 90%). There are no published studies of the utilities of different states of substance use, dependence and post-treatment abstinence. Obtaining patient and general population utilities across different substances and severity levels is an important area for further research.
We used past 30-day substance use to estimate 90-day use. Prior research has shown that substance use reported in monthly intervals is relatively stable over a 3-month time period among psychiatric outpatient samples (Carey, Carey, Maisto, & Henson, 2004) (Carey, Carey, Maisto, & Hensen, 2004).
A key ingredient of cost effectiveness of the BRIGHT intervention is the successful reliance on bachelor-level counselors. It is possible that BRIGHT could be delivered using a single therapist, and if so, costs would be reduced. We used a group supervision model, with either five counselors participating (research conditions) or three counselors participating (projected). In settings that had sufficient patients to support two or more groups running simultaneously, supervision costs would be decreased accordingly.
We used a provider perspective to estimate the costs of BRIGHT, because in this context it is the provider that decides whether to provide the intervention. In addition, most prior cost-effectiveness studies take the provider perspective, which will make our results more comparable to the existing cost-effectiveness literature (Neumann, 2009).
Despite its cost-effectiveness, substance use treatment programs may be reluctant to adopt BRIGHT as it increases per patient costs, and funding for substance use treatment traditionally has been low compared to other conditions. However, health care reform, with its expanded insurance coverage and parity in benefits, should increase overall funding for substance use services (Buck, 2011). It is also likely to shift care toward more integrated models. These changes would help to promote dissemination of cost-effective models such as BRIGHT. While BRIGHT has not been tested in outpatient substance abuse treatment or primary care settings, costs should be comparable, as the wages for outpatient and residential substance use counselors are similar (Bureau of Labor Statistics). Future research should test the effectiveness of delivering BRIGHT in outpatient and primary care settings.
ACKNOWLEDGMENT
We would like to acknowledge the contributions of Suzanne Wenzel (RAND Corporation and University of Southern California School of Social Work), Stephanie Woo (Pepperdine University), and Ricardo Muñoz (University of California San Francisco, San Francisco General Hospital, San Francisco State University).
We would also like to acknowledge Jim Gilmore and Shirley Summers (Behavioral Health Services) and Behavioral Health Services outpatient counselors Conswaila Jackson, Elizabeth Macias, Sabrina Navarette, James B. Thompson, and Pamela Webber-Sandres.
Grant support: This research was funded by 1R01AA014699-01A2.
Clinical Trials Registration: This study is registered at: www.clinicaltrials.gov, Clinical Trials Identifier: NCT01191788.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this paper were previously presented at Watkins, K.E., Cuellar, A., Hunter, S.B., Hepner, K.A., Paddock, S., Solomon, J. (2011, July). The cost-effectiveness of group CBT for patients with depression and substance use disorders. Presented at 21st NIMH Conference on Mental Health Services Research, Washington, DC.
Conflict of interest declaration “NONE”. All authors report no financial relationships with commercial interests or with alcohol, tobacco, pharmaceutical or gaming industries.
Contributor Information
Katherine E. Watkins, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401, USA
Alison E. Cuellar, George Mason University, 4400 University Drive, Fairfax, VA 22030, USA
Kimberly A. Hepner, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401, USA
Sarah B. Hunter, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401, USA
Susan M. Paddock, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401, USA
Brett A. Ewing, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401, USA
Erin de la Cruz, University of Washington, 1019 N. 36th Street, Apartment B, Seattle, WA 98103, USA
References
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. Journal of Personality Assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Brazier John E., Roberts Jennifer. The estimation of a preference-based measure of health from the SF-12. Medical Care. 2004;42:851–859. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- Brown J, Kranzler HR, Del Boca FK. Self-reports by alcohol and drug abuse inpatients: factors affecting reliability and validity. British Journal of Addiction to Alcohol and Other Drugs. 1992;87(7):1013–1024. doi: 10.1111/j.1360-0443.1992.tb03118.x. [DOI] [PubMed] [Google Scholar]
- Buck JA. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs. 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. doi: 30/8/1402 [pii] 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Building Recovery by Improving Goals, Habits, & Thoughts. 2011 10/26/2011). from http://www.rand.org/health/projects/bright.html.
- Bureau of Labor Statistics Occupational Employment and Wages, May 2010, 21-1011 Substance Abuse and Behavioral Disorder Counselors, Industry profile for this occupation. 2011 May 17; from http://www.bls.gov/oes/current/oes211011.htm#ind.
- Carey KB, Carey MP, Maisto SA, Henson JM. Temporal stability of the timeline followback interview for alcohol and drug use with psychiatric outpatients. Journal of Studies on Alcohol. 2004;65(6):774–781. doi: 10.15288/jsa.2004.65.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chouinard G, Albright PS. Economic and health state utility determinations for schizophrenic patients treated with risperidone or haloperidol. Journal of Clinical Psychopharmacology. 1997;17(4):298–307. doi: 10.1097/00004714-199708000-00010. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Gold Marthe R., Siegel Joanna E., Russell Louise B., Weinstein Milton C., editors. Cost effectiveness in health and medicine. Oxford University Press; New York, NY: 1996. [Google Scholar]
- Gonzalez HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: Too little for too few. Archives of General Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Russo J, Sherbourne C, Stein MB, Craske M, Fan MY, Roy-Byrne P. Incremental cost-effectiveness of a collaborative care intervention for panic disorder. Psychological Medicine. 2006;36(3):353–363. doi: 10.1017/S0033291705006896. doi: 10.1017/s0033291705006896. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Mechanisms of behavior change in alcoholics anonymous: does Alcoholics Anonymous lead to better alcohol use outcomes by reducing depression symptoms? Addiction. 2010;105(4):626–636. doi: 10.1111/j.1360-0443.2009.02820.x. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lave JR, Frank RG, Schulberg HC, Kamlet MS. Cost-effectiveness of treatments for major depression in primary care practice. Archives of General Psychiatry. 1998;55(7):645–651. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- Lenert LA, Sherbourne CD, Sugar C, Wells KB. Estimation of utilities for the effects of depression from the SF-12. Med Care. 2000;38(7):763–770. doi: 10.1097/00005650-200007000-00008. [DOI] [PubMed] [Google Scholar]
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Economics. 2005;14(5):487–496. doi: 10.1002/hec.944. doi: 10.1002/hec.944. [DOI] [PubMed] [Google Scholar]
- Mann R, Gilbody S, Richards D. Putting the ‘Q’ in depression QALYs: A comparison of utility measurement using EQ-5D and SF-6D health related quality of life measures. Social Psychiatry and Psychiatric Epidemiology. 2009;44(7):569–578. doi: 10.1007/s00127-008-0463-5. doi: 10.1007/s00127-008-0463-5. [DOI] [PubMed] [Google Scholar]
- Mathers Colin D., Loncar Dejan. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, Shapiro DA, Tylee A. Cost-effectiveness of computerised cognitive-behavioural therapy for anxiety and depression in primary care: randomised controlled trial. The British Journal of Psychiatry. 2004;185:55–62. doi: 10.1192/bjp.185.1.55. [DOI] [PubMed] [Google Scholar]
- Neumann PJ. Costing and perspective in published cost-effectiveness analysis. Medical Care. 2009;47(7 Suppl 1):S28–32. doi: 10.1097/MLR.0b013e31819bc09d. doi: 10.1097/MLR.0b013e31819bc09d. [DOI] [PubMed] [Google Scholar]
- Paddock S, Savitsky TD. Bayesian Hierarchical Semiparametric Modeling of Longitudinal Post-Treatment Outcomes from Open-Enrollment Therapy Groups. Journal of the Royal Statistical Society, Series A: Statistics in Society. 2013;176(3) doi: 10.1111/j.1467-985X.2012.12002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act H.R. 3590, Pub. L. No. 111-148, 124 Stat. Mar 23, 2010.
- Pickard AS, Wang Z, Walton SM, Lee TA. Are decisions using cost-utility analyses robust to choice of SF-36/SF-12 preference-based algorithm? Health and Quality of Life Outcomes. 2005;3:11. doi: 10.1186/1477-7525-3-11. doi: 1477-7525-3-11 [pii] 10.1186/1477-7525-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyne JM, Rost KM, Zhang M, Williams DK, Smith J, Fortney J. Cost-effectiveness of a primary care depression intervention. Journal of General Internal Medicine. 2003;18(6):432–441. doi: 10.1046/j.1525-1497.2003.20611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyne JM, Tripathi S, Williams DK, Fortney J. Depression-free day to utility-weighted score: Is it valid? Medical Care. 2007;45(4):357–362. doi: 10.1097/01.mlr.0000256971.81184.aa. doi: 10.1097/01.mlr.0000256971.81184.aa. [DOI] [PubMed] [Google Scholar]
- Revicki DA, Siddique J, Frank L, Chung JY, Green BL, Krupnick J, Miranda J. Cost-effectiveness of evidence-based pharmacotherapy or cognitive behavior therapy compared with community referral for major depression in predominantly low-income minority women. Archives of General Psychiatry. 2005;62(8):868–875. doi: 10.1001/archpsyc.62.8.868. doi: 10.1001/archpsyc.62.8.868. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Carmody TJ, Ibrahim HM, Trivedi MH, Biggs MM, Shores-Wilson K, Kashner TM. Comparison of self-report and clinician ratings on two inventories of depressive symptomatology. Psychiatric Services. 2006;57(6):829–837. doi: 10.1176/ps.2006.57.6.829. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. Journal of Consulting and Clinical Psychology. 1978;46(5):901–907. doi: 10.1037//0022-006x.46.5.901. [DOI] [PubMed] [Google Scholar]
- Stevenson MD, Scope A, Sutcliffe PA. The cost-effectiveness of group cognitive behavioral therapy compared with routine primary care for women with postnatal depression in the UK. Value in Health. 2010;13(5):580–584. doi: 10.1111/j.1524-4733.2010.00720.x. doi: 10.1111/j.1524-4733.2010.00720.x. [DOI] [PubMed] [Google Scholar]
- Stouthard MEA, Essink-Bot ML, Bonsel GJ, Barendregt JJ, Kramer PG, van de Water HPA, van der Maas PJ. Disability weights for diseases in the Netherlands. Erasmus University Rotterdam; Rotterdam: 1997. [Google Scholar]
- Substance Abuse and Mental Health Administration [07/19, 2012];Depression triples between the ages of 12 and 15 among adolescent girls. 2012 from http://www.samhsa.gov/data/spotlight/Spot077GirlsDepression2012.pdf.
- Wang Philip S., Lane Michael, Olfson Mark, Pincus Harold A., Wells Kenneth B., Kessler Ronald C. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Hepner KA, Paddock SM, de la Cruz E, Zhou AJ, Gilmore J. An effectiveness trial of group cognitive behavioral therapy for patients with persistent depressive symptoms in substance abuse treatment. Archives of General Psychiatry. 2011;68(6):577–584. doi: 10.1001/archgenpsychiatry.2011.53. doi: 10.1001/archgenpsychiatry.2011.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D. Validity of substance use self-reports in dually diagnosed outpatients. American Journal of Psychiatry. 1998;155(1):127–128. doi: 10.1176/ajp.155.1.127. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Villarroel NA. Dynamic association between negative affect and alcohol lapses following treatment. Journal of Consulting and Clinical Psychology. 2009;77(4):633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkin G, Dunlap L, Homsi G. The substance abuse services cost analysis program (SASCAP): A new method for estimating drug treatment services costs. Evaluation and Program Planning. 2004;27(1):35–43. [Google Scholar]
- Zimmerman M, Coryell W, Wilson S, Corenthal C. Evaluation of symptoms of major depressive disorder. Self-report vs. clinician ratings. J Nerv Ment Dis. 1986;174(3):150–153. doi: 10.1097/00005053-198603000-00004. [DOI] [PubMed] [Google Scholar]