Abstract
Objective
To test the efficacy of Counselor-Assisted Problem Solving (CAPS) versus an internet resources comparison (IRC) condition in reducing behavior problems in adolescents following traumatic brain injury (TBI).
Design
Randomized clinical trial with interviewers naïve to treatment condition.
Setting
Three large tertiary children's hospitals and two general hospitals with pediatric commitment.
Participants
132 children ages 12-17 years hospitalized during the previous 6 months for moderate to severe TBI.
Interventions
Participants in CAPS (n = 65) completed 8-12 online modules providing training in problem solving, communication skills, and self-regulation and subsequent synchronous videoconferences with a therapist. Participants in the IRC group (n = 67) received links to internet resources about pediatric TBI.
Main Outcome Measures
Child Behavior Checklist (CBCL) administered before and after completion of treatment (i.e., approximately six months after treatment initiation).
Results
Post hoc analysis of covariance (ANCOVA), controlling for pre-treatment scores, was used to examine group differences in behavior problems in the entire sample and among older (n=59) and younger adolescents (n=53). Among older but not younger adolescents, CAPS resulted in greater improvements on multiple dimensions of externalizing behavior problems than did IRC.
Conclusion
Online problem-solving therapy may be effective in reducing behavior problems in older adolescent survivors of moderate-severe TBI.
Keywords: traumatic brain injury, telehealth, adolescent, problem solving, behavior
Introduction
The Effects of TBI on Children and Families
Traumatic brain injury (TBI) is the most common cause of acquired disability in childhood and a source of significant morbidity and family burden 1. Emerging or intensifying behavior problems are among the most common and problematic consequences, with 1/3 to 3/4 of children with severe TBI experiencing clinically significant behavioral symptoms during the initial year post injury 2. Secondary ADHD and difficulties with emotion control and self-regulation are particularly common and troublesome 3placing children at risk for re-injury as well as social and legal difficulties4.
Evidence-based Approaches to Treatment
Problem-solving therapy may provide an evidence-based approach for improving the behavioral outcomes of pediatric survivors of TBI. Problem-solving therapy involves a structured approach to developing a realistic and optimistic framework for addressing problems. According to cognitive-behavioral theory, “problem solving is an important general coping process that increases adaptive situational coping and behavioral competence, which in turn reduces and prevents the negative effects of stress on psychological-physical well-being” 5. Training in problem-solving skills has been shown to be effective in reducing stress, negative affect, and depressive symptomatology in a wide range of clinical populations 6,7,8,9. Clinical observation and mounting research evidence suggest that young individuals with TBI exhibit specific deficits in problem-solving skills 10,11and that these deficits contribute to interpersonal, vocational, and behavioral problems. Thus, problem-solving therapy may also provide a key metacognitive strategy enabling children with TBI to function more effectively. Problem-solving therapy has been used with caregivers of adults with TBI 12, 13 and has been increasingly used in family-centered treatments for children and youth with TBI 14.
Two previous RCTs have investigated the efficacy of family problem-solving therapy in reducing behavior problems following pediatric TBI and provide preliminary evidence of its efficacy. Wade, Brown, and Michaud 15 compared the impact of family problem-solving therapy to standard psychosocial care in a cohort of 32 children ages 5 to 17 years with moderate to severe TBI. They found significant reductions in internalizing symptoms and anxiety/withdrawal in the treatment group relative to the controls, but no differences in externalizing symptoms. A second study by the same investigative team 16 examined the efficacy of an online-version of the family problem-solving treatment which integrated psycho-educational web modules with synchronous videoconferencing to apply the problem-solving process to problems identified by the family. The efficacy of online family problem-solving was examined relative to access to internet resources in a randomized clinical trial with 40 families of children ages 5 to 17 years with moderate to severe TBI. Greater improvements in social competence were revealed in older children and improvements in child externalizing behaviors were shown in children from lower income families. The improvements refer to the respective groups as they are listed in the sentence.
Although these studies provided preliminary support for the efficacy of family problem-solving intervention in reducing child behavior problems following TBI, they were limited by relatively small, heterogeneous samples. Further research with larger, more homogeneous samples with respect to age and time since injury is needed to clearly demonstrate its utility for the population and to identify the children for whom it is likely to be most beneficial.
Adolescence constitutes a critical period for neural, social, and emotional development. It is also one of the peak developmental periods for TBI 17. Adolescents with TBI must negotiate a number of normative developmental transitions such as navigating multiple classrooms and subjects, learning to drive, dating, and advancing to employment or higher education after high school. Teens with TBI often face these challenges in the context of impaired self-regulation, judgment, and problem-solving, thereby reducing their likelihood of a successful transition to adulthood. Thus, interventions designed to facilitate self-regulation and problem-solving post TBI may be particularly beneficial in this age group.
We examined the efficacy of online family problem-solving supported by synchronous sessions with a licensed psychologist (Counselor-Assisted Problem Solving; CAPS) compared to access to internet resources (Internet Resource Comparison; IRC) in reducing the behavioral consequences of TBI in adolescents. This study expands upon previous work 18 by examining this question in a large, homogeneous sample with respect to age and time since injury. Given previous findings that older teens were more likely to benefit from online problem-solving, we hypothesized that youth who were in high school at the time of treatment would experience greater reductions in behavior problems following CAPS, whereas improvements would be less pronounced among young teens.
Method
Participants
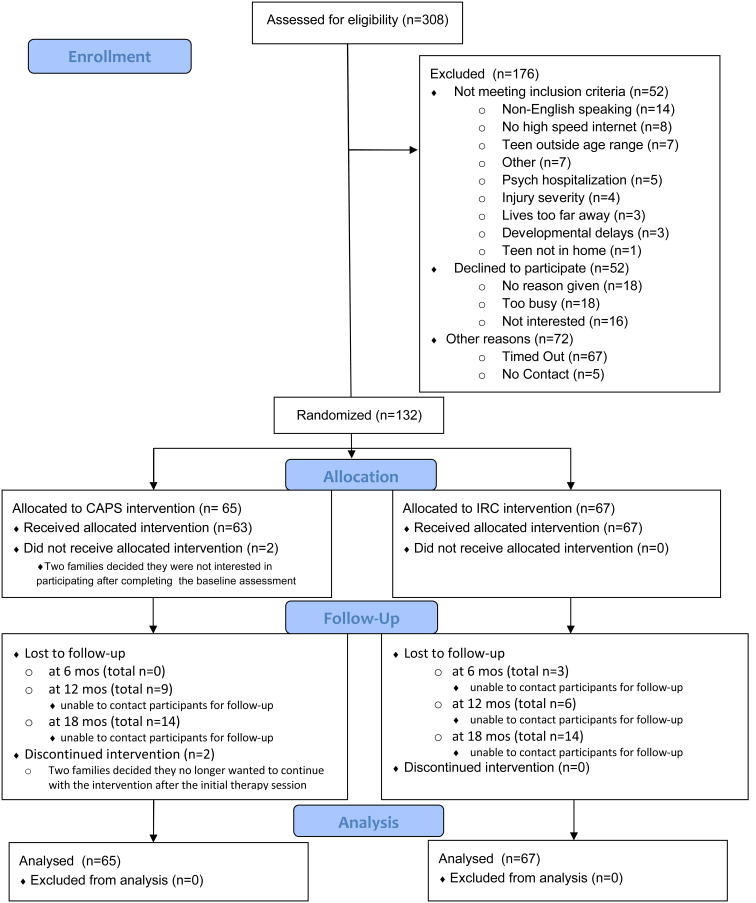
This clinical trial was registered with clinicaltrials.gov, assigned identifier: NCT00409448. Potential participants were identified from five major trauma-centers in the Central and Western regions of the United States. The study was approved by the Institutional Review Board of each participating medical center. Potential study participants were 12-17 year old adolescents who had been hospitalized overnight or longer for a complicated mild to severe TBI within the previous 1-6 months. Complicated mild TBI was defined as a lowest recorded Glasgow Coma Scale (GCS) score greater than 12 with evidence of a neurologic insult on magnetic resonance imaging or computerized tomography, moderate TBI as GCS score of 9-12, and severe TBI defined as GCS score of 8 or less. Eligibility requirements included documented alteration of neurological functioning as measured by a GCS score less than 13 or evidence of neurological insult as seen on magnetic resonance imaging or computerized tomography, English as the primary language spoken in the home, availability of the adolescent to participate in the intervention, and the family residence being within a 3 hour drive of the hospital. Participants were excluded for the following reasons: 1) the teen had not sufficiently recovered by 6 months post injury to participate in the intervention (e.g., was in a minimally responsive state), 2) either child or parent had experienced a psychiatric hospitalization during the year prior to the injury, 3) the family lived in an area without high speed internet access, 4) the child was residing outside the home (e.g., detention facility), or 5) the child had a diagnosis of intellectual disability prior to the injury. Seventeen percent (52/308) of those screened were ineligible for one or more of these reasons, with a primary language other than English constituting the most common reason for exclusion (see Figure 1. CONSORT Flow Chart).
Figure 1. Counselor Assisted Problem Solving (CAPS) CONSORT 2010 Flow Diagram.
Baseline Assessment and Random Assignment
After obtaining informed consent from the parents and assent from the teen, an initial baseline assessment at the family's home was completed by study personnel; at that time, the primary caregiver completed measures that assessed the functioning and behavior of the teen along with relevant demographic information. All families were provided with a new computer, web camera, and high speed internet access and shown how to log onto the study website and access the links to TBI resources on the web. A follow-up assessment was completed 6 months after baseline that included the same behavioral measures that had been completed at baseline.
Participating families were randomly assigned to one of two internet-based interventions: (1) CAPS, a 6-month web-based, family-centered intervention that focuses on problem-solving, communication, and self-regulation; (2) internet resource comparison (IRC) group that received a self-guided, information-based program. To ensure that both gender and race were balanced within each of the sites, randomization was carried out by stratifying on these two factors. The strata were nonwhite females, white females, nonwhite males, and white males within each site. A SAS program was created using permuted block sizes for each randomization. Group assignment was contained in a sealed envelope that was handed to the participants at the end of the baseline visit. In this fashion, group assignment was concealed from the research coordinators completing the baseline and follow-up assessments.
Treatment Groups
CAPS Intervention
Counselors in the CAPS program were four clinical psychologists who had been licensed an average of 3.25 years at the beginning of the study (range 0 -7). They participated in an initial, two-day training program and weekly supervision calls throughout the course of the project to maintain treatment fidelity. A detailed treatment manual (available from the first author) provided step-by-step instructions for meeting session objectives. Adherence to session objectives was verified by end-of-session checklists completed by the psychologists and participating parents.
Participants in the CAPS group had an initial face-to-face session with the psychologist in the family's home. During this 90-minute meeting, the psychologist learned about the adolescent's injury and how he/she and the family had been affected and identified goals that each family member wanted to address during the program. The psychologist also instructed the family in logging onto the CAPS website and demonstrated how to access the available treatment modules. In addition, the therapist assigned the family a Skype login and showed them how to log onto Skype for the videoconference sessions.
Each subsequent CAPS session consisted of a self-guided online portion providing didactic content regarding problem-solving skills, video clips modeling this skill, and exercises and assignments that offered the family opportunities to practice the new skill. New material was then released upon completion of each online session with the therapist which were scheduled biweekly for the first three months of the intervention for a total of six videoconference sessions. During these sessions, the therapist reviewed the online materials and practiced the problem-solving process using a problem that the family identified.
The individualized portion occurred during months four and five of the intervention. As part of the sixth online session, all participating parents completed a measure of family burden and a self-assessment of problem-solving and communication. Based on the results of the self-assessment, the therapist planned individualized sessions for the family with ongoing attention given to injury-related issues identified on the questionnaires. Up to two therapist sessions per month in months 4 and 5 were scheduled to address unresolved issues for a maximum of four individualized sessions. All families were scheduled for a final wrap-up session with the therapist in the sixth month.
Content of the core and supplemental sessions is listed in Table 1. The initial sessions on positive problem orientation and problem-solving were grounded in the problem-solving therapy model outlined by D'Zurilla and Nezu 5. Beginning in session 3, the counselor assisted the teen and family in applying the 5-step problem-solving process (Aim, Brainstorm, Choose, Do, and Evaluate) to a goal or problem identified by the family. The family's homework was to implement the agreed-upon plan during the 1-2 weeks between sessions and evaluate its success. Subsequent sessions continued to focus on collaborative family problem-solving while also providing didactic information and strategies for managing the common cognitive and behavioral consequences of TBI. Adolescents were taught a self-regulation heuristic (Stop, Monitor, Appraise, Reflect, Try) to promote inhibition and thoughtful responding. Basic communication skills were also covered in session 6 to facilitate effective family problem-solving and to address potential communication deficits in the teen with TBI. The teen with TBI and one parent or caregiver were required to participate in each core session, and both parents and school-age siblings, when present in the home, were also encouraged to participate when possible.
Table 1. CAPS Core and Supplemental Sessions.
| CAPS Core Sessions: |
|
|
| 1—Getting Started |
| Implementation & Monitoring |
| Goals |
| 2—Staying Positive |
| 3—Problem Solving |
| 4—Getting Organized & Working with the School |
| 5—Self-Management |
| 6—Verbal and Non-Verbal Communication |
| 7—Controlling Your Behavior II/Handling Crises |
| Self-Assessment of Skills |
| Identification of Supplemental Sessions |
| 8—Planning for the Future |
| Supplemental Sessions (up to four per family between session 7 and 8) |
|
|
| Talking with Your Teen |
| Taking Care of You/Marital Communication/Guilt, Grief, and Caregiver |
| Social Skills |
| After High School |
| Sibling Issues |
| Pain Management |
| Sleep Session |
| Memory Session |
IRC Intervention
Families in the IRC group also received a computer, web camera, and high speed internet access. (The web camera was provided to keep the research assistants unaware of group assignment.) IRC families were given access to a home page with links to online resources but were not able to access specific session content. Resources included links to local, state, and national brain-injury associations and to sites specific to pediatric brain injury, such as the Center on Brain Injury Research and Training, Brain Injury Partners and the National Database of Educational Resources on Traumatic Brain Injury. These websites provided didactic information about brain injury as well as modules about working with schools and family advocacy 19, handling stress, and problem-solving around common issues. Families were encouraged to spend at least an hour each week accessing information regarding pediatric brain injury on the web throughout the 6-month intervention period and to track the sites that they visited. At follow-up, parents provided information about the TBI-related websites visited and the time spent at each site.
Follow-up Assessment
Follow-up assessments were scheduled an average of 6 months after the baseline assessment and included re-administration of the measures completed at baseline. To equate the time between baseline and follow-up assessments between groups and to maintain concealment of group assignment, follow-ups were scheduled without knowledge of whether the participant had completed the treatment protocol or not.
Measures
Background Questionnaire
Information regarding injury severity was collected from relevant hospital records. Socio-demographic information, including median family income and primary caregiver educational attainment, was collected from the caregiver at the baseline assessment. Parents/primary caregivers completed a baseline interview regarding pre-injury diagnoses and treatments as well as current behavioral and medical treatments.
Behavioral Outcomes
Both parents were asked to complete the Child Behavior Checklist (CBCL) 20, a parental report that focuses on problematic behaviors in day-to-day family, social, and school situations. The CBCL has high test-retest reliability and criterion validity and is sensitive to behavioral problems commonly found following TBI 21. In addition, the CBCL was recommended by the Pediatric TBI Common Data Elements workgroup as a core measure of behavior problems following TBI 22. The CBCL provides Internalizing, Externalizing, and Total Behavior Problem composites as well as a number of subscales. The CAPS intervention emphasizes problem-solving skills and self-regulation. Thus, in addition to the Internalizing and Externalizing composites, we chose to examine the following subscales that were hypothesized to be affected by inhibition and self-regulation: Attention and Aggression and the subscales corresponding to related DSM diagnoses (DSM: ADHD, DSM: Conduct Disorder). Composites and subscales are reported as T-scores with a mean of 50 and a standard deviation of 10, with higher scores indicating more significant behavior problems. T scores of 65 or greater are considered to be clinically significant.
Analyses
T-tests and Fisher's exact tests were used to compare the groups (CAPS versus IRC) on baseline demographic, injury, and behavioral characteristics. Similar analyses were conducted to examine baseline differences between those who completed the study and those who dropped out. Overall group differences were sought using analysis of covariance, in which the baseline score on the measure of interest served as a covariate, thereby allowing us to assess residualized change over time. Partial eta squared was used to determine effect size from the ANCOVA. Cohen's23 conversion table for partial eta squared identifies values of 0.01, 0.06, and 0.14 as indicating small, medium, and large effect sizes, respectively. Post hoc paired t-tests were conducted to examine the magnitude of effects in each group. Effect sizes for the post hoc tests were computed using Cohen's d. All analysis was conducted using SPSS version 20.
Results
Participants
As detailed in the CONSORT Flow chart (Figure 1), 308 children were screened for eligibility; 256 met eligibility criteria and were invited to participate. Of these, 132 children (52%) completed the informed consent process and baseline assessment. Sixty-five were assigned to CAPS and sixty-seven to IRC. As indicated in Table 2, the groups were well matched with respect to demographic and injury characteristics. The groups did not differ significantly on behavior problems at baseline with the exception of internalizing symptoms which were significantly higher in the IRC than in the CAPS group. Given the rigorous randomization procedure, initial differences in internalizing symptoms are unlikely to reflect systematic bias. Further comparison of group differences (CAPS versus IRC) among older (9th-12th grade) and younger (6th-8th grade) participants revealed no significant differences in demographic (age, gender, family income) or injury characteristics (severity, time since injury) between the groups; all ps < .10.
Table 2. Most Frequently Visited Websites in the Internet-Resource Comparison Group (> 20 Unique Visitors).
| Website | Number of Participants Who Visited the Site |
|---|---|
|
|
|
| TBI Resource Center | 52 |
| http://www.braininjuryresources.org/ | |
| TBI Survival Guide | 47 |
| http://www.tbiguide.com/ | |
| Brain Injury Association of America | 45 |
| http://www.biausa.org | |
| Head Injury | 43 |
| http://www.headinjury.com | |
| Traumatic Brain Injury.com | 33 |
| http://www.traumaticbraininjury.com/ | |
| TBI Info | 30 |
| http://www.tbiinfo.com | |
| Brain Injury Resource Foundation | 23 |
| http://www.birf.info/home/links/caregivers.html | |
| International Brain Injury Association | 22 |
| http://www.internationalbrain.org | |
| Ohio Brain Injury Association | 22 |
| http://www.biaoh.org | |
| TBI Recovery Center | 22 |
| http://www.tbirecoverycenter.org |
Three participants provided consent but failed to complete the CBCL at baseline, and an additional 11 participants failed to complete the CBCL at the 6-month follow-up assessment for an attrition rate of 8%. Those who failed to complete the 6-month follow-up did not differ significantly from those who completed follow-up on child age, race/ethnicity, gender, grade, time since injury, injury severity, or baseline levels of behavior problems (all ps > .10). There was a nonsignificant trend (p < .10) for parents who did not complete the follow-up assessment to be younger than those who did [mean age (SD) = 38.82 (6.82) for dropouts and 42.87 (6.83) for completers]. Follow-up assessments were conducted an average of 6.96 and 6.74 months following baseline in the CAPS and IRC groups, respectively.
Time spent on the web viewing information regarding TBI did not differ by group. Forty-three percent of parents in the CAPS group and 48% in the IRC group reported spending fewer than 30 minutes per week viewing information about TBI (either the CAPS website or other links), and 50% of the CAPS group and 47% of the IRC group reported spending between 30 minutes and 2 hours per week. The distribution of time that adolescents reported spending at TBI websites was similar to that of their parents, with 43% of CAPS teens and 48% of IRC teens spending fewer than 30 minutes per week at TBI websites. Table 3 lists the websites visited by more than 20 participants in the IRC group (out of more than 175) and the number of participating family members who reported visiting each site.
Table 3. Improvements from Baseline to Follow-up in Child Behavior Problems in the CAPS versus IRC Treatments based on Grade Level (High School versus Middle School).
| Entire Sample | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| CAPS (57) | IRC (61) | |||||
| Behavior | Baseline | 6 Month | Baseline | 6 Month | F (df= 118) | Partial Eta-Square |
| Externalizing | 51.89 (10.13) | 49.82 (11.53) | 53.46 (10.54) | 52.69 (11.28) | 1.22 | 0.01 |
| Internalizing | 51.39 (11.28) | 49.37 (12.13) | 55.62 (11.56) | 52.56 (11.60) | 0 | 0 |
| Aggressive | 55.60 (6.39) | 54.86 (8.45) | 56.00 (8.01) | 56.16 (8.78) | 0.73 | 0.01 |
| Attention | 57.00 (7.08) | 56.32 (6.79) | 59.49 (7.85) | 60.00 (10.18) | 2.14 | 0.02 |
| ADHD | 56.61 (6.98) | 55.98 (7.47) | 58.36 (7.41) | 58.51 (8.75) | 1.11 | 0.01 |
| Conduct | 55.14 (5.90) | 54.68 (7.57) | 56.21 (8.29) | 56.59 (7.66) | 1.27 | 0.01 |
|
| ||||||
| Older Teens (9th-12thgrade) | ||||||
|
|
||||||
| CAPS (27) | IRC (35) | |||||
| Behavior | Baseline | 6 Month | Baseline | 6 Month | F = (df 118) | Partial Eta-Square |
|
| ||||||
| Externalizing | 52.92 (11.66) | 47.85 (10.60) | 54.33 (9.42) | 53.85 (9.63) | 6.75 * | 0.10 |
| Internalizing | 54.31 (11.51) | 49.54 (12.08) | 55.27 (10.38) | 52.06 (9.32) | 0.88 | 0.01 |
| Aggressive | 56.54 (6.65) | 53.04 (5.83) | 55.79 (5.73) | 55.67 (5.50) | 5.74 * | 0.09 |
| Attention | 59.46 (9.25) | 55.81 (6.91) | 59.91 (8.29) | 60.12 (9.43) | 4.73 * | 0.07 |
| ADHD | 58.46 (8.05) | 55.38 (7.65) | 58.33 (7.47) | 58.45 (8.20) | 4.38 * | 0.07 |
| Conduct | 55.96 (6.43) | 53.65 (6.12) | 56.36 (6.39) | 56.85 (6.96) | 4.80 * | 0.08 |
|
| ||||||
| Younger Teen s (6-8th grade) | ||||||
|
|
||||||
| CAPS (30) | IRC (26) | |||||
| Behavior | Baseline | 6 Month | Baseline | 6 Month | F (df= 118) | Partial Eta-Square |
|
| ||||||
| Externalizing | 52.14 (9.02) | 52.72 (11.83) | 54.12 (12.87) | 53.56 (14.31) | 0.72 | 0.01 |
| Internalizing | 50.31 (10.37) | 49.90 (12.53) | 55.76 (13.44) | 53.68 (14.06) | 0.66 | 0.01 |
| Aggressive | 55.34 (6.37) | 56.86 (10.16) | 57.80 (10.86) | 58.96 (12.44) | 0.22 | 0.00 |
| Attention | 55.97 (6.46) | 57.03 (6.85) | 59.36 (7.32) | 61.20 (7.46) | 0.24 | 0.00 |
| ADHD | 55.48 (5.91) | 56.72 (7.50) | 58.92 (7.42) | 60.28 (9.91) | 0 | 0 |
| Conduct | 54.83 (5.75) | 56.03 (8.72) | 57.64 (10.97) | 58.12 (9.51) | 0.3 | 0.01 |
indicates p < .05
Participants in the CAPS group completed an average of 8 sessions (range 0 – 13) with all but 7 (12%) completing 5 or more sessions. Overall, nearly all participants in both groups rated the website content as moderately to extremely helpful, and this did not differ by group (93% CAPS, 96% IRC). Participants in CAPS rated the videoconferences as easy to use overall (96%) and when compared to a phone call (94%) or face to face visit (90%) (AUTHORS: Are the last 2 figures supposed to be comparisons of video vs. phone and video vs. in-person? If so, “easy” should be “easier” for those comparisons – although the differences look trivial.). In addition, 96% rated the videoconferences as helpful overall, with 85% rating them as very or extremely helpful.
Analyses of covariance, controlling for baseline symptom levels on the CBCL, were conducted to test the hypothesis that CAPS was associated with greater improvements in behavior problems than was access to internet resources (IRC). Eighty-six percent of primary caregivers (104/121) were mothers, 10% were fathers (12/121) and 4% (5/121) were grandparents or other relations, and this did not differ by group. Two sets of analyses were conducted--one examining group differences in the sample as a whole and one examining group differences between participants in high school (n = 58) and those in middle school (n = 53) separately. The latter analyses were conducted given theoretical and empirical expectations that the effects of the CAPS intervention on self-regulation might be greater among older adolescents 15, 16, 18. As reported in Table 4, there were no significant differences between the CAPS and IRC groups on any of the behavioral outcomes in the sample as a whole.
Table 4. Comparison of CAPS Utilization, Adherence and Satisfaction Data for Middle School and High School Participants.
| Middle School | High School | t(60) | |
|---|---|---|---|
|
|
|
|
|
| Sessions @ 6 Months | 7.76 (3.05) | 6.54 (2.94) | 1.61 |
| Total Sessions Completed | 8.44 (2.79) | 7.74 (2.93) | .95 |
| Total Hours on Website | 11.58 (5.66) | 7.37 (4.53) | 2.12* |
| Sessions with Mother Only | 4.36 (4.32) | 5.35 (3.80) | -.84 |
| Sessions with Father Only | 1.32 (2.90) | 1.04 (2.46) | .36 |
| Sessions with Both Parents | 3.24 (4.31) | 2.17 (3.70) | .92 |
| Cancellations/No Shows | 4.18 (4.72) | 3.19 (3.60) | .95 |
| Helpfulness Ratings (1 = not at all to 5 = extremely) | |||
|
|
|||
| Website Overall | 3.78 (1.31) | 3.65 (1.50) | .31 |
| Information on Brain Injury | 4.17 (1.03) | 3.71 (1.45) | 1.22 |
| Problem-Solving Content | 4.04 (1.30) | 3.71 (1.49) | .78 |
| Self-Management Content | 4.09 (1.31) | 3.67 (1.39) | 1.03 |
| Communication Skills | 4.26 (1.10) | 3.71 (1.42) | 1.43 |
| Anger Management Skills | 4.35 (.98) | 3.38 (1.36) | 2.72** |
| Videoconferences Overall | 4.13 (1.10) | 4.30 (1.15) | -.53 |
indicates p < .01
Among participants in high school, those receiving CAPS had significantly lower levels of externalizing symptoms, aggression, attention problems, ADHD, and Conduct Disorder symptoms than did those receiving IRC after controlling for baseline symptoms. The effect sizes for significant group differences were of medium magnitude ranging from .07 to .10 (see Table 3). The groups did not differ on internalizing symptoms at follow-up, but both reported significant reductions in internalizing symptoms from baseline to follow-up with a medium effect size. Post hoc paired t-tests were used to examine the magnitude of improvements within each group. High school age participants in CAPS improved on all six behavioral indices with improvements ranging from 1/3 to ½ standard deviation. High school age participants in IRC only evidenced improvements in internalizing symptoms with a medium size effect.
Conversely, among participants in middle school at the time of treatment (n = 54), the groups did not differ on any CBCL subscale. Furthermore, there were no improvements, as assessed by paired t-tests, on any outcomes in either group. Taken together, these findings suggest that CAPS may promote improvements in self-regulation and behavioral functioning in older but not younger adolescents.
To better understand the differential treatment effects of CAPS in younger versus older participants, we conducted a series of post hoc t-test analyses examining average time spent completing sessions online, the number of sessions completed overall and with various family constellations (mom and teen alone, dad and teen alone, all three), number of cancellations or no shows, and teen satisfaction ratings. The results, reported in Table 4, revealed only two significant differences out of 13 analyses. Within a subset of participants (n = 28) for whom time spent on the web modules was available, the middle school age participants spent significantly more time on the website overall than did the high school age participants. Also, the middle-school age participants rated the anger management content as significantly more helpful than did those in high school. Thus, the greater improvements among older teens do not appear attributable to greater family involvement, greater exposure to the treatment content online or in sessions with the psychologist, or greater satisfaction with the program.
Discussion
We report the results from one of the largest, single-blind RCTs of an intervention to improve the behavioral outcomes of pediatric TBI to date. We compared the efficacy of two web-based interventions: Counselor-Assisted Problem Solving (CAPS) and access to internet resources and education regarding TBI (IRC).This study differed from previous studies examining the efficacy of online family problem-solving following pediatric TBI in a number of key respects including greater homogeneity with respect to participant age and time since injury and concealment of group assignment from the research personnel conducting the follow-up assessments. Findings indicate that CAPS is superior to IRC in improving externalizing behavior problems including attention/ADHD, aggression, and Conduct Disorder symptoms in high-school age youth with TBI, whereas neither CAPS nor IRC was associated with improved functioning in younger adolescents. Corresponding effect sizes, as assessed using Cohen's d, were medium in magnitude. While the CAPS intervention was associated with significant improvements among older adolescents on each behavioral outcome assessed, the IRC intervention was only associated with improvements in internalizing symptoms.
Given developmental theory and previous findings 15,16,18, we anticipated that the effects of CAPS would be more pronounced among older adolescents. The CAPS intervention trains teens and their families to use heuristics to improve problem-solving and self-regulation. Developmentally, adolescents in high school are more capable of employing these strategies in their daily lives without parental supervision or intervention than are younger adolescents (ages 12 to 13 years) who are likely to require additional parental support or scaffolding to utilize these skills.
Contrary to previous findings 15, 16, 18, younger teens in this cohort did not improve, regardless of their treatment group. This subset of the sample demonstrated small, non-significant decrements on a number of the CBCL subscales including aggressive behaviors, attention problems, ADHD, and Conduct Disorder symptoms. Post hoc analyses revealed very few differences between older and younger adolescents with respect to the number of sessions completed, the extent of involvement of both parents in treatment, nonadherence, or satisfaction with the program content. However, contrary to expectations, younger participants spent significantly more time on the website and rated some website content (i.e., anger management) more favorably than did older participants. These findings suggest that the associations among treatment dose, satisfaction, and response may be complex and vary as a function of age/developmental level. Taken together, this pattern of findings provides tentative evidence that older and younger adolescents may respond differently to behavioral interventions following TBI. CAPS is a relatively brief intervention (8 core sessions) and focuses on cognitive-behavioral skills. Younger adolescents may require longer or more intensive treatment or a qualitatively different treatment protocol. For example, younger adolescents may benefit more from a parent-focused intervention that emphasizes antecedent behavior controls and setting the child up for success 24.
Given the paucity of treatment studies for pediatric TBI, little is known about the optimal timing of interventions after injury. The current project targeted youth during the initial six months following TBI, allowing us to minimize the variability attributable to time since injury and to attempt to reduce the emergence of novel behavior problems. However, it is unclear whether this is invariably the most efficacious time to intervene or whether optimal timing may vary as a function of age (early versus later adolescence) or injury severity. Anecdotally, some caregivers of youth with severe TBI indicated that it was difficult for them to participate in the intervention while they were dealing with the child's continuing medical complications such as seizures and further surgeries. In addition, youth with TBI reported difficulty attending to the session content in the initial months after TBI. Thus, additional research is needed to clarify when in the course of recovery cognitive-behavioral interventions such as CAPS may be most effective for youth with TBI.
Telehealth interventions such as CAPS reduce barriers to treatment access such as time/distance, transportation, and perceived stigma. However, adoption into clinical practice has been limited and initially confined to more geographically remote locations such as rural Western United States, central Canada, and Australia. Increasingly, large institutions, including the Veteran's Administration, have sought to incorporate telehealth practices into standard care by identifying HIPAA compliant videoconferencing software (such as Movi) and working to address institutional barriers. 25Many families now own home computers and video cameras, and if not, these devices can be purchased at increasingly competitive prices. Nonetheless, issues such as third-party payment and inconsistent guidelines governing telehealth practice by psychologists across states continue to pose significant barriers to more widespread adoption of programs such as CAPS.
Despite our relatively large and homogeneous sample, a number of limitations of this study should be noted. Although the treatment conditions were equated for access to reliable information and resources concerning TBI, including websites regarding problem-solving strategies and stress management, the groups were not equated for therapist attention. Therefore, while we can tentatively conclude that CAPS is superior to access to internet resources alone in reducing behavior problems among older adolescents following TBI, we cannot conclude that it is superior to other forms of treatment affording therapist support. Future research that controls for the nonspecific effects of therapist attention is needed to disentangle the specific effects of problem-solving therapy on behavior after TBI. Furthermore, website utilization in the IRC group was assessed solely by parental report via weekly logs of sites visited and thus may be subject to social desirability biases. Also, evaluation of behavior problems was based on parent report. Although the CBCL was recommended as a core behavioral outcome measure by the Common Data Elements workgroup22, teacher or youth self-report measures of behavior would provide additional insights into the efficacy of the intervention. Given the nature of the interventions, one involving counselor-assistance and the other self-guided access online information, it was not possible to conceal group assignment from the participating families. Thus, difference in outcome may have been attributable to parental expectations and social desirability biases as well as the effectiveness of the treatment program. Further, recruitment of a subset of participants with no behavior problems at baseline may have contributed to floor effects. Finally, the sample was disproportionately white which may limit generalizability of our findings to individuals of other races or ethnicities.
The current results support the efficacy of CAPS, and online family problem-solving more broadly, in reducing externalizing behavior problems in older adolescents with TBI. Further research is needed to determine the optimal timing of intervention and the value of family versus individual intervention. Moreover, increasing attention must be devoted to identifying effective interventions for younger adolescents who may be less likely to benefit from the cognitive-behavioral heuristics in CAPS.
Acknowledgments
The authors wish to acknowledge the contributions of Robert Blaha, Elizabeth Hagesfeld, Michelle Jacobs, Daniel Maier, and Nina Fox in data collection and entry, Amy Cassedy in data management, and John Stullenberger in website support. We would also like to acknowledge the contributions of the therapists JoAnne Carey, Psy.D., Britt Nielsen, Psy.D., and Brad Jackson, Ph.D.
Sources of Funding: This work was supported in part by 1) NIH grant R01-MH073764 from the National Institute of Mental Health; and 2) a grant from the Colorado Traumatic Brain Injury Trust Fund Research Program, Colorado Department of Human Services, Division of Vocational Rehabilitation, Traumatic Brain Injury Program.
Abbreviations
- ADHD
Attention Deficit Hyperactivity Disorder
- ANCOVA
Analysis of Covariance
- CAPS
Counselor Assisted Problem Solving
- CBCL
Child Behavior Checklist
- DSM
Diagnostic and Statistical Manual of Mental Disorders, GCS, Glasgow Coma Scale
- IRC
Internet Resources Comparison
- RCT
Randomized Control Trial
- TBI
Traumatic Brain Injury
Footnotes
Conflicts of Interest: We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (e.g., NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
This clinical trial was registered with clinicaltrials.gov, assigned identifier: NCT00409448.
Contributor Information
Shari L. Wade, Cincinnati Children's Hospital Medical Center and the University of Cincinnati College of Medicine
Terry Stancin, Case Western Reserve University, MetroHealth Medical Center, Cleveland, OH
Michael Kirkwood, Children's Hospital Colorado and University of Colorado School of Medicine, Aurora, CO
Tanya Maines Brown, Cincinnati Children's Hospital Medical Center and the University of Cincinnati College of Medicine
Mayo Clinic Rochester, Cincinnati Children's Hospital Medical Center and the University of Cincinnati College of Medicine.
Kendra M. McMullen, Cincinnati Children's Hospital Medical Center and the University of Cincinnati College of Medicine.
H. Gerry Taylor, Case Western Reserve University, Rainbow Babies & Children's Hospital, University Hospitals Case Medical Center, Cleveland, OH
References
- 1.Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008 Nov-Dec;23(6):394–400. doi: 10.1097/01.HTR.0000341435.52004.ac. [DOI] [PubMed] [Google Scholar]
- 2.Bloom DR, Levin HS, Ewing-Cobbs L, Saunders AE, Song J, Fletcher JM, Kowatch RA. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2001 May;40(5):572–9. doi: 10.1097/00004583-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Max JE, Levin HS, Landis J, Schachar R, Saunders A, Ewing-Cobbs L, Chapman SB, Dennis M. Predictors of personality change due to traumatic brain injury in children and adolescents in the first six months after injury. J Am Acad Child Adolesc Psychiatry. 2005;44(5):434–442. doi: 10.1097/01.chi.0000156280.66240.61. [DOI] [PubMed] [Google Scholar]
- 4.Williams WH, Cordan G, Mewse AJ, Tonks J, Burgess CN. Self-reported traumatic brain injury in male young offenders: a risk factor for re-offending, poor mental health and violence? Neuropsychol Rehabil. 2010 Dec;20(6):801–12. doi: 10.1080/09602011.2010.519613. [DOI] [PubMed] [Google Scholar]
- 5.D'Zurilla T, Nezu AM. Problem-Solving Therapy A Positive Approach to Clinical Intervention. New York, NY: Springer Publishing Company; 2006. [Google Scholar]
- 6.Elliott TR, Berry JW. Brief problem-solving training for family caregivers of persons with recent-onset spinal cord injuries: a randomized controlled trial. J Clin Psychol. 2009 Apr;65(4):406–22. doi: 10.1002/jclp.20527. [DOI] [PubMed] [Google Scholar]
- 7.Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of women with disabilities: a randomized clinical trial. Behav Res Ther. 2009 Jul;47(7):548–58. doi: 10.1016/j.brat.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nezu AM, Perri MG. Social problem-solving therapy for unipolar depression: an initial dismantling investigation. J Consult Clin Psychol. 1989 Jun;57(3):408–13. [PubMed] [Google Scholar]
- 9.Robin AL, Foster SL. Negotiating Parent-Adolescent Conflict: A behavioral-family systems approach. New York: Guilford Press; 1989. [Google Scholar]
- 10.Jacobs R, Anderson V. Planning and problem solving skills following focal frontal brain lesions in childhood: analysis using the Tower of London. Child Neuropsychol. 2002 Jun;8(2):93–106. doi: 10.1076/chin.8.2.93.8726. [DOI] [PubMed] [Google Scholar]
- 11.Janusz JA, Kirkwood MW, Yeates KO, Taylor HG. Social problem-solving skills in children with traumatic brain injury: long-term outcomes and prediction of social competence. Child Neuropsychol. 2002 Sep;8(3):179–94. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- 12.Kreutzer JS, Stejskal TM, Ketchum JM, Marwitz JH, Taylor LA, Menzel JC. A preliminary investigation of the brain injury family intervention: impact on family members. Brain Inj. 2009 Jun;23(6):535–47. doi: 10.1080/02699050902926291. [DOI] [PubMed] [Google Scholar]
- 13.Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of persons with traumatic brain injuries: a randomized controlled trial. Arch Phys Med Rehabil. 2008 May;89(5):931–41. doi: 10.1016/j.apmr.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gan C, Gargaro J, Kreutzer JS, Boschen KA, Wright FV. Development and preliminary evaluation of a structured family system intervention for adolescents with brain injury and their families. Brain Inj. 2010;24(4):651–63. doi: 10.3109/02699051003692142. [DOI] [PubMed] [Google Scholar]
- 15.Wade SL, Michaud L, Brown TM. Putting the pieces together: preliminary efficacy of a family problem-solving intervention for children with traumatic brain injury. J Head Trauma Rehabil. 2006 Jan-Feb;21(1):57–67. doi: 10.1097/00001199-200601000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Wade SL, Carey J, Wolfe C. The efficacy of an online cognitive-behavioral family intervention in improving child behavior and social competence following pediatric brain injury. Rehabil Psychol. 2006 Aug;51(3):179–189. [Google Scholar]
- 17.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; p. 2010. [Google Scholar]
- 18.Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following pediatric brain injury. J Consult Clin Psychol. 2006 Jun;74(3):445–54. doi: 10.1037/0022-006X.74.3.445. [DOI] [PubMed] [Google Scholar]
- 19.McLaughlin KA, Glang A, Beaver SV, Gau JM, Keen S. Web-Based Training in Family Advocacy. J Head Trauma Rehabil. 2012 Jun;8 doi: 10.1097/HTR.0b013e31824e1d43. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Achenbach TM, Rescale LA. Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 21.Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol. 2003 Jun;28(4):251–63. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- 22.McCauley SR, Wilde EA, Anderson VA, Bedell G, Beers SR, Campbell TF, Chapman SB, Ewing-Cobbs L, Gerring JP, Gioia GA, Levin HS, Michaud LJ, Prasad MR, Swaine BR, Turkstra LS, Wade SL, Yeates KO Pediatric TBI Outcomes Workgroup. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. J Neurotrauma. 2012 Mar 1;29(4):678–705. doi: 10.1089/neu.2011.1838. Epub 2011 Aug 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 24.Feeney TJ, Ylvisaker M. Context-sensitive behavioral supports for young children with TBI: short-term effects and long-term outcome. J Head Trauma Rehabil. 2003 Jan-Feb;18(1):33–51. doi: 10.1097/00001199-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Department of Veterans Affairs. Strategic Plan FY 2010-2014. 2010 Available from: http://www1.va.gov/op3/Docs/StrategicPlanning/VA_2010_2014_Strategic_Plan.pdf.