Abstract
Background
There are limited data informing the optimal treatment strategy for acute myocardial infarction in the oldest old (aged ≥85 years). The study aim was to examine whether decade-long increases in guideline-based cardiac medication use mediate declines in post-discharge mortality among oldest old patients hospitalized with acute myocardial infarction.
Methods
The study sample included 1137 patients aged ≥85 years hospitalized in 6 biennial periods between 1997 and 2007 for acute myocardial infarction at all 11 greater Worcester, Massachusetts, medical centers. We examined trends in 90-day survival after hospital discharge and guideline-based medication use (aspirin, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, beta-blockers, lipid-lowering agents) for acute myocardial infarction during hospitalization and at discharge. Sequential multivariable Cox regression models examined the relationship among guideline-based medication use, study year, and 90-day post-discharge survival rates.
Results
Patients hospitalized between 2003 and 2007 experienced higher 90-day survival rates than those hospitalized between 1997 and 2001 (69.1% vs 59.8%, P < .05). Between 1997 and 2007, the average number of guideline-based medications prescribed at discharge increased significantly (1.8 to 2.9, P < .001). The unadjusted hazard ratio for 90-day post-discharge mortality in 2003-2007 compared with 1997-2001 was 0.73 (95% confidence interval, 0.60-0.89); after adjustment for patient characteristics and guideline-based cardiac medication use, this relationship was no longer significant (hazard ratio, 1.26; 95% confidence interval, 1.00-1.58).
Conclusions
Between 1997 and 2007, 90-day survival improved among a population-based sample of patients aged ≥85 years hospitalized for acute myocardial infarction. This encouraging trend was explained by increased use of guideline-based medications.
Keywords: Acute myocardial infarction, Geriatrics, Medication effects, Post-discharge survival
Increasing attention is focusing on the treatment–risk paradox in which older adults, including the oldest old (aged ≥85 years), are at high risk of morbidity and mortality from coronary heart disease but at lower risk for appropriate treatment. 1-3 Recent studies of older adults demonstrate high mortality from acute myocardial infarction and increased risk with advancing age.4 Although several recent reports describe efforts to improve acute myocardial infarction treatment5 and changing trends in acute myocardial infarction mortality and evidence-based medical therapy use for acute myocardial infarction in US adults aged 65 years or more,6-8 few studies focus on the oldest old. This research gap is important because the oldest old is a fast-growing subsegment of the aging population, and advanced age is a significant predictor for acute myocardial infarction–related morbidity and mortality, and treatment benefits and complications.
Recent data describe increased use of guideline-based pharmacotherapy in Americans aged 65 years or more with coronary heart disease7-9 and paralleled reductions in the risk-standardized acute myocardial infarction mortality rates6,10 Whether increases in appropriate pharmacotherapy explain the observed increases in survival after acute myocardial infarction has not been well established. Studies of adults aged ≥75 years11 and non-agenearians12 hospitalized with acute myocardial infarction suggest that recent gains in post-discharge acute myocardial infarction survival exist in association with the increased use of guideline-based treatment regimens, but these studies were small and based on cross-sectional11 and case series4 designs.
The purpose of this observational study was to examine recent trends in guideline-based medication use for acute myocardial infarction and post-discharge survival rates for oldest-old adults included in the Worcester Heart Attack Study, a population-based study of patients hospitalized with acute myocardial infarction at all central Massachusetts medical centers.12-14 We focused on changes in 90-day post-discharge survival rates in the oldest-old and describe decade-long trends in the use of in-hospital and discharge medications in this population. We further examined whether decade-long changes (1997-2007) in guideline-based medication use at the time of hospital discharge may explain increases in 90-day survival after hospital discharge.
Materials and Methods
Data are from the Worcester Heart Attack Study,12-14 an ongoing population-based observational study examining changes over time in the incidence, in-hospital, and long-term case-fatality rates of residents of the Worcester, Massachusetts, metropolitan area (2000 census estimate = 478,000) hospitalized with confirmed acute myocardial infarction at all 11 greater Worcester medical centers during the 6 biennial periods (1997, 1999, 2001, 2003, 2005, 2007). Although additional earlier study years were included in this investigation, we restricted the study sample to patients hospitalized with acute myocardial infarction between 1997 and 2007 to examine decade-long trends in medication patterns, use of invasive cardiac procedures, and post-discharge all-cause mortality.
Criteria for the diagnosis of acute myocardial infarction included a clinical history of prolonged chest pain not relieved by rest or use of nitrates, serum creatine phosphokinase-MB, and troponin level elevations in excess of the upper limit of normal as specified by the laboratory at each hospital, and serial electrocardiographic tracings during hospitalization showing changes in the ST segment or Q waves typical of acute myocardial infarction. At least 2 of these 3 criteria needed to be satisfied for study inclusion. All autopsy-proven cases of acute myocardial infarction were included irrespective of the other criteria. Cases of perioperative-associated acute myocardial infarction were not included. For the different periods under study, the clinical complications of acute myocardial infarction were assessed on the basis of information available from the review of clinical charts15-18.
Data Collection
The hospital records of patients with validated acute myocardial infarction were abstracted for demographic, medical history, and clinical data by trained study clinicians. Information included patient's age, sex, medical history (eg, angina, diabetes mellitus, heart failure, hypertension, stroke), and acute myocardial infarction order (initial vs prior) and type (Q wave or non–Q wave). Information on clinically significant in-hospital complications, including atrial fibrillation,15 heart failure,16 stroke,17 and cardiogenic shock, also was collected.18 Information about the use of cardiac medications during the index hospitalization was obtained through the review of hospital medical records and physician's and nurse's progress notes. Coronary revascularization procedures examined in this study were percutaneous coronary interventions (including balloon angioplasty and bare-metal and drugeluting stents) and coronary artery bypass grafting. Survival status after hospital discharge was ascertained through a review of medical records for additional hospitalizations and statewide searches of death records for residents of the Worcester metropolitan area with patient follow-up continued through the end of 2009.
Key Variables
The key predictor variable for this analysis was the time trend between 1997 and 2007, which was dichotomized into 2 periods for ease of analysis and interpretation: 1997-2001 and 2003-2007. We constructed a 3-level variable for each guideline-based medication (aspirin, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, lipid-lowering agents, and beta-blockers) to reflect 3 prescribing possibilities for each medication within each patient: never prescribed; prescribed during hospitalization but not at discharge; and prescribed during hospitalization and at hospital discharge. The never prescribed category is conceptualized to reflect underprescribing of a potentially beneficial medication. Prescribing during hospitalization only likely reflects patient inability to tolerate the medication because of an adverse effect or drug intolerance (eg, hypotension). The third category, medications prescribed during hospitalization and at hospital discharge, is conceptualized to reflect guideline-based practice. Hospital use of coronary interventional procedures was defined as the receipt of percutaneous coronary intervention or coronary artery bypass grafting. Because we postulated that short-term acute myocardial infarction–associated mortality was influenced by different factors than long-term mortality after acute myocardial infarction, and due to problems with measurement of long-term medication adherence, the main outcome variable for this analysis was 90-day post-discharge mortality.
Data Analysis
Descriptive statistics were used to characterize the patient population hospitalized with acute myocardial infarction. We used chi-square tests of statistical significance for categoric variables and analysis of variance for continuous variables to compare the distribution of selected patient characteristics over time. We described all-cause mortality between 1997 and 2007 in 2 time periods (1997-2001 vs 2003-2007) using Kaplan-Meier survival estimates and used the log-rank test to test for significant differences in post-discharge survival between patients hospitalized during the early versus later time periods.
We used tests of trends to examine trends in acute myocardial infarction medication treatment and interventions over time.19 To examine differences in the characteristics of patients who received guideline-based medication treatment and interventional procedures over time compared with those who did not, we used the chi-square test and Fisher exact test to examine the relationship between each patient characteristic and receipt of each of the acute myocardial infarction treatment variables (discharge medications and intervention procedures) in 2003-2007 compared with 1997-2001.
We developed a series of multivariable adjusted Cox regression models to examine the effect of guideline-based medications on temporal trends in 90-day mortality rates. The initial unadjusted model evaluated temporal trends in 90-day postdischarge mortality in the early (1997-2001) versus later patient cohorts (2003-2007). Model 2 adjusted for patient-level confounders, including comorbidities (history of heart failure, angina) and the predicted probability of 90-day mortality risk based on an adaptation of the model by Krumholz et al20 (including age, sex, diabetes mellitus, stroke, history of myocardial infarction, hypertension, chronic obstructive pulmonary disease, history of coronary artery bypass grafting or angioplasty, hypotension in the first 48 hours of hospitalization, hospital development of cardiogenic shock or heart failure, initial blood urea nitrogen, initial serum creatinine, initial white blood cell count, and initial electrocardiogram findings [left bundle branch block, right bundle branch block, and ST-segment elevation]). Model 3 also adjusted for the receipt of guideline-based medication use with medications prescribed during hospitalization and at hospital discharge included in the analytic models as the reference category to allow estimation of the increased hazard of death associated with never being prescribed a guideline-based medication or being prescribed a medication only during hospitalization relative to guideline-based practice. A final regression model also adjusted for the receipt of coronary interventional procedures. Sensitivity analysis included an additional multivariable model that adjusted for nonguideline-based medications (ie, medications that should have little to do with post-discharge mortality) to illustrate whether medication-mediated effects on observed survival trends reflected healthy user bias or intrinsic medication effects. For example, if inclusion of medications such as diuretics demonstrates mediating effects on observed survival trends similar to a guideline-based medication, there would be evidence that the medication prescribing practices were a marker of patient health rather than protective medication effects. All analyses were performed using SAS version 9 (SAS Institute Inc, Cary, NC) and STATA/SE 10.1 (StataCorp, College Station, Tex).
Results
Characteristics of the Oldest Old Hospitalized With Acute Myocardial Infarction
Our final study sample consisted of 1137 patients, including 527 patients hospitalized between 1997 and 2001 and 610 patients hospitalized between 2003 and 2007 (Table 1). The ages of this population ranged from 85 to 105 years, with an average age of 89.1 years (1997-2001) and 88.7 years (2003-2007), respectively. Notable differences in patient characteristics between the 2 time periods (1997-2001 vs 2003-2007) included the proportion of patients admitted with a history of angina (25.6% vs 19.5%, respectively), hypertension (71.4% vs 80.7%, respectively), and hyperlipidemia (20.1% vs 43.6%, respectively) (all P < .05).
Table 1. Characteristics of Oldest Old Patients Hospitalized with Acute Myocardial Infarction Over Time (1997-2007).
| Characteristic | 1997-2001 (n = 527) | 2003-2007 (n = 610) | P |
|---|---|---|---|
| Age, % | |||
| 85-89 y | 320 (60.7) | 350 (57.4) | <.001 |
| 90-94 y | 159 (30.2) | 122 (20.0) | |
| ≥95 y | 48 (9.1) | 138 (22.6) | |
| Female | 340 (64.5) | 390 (63.9) | .84 |
| Medical history, % | |||
| Angina pectoris | 135 (25.6) | 119 (19.5) | .01 |
| Diabetes mellitus | 125 (23.7) | 162 (26.6) | .27 |
| Hypertension | 376 (71.4) | 492 (80.7) | <.001 |
| Heart failure | 219 (41.6) | 244 (40.0) | .60 |
| Stroke | 78 (14.8) | 84 (13.8) | .62 |
| Hyperlipidemia | 106 (20.1) | 266 (43.6) | <.001 |
| AMI characteristics, % | |||
| Initial MI | 308 (58.4) | 360 (59.0) | .85 |
| Q-wave | 97 (18.4) | 87 (14.6) | .09 |
| Hospital length of stay, d Mean (SD) | 5.6 (4.1) | 5.5 (6.3) | .82 |
AMI = acute myocardial infarction; MI = myocardial infarction; SD = standard deviation.
Crude Survival Trends
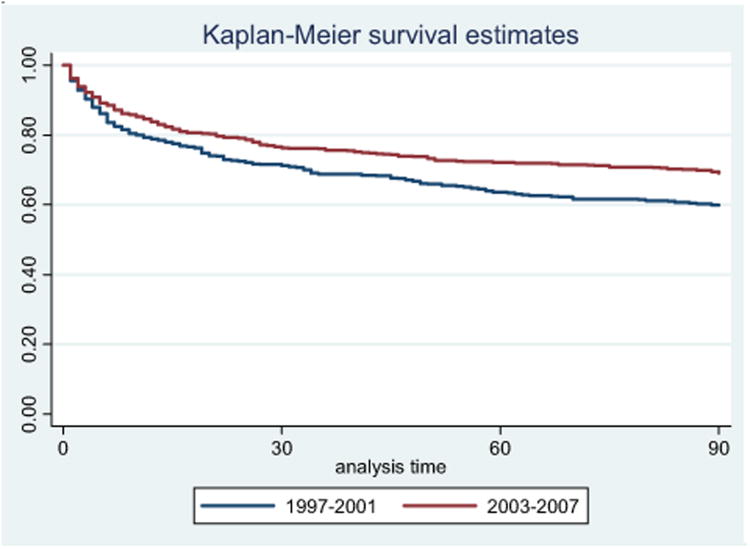
Patients hospitalized between 2003 and 2007 experienced significantly higher survival (69.1%; 95% confidence interval [CI], 65.3-72.7) during the 90-day period after hospital discharge than those hospitalized between 1997 and 2001 (59.8%; 95% CI, 55.5-63.9) (Figure 1, P < .05).
Figure 1.
Crude survival rates in patients hospitalized with acute myocardial infarction according to time period.
Time Trends in Acute Myocardial Infarction Medication Treatment
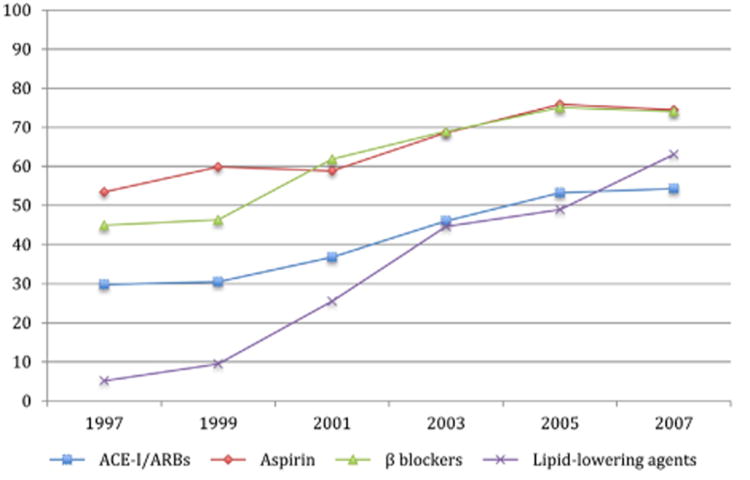
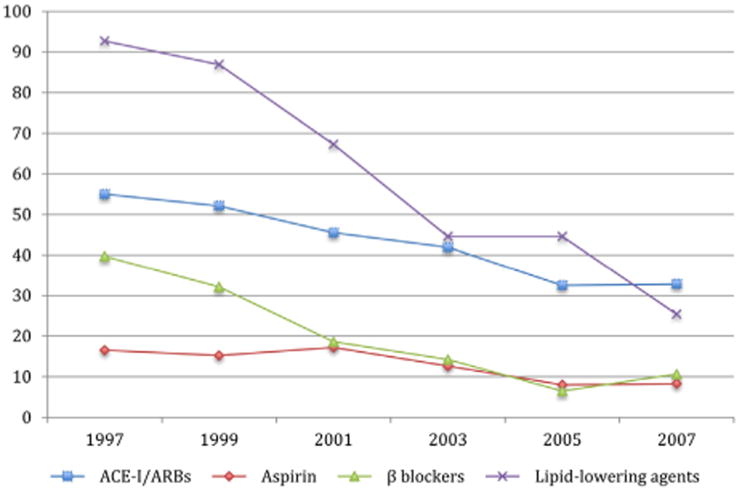
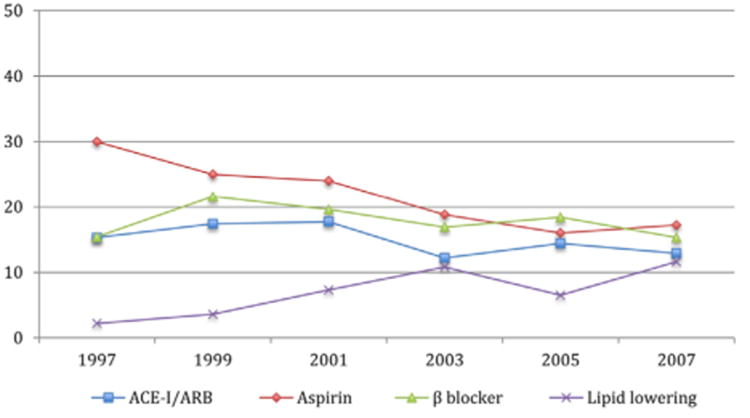
Between 1997 and 2007, the average number of guideline-based cardiac medications administered during hospitalization for acute myocardial infarction increased significantly from 2.3 to 3.4, and the average number prescribed at discharge increased from 1.8 to 2.9 (both P < .001). There were increases over time in all of the guideline-based medications (aspirin, beta-blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and lipid-lowering agents) during hospitalization and at hospital discharge (Figure 2, all P < .05). Corresponding trends for medications never prescribed also were observed (Figure 3). The proportion of patients who used aspirin during hospitalization only without continuation at discharge declined over time from 30.0% to 17.2% (P < .05) (Figure 4).
Figure 2.
Guideline-based medication used in hospital and at discharge in patients aged 85 years or more between 1997 and 2007. ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker.
Figure 3.
Guideline-based medications never prescribed in patients aged 85 years or more between 1997 and 2007. ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker.
Figure 4.
Guideline-based medications in hospital only in patients aged 85 years or more between 1997 and 2007. ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker.
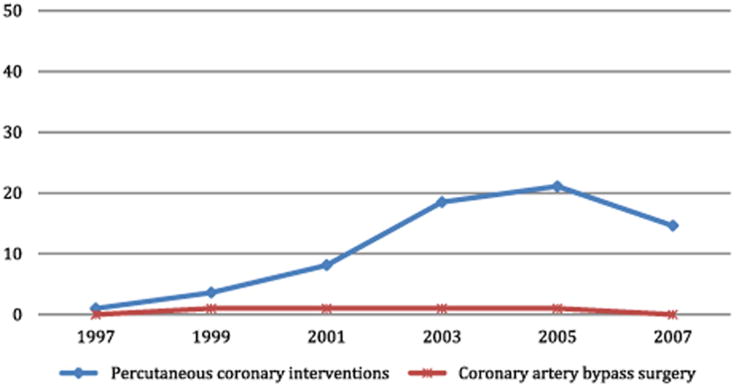
Time Trends in Acute Myocardial Infarction Procedural Interventions and Thrombolytics
The proportion of older patients receiving a percutaneous coronary intervention during hospitalization increased from <1% in 1997 to 14.6% by 2007 (P < .001), whereas coronary artery bypass grafting during the patient's index hospitalization remained essentially unused in this population throughout the entire time period examined (<1%). Thrombolytic use declined from 10.3% in 1997 to 0% in 2007 (P < .001) (Figure 5).
Figure 5.
Interventional procedures in patients aged 85 years or more between 1997 and 2007.
Effect of Cardiac Medication and Interventional Treatment Practices on 90-Day Survival Rates
We examined the possible mediating effect of guideline-based medications on 90-day survival using sequential regression models (Table 2). In model 1, unadjusted 90-day mortality was significantly lower in 2003-2007 compared with 1997-2001 for the oldest old (hazard ratio [HR], 0.73). Model 2 controlled for patient characteristics (comorbidities and predicted probability of 90-day acute myocardial infarction mortality risk) with similar mortality trends. Model 3 showed a loss of significant mortality effects in later years after additional adjustment for the 4 guideline-based medications, with a reversal of the direction of the year effect and lack of statistical significance (adjusted HR, 1.26; 95% CI, 1.00-1.58). In this model, patients who were prescribed each of the medications in the hospital only or not at all were at significantly higher mortality risk relative to patients who were prescribed guideline-based medications at discharge. Model 4 also adjusted for the receipt of coronary artery bypass grafting or percutaneous coronary interventions during hospitalization and shows a year effect (adjusted HR, 1.28; 95% CI, 1.02-1.62) similar to the result from the medication-adjusted model (model 3). In a sensitivity analysis, inclusion of diuretics into the regression model, in lieu of the guideline-based cardiac medications, resulted in little effect of the year parameter estimate (adjusted HR, 0.84; 95% CI, 0.69-1.02).
Table 2. Trends in 90-Day Post-Discharge Total Mortality in Patients Aged 85 Years or More Hospitalized with Acute Myocardial Infarction Between 1997 and 2007.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
|
|
|
|
|
|
| Characteristic | Unadjusted HR (95% CI) | Model 1 + Adjusted for Patient Characteristics (* Comorbidity and 90-d AMI Mortality Risk) Adjusted HR (95% CI) | Model 2 + Adjusted for Guideline-based Medication Use Adjusted HR (95% CI) | Model 3 + Adjusted for Interventional Procedures Adjusted HR (95% CI) |
| Study Year (2003-2007 vs 1997-2001 [ref]) | 0.73 (0.60-0.89) | 0.78 (0.64-0.96) | 1.26 (1.00-1.58) | 1.28 (1.02-1.62) |
| Prescribed in hospital and at discharge | ||||
| Aspirin | - | - | reference | reference |
| ACEI/ARB | - | - | reference | reference |
| Lipid-lowering agent | - | - | reference | reference |
| Beta-blocker | - | - | reference | reference |
| Prescribed in hospital only | ||||
| Aspirin | - | - | 2.61 (1.99-3.44) | 2.66 (2.03-3.50) |
| ACEI/ARB | - | - | 2.09 (1.50-2.90) | 2.24 (1.61-3.12) |
| Lipid-lowering agent | - | - | 1.65 (1.08-2.53) | 1.50 (0.98-2.30) |
| Beta-blocker | - | - | 2.44 (1.83-3.27) | 2.43 (1.82-3.25) |
| Never prescribed | ||||
| Aspirin | 2.03 (1.44-2.50) | 1.94 (1.43-2.65) | ||
| ACEI/ARB | 1.90 (1.38-2.32) | 1.87 (1.42-2.46) | ||
| Lipid-lowering agent | 1.60 (1.17-2.19) | 1.46 (1.07-2.00) | ||
| Beta-blocker | 2.16 (1.62-2.88) | 2.12 (1.60-2.83) | ||
| Interventional procedures | ||||
| PCI or CABG (vs none) | - | - | - | 0.40 (0.24-0.67) |
ACEI = angiotensin-converting enzyme inhibitor; AMI = acute myocardial infarction; ARB = angiotensin receptor blocker; CABG = coronary artery bypass grafting; CI = confidence interval; HR = hazard ratio; PCI = percutaneous coronary intervention.
Comorbidity (history of heart failure, angina) and the predicted probability of 90-day acute myocardial infarction mortality risk based on an adaptation of the model by Krumholzet al20 (including age, sex, diabetes, stroke, history of myocardial infarction, hypertension, chronic obstructive pulmonary disease, history of coronary artery bypass grafting or angioplasty, hypotension in the first 48 hours, in-hospital shock, in-hospital heart failure, initial blood urea nitrogen, initial serum creatinine, initial white blood cell count, and initial electrocardiogram findings [left bundle branch block, right bundle branch block, and ST elevation]).
Discussion
The results of this population-based study demonstrate improved 90-day post-discharge survival between 1997 and 2007 among the oldest old hospitalized with acute myocardial infarction; these encouraging trends seem to have been predominantly explained by increases in the use of guideline-based cardiac medications. Our findings demonstrate significant increases in the use of key guideline-based medications for acute myocardial infarction during hospitalization and at discharge between 1997 and 2007.
The sequential modeling approach helps demonstrate that time trends in survival were explained by guideline-based medication prescribing. First, we showed a significant relationship between time trend and 90-day post-acute myocardial infarction mortality. Second, we showed significant increases in guideline-based medication use over the study period. Third, the unadjusted relationship of time trends with post-discharge survival improvements did not persist after adjustment for guideline-based medication use, supporting the argument that the use of guideline-based medications mediated observed survival trends. Last, sensitivity analysis suggested that the guideline-based medication effect was not a result of a healthy user bias. Although we observed a significant increase in the percentage of older patients undergoing a percutaneous coronary intervention during the study period, the survival effects attributable to coronary interventions were small relative to the effect of the cardiac medications during the years under study.
Our results are similar to those of a study conducted in France among a cohort of elderly patients hospitalized for acute myocardial infarction that demonstrated increased use of evidence-based medications between 2000 and 2001 and 2005 and 2006, and an associated decline in 1-month mortality.11 A significant difference between these results and our findings is that the French study documented a marked increase in the use of coronary reperfusion therapy between their 2 study periods (12% vs 59%) that may have accounted for the observed declines in mortality. In the present study, we did not observe such a large increase in coronary reperfusion therapy use, suggesting that our findings are predominantly related to increased use of guideline-based medications.
Similar results were reported in a study from the Get With The Guidelines–Coronary Artery Disease project, which included more than 30,000 patients with an acute coronary syndrome (mean age, 85 years) hospitalized at more than 400 US medical centers between 2002 and 2009.21 In this population, the use of evidence-based cardiac therapies during hospitalization increased significantly during the study period, whereas the in-hospital death rate declined.
Our finding of increased use of guideline-based medications is important, because there remains underuse of guideline-based medications for acute myocardial infarction in the elderly. For example, the odds of ideal elderly candidates receiving aspirin within 6 hours of hospital arrival was approximately 50% lower relative to that of nonelderly patients22 in one study. In other study, the use of guideline-recommended medications was approximately 30% lower in older patients (mean age, 82 years) compared with the younger cohort (mean age, 60 years).23 Although some argue that the benefits far outweigh the risks for evidence-based medical therapies for acute myocardial infarction in the elderly,24 the paucity of evidence due to the systematic exclusion of the oldest-old from most clinical trials of acute myocardial infarction makes it difficult to guide treatment in this high-risk population25,26.
Study Strengths and Limitations
Our study must be interpreted in light of several strengths and limitations. First, we acknowledge that medication use may be a proxy for unmeasured health status and may contribute to a “healthy user bias” in adjusted analyses.27 Although accounting for hospital-only medication use could be conceptualized as a proxy for medication intolerance and patient frailty, we acknowledge that medications may be discontinued purposefully at discharge because of local practice conventions or patient preference. Although we acknowledge possible unmeasured residual confounding, the findings from our sensitivity analysis with diuretics (a nonguideline medication) argue against healthy-user bias as a causal explanation. Second, we were unable to determine whether patients were eligible for each of the therapies examined. Third, although our study was geographically limited to residents of the Worcester metropolitan area, this central Massachusetts population has been shown to be comparable in terms of sociodemographic and economic characteristics to the overall US population, enhancing the potential generalizability of our findings. We recognize that there is substantial regional variation in the management of patients hospitalized with acute myocardial infarction, but several studies have shown that beneficial cardiac medications are used more often in New England than elsewhere in the country.28 Finally, we lacked data on medication adherence in the 90 days after discharge.
Conclusions
In the 20 years since the systematic exclusion of older adults from acute myocardial infarction trials was originally observed,25 and despite efforts to increase the enrollment of older adults to acute myocardial infarction interventions, there is little direct trial evidence for most therapies used in the management of the oldest old.26 Our study documents that the oldest old segment of the elderly population has experienced considerable gains in 3-month post-discharge survival after acute myocardial infarction between 1997 and 2007 and that this increase in post-discharge survival was primarily accompanied by increased use of guideline-based cardiac medications, and to a lesser extent by the increased use of coronary interventional procedures. Further studies should examine the impact of individual and combined treatments on long-term survival and the effects of medication adherence on end points of clinical and public health importance, including quality of life and recurrent coronary events.
Clinical Significance.
Among a population-based sample of patients aged >85 years hospitalized for acute myocardial infarction, 90-day post-discharge survival improved between 1997 and 2007.
In the same time period, guideline-based medication use increased significantly for patients aged >85 years hospitalized for acute myocardial infarction.
Improvements in 90-day survival after acute myocardial infarction hospitalization seem to be explained by increased use of guideline-based medications.
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area.
Funding: This study was supported by funding from the National Institutes of Health (RO1 HL35434). Investigators received additional funding from the National Heart Lung and Blood Institute (1U01HL105268 to JSS and RJG) and the National Institute on Aging (K01AG033643 to JSS and K23AG034967 to JLG).
Footnotes
Presented in part at: the National Meeting of the American Geriatrics Society, May 12, 2011, Washington DC.
Conflict of Interest: None.
Authorship: All authors had access to the data and played a role in writing this manuscript.
References
- 1.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291:1864–1870. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- 2.Rathore SS, Mehta RH, Wang Y, Radford MJ, Krumholz HM. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am J Med. 2003;114:307–315. doi: 10.1016/s0002-9343(02)01531-0. [DOI] [PubMed] [Google Scholar]
- 3.Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 4.Hovanesyan A, Rich MW. Outcomes of acute myocardial infarction in nonagenarians. Am J Cardiol. 2008;101:1379–1383. doi: 10.1016/j.amjcard.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Jencks SF, Wilensky GR. The health care quality improvement initiative. A new approach to quality assurance in Medicare. JAMA. 1992;268:900–903. [PubMed] [Google Scholar]
- 6.Krumholz HM, Radford MJ, Wang Y, Chen J, Heiat A, Marciniak TA. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA. 1998;280:623–629. doi: 10.1001/jama.280.7.623. [DOI] [PubMed] [Google Scholar]
- 7.Tjia J, Briesacher B, Xie D, Fu J, Goldberg RJ. Disparities in combination drug therapy use in older adults with coronary heart disease. Drugs Aging. 2010;27:1–10. doi: 10.2165/11532150-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 9.Spencer FA, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–844. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Hunink MG, Goldman L, Tosteson AN, et al. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535–542. [PubMed] [Google Scholar]
- 11.Schiele F, Meneveau N, Seronde MF, et al. Changes in management of elderly patients with myocardial infarction. Eur Heart J. 2009;30:987–994. doi: 10.1093/eurheartj/ehn601. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 13.Floyd FC, Yorzebski J, Spencer FA, et al. A 30-year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 15.Saczynski J, McManus D, Zhou Z, et al. Trends in atrial fibrillation complicating acute myocardial infarction. Am J Cardiol. 2009;104:164–174. doi: 10.1016/j.amjcard.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spencer FA, Meyer TE, Goldberg RJ, et al. Twenty year trends (1975-1995) in the incidence, in-hospital and long-term death rates associated with heart failure complicating acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;34:1378–1387. doi: 10.1016/s0735-1097(99)00390-3. [DOI] [PubMed] [Google Scholar]
- 17.Saczynski JS, Spencer FA, Gore JM, et al. Twenty-year trends in the incidence of stroke complicating acute myocardial infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–2110. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119:1211–1219. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cuzick JA. Wilcoxon-type test for trend. Stat Med. 1985;4:87–88. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 21.Medina H, Cannon C, Zhao X, et al. Quality of acute myocardial infarction care and outcomes in 33,997 patients aged 80 years or older: findings from Get With The Guidelines-Coronary Artery Disease (GWTG-CAD) Am Heart J. 2011;162:283–290. doi: 10.1016/j.ahj.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 22.Tran CT, Laupacis A, Mamdani MM, Tu JV. Effect of age on the use of evidence-based therapies for acute myocardial infarction. Am Heart J. 2004;148:834–841. doi: 10.1016/j.ahj.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 23.Schuler J, Maier B, Behrens S, Thimme W. Present treatment of acute myocardial infarction in patients over 75 years–data from the Berlin Myocardial Infarction Registry (BHIR) Clin Res Cardiol. 2006;95:360–367. doi: 10.1007/s00392-006-0393-8. [DOI] [PubMed] [Google Scholar]
- 24.Alter DA, Manuel DG, Gunraj N, Anderson G, Naylor CD, Laupacis A. Age, risk-benefit trade-offs, and the projected effects of evidence-based therapies. Am J Med. 2004;116:540–545. doi: 10.1016/j.amjmed.2003.10.039. [DOI] [PubMed] [Google Scholar]
- 25.Gurwitz JH, Col NF, Avorn J. The exclusion of the elderly and women from clinical trials in acute myocardial infarction. JAMA. 1992;268:1417–1422. [PubMed] [Google Scholar]
- 26.Dodd KH, Saczynski JS, Zhao Y, et al. Exclusion of older adults and women from recent trials of acute coronary syndromes. J Am Geriatr Soc. 2011;59:506–511. doi: 10.1111/j.1532-5415.2010.03305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shrank WH, Patrick AR, Brookhart MA. Health user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med. 2010;26:546–550. doi: 10.1007/s11606-010-1609-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pilote L, Califf RM, Sapp S, et al. Regional variation across the United States in the management of acute myocardial infarction. GUSTO-1 Investigators. Global Utilization of Streptokinase and Tissue Plas-minogen Activator for Occluded Coronary Arteries. N Engl J Med. 1995;333:565–572. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]