Abstract
Significance
Scarring continues to present a significant clinical problem. Wound contraction leads to scarring and is mediated by myofibroblasts and contractile forces across the wound bed. Contracture formation can have a significant impact on the quality of life of the patient, particularly where function and appearance are affected.
Recent Advances
Novel tissue-engineered matrices, cell-based therapies, and medicinal therapeutics have shown significant reduction in wound contraction in in-vivo models, particularly at early time points. These have been accompanied in many cases by reduced numbers of myofibroblasts, and in some by increased angiogenesis and improved neodermal architecture.
Critical Issues
There are no animal models that replicate all aspects of wound healing as seen in patients. Therefore, information obtained from in vivo studies should be assessed critically. Additional studies, in particular those that seek to elucidate the mechanisms by which novel therapies reduce contraction, are needed to gain sufficient confidence to move into clinical testing.
Future Directions
The use of knockout mouse models in particular has generated significant advances in knowledge of the mechanisms behind myofibroblast conversion and other factors involved in generating tension across the wound. Medicinal therapeutics and tissue-engineering approaches that seek to disrupt/alter these pathways hold much promise for future development and translation to clinical practice.

Justin R. Sharpe, PhD
Scope
Full-thickness wounds heal with scarring, due to the abnormal arrangement of de novo collagen fibres in the neodermis and contractile forces exerted on the wound environment and surrounding tissue. Scar formation can have a negative impact on the patient and continues to present a significant clinical challenge. In vivo models take into account the physiological response to injury and the complex interactions that occur during wound repair that cannot be replicated in vitro. This review summarizes recent in vivo studies that have demonstrated efficacy in reducing wound contraction in model organisms.
Translational Relevance
The demonstration of efficacy in vivo of a potential therapy to reduce wound contraction provides strong evidence of potential clinical efficacy. Further investigation and investment can then be undertaken to translate the novel therapy to early-stage clinical studies. In some cases, the manipulation, through the application of novel wound therapies, of the complex cascade of events leading to wound repair may have unwanted deleterious side effects. Both the potential efficacy and any adverse reactions to a therapy can be evaluated in vivo and assessed to inform translation and future clinical development.
Clinical Relevance
The formation of scars after a burn continues to present a major reduction in the quality of life of patients. The treatment of contractures in particular may involve repeated surgical procedures with associated hospital stays and patient morbidity leading to further loss of quality of life. Effective early treatments, which result in a reduction in wound contraction during scar maturation, may be efficiently administered on admission after a burn injury. Treatments, including cell therapy, novel materials, and medicinal therapies, once developed, can be applied in conjunction with the best quality of standard care available to improve final clinical outcome.
Background
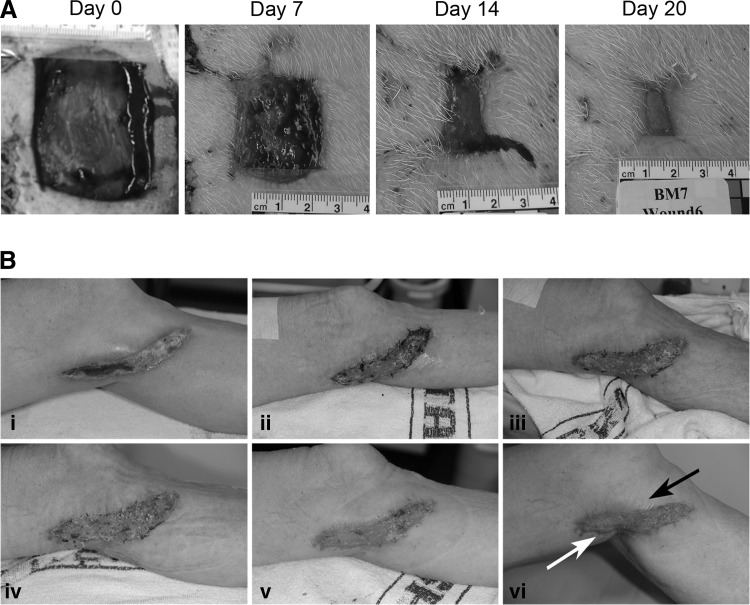
Cutaneous wounds heal through a combination of epithelial migration from the wound margins and contraction of the wound bed to bring the wound margins closer together (Fig. 1). Wound contraction is a vital part of the wound repair process and a highly evolved strategy to reduce the size of the area of wound exposed to the external environment, which subjects the patient to potentially lethal infection and fluid loss. With the development of modern medicine, the mortality rates associated with large acute injuries to the skin such as burns have significantly decreased. The wound contraction and scarring, which occur after such large injuries, can however lead to substantial loss of function and poor aesthetic appearance.1 Strategies and therapies that reduce wound contraction may therefore significantly improve the quality of the life of patients recovering from large cutaneous injuries such as burns.
Figure 1.
Wounds contract over time. (A) Contraction of porcine wounds left to heal by secondary intention for 20 days. (B) Human contact burn to the leg, at admission and at days 8, 12, 15, 20, and 32 after injury (i–vi, respectively). A skin graft was applied at day 8. Black arrow indicates the tension on the surrounding tissue caused by the contracting scar. White arrow indicates hypertrophic scar, possibly developing into contracture.
Contraction is known to proceed through the differentiation of dermal fibroblasts to myofibroblasts and their contractile action on the extracellular matrix through the expression of alpha–smooth muscle actin (α-SMA).2 A substantial amount of research has been undertaken to better understand both the biological mechanisms behind wound contraction and to develop approaches and therapies to reduce contraction and excessive scar formation.3 The differentiation of fibroblasts toward a myofibroblast phenotype is generally accepted as being dependent upon the influence of three primary factors: adhesion to the extracellular matrix via integrin cell surface receptors, stimulation by transforming growth factor beta (TGF-β), and mechanical tension. Therapeutic approaches to reducing wound contraction should therefore act either directly or indirectly on one or more of these key factors.
Wound contraction in animal models
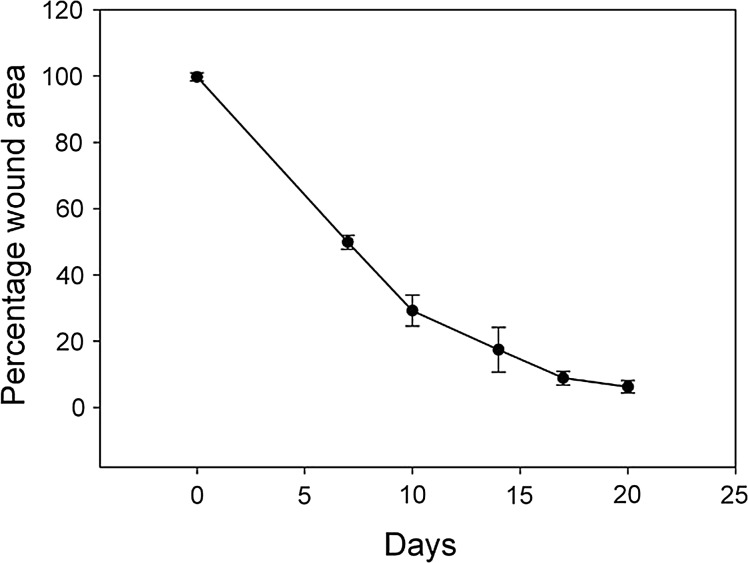
Wound contraction is measured as a reduction in wound area over time and is most accurately quantified in vivo through accurate quantitative measures of wound area at different time points after creation of a wound.4 A representative data set should therefore indicate the original wound size and how this size has decreased over time (Fig. 2). In some studies, wound contraction is described as an effective means of bringing about wound closure. While this is certainly correct with regard to chronic wounds and in reducing mortality rates, the subsequent scarring and contracture formation that occur in humans, especially when large acute wounds contract during the healing process, must be taken into consideration when investigating contraction in vivo. Measurements of re-epithelialization and restoration of barrier function should be separate from measurements of contraction as measured by contracting wound area.4
Figure 2.
Wound contraction measurement. Quantification of wound contraction in porcine full-thickness wounds left to heal by secondary intention for 20 days. Wound size was measured digitally and expressed as the percentage of original size.
No animal model perfectly replicates the effect that any treatment has on wound contraction in humans. However, important information can be inferred from studies in animal models, and the most commonly used models in this field of research are small rodents, rabbits, and pigs.4
Mice and rats are loose-skinned animals; thus, their dermis contracts much more readily than that of humans. This results in faster wound closure times, the mechanism being primarily through contraction.5,6 Information gained from experimental treatments in rodent studies may therefore not necessarily translate to large-animal models or humans. Mice and rats are, however, low-cost and easy to handle. In addition, their skin and physiology have been studied extensively, and detailed information on how an experimental treatment affects wound closure can be gained from rodent models. Efforts have been made to create modified models, where contraction is retarded to more closely mimic the physiology of human wound healing, for example, by splinting7 or by suturing the wound edges to the underlying tissue to prevent contraction.8 Morris et al.9 first described the rabbit ear excision model, which displays raised scars reminiscent of hypertrophic scars in humans, but does not heal by contraction. Others have since used other sites on the rabbit for evaluation of treatments for full-thickness skin defects,10,11 where contraction does occur. Pig skin has similar physiological, anatomical, and biochemical properties to human skin.12,13 With regard to studying epithelial and dermal repair, it is therefore the most appropriate model in the development of therapies for translation to clinical application (Fig. 1).14,15 Furthermore, good correlation between outcomes in the Large White porcine model and human wound healing has been reported.12,16–18 Another advantage of this model is that due to its size, larger wounds can be created than in the other models.19 This mimics more closely the clinical situation of a large burn. However, the Yorkshire/Large White pig does not develop scar tissue akin to humans,13 and long-term studies have not revealed significant effects on contraction.19
Although the advantages and drawbacks of the animal models used in this field are apparent, a wealth of information on the physiological and biological response to therapies can be gained from using these models in experimental settings closely mimicking the clinical situation. The limitations of in vitro studies mean that the complexity of vascularity, immune function, tissue durability, and host interaction cannot be adequately replicated experimentally.
Discussion of Findings and Relevant Literature
Tissue-engineered matrices and cell therapies
In any full-thickness wound, both dermal and epidermal structures must be restored to achieve wound healing. A full-thickness skin graft taken from elsewhere on the body most effectively restores skin function.20 However, in many cases, a surgeon may be presented with a shortage of grafting sites, and other approaches must be considered. The use of split-thickness skin grafts (STSG), which create a donor site that generally heals with minimal scarring, is the most commonly used approach in such cases. In large-burn injuries, however, donor-site availability is limited, and grafts may be meshed to increase the area that they cover. Biocompatible materials, with and without the addition of cells and other molecules, may provide alternative strategies for skin repair. These may negate or reduce the need for autologous donor tissue and may reduce wound contraction.
Several approaches based on collagen type I materials have recently been reported to reduce contraction in vivo. In one such study,21 a novel acellular composite skin replacement was described, consisting of a porous dermal layer of collagen type I, elastin, dermatan sulfate, heparin, fibroblast growth factor (FGF) 2, and vascular endothelial growth factor with a thin epidermal layer of type I collagen, heparin, and FGF 7. In a rat excisional model, this novel skin replacement scaffold was compared with treatment with the dermal substitute Integra™ and with wounds left to heal by secondary intention. At early time points (up to 14 days), there was a clear delay in contraction in the skin replacement group compared with the Integra™ and the control wounds. This was accompanied by reduced numbers of myofibroblasts and an increase in blood vessel ingrowth/formation. By 28 days, all wounds had contracted significantly, and no statistically significant differences remained. Although epithelial migration from the wound edges was observed, the addition of an epithelial component, such as a meshed or ultrathin skin graft, may have more closely modeled the relevant clinical situation, thus leaving many questions unanswered as to the suitability of this treatment method. Other studies using collagen type I-based materials have also shown improvements in wound healing and reduction in contraction at early time points, but no significant results at later time points have been reported to date.10,22
Other natural materials, such as amniotic membrane and acellular porcine dermal matrix, have further shown therapeutic potential in vivo.11,23,24 A comparison between human amniotic membrane and Integra™, both in combination with STSG, applied to Berlin minipigs showed a reduction in contraction in amniotic membrane-treated wounds at 60 days postsurgery. This was accompanied by a delay in the appearance of myofibroblasts in the tissue.24 Contraction was also significantly reduced in a rabbit model when an acellular porcine dermal matrix with hyaluronic acid (HA) was applied in combination with STSG, in comparison with the dermal matrix without HA or STSG alone.11 The authors further noted that collagen deposition in the wounds treated with HA more closely resembled that of normal skin, compared with other wounds, and that vascularization of the grafts was improved.11
Although natural materials have shown promising results in reducing wound contraction, their use may have several drawbacks. As they are obtained from allogeneic or xenogeneic sources, the risk of disease transmission as well as immune reactions to any cellular components remaining in the materials is increased. The use of synthetic polymers may thus overcome such problems. One such scaffold, a polyurethane (PUR) scaffold mixed with polysaccharide (HA or carboxymethylcellulose), was assessed in full-thickness excisional wounds in rats.25 A reduction in contraction was observed at early time points, but this was not statistically significant at later time points. However, the authors investigated the distribution of myofibroblasts and found that the appearance of myofibroblasts was delayed in PUR–polysaccharide-treated wounds, and that the presence of the porous scaffold had disrupted the linear alignment of the cells that could be seen in the untreated wounds. Collagen fiber arrangement followed this pattern, and the authors suggest that by delaying the appearance of myofibroblasts and altering their alignment and subsequent collagen fiber distribution, the linear pattern of contraction seen in the untreated wounds was disrupted.
The incorporation of an epidermal replacement, for example, by the use of autologous cell therapy, in combination with suitable matrix materials, may be a more clinically relevant approach to reducing contraction during wound healing, as both epidermal and dermal structures must be repaired. Such approaches have been investigated for some time, for example, by the addition of fibroblasts to collagen–elastin dermal substitutes in combination with meshed STSG, which resulted in reduced wound contraction in a porcine model.26 More recently, we compared meshed STSG with and without application of sprayed autologous keratinocytes (SAK) with untreated wound left to heal by secondary intention in a porcine model. Significant differences at 3 weeks showed that the addition of SAK to the meshed STSG had reduced contraction further than meshed STSG alone, although this also contracted significantly less than untreated wounds.16 Furthermore, we have found an additional reduction in wound contraction when autologous keratinocytes were applied on gelatin microcarriers in combination with meshed skin grafts in the porcine model compared with spraying the cells onto the wound bed in solution.27
A number of promising treatments utilizing tissue-engineering strategies with biomaterials and cells have been reported in recent years, which have shown a reduction in wound contraction, primarily at early time points.4 Some of these studies have further reported delayed or reduced appearance of myofibroblasts and collagen deposition more closely resembling uninjured skin. However, the exact mechanisms by which these treatments reduce contraction remain unclear at this time, and it thus remains to be seen to what extent they will reduce contraction and scarring in patients. An increased understanding of the mechanisms behind wound contraction has also led to the identification of a number of potential targets toward which medicinal therapies can be directed.
Medicinal therapeutic approaches
The wound repair process is controlled by complex interactions between a large number of growth factors and cytokines,28 and there is significant therapeutic potential in targeting these pathways. Medicinal/biological therapies that inhibit scarring have gained much attention due to their potential to improve the function and aesthetic appearance of patients after surgery or injury. The majority of these therapies are aimed primarily at reducing hypertrophic or keloid scarring characterized by abnormal collagen deposition, although many have also been shown to reduce wound contraction, and these are discussed below.
TGF-β antagonists
TGF-β
Subtypes of the TGF-β family are thought to be responsible for controlling a number of the processes that occur during wound repair, including epithelization, inflammatory cell recruitment, and myofibroblast conversion.29 The subtypes TGF-β1 and TGF-β2, which stimulate fibroblasts toward the contractile myofibroblast phenotype,30 have attracted much attention as potential therapeutic targets. While inhibition of TGF-β1 is an attractive target in terms of reducing myofibroblast-mediated contraction, TGF-β1 is also essential in stimulating other elements of the wound-healing process such as inflammation, angiogenesis,31 and epithelialization.32
While numerous in vitro studies have provided significant information describing the autocrine and paracrine cell-signaling pathways associated with TGF-β–mediated wound contraction,33 a limited number of studies have demonstrated significant therapeutic potential in vivo. Both in vivo and in vitro research into the fundamental mechanisms behind the mode of action of the TGF-β family may provide potential targets for therapies. A range of molecules have been investigated that aim to reduce or modulate the effects of one or more of the TGF-β family.30,34
TGF-β1 and TGF-β2 agonists
In a comprehensive series of studies, the therapeutic potential of blocking TGF-β1 and TGF-β2 was investigated in rat incision wounds.30,35 While parameters associated with wound contraction were not measured, a reduction in scarring was observed through improvements in the architecture of the neodermis. Additionally, exogenous administration of recombinant TGF-β3 indicated a therapeutic potential due to a reduction in monocyte and macrophage numbers and a reduction in collagen type I and type III deposition.30 These initial in vivo studies lead to successful Phase 1 and 2 clinical studies;36 however, after phase 3 studies, the therapy ultimately failed to meet both the primary and secondary end points.
Other studies using amino acid residues 41–65 of TGF-β1 as a TGF-β1 receptor antagonist demonstrated increased epithelialization, reduced wound contraction, and reduced scarring in full-thickness porcine burn and excisional models as well as reduced scarring in a rabbit ear-scarring model.37 Treatment with the same peptide antagonist in partial-thickness porcine burn wounds also demonstrated improved re-epithelialization with reduced contraction and reduced scarring, indicating early potential as a possible therapeutic to reduce contracture formation.32
The inhibition of TGF-β1 action via the Smad signaling pathway is also an attractive therapeutic target for reducing wound contraction. Studies by Au and Ehrlich investigated the effect of SB-505124, which disrupts the Smad pathway through inhibition of activin receptor-like kinase (ALK).38 Excisional wounds in the rat dorsum treated with SB-505124 were found to have a reduced number of myofibroblasts without any reduction in the degree of wound contraction. Contraction was thought to proceed in these studies through the organization of collagen bundles rather than through contractile forces mediated by myofibroblasts. While no increase in epithelialization was found in these studies, the reduction in myofibroblasts may lead to an overall reduction in fibrosis through a change in the mechanism of wound closure. Findings from this and an earlier study39 indicate that wound contraction can proceed in the absence of myofibroblast contractile forces, and that there may be other, as yet unknown, mechanisms causing wound contraction.
Basic fibroblast growth factor
Basic fibroblast growth factor (bFGF) has also been implicated in reducing wound contraction initially though in vitro models40 and more latterly using a collagen sponge model incorporated into full-thickness wounds in rats,41 where a significant reduction in wound contraction and mature collagen formation was found in wounds treated with bFGF. The reduction in contraction was attributed to inhibition of α-SMA expression and apoptosis of α-SMA–positive myofibroblasts. These findings were further supported by an additional study in rats by Ishiguro et al., which showed a decrease in the area positive for α-SMA and an increase in markers of apoptosis.42 In vitro studies have suggested that bFGF stimulated apoptosis selectively in myofibroblasts, but not fibroblasts, and that this may promote reduced contraction and scarring in vivo.43
Rho-associated kinase inhibition
Rho-associated kinase (ROCK) is responsible for promoting contractile force generation through a variety of functions, including the formation of stress fibres, focal adhesions, and the upregulation of α-SMA.44 In excised human scar tissue, ROCK was found to be associated with fibroblasts and expressed to a greater extent than in normal tissue.45 In vivo studies investigated the effect of the ROCK inhibitor fasudil on wounds in a rat excisional model. The subcutaneous administration of fasudil resulted in a significant reduction in wound contraction, while proliferation and neovascularization were unaffected. The authors also reported an in vitro study, which confirmed a reduction in contraction in collagen gels with fasudil, which was accompanied by a reduction in the expression of α-SMA in the presence of TGF-β.45
Matrix metalloproteinase inhibitors
Matrix metalloproteinases (MMPs) are zinc-dependent endopeptidases, which are involved in all stages of wound healing. MMPs contribute to the detachment of keratinocytes from the basement membrane, which allows migration from the wound edges. Later in the wound-healing process, they are also implicated in scar formation.46,47 Broad-spectrum MMP inhibitors, administered both systemically48 and topically49 in rat excisional models, showed a significant reduction in wound contraction, accompanied by a delay in myofibroblast appearance. This was however accompanied by a delay in re-epithelialization from the wound edges. It was suggested that the absence of migrating keratinocytes may have altered epithelial–mesenchymal interactions, which are implicated in causing myofibroblast formation. MMP inhibitors may therefore have potential in reducing contraction, but their targeting ability should be uncoupled from their inhibition of re-epithelialization. It remains to be seen if selective MMP inhibitors can successfully target myofibroblast differentiation and reduce contraction, while normal epithelial repair can proceed.
Take-Home Messages.
Animal models, including rodents, rabbits and pigs, can be used to assess wound contraction by measuring wound size over time.
Tissue-engineering approaches have shown that biocompatible materials can delay the appearance and reduce numbers of myofibroblasts.
Medicinal approaches targeting signaling and biochemical pathways in the wound bed have also shown reduced wound contraction.
Future approaches must focus on clearly identifying the mechanisms underlying reduced wound contraction. These must be harnessed to develop treatments that can be translated to clinic for patient benefit.
Caution, Critical Remarks, and Recommendations
A wide variety of approaches and strategies have been investigated as putative treatments to reduce the severity of pathological wound contraction after full-thickness cutaneous injury. Strategies that aim to reconstruct and restore the function of the dermis or epidermis through the use of materials and/or transplanted cells have shown great potential. By guiding the regeneration of the dermis or epidermis, interaction and interplay between the cells responsible for wound contraction may be modulated to reduce the subsequent formation of myofibroblasts and resultant wound contraction. The early provision of viable epithelial and dermal elements reduces subsequent contraction,16 and the presence of a physical and biological environment conducive to a normal rather than contractile myofibroblast phenotype is crucial.
Similarly, medicinal therapeutic approaches seek to manipulate paracrine and autocrine influences on a number of cell types such that a biological environment biased toward epithelial healing rather than wound contraction is created. While only a number of potential therapeutics have demonstrated efficacy in vivo to date, many potential therapeutic targets are being identified through studies seeking to elucidate the underlying biological processes that cause contraction.
Much work, which falls outside the scope of this review, has been undertaken utilizing in vitro models to screen compounds, which have provided preliminary evidence for potential future therapies. Studies using knockout mice have also indicated further potential therapeutic targets, in particular along the TGF-β–signaling pathway. One such study investigated Smad3 knockout mice,50 which showed accelerated wound closure and variations in wound healing and contraction, which were dependent on the anatomical site of the wound.51 Other studies have shown a decrease in contraction accompanied by reductions in myofibroblast numbers after knockout of periostin52 and myostatin.53 Additional studies into targets outside the TGF-β–signaling pathways have investigated the effect of β2-adrenergic receptor gene deletion. These investigations found that wound contraction was delayed and epithelialization increased through enhanced cell motility and increased VEGF secretion by keratinocytes.54
Such studies highlight the complex relationships between the signaling pathways and the delicate balance between wound contraction and epithelialization. Many of the growth factors such as TGF-β1 have numerous functions that may elicit both positive and negative effects toward contraction-free healing. Future work should seek to combine expertise in surgery and regenerative medicine with fundamental mechanistic research such that the mechanisms behind any observed reduction in wound contraction are better understood. The complexity of wound repair may mean that a combined strategy, employing a number of different surgical, biomaterial, cell therapy, or medicinal therapeutic approaches, will be required to bring about tangible clinical benefits.
Summary
In an effort to reduce contraction during healing and subsequent scarring, several approaches, including tissue engineering and medicinal therapeutic approaches, have been investigated. Some have shown promising results in vivo. Through a better understanding of the mechanism behind wound contraction, new therapeutic targets may emerge. Any reduction in wound contraction after burn injury will result in significant improvements in the quality of life of patients through improvement of function and appearance.
Abbreviations and Acronyms
- ALK
activin receptor-like kinase
- α-SMA
alpha–smooth muscle actin
- bFGF
basic fibroblast growth factor
- HA
hyaluronic acid
- MMP
matrix metalloproteinase
- PUR
polyurethane
- ROCK
rho-associated kinase inhibitor
- SAK
sprayed autologous keratinocytes
- STSG
split-thickness skin graft
- TGF-β
transforming growth factor beta
Acknowledgments and Funding Sources
The authors did not receive any funding for the preparation of this manuscript.
Author Disclosure and Ghostwriting
No competing financial interests exist. The content of this article was expressly written by the authors listed. No ghostwriters were used to write this article.
About the Authors
Dr. Justin R. Sharpe is Head of Research at the Blond McIndoe Research Foundation. He has a long-standing interest in translational research in the field of wound healing and regenerative medicine, with a particular focus on burn wounds. Dr. Yella Martin is a Postdoctoral Fellow at the Blond McIndoe Research Foundation and an Honorary Visiting Fellow at the University of Brighton. Her main research interests are the manipulation of stem cells and the development of novel cell-based therapies to improve wound healing and soft tissue regeneration.
References
- 1.Billingham RE. Medawar PB. Contracture and intussusceptive growth in the healing of extensive wounds in mammalian skin. J Anat. 1955;89:114. [PMC free article] [PubMed] [Google Scholar]
- 2.Wipff PJ. Rifkin DB. Meister JJ. Hinz B. Myofibroblast contraction activates latent TGF-beta1 from the extracellular matrix. J Cell Biol. 2007;179:1311. doi: 10.1083/jcb.200704042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gauglitz GG. Korting HC. Pavicic T. Ruzicka T. Jeschke MG. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Mol Med. 2011;17:113. doi: 10.2119/molmed.2009.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lammers G. Verhaegen PD. Ulrich MM. Schalkwijk J. Middelkoop E. Weiland D. Nillesen ST. Van Kuppevelt TH. Daamen WF. An overview of methods for the in vivo evaluation of tissue-engineered skin constructs. Tissue Eng Part B Rev. 2011;17:33. doi: 10.1089/ten.TEB.2010.0473. [DOI] [PubMed] [Google Scholar]
- 5.Mogford J. Mustoe T. Experimental models of wound healing. In: Falanga V, editor. Cutaneous Wound Healing. London: Martin Dunitz Ltd.; 2001. pp. 109–122. [Google Scholar]
- 6.Dorsett-Martin WA. Rat models of skin wound healing: a review. Wound Repair Regen. 2004;12:591. doi: 10.1111/j.1067-1927.2004.12601.x. [DOI] [PubMed] [Google Scholar]
- 7.Galiano RD. Michaels J. Dobryansky M. Levine JP. Gurtner GC. Quantitative and reproducible murine model of excisional wound healing. Wound Repair Regen. 2004;12:485. doi: 10.1111/j.1067-1927.2004.12404.x. [DOI] [PubMed] [Google Scholar]
- 8.Seland H. Gustafson CJ. Johnson H. Junker JP. Kratz G. Transplantation of acellular dermis and keratinocytes cultured on porous biodegradable microcarriers into full-thickness skin injuries on athymic rats. Burns. 2011;37:99. doi: 10.1016/j.burns.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 9.Morris DE. Wu L. Zhao LL. Bolton L. Roth SI. Ladin DA. Mustoe TA. Acute and chronic animal models for excessive dermal scarring: quantitative studies. Plast Reconstr Surg. 1997;100:674. doi: 10.1097/00006534-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Ananta M. Brown RA. Mudera V. A rapid fabricated living dermal equivalent for skin tissue engineering: an in vivo evaluation in an acute wound model. Tissue Eng Part A. 2012;18:353. doi: 10.1089/ten.TEA.2011.0208. [DOI] [PubMed] [Google Scholar]
- 11.Zhao JY. Chai JK. Song HF. Zhang J. Xu MH. Liang YD. Influence of hyaluronic acid on wound healing using composite porcine acellular dermal matrix grafts, autologous skin in rabbits. Int Wound J. 2012 Jun 11; doi: 10.1111/j.1742-481X.2012.01023.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan TP. Eaglstein WH. Davis SC. Mertz P. The pig as a model for human wound healing. Wound Repair Regen. 2001;9:66. doi: 10.1046/j.1524-475x.2001.00066.x. [DOI] [PubMed] [Google Scholar]
- 13.Zhu KQ. Carrougher GJ. Gibran NS. Isik FF. Engrav LH. Review of the female Duroc/Yorkshire pig model of human fibroproliferative scarring. Wound Repair Regen. 2007;15(Suppl 1):S32. doi: 10.1111/j.1524-475X.2007.00223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Middelkoop E. van den Bogaerdt AJ. Lamme EN. Hoekstra MJ. Brandsma K. Ulrich MM. Porcine wound models for skin substitution and burn treatment. Biomaterials. 2004;25:1559. doi: 10.1016/s0142-9612(03)00502-7. [DOI] [PubMed] [Google Scholar]
- 15.Branski LK. Mittermayr R. Herndon DN. Norbury WB. Masters OE. Hofmann M. Traber DL. Redl H. Jeschke MG. A porcine model of full-thickness burn, excision and skin autografting. Burns. 2008;34:1119. doi: 10.1016/j.burns.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reid MJ. Currie LJ. James SE. Sharpe JR. Effect of artificial dermal substitute, cultured keratinocytes and split thickness skin graft on wound contraction. Wound Repair Regen. 2007;15:889. doi: 10.1111/j.1524-475X.2007.00313.x. [DOI] [PubMed] [Google Scholar]
- 17.James SE. Booth S. Dheansa B. Mann DJ. Reid MJ. Shevchenko RV. Gilbert PM. Sprayed cultured autologous keratinocytes used alone or in combination with meshed autografts to accelerate wound closure in difficult-to-heal burns patients. Burns. 2010;36:e10. doi: 10.1016/j.burns.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Wang XQ. Kravchuk O. Winterford C. Kimble RM. The correlation of in vivo burn scar contraction with the level of alpha-smooth muscle actin expression. Burns. 2011;37:1367. doi: 10.1016/j.burns.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Philandrianos C. Andrac-Meyer L. Mordon S. Feuerstein JM. Sabatier F. Veran J. Magalon G. Casanova D. Comparison of five dermal substitutes in full-thickness skin wound healing in a porcine model. Burns. 2012;38:820. doi: 10.1016/j.burns.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Harrison CA. MacNeil S. The mechanism of skin graft contraction: an update on current research and potential future therapies. Burns. 2008;34:153. doi: 10.1016/j.burns.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Nillesen ST. Lammers G. Wismans RG. Ulrich MM. Middelkoop E. Spauwen PH. Faraj KA. Schalkwijk J. Daamen WF. Van Kuppevelt TH. Design and in vivo evaluation of a molecularly defined acellular skin construct: reduction of early contraction and increase in early blood vessel formation. Acta Biomater. 2011;7:1063. doi: 10.1016/j.actbio.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Garcia Y. Wilkins B. Collighan RJ. Griffin M. Pandit A. Towards development of a dermal rudiment for enhanced wound healing response. Biomaterials. 2008;29:857. doi: 10.1016/j.biomaterials.2007.10.053. [DOI] [PubMed] [Google Scholar]
- 23.Huang G. Ji S. Luo P. Liu H. Zhu S. Wang G. Zhou P. Xiao S. Xia Z. Accelerated expansion of epidermal keratinocyte, improved dermal reconstruction achieved by engineered amniotic membrane. Cell Transplant. 2012 Oct 12; doi: 10.3727/096368912X657945. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Loeffelbein DJ. Baumann C. Stoeckelhuber M. Hasler R. Mucke T. Steinstrasser L. Drecoll E. Wolff KD. Kesting MR. Amniotic membrane as part of a skin substitute for full-thickness wounds: an experimental evaluation in a porcine model. J Biomed Mater Res B Appl Biomater. 2012;100:1245. doi: 10.1002/jbm.b.32689. [DOI] [PubMed] [Google Scholar]
- 25.Adolph EJ. Hafeman AE. Davidson JM. Nanney LB. Guelcher SA. Injectable polyurethane composite scaffolds delay wound contraction and support cellular infiltration and remodeling in rat excisional wounds. J Biomed Mater Res A. 2011;100A:450. doi: 10.1002/jbm.a.33266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lamme EN. Van Leeuwen RT. Brandsma K. Van Marle J. Middelkoop E. Higher numbers of autologous fibroblasts in an artificial dermal substitute improve tissue regeneration and modulate scar tissue formation. J Pathol. 2000;190:595. doi: 10.1002/(SICI)1096-9896(200004)190:5<595::AID-PATH572>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 27.Eldardiri M. Martin Y. Roxburgh J. Lawrence-Watt DJ. Sharpe JR. Wound contraction is significantly reduced by the use of microcarriers to deliver keratinocytes and fibroblasts in an in vivo pig model of wound repair and regeneration. Tissue Eng Part A. 2012;18:587. doi: 10.1089/ten.TEA.2011.0258. [DOI] [PubMed] [Google Scholar]
- 28.Werner S. Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- 29.Singer AJ. Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 30.Shah M. Foreman DM. Ferguson MW. Neutralisation of TGF-beta 1 and TGF-beta 2 or exogenous addition of TGF-beta 3 to cutaneous rat wounds reduces scarring. J Cell Sci. 1995;108(Pt 3):985. doi: 10.1242/jcs.108.3.985. [DOI] [PubMed] [Google Scholar]
- 31.Penn JW. Grobbelaar AO. Rolfe KJ. The role of the TGF-beta family in wound healing, burns and scarring: a review. Int J Burns Trauma. 2012;2:18. [PMC free article] [PubMed] [Google Scholar]
- 32.Singer AJ. Huang SS. Huang JS. McClain SA. Romanov A. Rooney J. Zimmerman T. A novel TGF-beta antagonist speeds reepithelialization and reduces scarring of partial thickness porcine burns. J Burn Care Res. 2009;30:329. doi: 10.1097/BCR.0b013e31819a6369. [DOI] [PubMed] [Google Scholar]
- 33.Carthy JM. Garmaroudi FS. Luo Z. McManus BM. Wnt3a induces myofibroblast differentiation by upregulating TGF-beta signaling through SMAD2 in a beta-catenin-dependent manner. PLoS One. 2011;6:e19809. doi: 10.1371/journal.pone.0019809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laverty HG. Occleston NL. Johnson M. Little J. Jones R. Fairlamb D. Ferguson MW. O'Kane S. Effects of avotermin (transforming growth factor beta3) in a clinically relevant pig model of long, full-thickness incisional wounds. J Cutan Med Surg. 2010;14:223. doi: 10.2310/7750.2010.09069. [DOI] [PubMed] [Google Scholar]
- 35.Shah M. Foreman DM. Ferguson MW. Neutralising antibody to TGF-beta 1,2 reduces cutaneous scarring in adult rodents. J Cell Sci. 1994;107(Pt 5):1137. doi: 10.1242/jcs.107.5.1137. [DOI] [PubMed] [Google Scholar]
- 36.So K. McGrouther DA. Bush JA. Durani P. Taylor L. Skotny G. Mason T. Metcalfe A. O'Kane S. Ferguson MW. Avotermin for scar improvement following scar revision surgery: a randomized, double-blind, within-patient, placebo-controlled, phase II clinical trial. Plast Reconstr Surg. 2011;128:163. doi: 10.1097/PRS.0b013e318217429b. [DOI] [PubMed] [Google Scholar]
- 37.Huang JS. Wang YH. Ling TY. Chuang SS. Johnson FE. Huang SS. Synthetic TGF-beta antagonist accelerates wound healing and reduces scarring. FASEB J. 2002;16:1269. doi: 10.1096/fj.02-0103fje. [DOI] [PubMed] [Google Scholar]
- 38.Au K. Ehrlich HP. When the Smad signaling pathway is impaired, fibroblasts advance open wound contraction. Exp Mol Pathol. 2010;89:236. doi: 10.1016/j.yexmp.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ehrlich HP. Keefer KA. Myers RL. Passaniti A. Vanadate and the absence of myofibroblasts in wound contraction. Arch Surg. 1999;134:494. doi: 10.1001/archsurg.134.5.494. [DOI] [PubMed] [Google Scholar]
- 40.Khouw IM. van Wachem PB. Plantinga JA. Vujaskovic Z. Wissink MJ. de Leij LF. van Luyn MJ. TGF-beta and bFGF affect the differentiation of proliferating porcine fibroblasts into myofibroblasts in vitro. Biomaterials. 1999;20:1815. doi: 10.1016/s0142-9612(99)00077-0. [DOI] [PubMed] [Google Scholar]
- 41.Akasaka Y. Ono I. Tominaga A. Ishikawa Y. Ito K. Suzuki T. Imaizumi R. Ishiguro S. Jimbow K. Ishii T. Basic fibroblast growth factor in an artificial dermis promotes apoptosis and inhibits expression of alpha-smooth muscle actin, leading to reduction of wound contraction. Wound Repair Regen. 2007;15:378. doi: 10.1111/j.1524-475X.2007.00240.x. [DOI] [PubMed] [Google Scholar]
- 42.Ishiguro S. Akasaka Y. Kiguchi H. Suzuki T. Imaizumi R. Ishikawa Y. Ito K. Ishii T. Basic fibroblast growth factor induces down-regulation of alpha-smooth muscle actin and reduction of myofibroblast areas in open skin wounds. Wound Repair Regen. 2009;17:617. doi: 10.1111/j.1524-475X.2009.00511.x. [DOI] [PubMed] [Google Scholar]
- 43.Abe M. Yokoyama Y. Ishikawa O. A possible mechanism of basic fibroblast growth factor-promoted scarless wound healing: the induction of myofibroblast apoptosis. Eur J Dermatol. 2012;22:46. doi: 10.1684/ejd.2011.1582. [DOI] [PubMed] [Google Scholar]
- 44.Riento K. Ridley AJ. Rocks: multifunctional kinases in cell behaviour. Nat Rev Mol Cell Biol. 2003;4:446. doi: 10.1038/nrm1128. [DOI] [PubMed] [Google Scholar]
- 45.Bond JE. Kokosis G. Ren L. Selim MA. Bergeron A. Levinson H. Wound contraction is attenuated by fasudil inhibition of Rho-associated kinase. Plast Reconstr Surg. 2011;128:438e. doi: 10.1097/PRS.0b013e31822b7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gill SE. Parks WC. Metalloproteinases, their inhibitors: regulators of wound healing. Int J Biochem Cell Biol. 2008;40:1334. doi: 10.1016/j.biocel.2007.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toriseva M. Kahari VM. Proteinases in cutaneous wound healing. Cell Mol Life Sci. 2009;66:203. doi: 10.1007/s00018-008-8388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mirastschijski U. Haaksma CJ. Tomasek JJ. Agren MS. Matrix metalloproteinase inhibitor GM 6001 attenuates keratinocyte migration, contraction and myofibroblast formation in skin wounds. Exp Cell Res. 2004;299:465. doi: 10.1016/j.yexcr.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Mirastschijski U. Schnabel R. Claes J. Schneider W. Agren MS. Haaksma C. Tomasek JJ. Matrix metalloproteinase inhibition delays wound healing and blocks the latent transforming growth factor-beta1-promoted myofibroblast formation and function. Wound Repair Regen. 2010;18:223. doi: 10.1111/j.1524-475X.2010.00574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Falanga V. Schrayer D. Cha J. Butmarc J. Carson P. Roberts AB. Kim SJ. Full-thickness wounding of the mouse tail as a model for delayed wound healing: accelerated wound closure in Smad3 knock-out mice. Wound Repair Regen. 2004;12:320. doi: 10.1111/j.1067-1927.2004.012316.x. [DOI] [PubMed] [Google Scholar]
- 51.Arany PR. Flanders KC. Kobayashi T. Kuo CK. Stuelten C. Desai KV. Tuan R. Rennard SI. Roberts AB. Smad3 deficiency alters key structural elements of the extracellular matrix and mechanotransduction of wound closure. Proc Natl Acad Sci USA. 2006;103:9250. doi: 10.1073/pnas.0602473103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elliott CG. Wang J. Guo X. Xu SW. Eastwood M. Guan J. Leask A. Conway SJ. Hamilton DW. Periostin modulates myofibroblast differentiation during full-thickness cutaneous wound repair. J Cell Sci. 2012;125:121. doi: 10.1242/jcs.087841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang C. Tan CK. McFarlane C. Sharma M. Tan NS. Kambadur R. Myostatin-null mice exhibit delayed skin wound healing through the blockade of transforming growth factor-beta signaling by decorin. Am J Physiol Cell Physiol. 2012;302:C1213. doi: 10.1152/ajpcell.00179.2011. [DOI] [PubMed] [Google Scholar]
- 54.Pullar CE. Le Provost GS. O'Leary AP. Evans SE. Baier BS. Isseroff RR. β2AR antagonists and β2AR gene deletion both promote skin wound repair processes. J Invest Dermatol. 2012;132:2076. doi: 10.1038/jid.2012.108. [DOI] [PMC free article] [PubMed] [Google Scholar]