Abstract
Background
The indications for microsurgical toe-to-hand transfers in congenital hand surgery have not been defined as clearly as for posttraumatic reconstruction of thumb and finger amputations. The purpose of this study was to develop simple guidelines for referral of children with congenital absent digits for consideration of microsurgical reconstruction with toe-to-hand transfers, based on the morphological or radiographic anatomy of the hand anomaly, not on embryological classifications.
Methods
From a consecutive series of 204 children referred with congenital absence of the thumb and fingers, 100 toe-to-hand transfers were performed. The indications for microsurgical reconstruction of these children were analyzed retrospectively.
Results
Forty-one thumbs were reconstructed in 38 children—15 children with an absent thumb distal to the metacarpal base but with four relatively normal fingers; 12 children with an absent thumb and only one or two digits remaining on the ulnar side of the hand; and 11 children with complete absence of all five digits. Twenty-nine second toes and 12 great toes were transferred to reconstruct congenital absent thumbs. Fifty-nine fingers in 52 children were reconstructed mostly with single second toe transfers—41 children with a thumb but absence of all four fingers and 11 children with absence of all five digits.
Conclusions
The morphological or radiographic anatomy of a child’s hand with congenital absent digits is a more logical indication for microsurgical reconstruction than any embryological classification. The three most common indications for toe transfers for reconstruction of congenital absent thumbs are (1) absent thumb distal to the carpometacarpal joint with four relatively normal fingers, (2) absent thumb with only one or two fingers remaining on the ulnar border of the hand, and (3) complete absence of the thumb and all four fingers. The two indications for toe transfers for reconstruction of congenital absent fingers are (1) absence of all four fingers but with a normal thumb remaining and (2) complete absence of all five digits.
Keywords: Toe to thumb transfers, Congenital hand anomalies, Toe to hand transfers
Introduction
Posttraumatic reconstruction of amputations of the thumb and multiple amputations of the fingers has become well-established, using either the great toe [5, 8], the Morrison “wrap-around” flap [26] and “trimmed” toe [35, 38] variations of the great toe, the second toe [41], simultaneous double second toes [9], and combined second and third toe transfers [39]. Success rates of toe transfers for posttraumatic reconstruction of children’s hands are comparable to adults [40].
Conventional nonmicrosurgical reconstruction of congenital absent digits usually involves pollicization of the index finger for children born with hypoplastic or absent thumbs [4, 21], nonvascularized toe phalangeal bone grafting [29], and distraction lengthening [25] of hypoplastic digits due to symbrachydactyly, cleft hand, and congenital constriction ring syndrome. The first microsurgical toe transfer to reconstruct a congenital hand anomaly was performed by O’Brien et al. in 1977 who successfully transferred the great toe to reconstruct a hypoplastic thumb in two children [28]. May et al. [23] reported bilateral great toe-to-thumb transfers to reconstruct a 9-year-old boy with bilateral aplasia of his thumb, index, and middle fingers. Yoshimura [42] reported 33 pediatric toe transfers in 28 children, 2 of whom had congenital anomalies—one child had an absent thumb, index, and middle fingers and the second child had congenital constriction ring syndrome. After other case reports [24, 27], several surgeons have reported larger series of microsurgical toe-to-hand transfers to reconstruct various congenital anomalies of the hand [3, 10–13, 15, 17–20, 30, 31, 36, 37].
All these series have focused on the embryological types of congenital hand anomalies, the surgical techniques, and the results with respect to motion, sensibility, and growth; but very little has been published on the specific indications for microsurgical reconstruction of congenital absent digits. Most pediatricians and even some hand surgeons do not understand which children should be considered for microsurgical reconstruction. This study attempts to define the evolving indications for toe-to-hand transfers for children born with congenital absence of the thumb and fingers and provides guidelines for the referral of these children for consideration of microsurgical reconstruction, based simply on the morphological and radiographic anatomy of the hand anomaly itself and not on any embryological classification.
Materials and Methods
After institutional review board approval, analysis of 204 children born with congenital absent digits who had been referred to the senior author (NFJ) over the period 1995–2010 for either conventional or microsurgical reconstruction [16] identified 79 children who had been reconstructed with 100 consecutive toe transfers. The medical records, photographs, and radiographs of this cohort of children were analyzed retrospectively. Forty-one children were boys and 38 were girls with an age range from 2 to 14 years. The congenital anomalies had been classified embryologically as symbrachydactyly in 45 children, congenital constriction ring syndrome in 23 children, and transverse failure of formation in 8 children. No children born with congenitally deficient Blauth IV or V thumbs [1] were reconstructed with toe transfers in this series. Two children had congenital vascular malformations and one child developed gangrene of the remaining thumb after excision of Wassel type IV thumb polydactyly. Forty-one thumbs in 38 children and 59 fingers in 52 children were reconstructed. Eighty-five second toes, 13 great toes, and 1 combined second-third toe were transferred. Three children underwent bilateral reconstructions and 18 children underwent two toe transfers for reconstruction of an unilateral hand anomaly, either sequentially or simultaneously.
Results
Fifteen toe-to-thumb transfers (14 second toes and 1 great toe) were performed in 15 children born with four fingers but an absent thumb distal to the metacarpal base with an intact carpometacarpal joint and remnant of thenar muscles, due to congenital constriction ring syndrome or transverse failure. These transversely deficient thumbs are completely different from radial longitudinally hypoplastic Blauth type IV and V thumbs [1]. Twelve children underwent 15 toe-to-thumb transfers (11 great toes and 4 second toes) for a congenital absent thumb and only one or two fingers remaining on the ulnar border of the hand, due to type III monodactylous symbrachydactyly, radial longitudinal deficiency, or congenital constriction ring syndrome. Eleven toe-to-thumb transfers (11 second toes) were performed in 11 children born with complete absence of all five digits due to type IV adactylous symbrachydactyly or transverse deficiency. Twenty-nine second toes and 12 great toes were transferred to reconstruct congenital absent thumbs.
Forty-one children born with a thumb but absence of all four fingers proximal to the proximal interphalangeal joints, due to type III monodactylous symbrachydactyly, transverse deficiency, congenital constriction ring syndrome, or severe ulnar deficiency, underwent finger reconstruction with 48 toe transfers (33 single second toes, 12 bilateral second toes, 1 combined second–third toes, and 1 great toe). Eleven children born with complete absence of all five digits, due to type IV adactylous symbrachydactyly or transverse deficiency, underwent reconstruction of both a thumb and a finger on the ulnar border of the hand (11 second toes). Forty-four single second toes, 12 bilateral second toes, 1 combined second–third toe transfer, and 1 great toe transfer were performed to reconstruct congenital absent fingers (Table 1 and Fig. 1).
Table 1.
Morphological indications for microsurgical reconstruction of children with congenital absent digits
| Children | Toe transfers | Great toe | Single second toe | Double second toes | Combined 2nd and 3rd toes | |
|---|---|---|---|---|---|---|
| Thumb reconstruction | ||||||
| Absent thumb but 4 normal fingers | 15 | 15 | 1 | 14 | – | – |
| Absent thumb but only 1–2 fingers | 12 | 15 | 11 | 4 | – | – |
| Absent thumb and 4 fingers | 11 | 11 | – | 11 | – | – |
| Finger reconstruction | ||||||
| Absence of all 4 fingers but normal thumb | 41 | 48 | 1 | 33 | 12 | 1 |
| Absence of all 4 fingers and thumb | 11 | 11 | – | 11 | – | – |
| Total | 79 | 100 | 13 | 73 | 12 | 1 |
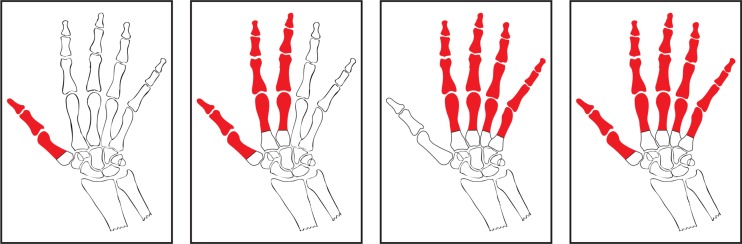
Fig. 1.
Diagrammatic representation of the four most common morphological indications for microsurgical reconstruction of congenital absence of the thumb and fingers by toe-to-hand transfers
Discussion
Gilbert [12, 13] described 17 children with constriction ring syndrome and aplasia who underwent 21 second toe transfers to reconstruct 4 thumbs and 17 fingers. Results were better in constriction ring syndrome compared with aplasia because the structures were normal proximally. The ideal diagnosis was constriction ring syndrome with an intact metacarpophalangeal joint. Lister [10, 20] reported 12 children who underwent second toe transfers to reconstruct congenitally deficient thumbs due to transverse deficiency, constriction ring syndrome, and symbrachydactyly. Shvedovchenko [31] reported 103 toe transfers in 66 children, 49 of whom had ectrodactyly, brachydactyly, adactyly, and hypoplasia. Vilkki [37] performed toe transfers in 30 children with congenital hand anomalies, 14 for aplasia of all four fingers, and 4 for thumb reconstruction. Kay et al. [3, 17–19] transferred 45 toes for symbrachydactyly, transverse deficiency, complex syndactyly, and constriction ring syndrome. The ideal diagnosis was constriction ring syndrome involving the thumb because structures were normal proximally. The benefits of simultaneous double second toe transfers were emphasized. Foucher et al. [11] performed 65 toe transfers in 58 children for category I (failure of formation), category V (undergrowth), and category VI (constriction ring syndrome) anomalies [33]. Symbrachydactyly was the most common diagnosis (45 children, 51 transfers) and much less frequently, transverse deficiency, IIIB thumb hypoplasia [22], ulnar deficiency, central deficiency, and macrodactyly. Van Holder et al. [36] reconstructed 14 children with constriction ring syndrome, symbrachydactyly, and transverse deficiency with sequential double second toe transfers. Richardson et al. [30] transferred 18 toes in 13 children with types III and IV symbrachydactyly [2]. Jones et al. [15] reported 82 toe transfers in 68 children with symbrachydactyly, constriction ring syndrome, and transverse deficiencies and described specific indications for “spare parts” great toe transfers to reconstruct the thumb in children with cleft hand and cleft feet [7]. Harashina et al. [14] described one child and Tu et al. [34] reported 11 children who underwent second toe transfers to reconstruct Blauth types IIIB, IV, and V hypoplastic thumbs [1] because the parents refused pollicization.
Microsurgical reconstruction of congenital hand anomalies remains controversial. Firstly, surgeons may be reluctant to risk the small but potential loss of a toe transfer in a child who is already missing one or more digits in their hands. Secondly, some pediatric hand surgeons still maintain that children with unilateral absence of one of more digits adapt to their impairment as they grow or can be helped with a static or functional prosthesis. Finally, parents may be reluctant to accept a very complicated reconstructive procedure that carries a small risk of ending up with a missing second or great toe as well as more scars on the hand to show for the failed endeavor.
Rather than just showing pre- and postoperative photographs, videos, or moulages, the senior author’s practice is to arrange for prospective parents to meet the parents of a child with a similar congenital hand anomaly who has previously undergone a toe transfer, so that the parents can see for themselves the potential function and appearance of the reconstructed hand, as well as speak with the parents about their concerns.
Previous reports of toe transfers for congenital hand anomalies have been based primarily on the embryological diagnoses [33]. However, it is the authors’ contention that specific indications for toe transfers are more logically defined by the morphological or radiographic anatomy of the hand anomaly itself, a concept that is also much more easily understood by referring pediatricians and surgeons. For a child born missing a thumb but with four relatively normal fingers, or missing a thumb as well as the index, middle (and ring) fingers, it is intuitive to reconstruct a thumb to oppose to these fingers. Similarly, for a child missing all four fingers, it is logical to reconstruct one or two fingers to allow pinch and grasp to the more mobile thumb.
Based on this experience of 100 toe transfers, there are three indications for considering microsurgical reconstruction of an absent thumb (Fig. 1):
Isolated absence of the thumb, distal to the metacarpal base with preservation of the carpometacarpal joint and thenar muscles and with four normal or relatively normal fingers (Fig. 2). Reconstruction of these thumbs with a toe transfer is superior to index finger pollicization, distraction lengthening, or nonvascularized toe phalangeal bone grafting because it provides greater length and growth potential and preserves the full complement of fingers (Figs. 3 and 4). Very rarely, a child’s thumb can become involved by progressive macrodactyly or a rapidly growing vascular malformation unresponsive to embolization or sclerotherapy. This situation can potentially be salvaged by radical resection of the thumb preserving the carpometacarpal joint and base of the thumb metacarpal and thenar muscles, followed immediately by a second toe transfer [6].
Absence of the thumb as well as the index, middle, and ring fingers, but with one or two fingers remaining on the ulnar side of the hand (Fig. 5). A second toe can be transferred to reconstruct the absent thumb with minimal donor site morbidity, but the modified “wrap-around” [26] or trimmed great toe [35, 38] techniques can occasionally be considered in older children to provide an excellent functional result and a “thumb” very similar in appearance to the contralateral normal thumb (Figs. 6 and 7). In unilateral or bilateral cleft hand and cleft foot, an abnormal great toe may occasionally need to be amputated to facilitate shoe fitting and can be transferred to reconstruct an absent thumb [7], although these abnormal great toes require secondary revision to achieve more normal alignment to the new thumb.
Unilateral and extremely rarely bilateral absence of all five digits (Fig. 10).
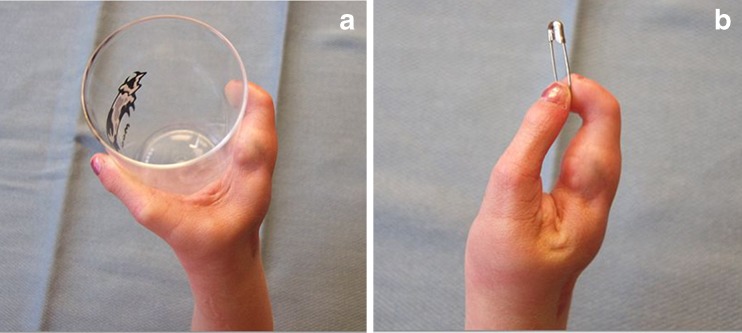
Fig. 2.
a Preoperative photograph and b radiograph of a 2-year-old girl with congenital constriction ring syndrome affecting her right thumb. The thumb is missing from just distal to the metacarpophalangeal joint but the thenar muscles are preserved
Fig. 3.
The congenital constriction ring syndrome also caused an above knee amputation of the left lower extremity and a an abnormality of the right great toe, so only the b right second toe was available for transfer
Fig. 4.

Three years postoperatively, the second toe to right thumb transfer has comparable appearance to the normal left thumb and excellent opposition to the small finger
Fig. 5.
a Preoperative photograph and b radiograph of a three-year-old girl with severe congenital constriction ring syndrome affecting the right thumb, index, middle, and ring fingers. The thumb is missing from just distal to the metacarpophalangeal joint but the thenar muscles are preserved and the ring and small fingers are relatively functional
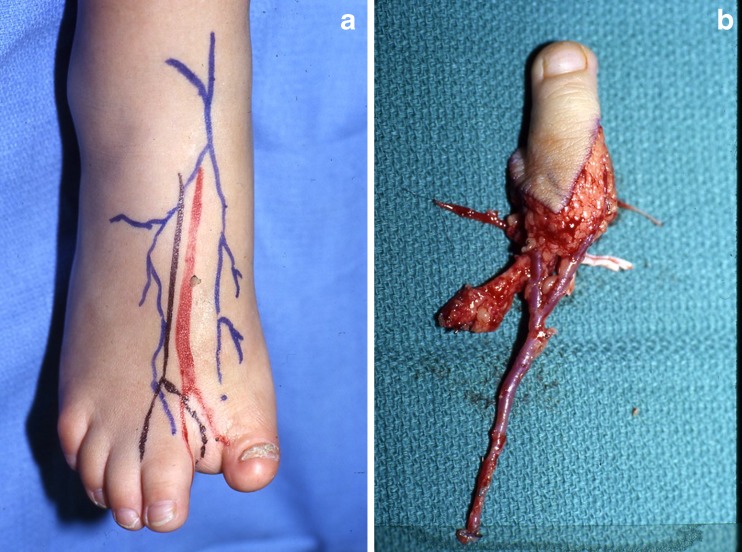
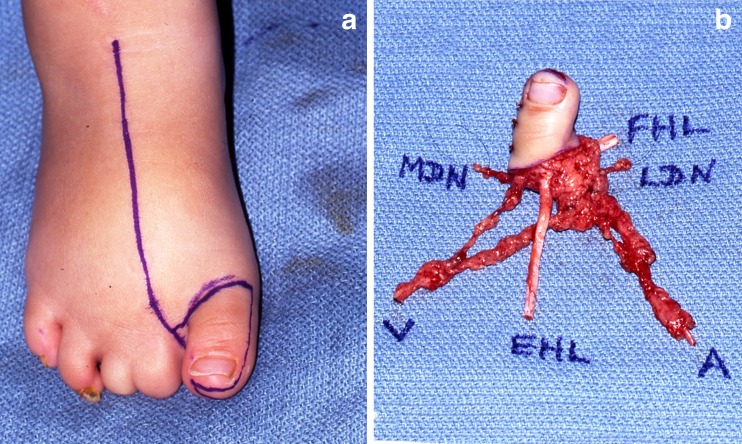
Fig. 6.
Because the second and third toes in both feet were affected by the congenital constriction ring syndrome, a a trimmed right great toe transfer was designed for b transfer to the hand
Fig. 7.

Two years postoperatively, the trimmed right great toe-to-right thumb transfer has comparable appearance to the normal left thumb and excellent opposition to the only normal small finger
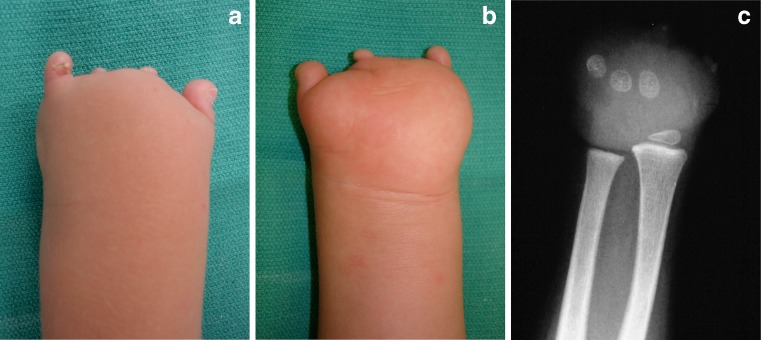
Fig. 10.
a Dorsal photograph, b palmar photograph, and c radiograph of a 2-year-old boy with symbrachydactyly affecting his left hand. All five digits are missing from the level of the metacarpal bases
It could be argued that subcategorizing children with just an isolated absent thumb and children with absence of the thumb as well as one, two, or three fingers is not necessary. However, there is a definite subgroup of children who only have an absent thumb and another separate subgroup who have absence of their thumb, index, middle, and ring fingers. Secondly, children with only an absent thumb may be candidates for conventional reconstruction by index finger pollicization or distraction lengthening or microsurgical reconstruction by toe-to-thumb transfer, whereas the only option for children missing their thumb, index, middle, and ring fingers is a toe-to-thumb transfer.
Based on this experience of 100 toe transfers, there are two indications for considering toe transfers to reconstruct absent fingers (Fig. 1):
Absence of all four fingers proximal to the base of the middle phalanges, but with a normal thumb (Fig. 8). Microsurgical reconstruction of at least one finger against which the thumb can oppose to may be accomplished by a single second toe transfer into the ring or small finger position to allow both pinch and grasp (Fig. 9). Alternatively, two second toes can be transferred, either simultaneously or sequentially, into the middle and small finger positions to allow three-point pinch. Occasionally, combined second and third toes can be transferred into the middle–ring or ring–small finger positions.
Complete absence of all five digits (Fig. 10) can be reconstructed using two second toe transfers into the thumb and ring or small finger positions. This can be performed simultaneously, but is probably better performed sequentially, so that positioning of the second transfer into a finger position can be adjusted to the position and mobility of the first toe transfer into the thumb position (Fig. 11).
Fig. 8.

Photograph of a 6-month-old baby girl with symbrachydactyly of her right hand, with a normal thumb but absence of all four fingers, represented just by nubbins
Fig. 9.
Five years postoperative second toe-to-small finger transfer, the child has a excellent grasp between the thumb and second toe transfer into the small finger position and b very precise pinch between the thumb and toe transfer
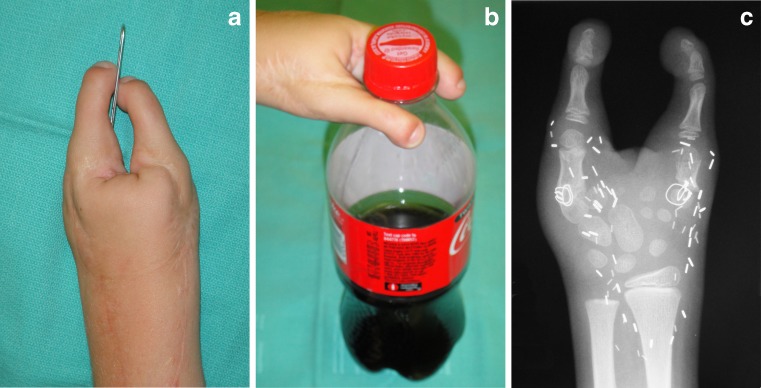
Fig. 11.
The child underwent staged second toe transfers, firstly into the thumb position and 6 months later into the small finger position. Five years postoperatively, the child demonstrates a excellent ability to pick up small objects by side-to-side pinch between the two second toe transfers and b strong grasp to lift a heavy bottle. c Radiograph showing reconstruction of his left hand with staged sequential second toe transfers into the thumb and small finger positions
Even though the external morphological appearance and a plain radiograph of the hand are reliable indications for consideration of a toe-to-hand transfer, they do not imply availability of internal recipient structures. Several authors [12, 13, 17, 18] have observed that tendons and nerves are more likely to be normal proximal to a constriction ring compared with symbrachydactyly, and this has been confirmed in this series. However, with increasing experience, the lack of suitable recipient tendons and nerves, which may be encountered in symbrachydactyly, can be circumvented by using tendon grafts or tendon transfers and nerve grafts or nerve transfers.
Microsurgical toe transfers for reconstruction of congenital hand anomalies will hopefully become accepted into the armamentarium of pediatric hand surgeons, although it requires a very high level of microsurgical skill by the surgeon and the ultimate trust of the parents. The optimal age for toe transfers remains unknown, but most experienced surgeons believe toe transfers between 2 and 3 years of age have the best cortical integration, although transfers have been successfully reported in older children [32]. It is very difficult to prove conclusively that microsurgical reconstruction is superior to either no surgical intervention or conventional reconstruction, but a child able to write his/her name for the first time, or pick up a cup singlehandedly, or ride a bicycle provides far greater confirmation than the most sophisticated outcome instruments. Parental assessment of their children’s functional outcomes and even the child’s own assessment is the subject of a future publication.
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Blauth W. The hypoplastic thumb. Arch Orthop Unfallchir. 1967;62(3):225–246. doi: 10.1007/BF00416751. [DOI] [PubMed] [Google Scholar]
- 2.Blauth W, Gekeler J. Morphology and classification of symbrachydactylia. Handchirurgie. 1971;3(4):123–128. [PubMed] [Google Scholar]
- 3.Bradbury ET, Kay SP, Hewison J. The psychological impact of microvascular free toe transfer for children and their parents. J Hand Surg Br. 1994;19(6):689–695. doi: 10.1016/0266-7681(94)90236-4. [DOI] [PubMed] [Google Scholar]
- 4.Buck-Gramcko D. Pollicization of the index finger. Method and results in aplasia and hypoplasia of the thumb. J Bone Joint Surg Am. 1971;53(8):1605–1617. [PubMed] [Google Scholar]
- 5.Buncke HJ, Jr, McLean DH, George PT, Creech BJ, Chater NL, Commons GW. Thumb replacement: great toe transplantation by microvascular anastomosis. Br J Plast Surg. 1973;26(3):194–201. doi: 10.1016/0007-1226(73)90002-7. [DOI] [PubMed] [Google Scholar]
- 6.Carlsen B, Jones NF. Radical resection of a massive venous malformation of the thumb and immediate reconstruction with a microsurgical toe transfer. J Hand Surg Am. 2007;32(10):1587–1591. doi: 10.1016/j.jhsa.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 7.Chang J, Jones NF. Simultaneous toe-to-hand transfer and lower extremity amputations for severe upper and lower limb defects: the use of spare parts. J Hand Surg Br. 2002;27(3):219–223. doi: 10.1054/jhsb.2001.0735. [DOI] [PubMed] [Google Scholar]
- 8.Cobbett JR. Free digital transfer. Report of a case of transfer of a great toe to replace an amputated thumb. J Bone Joint Surg Br. 1969;51(4):677–679. [PubMed] [Google Scholar]
- 9.Coskunfirat OK, Wei F-C, Lin C-H, Chen H-C, Lin Y-T. Simultaneous double second toe transfer for reconstruction of adjacent fingers. Plast Reconstr Surg. 2005;115(4):1064–1069. doi: 10.1097/01.PRS.0000156144.86563.A9. [DOI] [PubMed] [Google Scholar]
- 10.Eaton CJ, Lister GD. Toe transfer for congenital hand defects. Microsurgery. 1991;12(3):186–195. doi: 10.1002/micr.1920120308. [DOI] [PubMed] [Google Scholar]
- 11.Foucher G, Medina J, Navarro R, Nagel D. Toe transfer in congenital hand malformations. J Reconstr Microsurg. 2001;17(1):1–7. doi: 10.1055/s-2001-12682. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert A. Toe transfers for congenital hand defects. J Hand Surg Am. 1982;7(2):118–124. doi: 10.1016/S0363-5023(82)80074-9. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert A. Reconstruction of congenital hand defects with microvascular toe transfers. Hand Clin. 1985;1(2):351–360. [PubMed] [Google Scholar]
- 14.Harashina T, Inoue T, Fujino T, Uchinishi K, Itoh Y. Reconstruction of a floating thumb with an excess big toe. J Reconstr Microsurg. 1994;10(1):11–15. doi: 10.1055/s-2007-1006565. [DOI] [PubMed] [Google Scholar]
- 15.Jones NF, Hansen SL, Bates SJ. Toe-to-hand transfers for congenital anomalies of the hand. Hand Clin. 2007;23(1):129–136. doi: 10.1016/j.hcl.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Jones NF, Kaplan J. A new documentation system for congenital absent digits. Hand. 2012;7(4):391–399. [DOI] [PMC free article] [PubMed]
- 17.Kay S, McGuiness C. Microsurgical reconstruction in abnormalities of children’s hands. Hand Clin. 1999;15(4):563–583. [PubMed] [Google Scholar]
- 18.Kay SP, Wiberg M. Toe to hand transfer in children. Part 1: technical aspects. J Hand Surg Br. 1996;21(6):723–734. doi: 10.1016/S0266-7681(96)80176-8. [DOI] [PubMed] [Google Scholar]
- 19.Kay SP, Wiberg M, Bellew M, Webb F. Toe to hand transfer in children. Part 2: functional and psychological aspects. J Hand Surg Br. 1996;21(6):735–745. doi: 10.1016/S0266-7681(96)80177-X. [DOI] [PubMed] [Google Scholar]
- 20.Lister G. Microsurgical transfer of the second toe for congenital deficiency of the thumb. Plast Reconstr Surg. 1988;82(4):658–665. doi: 10.1097/00006534-198810000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Manske PR, McCaroll HR., Jr Index finger pollicization for a congenitally absent or nonfunctioning thumb. J Hand Surg Am. 1985;10(5):606–613. doi: 10.1016/S0363-5023(85)80192-1. [DOI] [PubMed] [Google Scholar]
- 22.Manske PR, McCarroll HR, Jr, James M. Type III-A hypoplastic thumb. J Hand Surg Am. 1995;20(2):246–253. doi: 10.1016/S0363-5023(05)80018-8. [DOI] [PubMed] [Google Scholar]
- 23.May JW, Jr, Smith RJ, Peimer CA. Toe-to-hand free tissue transfer for thumb construction with multiple digit aplasia. Plast Reconstr Surg. 1981;67(2):205–213. [PubMed] [Google Scholar]
- 24.Meals RA, Lesavoy MA. Hallux-to-hand transfer during ankle disarticulation for multiple limb anomalies. JAMA. 1983;249(1):72–73. doi: 10.1001/jama.1983.03330250052028. [DOI] [PubMed] [Google Scholar]
- 25.Miyawaki T, Masuzawa G, Hirakawa M, Kurihara K. Bone-lengthening for symbrachydactyly of the hand with the technique of callus distraction. J Bone Joint Surg Am. 2002;84-A(6):986–991. doi: 10.2106/00004623-200206000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Morrison WA, O’Brien BM, MacLeod AM. Thumb reconstruction with a free neurovascular wrap-around flap from the big toe. J Hand Surg Am. 1980;5(6):575–583. doi: 10.1016/S0363-5023(80)80110-9. [DOI] [PubMed] [Google Scholar]
- 27.Nyárády J, Szekeres P, Vilmos Z. Toe-to-thumb transfer in congenital grade III thumb hypoplasia. J Hand Surg Am. 1983;8(6):898–901. doi: 10.1016/S0363-5023(83)80090-2. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien BM, Black MJ, Morrison WA, MacLeod AM. Microvascular great toe transfer for congenital absence of the thumb. Hand. 1978;10(2):113–124. doi: 10.1016/S0072-968X(78)80001-1. [DOI] [PubMed] [Google Scholar]
- 29.Radocha RF, Netscher D, Kleinert HE. Toe phalangeal grafts in congenital hand anomalies. J Hand Surg Am. 1993;18(5):833–841. doi: 10.1016/0363-5023(93)90050-D. [DOI] [PubMed] [Google Scholar]
- 30.Richardson PWF, Johnstone BR, Coombs CJ. Toe-to-hand transfer in symbrachydactyly. Hand Surg. 2004;9(1):11–18. doi: 10.1142/S0218810404001929. [DOI] [PubMed] [Google Scholar]
- 31.Shvedovchenko IV. Toe-to-hand transfers in children. Ann Plast Surg. 1993;31(3):251–254. doi: 10.1097/00000637-199309000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Spokevicius S, Radzevicius D. Late toe-to-hand transfer for the reconstruction of congenital defects of the long fingers. Scand J Plast Reconstr Surg Hand Surg. 1997;31(4):345–350. doi: 10.3109/02844319709008982. [DOI] [PubMed] [Google Scholar]
- 33.Swanson AB. A classification for congenital limb malformations. J Hand Surg Am. 1976;1(1):8–22. doi: 10.1016/S0363-5023(76)80021-4. [DOI] [PubMed] [Google Scholar]
- 34.Tu Y-K, Yeh W-L, Sananpanich K, et al. Microsurgical second toe-metatarsal bone transfer for reconstructing congenital radial deficiency with hypoplastic thumb. J Reconstr Microsurg. 2004;20(3):215–225. doi: 10.1055/s-2004-823109. [DOI] [PubMed] [Google Scholar]
- 35.Upton J, Mutimer K. A modification of the great-toe transfer for thumb reconstruction. Plast Reconstr Surg. 1988;82(3):535–538. doi: 10.1097/00006534-198809000-00033. [DOI] [PubMed] [Google Scholar]
- 36.Van Holder C, Giele H, Gilbert A. Double second toe transfer in congenital hand anomalies. J Hand Surg Br. 1999;24(4):471–475. doi: 10.1054/jhsb.1999.0162. [DOI] [PubMed] [Google Scholar]
- 37.Vilkki SK. Advances in microsurgical reconstruction of the congenitally adactylous hand. Clin Orthop Relat Res. 1995;314:45–58. [PubMed] [Google Scholar]
- 38.Wei FC, Chen HC, Chuang CC, Noordhoff MS. Reconstruction of the thumb with a trimmed-toe transfer technique. Plast Reconstr Surg. 1988;82(3):506–515. doi: 10.1097/00006534-198809000-00025. [DOI] [PubMed] [Google Scholar]
- 39.Wei FC, Colony LH, Chen HC, Chuang CC, Noordhoff MS. Combined second and third toe transfer. Plast Reconstr Surg. 1989;84(4):651–661. [PubMed] [Google Scholar]
- 40.Wei FC, el-Gammal TA, Chen HC, Chuang DC, Chiang YC, Chen SH. Toe-to-hand transfer for traumatic digital amputations in children and adolescents. Plast Reconstr Surg. 1997;100(3):605–609. doi: 10.1097/00006534-199709000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Yang DY. Thumb reconstruction by free second toe transplantation. Report of 40 cases. Clin J Surg (Chinese). 1977;15:13.
- 42.Yoshimura M. Toe-to-hand transfer. Plast Reconstr Surg. 1980;66(1):74–84. doi: 10.1097/00006534-198007000-00015. [DOI] [PubMed] [Google Scholar]