Abstract
Background
We evaluated the outcome of intraarticular middle phalanx fractures after dynamic treatment with the Ligamentotaxor® system.
Materials and methods
Ten consecutive patients (seven male, three female; mean age 52 years) with intraarticular middle phalanx fractures were treated with the Ligamentotaxor® between 2009 and 2011. Proximal interphalangeal joint mobility, grip strength and ‘Disabilities of the Arm, Shoulder and Hand’ (DASH) score were evaluated in a 15-month follow-up. The reconstitution of the intraarticular space was measured immediately after trauma, at 6 weeks and at 15 months by radiograph control. The severity of the trauma was classified according to AO.
Results
We found B1 30 %, C1 (Seno I + II) 50 % and C3 (Seno III–V) 20 %. In 60 % of the cases, fractures were localized on the middle base of the fifth digit, in 20 % on the third digit and in 20 % on the index finger. The dynamic treatment lasted 7 weeks; patients were exposed to full workload after 9 weeks. The mean flexion mobility after 15 months reached 73° (range 60–100°), and the extension deficit was 13° (range 0–20°) on average. Grip strength attained 71.3 % (range 60–87 %) of the contralateral side. Initial x-ray after trauma compared to the x-ray after 15 months showed an intraarticular space reconstitution average of 0.5 mm (range 0.1–0.9 mm) anterior–posterior and 0.6 mm (range 0.1–1 mm) lateral. Patients evaluated their outcome with an average of 14.6 points (range 3.3–26.7) using the DASH score.
Conclusion
Good results can be obtained with the Ligamentotaxor®. We recommend it for the dynamic treatment of intraarticular middle phalanx finger fractures. Larger series and long-term results are needed.
Keywords: Intraarticular middle phalanx fractures, Ligamentotaxor®, Pins and rubber traction system, PIP joint resurfacing, Dynamic fixator
Introduction
The treatment of intraarticular middle phalanx fractures is still challenging in hand surgery. Trauma often occurs perpendicular to the axis of the finger and is often associated with sports. Intraarticular middle phalanx fractures provide a poor prognosis for the range of motion of the injured joint due to the period of immobilisation following most osteosynthesis systems. The proximal interphalangeal joint makes up 40 % of the total finger flexion and is therefore biomechanically crucial for fist clenching and grip strength [5]. External fixators with the option of dynamic exercising during the healing period prevent ligamentous and tendinous adhesions. We established the Ligamentotaxor® from Arex, France, as a dynamic system in a series of ten patients who were followed up for 15 months (Fig. 1).
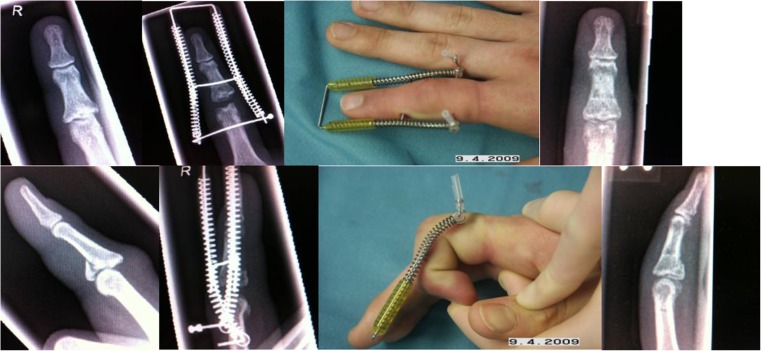
Fig. 1.
Case 1: trauma and Ligamentotaxor x-ray, dynamic treatment and x-ray at 6 weeks
Material and Methods
Our patients were mainly male candidates (m/f 7:3) and 52 years of age (range 28–79 years). The trauma occurred typically perpendicular to the axis of the finger and was often associated with sports. All fractures were classified by AO and Seno [10]. The operation was carried out by the same hand surgeon in all cases. The company delivered each Ligamentotaxor® set consisting of two k-wires, two springs, two pulleys and operating instructions. The drill target allows precise positioning under dynamic radiograph imaging. In all cases the period between the initial trauma and the operation was documented, and the duration between the Ligamentotaxor® treatment and postoperative physiotherapy was analysed. Our patients underwent x-ray at first consultation after trauma, at 6 weeks to evaluate consolidation and at 15 months to measure the intraarticular space compared to the initial finding. We used the computer program Chili/Web v1.30.2 (Chili GmbH, Digital Radiology, Germany) for analysis of the digital radiographs. The reconstitution of the intraarticular space was measured in millimetres and was taken as a quality marker for the joint surface. Proximal interphalangeal joint mobility and grip strength were evaluated with standardized devices (Baseline®, Fabrication Enterprises Inc., New York) and compared to the contralateral side. The mean follow-up period was 15 months after the operation. ‘Disabilities of the Arm, Shoulder and Hand’ (DASH) score was recorded (Figs. 2 and 3).
Fig. 2.
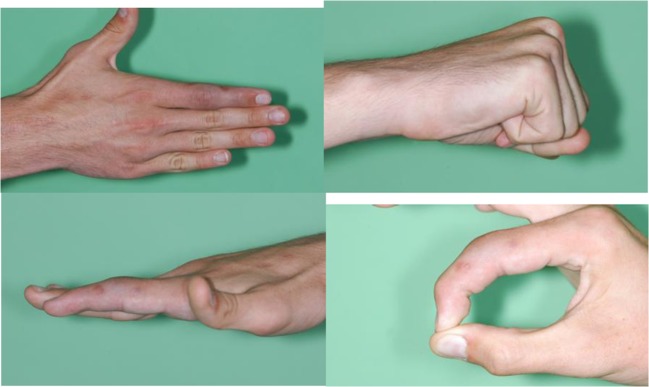
Case 1: clinical function at 2 years after trauma, PIP joint: 0–15–85°
Fig. 3.

Case 2: trauma x-ray, Ligamentotaxor, treatment result at 1 year, PIP joint: 0–30–85°
Results
We operated on 16 patients and had six dropouts from our initial collective because patients were not willing to take part in our study. Ten patients could be followed up as intended. The highest incidence of trauma occurred at the middle base of the fifth digit followed by the third and index fingers (Table 1). The severity of most fractures was classified with AO type C1 and Seno type I and II (Table 2).
Table 1.
Fracture localisation
| AO localisation: middle base | Percent |
|---|---|
| 722–digit II | 20 % |
| 732–digit III | 20 % |
| 752–digit V | 60 % |
Table 2.
Fracture classification
| AO classification | Seno classification | Percent |
|---|---|---|
| B1 | – | 30 % |
| C1 | Seno I + II | 50 % |
| C3 | Seno III–V | 20 % |
The mean period between the trauma and application of Ligamentotaxor® lasted 3.8 days; fractures were stabilized for 7 weeks, and patients started exercising 1 day after surgery. X-ray after 6 weeks showed improved fracture consolidation compared to the x-ray after 4 weeks so that the Ligamentotaxor® was removed after 7 weeks on average. After removal of the Ligamentotaxor®, patients underwent an average of 24 physiotherapy units and were exposed to full workload after 9 weeks. One patient happened to have a second trauma 2 weeks after the application of the Ligamentotaxor® and underwent an additional K-wire osteosynthesis. In this case the external fixator was left in place for 9 weeks in total. The final outcome 15 months after surgery showed a mean flexion mobility of 73° (range 60–100°) in the proximal interphalangeal joint and an extension deficit of 13° (range 0–20°) while the grip strength attained 71.3 % (range 60–87 %) of the contralateral side. Initial x-ray after impaction fracture showed an intraarticular space average of 0.6 mm (range 0–1.3 mm) anterior–posterior and 0.7 mm (range 0–1.6 mm) lateral; the posttreatment x-ray at 15 months showed a reconstituted mean intraarticular space of 1.1 mm (range 0.8–1.6 mm) anterior–posterior and 1.3 mm (range 0.9–1.7) lateral. Patients evaluated their outcome with an average of 14.6 points (range 3.3–26.7) using the DASH score (Table 3).
Table 3.
Table of all measures and results
| Measure | Patients | Average result |
|---|---|---|
| Trauma until Ligamentotaxor | N = 10 | 3.8 days |
| Ligamentotaxor treatment period | N = 10 | 7 weeks |
| Physiotherapy | N = 10 | 24 units |
| Full workload | N = 10 | 9 weeks |
| AROM (extension–neutral–flexion) | N = 10 | 0–13–73° |
| Active flexion range | N = 10 | 60–100° |
| Active extension range | N = 10 | 0–20° |
| PROM (extension–neutral–flexion) | N = 10 | 0–10–80° |
| Grip strength | N = 10 | 71.3 % of the contralateral hand |
| Grip strength range | N = 10 | 60–87 % of the contralateral hand |
| Intraarticular space at trauma x-ray | N = 10 | 0.6 mm anterior–posterior |
| N = 10 | 0.7 mm lateral | |
| Intraarticular space posttreatment | N = 10 | 1.1 mm anterior–posterior |
| N = 10 | 1.3 mm lateral | |
| DASH score | N = 10 | 14.6 |
| DASH score range | N = 10 | 3.3–26.7 |
Discussion
Intraarticular middle phalanx fractures are severe injuries of the finger with high incidences of irreversible sequelae due to ligamentous and tendinous adhesions during the immobility period [1]. Conservative treatment of intraarticular middle phalanx fractures can lead to satisfying bone consolidation while permanent fracture reduction is not guaranteed, and periarticular adhesions are unavoidable [11]. The Ligamentotaxor® allows immediate postoperative exercising throughout the bone healing period. This is a key function in preventing oedema, adhesions and proximal interphalangeal joint stiffness. The central principle of the Ligamentotaxor® is to achieve joint reshaping via early motion with minimal stress for the fracture site [7]. The device is delivered with drill templates which allow precise positioning of each k-wire through radiolucent target holes. Postoperative assessment of the radiograph control used to be difficult since the Ligamentotaxor® springs were radiodense. By turning the facture site through dynamic radiograph imaging, the base of the middle phalanx could yet be displayed. Radiograph control has improved since Arex offers radiolucent springs with full view on the fracture site in the lateral plane. We appreciate precise positioning of the k-wires as well as exact spring adjustment in the aftercare with the Arex system. An alternative well-established fixator is the ‘pins and rubber traction system’, PRTS, described by Suzuki. It is convenient because no additional equipment is needed besides standard k-wires and orthodontic rubber bands, and it is cheap and easy to install [12]. Yet positioning and adjustment of the device is less precise, and the outcome is much more dependent on the skill of the surgeon in charge [2]. Different authors published their outcome with the PRTS with an average flexion mobility of the proximal interphalangeal (PIP) joint of 64–85° [3, 4, 6, 8]. Follow-up periods diverged between 10 and 26 months after PRTS osteosynthesis. Secondary fracture dislocation with the PRTS is described by Syed in 2 out of 8 and by Morgan in 5 out of 14 cases (Morgan, 1995, #14; Syed, 2003, #13). This could not be observed in our Ligamentotaxor® group but is described by Körting et al. in 1 out of 15 patients treated with Ligamentotaxor® [7]. An interesting aspect of any dynamic fixator system is the long-term improvement of flexion mobility found 8 years after PRTS use. Mean flexion mobility increased from 64° to 74° after this period [9]. This phenomenon can be explained by the remodelling capacity of the PIP joint surface resulting from early exercising. Using dynamic fixator systems, Richter et al. describe that secondary arthrosis is not seen in the long term [9]. Any dynamic treatment of intraarticular middle phalanx fractures has become the method of choice in modern hand surgery. Employing the benefit of anatomical ligamentotaxis, dynamic fixator systems have a key function in the reconstitution of the PIP joint. Other authors like Körting et al. report of similar encouraging outcomes using the Ligamentotaxor: grip strength of 85.7 % compared to the contralateral hand, AROM 0–19–76°, and DASH score 17 after 10 months follow-up [7]. We appreciate precise positioning of the k-wires as well as exact spring adjustment in the aftercare with the Arex system and recommend it for the dynamic treatment of intraarticular middle phalanx fractures. Larger series and long-term results are needed.
Acknowledgments
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for inclusion in the study.
Conflict of Interest
All the authors declare that they have no conflict of interest.
References
- 1.Bayer-Sandow T, Bruser P. The dynamic treatment of intraarticular fractures of the base of the middle phalanx with the Suzuki dynamic fixator. Handchir Mikrochir Plast Chir. 2001;33(4):267–270. doi: 10.1055/s-2001-16594. [DOI] [PubMed] [Google Scholar]
- 2.Debus G, Courvoisier A, Wimsey S, Pradel P, Moutet F. Pins and rubber traction system for intra-articular proximal interphalangeal joint fractures revisited. J Hand Surg Eur. 2010;35(5):396–401. doi: 10.1177/1753193409359493. [DOI] [PubMed] [Google Scholar]
- 3.Deshmukh SC, Kumar D, Mathur K, Thomas B. Complex fracture-dislocation of the proximal interphalangeal joint of the hand. Results of a modified pins and rubbers traction system. J Bone Joint Surg Br. 2004;86(3):406–412. doi: 10.1302/0301-620X.86B3.14350. [DOI] [PubMed] [Google Scholar]
- 4.Duteille F, Pasquier P, Lim A, Dautel G. Treatment of complex interphalangeal joint fractures with dynamic external traction: a series of 20 cases. Plast Reconstr Surg. 2003;111(5):1623–1629. doi: 10.1097/01.PRS.0000054160.46502.D0. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg E, Unglaub F, Kneser U, Horch RE. Intraarticular fractures of the proximal interphalangeal joint: dynamic early functional therapy with an external fixation system. Unfallchirurg. 2009;112(3):337–345. doi: 10.1007/s00113-008-1553-2. [DOI] [PubMed] [Google Scholar]
- 6.Keramidas E, Solomos M, Page RE, Miller G. The Suzuki frame for complex intra-articular fractures of the proximal interphalangeal joint of the fingers. Ann Plast Surg. 2007;58(5):484–488. doi: 10.1097/01.sap.0000244975.89885.c7. [DOI] [PubMed] [Google Scholar]
- 7.Korting O, Facca S, Diaconu M, Liverneaux P. Treatment of complex proximal interphalangeal joint fractures using a new dynamic external fixator: 15 cases. Chir Main. 2009;28(3):153–157. doi: 10.1016/j.main.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Majumder S, Peck F, Watson JS, Lees VC. Lessons learned from the management of complex intra-articular fractures at the base of the middle phalanges of fingers. J Hand Surg (Br) 2003;28(6):559–565. doi: 10.1016/S0266-7681(03)00139-6. [DOI] [PubMed] [Google Scholar]
- 9.Richter M, Bruser P. Long-term follow-up of fracture dislocations and comminuted fractures of the PIP joint treated with Suzuki's pin and rubber traction system. Handchir Mikrochir Plast Chir. 2008;40(5):330–335. doi: 10.1055/s-2008-1038450. [DOI] [PubMed] [Google Scholar]
- 10.Seno N, Hashizume H, Inoue H, Imatani J, Morito Y. Fractures of the base of the middle phalanx of the finger. Classification, management and long-term results. J Bone Joint Surg Br. 1997;79(5):758–763. doi: 10.1302/0301-620X.79B5.7664. [DOI] [PubMed] [Google Scholar]
- 11.Stern PJ, Roman RJ, Kiefhaber TR, McDonough JJ. Pilon fractures of the proximal interphalangeal joint. J Hand Surg [Am] 1991;16(5):844–850. doi: 10.1016/S0363-5023(10)80147-9. [DOI] [PubMed] [Google Scholar]
- 12.Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg (Br) 1994;19(1):98–107. doi: 10.1016/0266-7681(94)90059-0. [DOI] [PubMed] [Google Scholar]