Abstract
Background
Dorsal plate and screw fixation is a popular choice for metacarpal stabilization. The balance between construct stability and soft tissue dissection remains a surgical dilemma. Historically, six cortices of bone fixation on either side of a fracture were deemed necessary. This study aims to elucidate whether four cortices of locked fixation on either side of the fracture is equivalent to the current gold standard of six cortices of nonlocked fixation on either side of the fracture. If so, less dissection to insert shorter plates with fewer screws could be used to stably fix these fractures.
Methods
With biomechanical testing-grade composite Sawbones, a comminuted metacarpal fracture model was used to test two fixation constructs consisting of a standard dorsal plate and either six bicortical nonlocking screws (three screws per segment) or four bicortical locking screws (two screws per segment). Thirty specimens were tested to failure in cantilever bending and torsion.
Results
There was statistical equivalence between the locking and nonlocking constructs in cantilever bending stiffness, torsional stiffness, maximum bending load, and maximum torque.
Conclusion
The tested metacarpal fracture model had equivalent biomechanical properties when fixed with a standard dorsal plate and either six bicortical nonlocking screws or four bicortical locking screws. By utilizing fewer cortices of fixation, there will be less dissection and less soft tissue stripping during fixation of metacarpal fractures. This will also be of benefit in very proximal or distal fractures as multiple cortices of fixation are often difficult to obtain during stabilization of these challenging fractures.
Keywords: Metacarpal, Fracture fixation, Biomechanics, Cortices of fixation, Locked versus nonlocked, Screws, Fracture, Plating
Introduction
Metacarpal fractures are a common presenting problem to the hand surgeon. The majority of these fractures are closed, simple, and minimally displaced leading to successful nonoperative treatment. Surgical stabilization is often chosen for unstable, open, irreducible, or high-energy injuries with extensive soft tissue stripping [10]. When performing surgery on these fractures, attention to reduction is important. A biomechanical cadaveric study shows that as much as 8 % loss of grip power may result from every 2 mm of metacarpal shortening [19]. A few degrees of malrotation may lead to digital overlap when a fist is made [10, 21, 25]. Although numerous techniques and implants have been proposed for internal fixation of metacarpal fractures, no standard method exists [1, 9, 14, 22, 24, 31, 32]. Dorsal plate and screw fixation remains a popular choice, with such constructs providing superior biomechanical strength compared to other methods, including intramedullary Kirschner wires (K-wires), crossed K-wires, and simple lag screws [8, 9, 18, 30]. Locking plate technology is now also being utilized in open reduction and internal fixation of metacarpal fractures, although its ultimate role remains unclear [11, 20, 26].
Traditionally, it has been recommended that long bone fractures treated surgically with a plate construct should be fixed with three nonlocking screws placed both proximal and distal to the fracture [27]. More recently, however, it has been shown in certain long bone fractures that fewer screws placed strategically provide similar fixation strength and clinical outcomes [15, 17]. The optimal plate and screw construct for metacarpal fractures still remains unclear. The plate design, number of screws, and number of cortices per segment continue to be a topic of debate for metacarpal fracture fixation. Although traditional AO technique recommends a dorsal plate with six cortices of fixation on either side of the fracture, locked plates and/or fewer cortices of screw fixation may provide similar strength while allowing for less soft tissue disruption and related complications. Furthermore, many metacarpal fractures do not allow for six cortices of fixation on either side with standard plates due to the proximal or distal nature of the fracture pattern.
The purpose of this biomechanical study is to help elucidate the optimal number of cortices needed when using locked and nonlocked dorsal plate and screw constructs for metacarpal fracture fixation.
Materials and Methods
Sixty fourth-generation composite left long finger metacarpal Sawbones (Pacific Research Laboratories, Inc., Vashon, WA, USA) were cut using a custom jig, creating uniform 3-mm diaphyseal fracture gaps. This model has been used previously to simulate comminuted metacarpal fractures [12]. The specimens were then fixed with a seven-hole 2.0-mm LCP stainless steel straight plate (Synthes, West Chester, PA, USA) and either six bicortical nonlocking screws or four bicortical locking screws. A total of four groups were assigned based on fixation mode (locking screws versus nonlocking screws) and loading configuration (cantilever bending or torsion). Groups 1 and 3 were plated with six bicortical nonlocking screws, three on either side of the fracture. Groups 2 and 4 were plated with four bicortical locking screws, two on either side of the fracture. All screws were placed in the plate holes closest to the fracture site. Screw lengths were chosen to assure complete purchase of the far cortex.
A power analysis for equivalence identified 30 samples necessary for bending testing and torsion testing: group 1 (n = 15), nonlocked bending; group 2 (n = 15), locked bending; group 3 (n = 15), nonlocked torsion; group 4 (n = 15), locked torsion.
Mechanical testing was conducted on an Instron ElectroPuls E10000 (Instron Corporation, Norwood, MA, USA). For cantilever bending testing (groups 1 and 2), the proximal end of each specimen was rigidly held in a custom fixture with molded polymethylmethacrylate (PMMA) clamps (Fig. 1). Following preloading to 1 N, a perpendicular load was applied on the dorsal side of the specimen 53 mm from the fixed end at a rate of 10 mm/min until failure. The loading position was centered between the distal aspect of the plate and the end of the metacarpal. The loading rate was similar to that used in previous metacarpal plating studies [11, 28]. Bending stiffness, maximum load, and failure location were determined for each specimen. Bending stiffness was calculated from the linear portion of the load versus deflection curve.
Fig. 1.
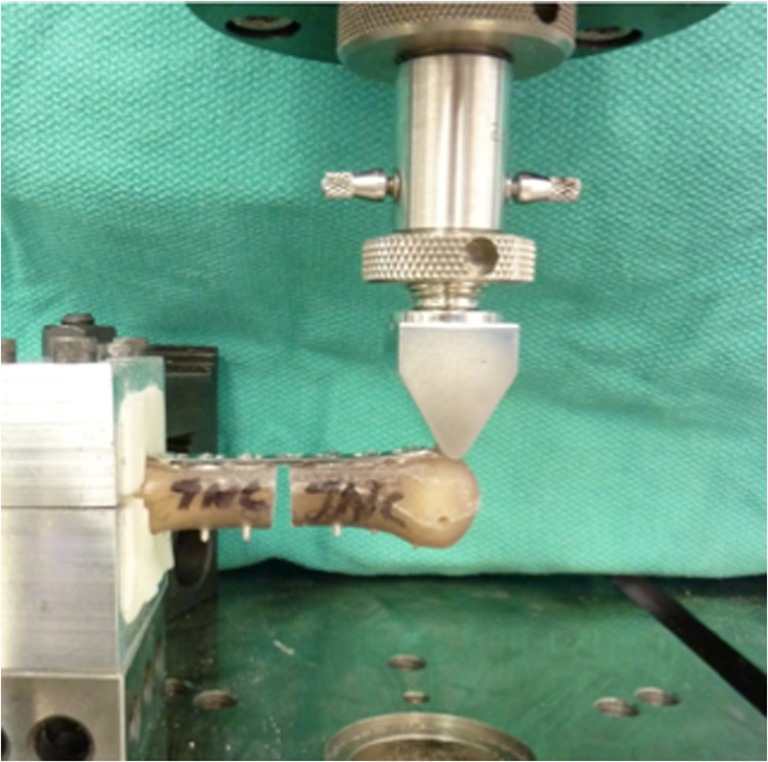
Setup for cantilever bending testing. The specimen represents a locking construct with four cortices of fixation per segment
For torsion testing (groups 3 and 4), specimens were held at each end in molded PMMA clamps (Fig. 2). The length between clamped ends was 53 mm. During testing, the direction of rotation was clockwise relative to the proximal segment. Specimens were rotated at 2°/s until maximum torque to failure or until a maximum angular displacement of 90° was reached. Stiffness and maximum torque were recorded for each specimen. The linear portion of the torque versus angular deflection curve was used to determine torsional stiffness.
Fig. 2.
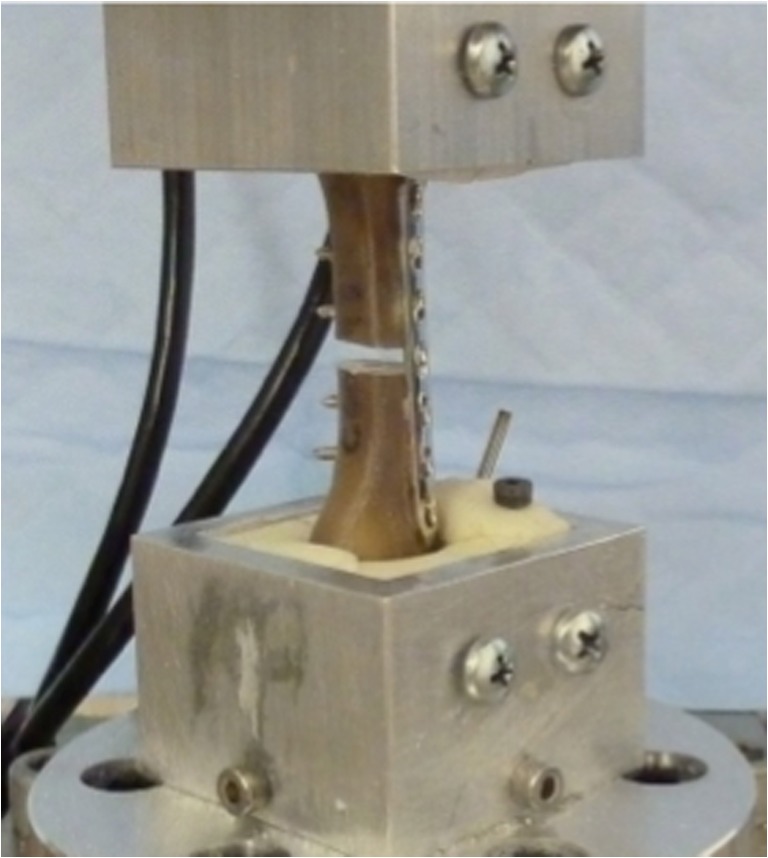
Setup for torsion testing. The specimen represents a locking construct with four cortices of fixation per segment
Means and standard deviations for bending stiffness, maximum bending, torsional stiffness, and maximum torque were calculated for the groups. Comparisons between the two constructs were carried out with a two-tailed t test with significance set at alpha = 0.05. If no statistical difference was found, we tested the hypothesis that the groups were equivalent using a 10 % difference as the threshold for equivalence. The equivalence hypotheses were evaluated with a two one-sided test (TOST) procedure and by constructing confidence intervals for the differences between the means. Significance was set at p < 0.05.
Results
All constructs undergoing cantilever bending testing failed with fracture through the bone (Fig. 3). Of the nonlocked bending specimens (group 1), 93 % (14/15) broke at the proximal screw hole furthest from the applied force. Of the locked bending specimens (group 2), 73 % (11/15) broke at the proximal bone–cement interface, and the remainder broke at the proximal screw hole. There were no cases of plate failure or screw pullout with bending testing. None of the nonlocked or locked specimens undergoing torsion testing (groups 3 and 4) were fractured through bone, but each exhibited a plateauing of torque near the 90° end point defined in the test and a large degree of permanent deformation of the plate (Fig. 4).
Fig. 3.
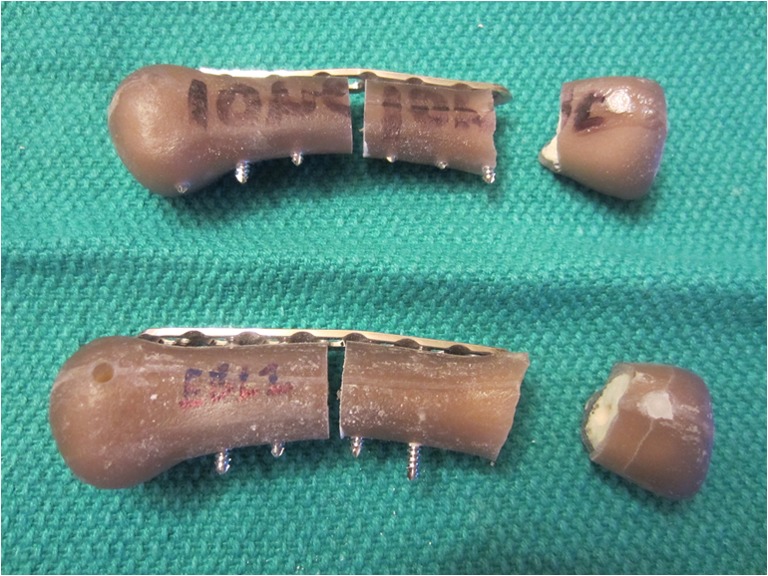
Failure of nonlocked (top) and locked (bottom) specimens in cantilever bending. The nonlocked specimen failed at the proximal screw hole and the locked specimen failed at the bone-cement interface
Fig. 4.
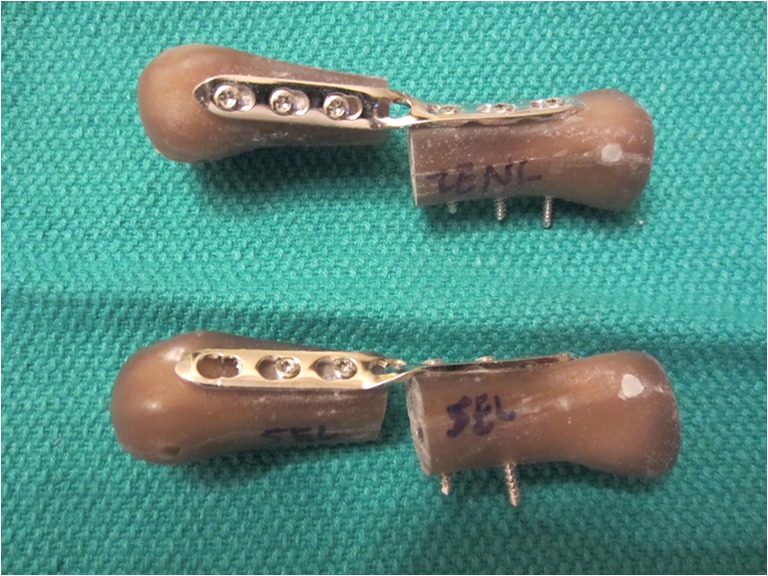
Failure of nonlocked (top) and locked (bottom) specimens in torsion. Both exhibited a plateauing of torque near the 90° end point with permanent deformation of the plate
There was no statistically significant difference (p > 0.05) between the two constructs in any of the mechanical tests (Table 1). Equivalence testing was carried forward for each comparison.
Table 1.
Results of cantilever bending and torsion tests for locked and nonlocked groups (mean ± SD)
| Construct | Bending stiffness (N/mm)*° | Maximum bending load (N)*° | Torsional stiffness (Nmm/deg)*° | Maximum torque (Nmm)*° |
|---|---|---|---|---|
| Locked, 4 cortices/segment | 5.4 ± 0.7 | 184 ± 27 | 69.6 ± 9.3 | 1,858 ± 161 |
| Nonlocked, 6 cortices/segment | 5.5 ± 0.5 | 185 ± 22 | 68.6 ± 7.9 | 1,862 ± 196 |
*p > 0.05, no statistical significant difference; °p < 0.05, statistical equivalence
The bending stiffness in groups 1 (nonlocked) and 2 (locked) were 5.5 ± 0.5 and 5.4 ± 0.7 N/mm, respectively. These values were statistically equivalent (p = 0.03). The maximum bending load in group 1 (185 ± 22 N) and group 2 (184 ± 27 N) also reached statistical equivalence (p = 0.03).
The torsional stiffness in groups 3 (nonlocked) and 4 (locked) were 68.6 ± 7.9 and 69.6 ± 9.3 Nmm/deg, respectively. This reached statistical equivalence (p = 0.04). The maximum torque in group 3 (1,862 ± 196 Nmm) and group 4 (1,858 ± 161 Nmm) also reached statistical equivalence (p = 0.004).
Discussion
Metacarpal fractures are often amenable to nonoperative management. However, for those that require surgical fixation, such as comminuted diaphyseal fractures, dorsal plate constructs have been shown to offer superior stability [8, 9, 18, 30]. Although results are frequently satisfactory, complications such as adhesions, finger stiffness, tendon irritation, tendon rupture, and need for hardware removal are not uncommon [7, 29]. There is an inherent balance surgeons face between providing adequate stability and minimizing soft tissue disruption during plating of a metacarpal fracture.
The results of this study show equivalent bending stiffness, torsional stiffness, maximum bending load, and maximum torque between metacarpal fractures fixed using a dorsal plate with either (1) three bicortical nonlocking screws (six cortices of fixation) or (2) two bicortical locking screws (four cortices of fixation) on either side of the fracture. If biomechanical properties are similar between the two constructs, it therefore may be advantageous to use fewer screws with a smaller plate, thereby requiring less dissection and disruption of the surrounding soft tissues. Furthermore, it is often not feasible to place three screws on either side of a fracture if the fracture is too proximal or distal along the metacarpal.
Using a porcine metacarpal model, Ochman et al. [20] compared the stiffness and load to failure of 2.3-mm straight titanium plates fixed with four nonlocking screws or four locking screws (two on either side of the fracture). Although the locking construct using unicortical screws was found to be stronger than the nonlocking construct using unicortical screws, there was no significant difference between locking and nonlocking constructs when using bicortical fixation. Our study did not intend to confirm again that locking constructs were no different than nonlocking constructs with similar screw number and cortical purchase. Rather, we wanted to compare two commonly used fixation constructs that can pose an intraoperative dilemma. We hope to add to the Ochman study and, more importantly, provide surgeons the information that a shorter locking construct is equivalent to a longer nonlocking construct. To our knowledge, there has been no previous study comparing the biomechanical strength of metacarpal fractures fixed with dorsal plates using either six nonlocking screws or four locking screws, nor was construct equivalence detected in any of the previous studies.
Correlation of the results to in vivo measures may be made. For example, the average values for both constructs in maximum bending load were several magnitudes greater than forces normally generated across metacarpals in vivo. The average bending moment of an intact metacarpal during maximum flexion is 0.35 Nm [30]. The values obtained during our testing are over 20 times greater, and it is unlikely that such high loads would ever be reached during a normal postoperative period. It is also important to note that increasing construct rigidity is not without clinical concerns. A more recent view of locking plate technology shows an environment that is too stiff to reliably promote bone healing if there is not sufficient compression and bony contact at the time of plate application. Recent studies suggest that locked plate constructs suppress interfragmentary motion to a level that is insufficient to promote healing, especially at the cortex adjacent to the plate [3, 12].
Although unicortical screw fixation is often used clinically with locking plate technology, bicortical screw fixation was chosen for both the nonlocking and locking plates in this study in order to eliminate an additional variable. Furthermore, it is still not fully clear when to use unicortical or bicortical screw fixation with locking plates in long bone fractures [2, 5, 6, 13]. Gautier and Sommer [13] recommend at least two locking screws per main fragment with purchase of at least three cortices for simple fractures and at least two locking screws per main fragment with purchase of at least four cortices for comminuted fractures.
Fewer than three screws per segment have been tested in other long bone fracture models. Lindvall and Sagi [17] followed 75 diaphyseal forearm fractures treated with open reduction internal fixation with a plate and a total of four bicortical screws (two on either side of the fracture). At an average of 14 months follow up, there were no refractures and no infections and only one nonunion; these results are similar to forearm fractures treated with six bicortical screws. Hak et al. [15] compared the biomechanical behavior of two versus three locking screws per bone segment in a humerus fracture model and found that the addition of a third screw did not add to the stability in axial loading, bending, or torsion.
The purpose of our study was not necessarily to compare screw type (locking versus nonlocking) as this has already been studied in the metacarpal [20]. Rather, we intended to add biomechanical data behind two specific and commonly used plating techniques, with the goal of assisting with intraoperative decision-making. This was achieved by not only performing a superiority trial, but more importantly an equivalence study, which is often an underappreciated distinction and strength of this study [16]. Based on this study, there is biomechanical data to support using either of the tested plate and screw constructs.
This study is not without its limitations. First, a sawbone model was used in place of cadaveric specimens. It is has been shown, however, that sawbones provide a consistent test medium incorporating cortical and cancellous bone surrogates with mechanical and structural properties in the range of normal human bone. Cadaver specimens would have required significantly more samples to account for variation in mechanical properties and geometry among specimens of differing age, bone density, etc. Second, the multiple in vivo forces experienced by a metacarpal are difficult to replicate in a laboratory setting. We chose unidirectional forces that we felt were most relevant. Previous authors have highlighted that the predominant force across the metacarpal is apex dorsal bending given the stronger force of the flexor tendons compared to the extensor tendons [4, 23]. In cantilever bending tests, the bending moment increases linearly from zero at the point of load application to a maximum at the fixed end of the specimen. The most proximal screw in the nonlocking model is located farther away from the loading point than the most proximal screw in the locking model. Consequently, the nonlocked model is subjected to a higher moment at the screw (stress riser) location. Because the specimens will fail at the location of highest stress, nonlocked specimens typically failed at the most proximal screw hole, while the locked specimens failed either at the most proximal screw hole (location of the stress riser) or the fixed end (location of highest moment) of the specimen. The cantilever bending test is only an approximation of physiologic loading, and it should be recognized that the failure locations observed in this study cannot be extrapolated to the estimates of expected failure locations observed in clinical practice. For this reason, the bending stiffness is a more reliable indication of construct stability than maximum bending load. Third, although cyclical loading would better mimic in vivo failure, our methods test the properties of the initial stability of the construct following surgery when no healing has occurred. Finally, we chose to use the same length plate for both arms of the study. Although we could have used a smaller plate for the locking construct, it is important to note that the section of the plate extending beyond the outermost screw holes employed during fixation does not contribute to the mechanical response of the plate under the loading protocols used in the study. The loaded portion of the plate is determined by the locations of the most proximal and distal screw holes used.
In conclusion, this study shows biomechanical equivalence between simulated comminuted metacarpal fractures fixed using a dorsal plate with either (1) three nonlocking screws (six cortices of fixation) or (2) two locking screws (four cortices of fixation) on either side of the fracture. With the use of fewer screws, there is an opportunity for less soft tissue disruption and possibly fewer postoperative complications. Further studies will be necessary to correlate the findings of this biomechanical study with clinical outcomes.
Acknowledgments
We wish to thank Alex HS Harris, PhD, for his assistance with the statistical design and analysis. We wish to thank Synthes for providing the plates and screws used in this study.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Statement of Informed Consent
There were no patients in this study.
Conflict of Interest
The authors declare that they have no conflicts of interest, commercial associations, or intent of financial gain regarding this research.
References
- 1.Bach HG, Gonzalez MH, Hall RF. Locked intramedullary nailing of metacarpal fractures secondary to gunshot wounds. J Hand Surg [Am] 2006;31A(7):1083–1087. doi: 10.1016/j.jhsa.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Bottlang M, Doornink J, Fitzpatrick DC, et al. Far cortical locking can reduce stiffness of locked plating constructs while retaining construct strength. J Bone Joint Surg Am. 2009;91(8):1985–1994. doi: 10.2106/JBJS.H.01038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bottlang M, Doornink J, Lujan TJ, Fitzpatrick DC, Marsh JL, Augat P, et al. Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92(2):12–22. doi: 10.2106/JBJS.J.00780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dona E, Gillies RM, Gianoutsos MP, et al. Plating of metacarpal fractures: unicortical or bicortical screws? J Hand Surg (Br) 2004;29(3):218–221. doi: 10.1016/j.jhsb.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Dougherty PJ, Kim D, Meisterling S, et al. Biomechanical comparison of bicortical versus unicortical screw placement of proximal tibia locking plates: a cadaveric study. J Orthop Trauma. 2008;22(6):399–403. doi: 10.1097/BOT.0b013e318178417e. [DOI] [PubMed] [Google Scholar]
- 6.Egol KA, Kubiak EN, Fulkerson E, et al. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18(8):488–493. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Fambrough RA, Green DP. Tendon rupture as a complication of screw fixation in fractures in the hand. A case report. J Bone Joint Surg Am. 1979;61(5):781–782. [PubMed] [Google Scholar]
- 8.Firoozbakhsh KK, Moneim MS, Doherty W, et al. Internal fixation of oblique metacarpal fractures. A biomechanical evaluation by impact loading. Clin Orthop. 1996;325:296–301. doi: 10.1097/00003086-199604000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Firoozbakhsh KK, Moneim MS, Howey T, et al. Comparative fatigue strengths and stabilities of metacarpal internal fixation techniques. J Hand Surg [Am] 1993;18(6):1059–1068. doi: 10.1016/0363-5023(93)90403-P. [DOI] [PubMed] [Google Scholar]
- 10.Freeland AE, Orbay JL. Extraarticular hand fractures in adults: a review of new developments. Clin Orthop. 2006;445:133–145. doi: 10.1097/01.blo.0000205888.04200.c5. [DOI] [PubMed] [Google Scholar]
- 11.Gajendran VK, Szabo RM, Myo GK, et al. Biomechanical comparison of double-row locking plates versus single- and double-row non-locking plates in a comminuted metacarpal fracture model. J Hand Surg [Am] 2009;34(10):1851–1858. doi: 10.1016/j.jhsa.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Gardner MJ, Nork SE, Huber P, Krieg JC. Stiffness modulation of locking plate constructs using near cortical slotted holes: a preliminary study. J Orthop Trauma. 2009;23:281–287. doi: 10.1097/BOT.0b013e31819df775. [DOI] [PubMed] [Google Scholar]
- 13.Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–B76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez MH, Igram CM, Hall RF., Jr Flexible intramedullary nailing for metacarpal fractures. J Hand Surg [Am] 1995;20(3):382–387. doi: 10.1016/S0363-5023(05)80091-7. [DOI] [PubMed] [Google Scholar]
- 15.Hak DJ, Althausen P, Hazelwood SJ. Locked plate fixation of osteoporotic humeral shaft fractures: are two locking screws per segment enough? J Orthop Trauma. 2010;24(4):207–211. doi: 10.1097/BOT.0b013e3181bdd1da. [DOI] [PubMed] [Google Scholar]
- 16.Harris AH, Fernandes-Taylor S, Giori N. “Not statistically different” does not necessarily mean “the same”: the important but underappreciated distinction between difference and equivalence studies. J Bone Joint Surg Am. 2012;94(5):e29 1–4. [DOI] [PubMed]
- 17.Lindvall EM, Sagi HC. Selective screw placement in forearm compression plating: results of 75 consecutive fractures stabilized with 4 cortices of screw fixation on either side of the fracture. J Orthop Trauma. 2006;20(3):157–162. doi: 10.1097/00005131-200603000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Mann RJ, Black D, Constine R, et al. A quantitative comparison of metacarpal fracture stability with five different methods of internal fixation. J Hand Surg [Am] 1985;10(6 Pt 2):1024–1028. doi: 10.1016/S0363-5023(85)80029-0. [DOI] [PubMed] [Google Scholar]
- 19.Meunier MJ, Hentzen E, Ryan M, et al. Predicted effects of metacarpal shortening on interosseous muscle function. J Hand Surg [Am] 2004;29(4):689–693. doi: 10.1016/j.jhsa.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Ochman S, Doht S, Paletta J, et al. Comparison between locking and non-locking plates for fixation of metacarpal fractures in an animal model. J Hand Surg [Am] 2010;35(4):597–603. doi: 10.1016/j.jhsa.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 21.Opgrande JD, Westphal SA. Fractures of the hand. Orthop Clin North Am. 1983;14(4):779–792. [PubMed] [Google Scholar]
- 22.Orbay J. Intramedullary nailing of metacarpal shaft fractures. Tech Hand Up Extrem Surg. 2005;9(2):69–73. doi: 10.1097/01.bth.0000167253.31976.95. [DOI] [PubMed] [Google Scholar]
- 23.Prevel CD, Eppley BL, Jackson JR, et al. Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical study. J Hand Surg [Am] 1995;20(1):44–49. doi: 10.1016/S0363-5023(05)80057-7. [DOI] [PubMed] [Google Scholar]
- 24.Prevel CD, McCarty M, Katona T, et al. Comparative biomechanical stability of titanium bone fixation systems in metacarpal fractures. Ann Plast Surg. 1995;35(1):6–14. doi: 10.1097/00000637-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Royle SG. Rotational deformity following metacarpal fracture. J Hand Surg (Br) 1990;15(1):124–125. doi: 10.1016/0266-7681(90)90068-F. [DOI] [PubMed] [Google Scholar]
- 26.Ruchelsman DE, Mudgal CS, Jupiter JB. The role of locking technology in the hand. Hand Clin. 2010;26(3):307–319. doi: 10.1016/j.hcl.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Ruedi TP, Murphy WM. AO principles of fracture management. New York: Thieme; 2000. [Google Scholar]
- 28.Sohn RC, Jahng KH, Curtiss SB, et al. Comparison of metacarpal plating methods. J Hand Surg [Am] 2008;33(3):316–321. doi: 10.1016/j.jhsa.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop. 1987;214:59–65. [PubMed] [Google Scholar]
- 30.Vanik RK, Weber RC, Matloub HS, et al. The comparative strengths of internal fixation techniques. J Hand Surg [Am] 1984;9(2):216–221. doi: 10.1016/S0363-5023(84)80145-8. [DOI] [PubMed] [Google Scholar]
- 31.Waris E, Ashammakhi N, Happonen H, et al. Bioabsorbable miniplating versus metallic fixation for metacarpal fractures. Clin Orthop. 2003;410:310–319. doi: 10.1097/01.blo.0000063789.32430.c6. [DOI] [PubMed] [Google Scholar]
- 32.Waris E, Ashammakhi N, Raatikainen T, et al. Self-reinforced bioabsorbable versus metallic fixation systems for metacarpal and phalangeal fractures: a biomechanical study. J Hand Surg [Am] 2002;27(5):902–909. doi: 10.1053/jhsu.2002.35082. [DOI] [PubMed] [Google Scholar]


