Abstract
Objective:
Depression is one of the most common psychiatric disorders in the world. Lifetime prevalence is 15% among men and 25% among women. Selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants and monoamine oxidase inhibitor antidepressants are often used for depression, with their own side effects. This study was carried out since little information on sexual dysfunction due to these medications is available in Iran.
Methods:
This observational cross-sectional study included 100 patients attending a university or private psychiatry clinic who, after an interview based on Diagnostic and Statistical Manual of Mental Disorders fourth edition criteria, were considered depressed. These patients had no history of depression, sexual dysfunction or use of psychiatric medications. Sexual functioning of patients was evaluated at the start of the study, and after 2, 4 and 8 weeks of treatment. Data were evaluated using SPSS software and t and χ2 tests.
Results:
A total of 75% of patients reported sexual dysfunction: 66.7% of men and 79.7% of women. A total of 74.1% of patients on fluvoxamine, 100% on fluoxetine, 75% on sertraline, 71.4% on citalopram and 100% on paroxetine reported sexual dysfunction. The most frequent sexual dysfunction was difficulty with orgasm, which affected 41.17% of women and 33.33% of men.
Conclusion:
The incidence of sexual dysfunction among users of SSRIs was highest in patients on fluvoxamine, but this was not statistically significant. Minimization of sexual side effects should be an essential consideration when prescribing antidepressants.
Keywords: depression, selective serotonin reuptake inhibitors, sexual dysfunction
Introduction
Depression is among the most common psychiatric disorders across the world, including in Iran. Lifetime prevalence of depression is 15% for men and 25% for women. Depression is among the most common causes of disability. Every year many people have depression and difficulty with their economic and social activities, and expenditure for treating depression is also significant [Rafii and Sobhanian, 2003].
Depression has been cited in many old stories, such as the story of King Saul and the story of suicide by Ajax in Homer’s The Iliad. About 450 years BC, Hippocrates used the terms mania and melancholia to describe psychiatric conditions. Furthermore, 100 years BC, Cornelius Celsus described depression as a consequence of black bile.
At times, diagnosis of psychiatric disease can be difficult in general practice, particularly if physical symptoms are also present. Antidepressants are the most common treatment modality for depression. Among them, selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are commonly prescribed and have some side effects. Almost all antidepressants can cause sexual dysfunction and the prevalence of this side effect is over 90% [Harvey and Balon, 1995].
Mitchell and Popkin believe that opinions vary regarding sexual dysfunction in men due to antidepressants. One reason for this difference is a lack of clear understanding of sexual dysfunction caused by depression itself. Mitchell and Popkin showed that difficulty with arousal, ejaculation and change in sexual interest after antidepressant use have been reported by patients, although no related cases of priapism have been noted [Mitchell and Popkin, 1983].
The sexual experience can broadly be divided into three stages: stage 1, interest and desire (libido); stage 2, physiologic arousal; and stage 3, orgasm. Neurotransmitters and hormones are believed to influence SSRI-associated sexual dysfunction. Dopamine, serotonin [5-hydroxytryptamine (5HT)], testosterone and oestrogen all have an influence on sexual interest and desire (libido). Nitric oxide, acetylcholine and 5HT are important modulators of physiological sexual arousal. Finally, norepinephrine and 5HT play important roles in orgasm. Recent evidence suggests that additional neurotransmitters such as glutamate may also be involved in sexual physiology [Perlis et al. 2009].
Among the antidepressants, SSRIs cause delayed ejaculation and interfere with orgasm [Arjmand and Sadeghi, 2005]. Precise statistics are not available but difficulty with orgasm has been reported in 15–50% of men and women in most studies. Sexual dysfunction with use of MAOI and TCA drugs were first reported in the 1960s. With the introduction of new antidepressants in the 1980s and 1990s, these reports have increased in number. Patients on SSRIs have reported more problems than those taking TCA medications and other antidepressants. SSRIs may have a negative effect on one or all stages of sexual functioning, difficulty with ejaculation or delayed orgasm, but delayed ejaculation or orgasm are the most commonly reported side effects [Baonm, 2006].
One of the obstacles that make it difficult to evaluate the prevalence of sexual dysfunction in relation to antidepressants is that patients who have psychiatric disorders are more likely to have sexual dysfunction due to the effect of their illness on their behaviour and relationships [Corretti et al. 2006].
In one study, the prevalence of sexual dysfunction in relation to antidepressant use (SSRIs and others) in England and France was estimated at 39% and 27%, respectively [Williams et al. 2006]. Some other research has shown that up to 60% of patients who use SSRIs have sexual problems [Zajecka et al. 1997].
Since many patients discontinue SSRIs due to their impact on sexual function, developing strategies to predict who may be at highest risk of adverse changes in their wellbeing is an important step in improving the quality of life and treatment of patients who require antidepressant therapy. Therefore, continued efforts to characterize the relationships between genetic markers and antidepressant outcomes and to translate this knowledge into patient care have the potential to significantly improve the empiric selection of antidepressant agents and to minimize the risk of intolerable side effects [Osis and Bishop, 2010].
Since little information on these side effects is available in Iran, this study was designed to obtain more information. Patients were interviewed by a psychoneurologist about any sexual dysfunction and the information was recorded.
Materials and methods
This was an observational cross-sectional study. Patients presenting to the neuropsychology clinic at the university hospital or specialist clinics in the city of Lorestan from March 2011 to March 2012 who were diagnosed with depression after clinical evaluation based on Diagnostic and Statistical Manual of Mental Disorders fourth edition text revision (DSM-IV-TR) criteria, who gave informed consent to participate and were taking antidepressant medication were included. Patients with a previous history of psychotropic medication use, psychiatric conditions or sexual dysfunction were excluded.
All patients were re-evaluated after 2, 4 and 8 weeks of treatment initiation. At each visit, the evaluation was carried out by a neuropsychologist and all four parts of sexual functioning were assessed and any change recorded.
Data were entered into the computer and analysed using SPSS software and presented in the form of distribution tables. Correlations were assessed using t and χ2 tests.
Results
Patients included in the study were between 18 and 50 years of age. Most were in the age range of 28–37 years (44 patients, 44%).
The mean age of patients was 31.11 ± 7.48 years and the mean age of patients with sexual dysfunction was 31.33 ± 7.80 years. A total of 23% of patients in the age range 18–27 years and 33% of patients in the age range 28–37 years had sexual dysfunction. In addition, 19% of patients in the age range 38–50 years developed sexual dysfunction. Sexual dysfunction was most prevalent in the age range 28–37 (33%) (Figure 1).
Figure 1.
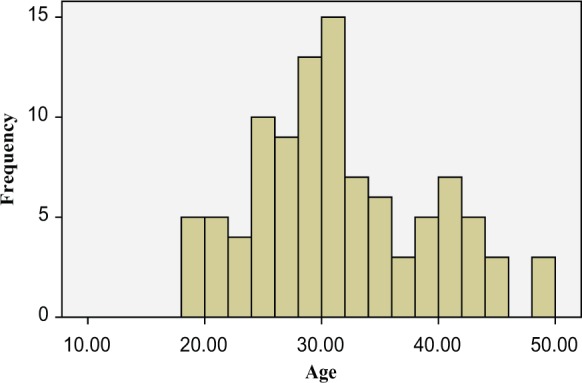
Distribution of sexual dysfunction based on age.
A total of 36% of patients were men, of which 24 (66.7%) reported sexual dysfunction. Of the remaining 64% female patients were women, 51 (79.7%) developed dysfunction. There was no significant difference noted in the incidence of sexual dysfunction between men and women (p = 0.16) (Table 1).
Table 1.
Distribution of sexual dysfunction based on sex.
| Sex | Sexual dysfunction |
|||||
|---|---|---|---|---|---|---|
| Yes |
No |
Total |
||||
| N | % | N | % | N | % | |
| Men | 24 | 66.7 | 12 | 33.3 | 36 | 100 |
| Women | 51 | 79.7 | 13 | 20.3 | 64 | 100 |
p = 0.16, χ2 = 2.08.
A total of 91% were married and 9% were single. Highest completed education levels were as follows: 8% had completed primary school education; 23% had completed junior high school education; 51% had a high-school diploma; and 18% were university graduates, as shown in Figure 2.
Figure 2.
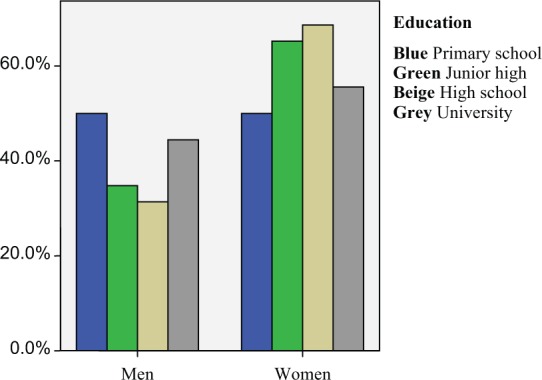
Distribution of sexual dysfunction based on education and sex.
The SSRI medication used was fluvoxamine in 58%, fluoxetine in 4%, sertraline in 16%, citalopram in 21% and paroxetine in 1% (Figure 3).
Figure 3.
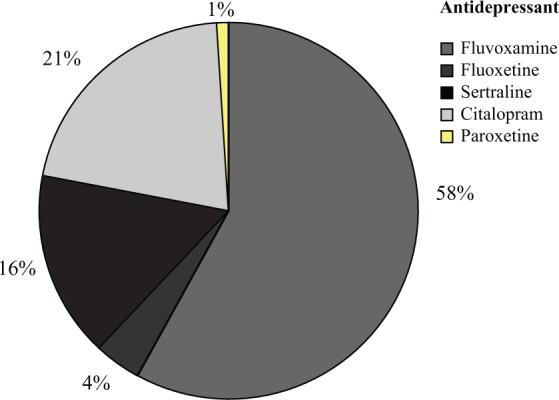
Distribution of sexual dysfunction based on kind of antidepressant.
The results of t and χ2 tests showed that 15% had decreased sex drive, 1% had decreased arousal, 29% had difficulty with orgasm, 9% had combined decreased desire and arousal, 3% had combined decreased desire and difficulty with orgasm, 10% had decreased arousal and difficulty with orgasm, and 8% had decreased desire, difficulty with orgasm and arousal (Table 2).
Table 2.
Distribution of patients taking selective serotonin reuptake inhibitors based on kind of sexual dysfunction.
| Kind of dysfunction | N | % |
|---|---|---|
| None | 25 | 25 |
| Decreased desire | 15 | 15 |
| Decreased arousal | 1 | 1 |
| Difficulty with orgasm | 29 | 29 |
| Decreased desire and arousal | 9 | 9 |
| Decreased desire and difficulty with orgasm | 3 | 3 |
| Decreased arousal and difficulty with orgasm | 10 | 10 |
| Dysfunction in three stages | 8 | 8 |
| Total | 100 | 100 |
Sexual dysfunction based on age involved decreased desire in 5 patients between 18 and 27 years of age (21.74%) and 11 (47.82%) had difficulty with orgasm. Two patients (27.8%) developed decreased desire and arousal, two (8.7%) had decreased desire and difficulty with orgasm and one (4.3%) had decreased arousal and difficulty with orgasm.
In patients in the age range 28–37 years, 8 (24.24%) had decreased desire, 1 (3.53%) had decreased arousal, 10 (30.3%) had difficulty with orgasm, 6 (18.18%) had decreased desire and arousal together and 6 (18.18%) had both decreased arousal and difficulty with orgasm.
In the age range 38–50 years, 2 patients (10.52%) had decreased desire, 8 (42.10%) had difficulty with orgasm, 1 (5.26%) had decreased arousal and desire together, 1 (5.26%) had decreased desire and difficulty with orgasm and 3 (15.78%) had both decreased arousal and difficulty with orgasm. Women had the most difficulty with orgasm (41.1%) and the highest percentage of sexual dysfunction in men was related to decreased desire (20.8%). A large proportion of 18–27-year-old patients (47.8%) had difficulty with orgasm and the prevalence of dysfunction in three stages was the lowest among patients aged 38–50 years (1.05%).
Among the 24 men, 29.18% had decreased appetite, 20.83% had decreased desire, 33.33% had difficulty with orgasm, none had decreased arousal and 16.66% had dysfunction in all three stages. Among the 51 women, 29.43% had decreased appetite, 19.6% had decreased desire, 1.96% had decreased arousal, 41.17% had difficulty with orgasm and the remaining 7.84% had dysfunction in all three stages.
Based on the medication used, of 58 patients on fluvoxamine, 43 (74.1%) developed sexual dysfunction, and of 4 patients taking fluoxetine, all reported sexual dysfunction. Among 16 patients taking sertraline, 12 (75%) developed sexual dysfunction. In addition, of 21 patients taking citalopram, 15 (71.4%) had dysfunction; 1 patient who took paroxetine also developed dysfunction. Statistically significant correlations between sexual dysfunction and the type of drug was not found (p = 0.77) (Table 3). Of 43 patients on fluvoxamine, 2 (4.65%) had decreased desire, 24 (55.81%) had difficulty with orgasm, none had decreased arousal, 4 (9.3%) developed decreased desire and arousal at the same time, 2 (4.65%) had decreased desire and difficulty with orgasm and 6 (13.95%) had decreased arousal and difficulty with orgasm.
Table 3.
Distribution of patients with one or more sexual dysfunction based on sex.
| Sex | Sexual dysfunction |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Decreased desire |
Decreased arousal |
Difficulty with orgasm |
Decreased desire and arousal |
Decreased desire and difficulty with orgasm |
Decreased arousal and difficulty with orgasm |
Three dysfunctions |
||||||||
| No | % | No | % | No | % | No | % | No | % | No | % | No | % | |
| Men | 5 | 20.8 | 0 | 0 | 8 | 33.3 | 4 | 16.6 | 1 | 4.2 | 2 | 8.3 | 4 | 16.6 |
| Women | 10 | 19.6 | 1 | 1.96 | 21 | 41.1 | 5 | 9.8 | 2 | 3.9 | 8 | 15.7 | 4 | 7.8 |
Of 4 patients taking fluoxetine, all developed decreased desire. Of 12 patients on sertraline, 3 (25%) had decreased desire, 4 (33.33%) had difficulty with orgasm, 3 (25%) had both decreased desire and arousal and 1 (8.33%) had decreased arousal and difficulty with orgasm. Of 15 patients taking citalopram, 6 (40%) had decreased desire, 1 (6.66%) had difficulty with orgasm, 2 (13.33%) had decreased desire and arousal, 1 (6.66%) had difficulty with orgasm and 3 (20%) had decreased arousal and difficulty with orgasm at the same time. In addition, one person on paroxetine developed decreased arousal (Table 4).
Table 4.
Distribution of patients with sexual dysfunction based on kind of antidepressant.
| Antidepressant | Sexual dysfunction |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Decreased desire |
Decreased arousal |
Difficulty with orgasm |
Decreased desire and arousal |
Decreased desire and difficulty with orgasm |
Decreased arousal and difficulty with orgasm |
Three dysfunctions |
||||||||
| No | % | No | % | No | % | No | % | No | % | No | % | No | % | |
| Fluvoxamine | 2 | 4.65 | 0 | 0 | 24 | 55.8 | 4 | 9.3 | 2 | 4.65 | 6 | 13.9 | 5 | 11.62 |
| Fluoxetine | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sertraline | 3 | 25 | 0 | 0 | 4 | 33.3 | 3 | 0.25 | 0 | 0 | 1 | 8.3 | 1 | 8.3 |
| Citalopram | 6 | 40 | 0 | 0 | 1 | 6.6 | 2 | 13.3 | 1 | 6.66 | 3 | 20 | 2 | 12.3 |
| Paroxetine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| Total | 15 | 15 | 1 | 1 | 29 | 29 | 9 | 9 | 3 | 3 | 10 | 10 | 30 | 30 |
Discussion and conclusion
Because information on sexual dysfunction due to SSRI use is lacking in Iran, this study was designed to gain more knowledge.
A total of 100 patients were included in this study. These patients presented to the neuropsychology clinic at the university or private specialty clinics and were diagnosed with depression after an interview with a psychologist based on DSM-IV-TR criteria. These patients were being treated with SSRIs. Of these 100 patients, 75 (75%) developed sexual dysfunction and 25 (25%) had no similar complaints. A study by Steffany and colleagues in 2003 also showed that the incidence of sexual dysfunction after SSRI use is about 30–70% greater than with after the use of other antidepressants [Steffany et al. 2003].
Our study agrees with findings from similar studies that, after SSRI use, women complain more about sexual dysfunction than men. A study by Montejo and colleagues in 1996 showed that men have increased incidence of sexual dysfunction compared with women but the degree of dysfunction is more prominent in women. They showed that decreased desire and difficulty with orgasm is more common in men and difficulty with arousal is more common in women [Montejo et al. 1996].
In another study by Clyton and colleagues in 2006, the results showed that 95.6% of women and 97.9% of men showed dysfunction at least in one phase of sexual functioning. Compared with women, men had more significant dysfunction with desire and orgasm and less significant dysfunction with arousal. However, sexual dysfunction in different stages did not significantly differ among men and women, which is also what we found in our study [Clyton et al. 2006].
Based on the kind of antidepressant, the prevalence of sexual dysfunction due to SSRIs was greatest in fluvoxamine, followed by citalopram, sertraline, fluoxetine and paroxetine. Fluvoxamine caused dysfunction mostly with orgasm, citalopram with desire, fluoxetine with desire, sertraline with orgasm and paroxetine with arousal. Paroxetine is considered more commonly associated with delayed orgasm, ejaculation and sexual dysfunction compared with fluvoxamine and fluoxetine and sertraline (p < 0.05).
In a study by Montejo and Liorca covering the period 1986–2000, 30–60% of patients treated with SSRIs developed sexual dysfunction, particularly noted when direct questioning was performed (more than 70%) [Hirschfeld, 2003]. This study showed that sexual dysfunction occurred in 57.7% of patients on fluoxetine, 70.7% on paroxetine, 62.9% on sertraline, 62.3% on fluvoxamine, 72.7% on citalopram, 67.3% on venlafaxine, 24.4% on mirtazapine and 8% on nefazodone. Incidence of sexual dysfunction in men was 62.4% compared with 56.9% in women [Montejo and Liorca, 2001].
In another study by Fiona and Lee in 1999, sexual dysfunction associated with SSRIs was reported in 2–57% of participants. In men, complaints included decreased desire, delayed ejaculation, difficulty or lack of orgasm, and in women complaints decreased desire and difficulty with orgasm [Fiona and Lee, 1999].
In the study by Steffany and colleagues in 2003, sexual dysfunction was reported to be a common side effect resulting from antidepressant use, particularly SSRIs. Bupropion and nefazodone, unlike other medications, showed decreased sexual dysfunction [Steffany et al. 2003].
Sexual dysfunction due to medical treatment was studied in 1022 outpatients (610 women and 412 men) with a mean age of 39.8 ± 11.3 years. A questionnaire covering sexual desire, orgasm, ejaculation, arousal and sexual satisfaction was administered. Prevalence with medication use was reported as 59.1% [Montejo et al. 1996].
SSRIs differ in their side effects, with paroxetine causing more delayed orgasm and ejaculation and sexual dysfunction compared with fluvoxamine, fluoxetine and sertraline (p < 0.05). Only 22.6% of patients had no complaints of sexual dysfunction. Men had a higher rate of dysfunction while women had a higher degree of dysfunction [Montejo et al. 1996].
In a study by Clyton, it was showed that 50–70% and even as high as 90% patients who had take SSRIs developed sexual dysfunction [Clyton et al. 2006].
In multiple double-blind studies, sexual dysfunction caused by sertraline has been compared with placebo and other antidepressants. Nefazodone and bupropion did not have a negative influence on sexual functioning, but 67% of patients on sertraline had difficulty with arousal; 10% also had this problem before treatment. In addition, in a group of women who did not have problems before treatment, 41% developed difficulty with orgasm using sertraline (Wirsch and Birnbaum, 2008).
Another related study was performed by Clyton and colleagues in 2006. Sexual dysfunction was assessed in patients with depression without prior history of treatment with SSRIs. A total of 6297 adult outpatients on single antidepressant drug therapy were evaluated for sexual functioning using a questionnaire. The results showed that 95.6% of women and 97.9% of men had dysfunction at least in one phase of sexual functioning. Men compared with women had significantly more decreased desire and difficulty with orgasm and significantly less dysfunction with arousal. The prevalence of sexual dysfunction in different stages due to SSRIs was not statistically different between men and women [Clyton et al. 2006].
In a study by Hu and colleagues conducted in the period 15 December 1999 to 31 May 2000, patients on SSRIs for depression or recently started on these drugs were interviewed by telephone 75–105 days after medication initiation. Patients were requested to note any of 17 side effects arising from SSRI use. Of 401 patients who were followed up by telephone, 344 (86%) had one side effect and 219 (55%) noted more than one side effect. The most common side effect was sexual dysfunction and drowsiness (17%). Side effects occurred mostly in the first 2 weeks of treatment, and 82% of respondents complained of sexual dysfunction [Hu et al. 2004].
Our study was performed according to current ethical standards. Patients were reassured that their personal information would be protected, and data would be evaluated and reported for the whole study population.
According to the DSM-IV-TR, decreased sexual desire may itself be among the symptoms noted by patients with depression. As a result, this should be differentiated from sexual dysfunction and decreased desire due to medication side effects. As noted in the DSM-IV-TR, sexual dysfunction as a side effect of medication use presents as difficulty with stages of sexual functioning (desire, arousal, orgasm, relaxation) or pain with intercourse. In addition, side effects increase during the first month of medication use [Baonm, 2006].
Sexual side effects from SSRI antidepressants are common, persistent and vary in intensity and presentation among patients. Initial studies characterizing the contribution of genetic variability and SSRI-associated changes in sexual function provide important insights into the potential for pharmacogenetic information to influence drug selection for depression and other disorders treated with SSRIs. While requiring further mechanistic clarification and replication, variants in serotonin genes (HTR2A and SLA64A), a gene interacting with the serotonin system (BDNF) as well as glutamate system genes (GRIK2, GIRA3 and GRIA1) appear to be associated with SSRI-associated sexual dysfunction. In some cases, the nature of these relationships appears to differ in men and women, as well as the domain of sexual function studied. The importance of study design and methods of assessing sexual function are important and heterogeneity in these aspects across studies makes direct comparison of results across investigations difficult [Osis and Bishop, 2010].
One study has shown that the 5HT2 antagonist trazodone may be beneficial in the management of SSRI-induced sexual dysfunction. It has also been suggested that improvement in sexual function and overall clinical improvement (depression, anxiety) occur. Specific differences in men and women were improvement in erectile performance in men and lubrication in women. No correlations were noted between clinical improvement of depression or anxiety and improvement in sexual dysfunction [Stryjer et al. 2009].
Suggestions
Suggestions for practitioners include the following:
Question patients directly about sexual dysfunction.
Since sexual functioning is physiological, if side effects occur, change in treatment modality, medication counselling and other counselling, and patient education is recommended.
When prescribing medication, drugs with the fewest sexual side effects should be considered.
Sexual dysfunction in married couples can influence family relations and psychiatric treatment is recommended.
Acknowledgments
The authors of this article are grateful to their coworkers at Lorestan University of Medical Sciences for their help with this study.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
Contributor Information
Mitra Safa, Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Saeid Sadr, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Firouzeh Talischi, Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Fatemeh Ghasem Boroujerdi, Clinical Tuberculosis and Epidemiology Research Center, NRITLD, Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Darabad Street, Niavaran Street, Tehran, Iran.
References
- Arjmand M., Sadeghi M. (2006) Oxford Psychiatry, 1st edn (translation of the 2005. English original by Geddes, Goodman and Meyers). Tehran: Arjmand Publishers [Google Scholar]
- Baonm R. (2006) SSRI-associated sexual dysfunction. Am J Psychiatry 163: 1504–1509 [DOI] [PubMed] [Google Scholar]
- Clyton A., Keller A., McGrvey E. (2006) Burden of phase-specific sexual dysfunction with SSRIs. J Affect Disorder 91: 27–32 [DOI] [PubMed] [Google Scholar]
- Corretti G., Pierucci S., De Scisciolo M., Nisita C.(2006) Comorbidity between social phobia and premature ejaculation: study on 242 males affected by sexual disorders. J Sex Marital Ther 32: 183–187 [DOI] [PubMed] [Google Scholar]
- Fiona M, Lee A. (1999) Drug-induced sexual dysfunction and infertility. Pharm J 29: 780–784 [Google Scholar]
- Harvey K., Balon R. (1995) Clinical implications of antidepressant drug effects on sexual function. Ann Clin Psychiatry 7: 189–201 [DOI] [PubMed] [Google Scholar]
- Hirschfeld R. (2003) Long term side effects of SSRIs: sexual dysfunction and weight gain. J Clin Psychiatry 64(Suppl.): 20–24 [PubMed] [Google Scholar]
- Hu X., Bull S., Hunkeler E., Ming E., Lee J., Fireman B., et al. (2004) Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression. J Clin Psychiatry 65: 959–965 [DOI] [PubMed] [Google Scholar]
- Mitchell J., Popkin M. (1983) Antidepressant drug therapy and sexual dysfunction in men: a review. J Clin Psychopharmacol 3: 76–79 [PubMed] [Google Scholar]
- Montejo A., Liorca G. (2001) Incidence of sexual dysfunction associated with antidepressant agents. J Clin Psychiatry 62(Suppl. 3): 10–21 [PubMed] [Google Scholar]
- Montejo A., Liorca G., Izquierdo J., Ledesma A., Bousono M., Calcedo A., et al. (1996) Sexual dysfunction secondary to SSRIs a comparative analysis in 308 patients. Actas Luso ESP Neurol Psiquiatr Cienc Afines 24: 311–321 [PubMed] [Google Scholar]
- Osis L., Bishop J. (2010) Pharmacogenetics of SSRIs and sexual dysfunction. Pharmaceuticals 3: 3614–3628 [Google Scholar]
- Perlis R., Laje G., Smoller J., Fava M., Rush A., McMahon F. (2009) Genetic and clinical predictors of sexual dysfunction in citalopram-treated depressed patients. Neuropsychopharmacology 34: 1819–1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafii H., Sobhanian K. (2003) Synopsis of Psychiatry/Clinical Psychiatry, 1st edn Tehran: Arjmand Publishers [Google Scholar]
- Steffany J., Fredman M., Jerrold F., Rosenbaum M. (2003) Antidepressant induced sexual dysfunction and its management. In: Proceedings of the American Psychiatric Association 156th Annual Meeting, San Francisco, CA, 17–22 May 2003 [Google Scholar]
- Stryjer R., Spivak B., Strous R., Shiloh R., Harary E., Polak L., et al. (2009) Trazodone for the treatment of sexual dysfunction induced by serotonin reuptake inhibitors: a preliminary open-label study. Clin Neuropharmacol 32: 82–84 [DOI] [PubMed] [Google Scholar]
- Williams V., Baldwin D., Hogue S., Fehnel S., Hollis K., Edin H. (2006) Estimating the prevalence and impact of antidepressant-induced sexual dysfunction in 2 European countries: a cross-sectional patient survey. J Clin Psychiatry 67: 204–210 [DOI] [PubMed] [Google Scholar]
- Wirsch M., Birnbaum R. (2008) Sexual dysfunction associated with selective serotonin reuptake inhibitor (SSRI) antidepressant. Available at: http://www.uptodate.com/contents/
- Zajecka J., Mitchell S., Fawcett J. (1997) Treatment-emergent changes in sexual function with selective serotonin reuptake inhibitors as measured with the Rush Sexual Inventory. Psychopharmacol Bull 33: 755–760 [PubMed] [Google Scholar]


