Abstract
This study examined the ability of the HRindex model to accurately predict maximal oxygen uptake ( O2max) across a variety of incremental exercise protocols. Ten men completed five incremental protocols to volitional exhaustion. Protocols included three treadmill (Bruce, UCLA running, Wellness Fitness Initiative [WFI]), one cycle, and one field (shuttle) test. The HRindex prediction equation (METs = 6 × HRindex − 5, where HRindex = HRmax/HRrest) was used to generate estimates of energy expenditure, which were converted to body mass-specific estimates of
O2max) across a variety of incremental exercise protocols. Ten men completed five incremental protocols to volitional exhaustion. Protocols included three treadmill (Bruce, UCLA running, Wellness Fitness Initiative [WFI]), one cycle, and one field (shuttle) test. The HRindex prediction equation (METs = 6 × HRindex − 5, where HRindex = HRmax/HRrest) was used to generate estimates of energy expenditure, which were converted to body mass-specific estimates of  O2max. Estimated
O2max. Estimated  O2max was compared with measured
O2max was compared with measured  O2max. Across all protocols, the HRindex model significantly underestimated
O2max. Across all protocols, the HRindex model significantly underestimated  O2max by 5.1 mL·kg−1·min−1 (95% CI: −7.4, −2.7) and the standard error of the estimate (SEE) was 6.7 mL·kg−1·min−1. Accuracy of the model was protocol-dependent, with
O2max by 5.1 mL·kg−1·min−1 (95% CI: −7.4, −2.7) and the standard error of the estimate (SEE) was 6.7 mL·kg−1·min−1. Accuracy of the model was protocol-dependent, with  O2max significantly underestimated for the Bruce and WFI protocols but not the UCLA, Cycle, or Shuttle protocols. Although no significant differences in
O2max significantly underestimated for the Bruce and WFI protocols but not the UCLA, Cycle, or Shuttle protocols. Although no significant differences in  O2max estimates were identified for these three protocols, predictive accuracy among them was not high, with root mean squared errors and SEEs ranging from 7.6 to 10.3 mL·kg−1·min−1 and from 4.5 to 8.0 mL·kg−1·min−1, respectively. Correlations between measured and predicted
O2max estimates were identified for these three protocols, predictive accuracy among them was not high, with root mean squared errors and SEEs ranging from 7.6 to 10.3 mL·kg−1·min−1 and from 4.5 to 8.0 mL·kg−1·min−1, respectively. Correlations between measured and predicted  O2max were between 0.27 and 0.53. Individual prediction errors indicated that prediction accuracy varied considerably within protocols and among participants. In conclusion, across various protocols the HRindex model significantly underestimated
O2max were between 0.27 and 0.53. Individual prediction errors indicated that prediction accuracy varied considerably within protocols and among participants. In conclusion, across various protocols the HRindex model significantly underestimated  O2max in a group of aerobically fit young men. Estimates generated using the model did not differ from measured
O2max in a group of aerobically fit young men. Estimates generated using the model did not differ from measured  O2max for three of the five protocols studied; nevertheless, some individual prediction errors were large. The lack of precision among estimates may limit the utility of the HRindex model; however, further investigation to establish the model's predictive accuracy is warranted.
O2max for three of the five protocols studied; nevertheless, some individual prediction errors were large. The lack of precision among estimates may limit the utility of the HRindex model; however, further investigation to establish the model's predictive accuracy is warranted.
Keywords: Cardiorespiratory fitness, exercise testing, prediction equation, resting heart rate
Introduction
High cardiorespiratory fitness (CRF) is associated with health benefits, a lower risk of all-cause mortality, (Blair et al. 1989; Kodama et al. 2009; Lee et al. 2011) and a high physical work capacity (Astrand 1956; Balke and Ware 1959). CRF is assessed for diagnostic and prognostic objectives, the evaluation of fitness, the development of exercise prescriptions, and the appraisal of training programs; hence the assessment of CRF is of interest to researchers and clinicians alike. Maximal oxygen uptake ( O2max) is considered the criterion measure of CRF (American College of Sports Medicine [ACSM] 2006). Direct measurement of
O2max) is considered the criterion measure of CRF (American College of Sports Medicine [ACSM] 2006). Direct measurement of  O2max, however, requires expensive laboratory equipment, trained personnel, and does not lend itself to testing large numbers of individuals; therefore,
O2max, however, requires expensive laboratory equipment, trained personnel, and does not lend itself to testing large numbers of individuals; therefore,  O2max is often estimated indirectly rather than measured.
O2max is often estimated indirectly rather than measured.
Estimates of  O2max obtained using maximal exercise protocols are typically based on a performance measure such as time or distance covered (Balke and Ware 1959; Cooper 1968; Bruce et al. 1973; Cureton et al. 1995) or in cycle ergometry, peak work rate (Storer et al. 1990). Alternatively, prediction models employing submaximal exercise tests, generally base predictions on the heart rate (HR) response and its well-established linear relationship with oxygen uptake (
O2max obtained using maximal exercise protocols are typically based on a performance measure such as time or distance covered (Balke and Ware 1959; Cooper 1968; Bruce et al. 1973; Cureton et al. 1995) or in cycle ergometry, peak work rate (Storer et al. 1990). Alternatively, prediction models employing submaximal exercise tests, generally base predictions on the heart rate (HR) response and its well-established linear relationship with oxygen uptake ( O2) over a wide range of exercise intensities (Astrand and Ryhming 1954; Asmussen and Hemmingsen 1958; Margaria et al. 1965). However, it is equally well known that the use of a submaximal HR response to estimate
O2) over a wide range of exercise intensities (Astrand and Ryhming 1954; Asmussen and Hemmingsen 1958; Margaria et al. 1965). However, it is equally well known that the use of a submaximal HR response to estimate  O2 involves assumptions that do not always hold true, such as a uniform age-related maximal heart rate (HRmax) and the linearity of the HR and
O2 involves assumptions that do not always hold true, such as a uniform age-related maximal heart rate (HRmax) and the linearity of the HR and  O2 relationship (Davies et al. 1984; Shephard 1984).
O2 relationship (Davies et al. 1984; Shephard 1984).
Recently, Wicks et al. (2011) conducted a retrospective analysis of data extracted from 60 published studies and investigated the relationship between various HR measures and oxygen uptake. The authors concluded that the prediction model employing the ratio of HR during exercise (HRabsolute) to resting HR (HRrest), which was termed the HRindex, was the preferred model and could be used to predict submaximal and maximal  O2. Furthermore, the researchers indicated that the HRindex method was independent of testing mode (e.g., treadmill, cycle, free-range-activity) and accounted for factors known to contribute to variability in
O2. Furthermore, the researchers indicated that the HRindex method was independent of testing mode (e.g., treadmill, cycle, free-range-activity) and accounted for factors known to contribute to variability in  O2max, including age, sex, fitness, and body mass.
O2max, including age, sex, fitness, and body mass.
A prediction model that accurately predicts  O2max independent of protocol from readily obtained variables would be an attractive tool for field, laboratory, and clinical settings. Wicks et al. (2011) recently reported that their HRindex prediction equation could accurately predict
O2max independent of protocol from readily obtained variables would be an attractive tool for field, laboratory, and clinical settings. Wicks et al. (2011) recently reported that their HRindex prediction equation could accurately predict  O2max. Therefore, the purpose of this exploratory study was to examine the validity of the HRindex prediction equation proposed by Wicks et al. (2011) in predicting
O2max. Therefore, the purpose of this exploratory study was to examine the validity of the HRindex prediction equation proposed by Wicks et al. (2011) in predicting  O2max in healthy, active subjects performing a variety of maximal incremental protocols.
O2max in healthy, active subjects performing a variety of maximal incremental protocols.
Methods
Experimental design
This retrospective study utilized data from a parent study that examined the effects of exercise protocol and mode on cardiovascular and metabolic responses to graded exercise testing. These data were further analyzed to investigate the accuracy of the HRindex model for predicting  O2max. The parent study employed a within-subjects repeated measures design in which participants completed five different incremental exercise tests to volitional exhaustion. Incremental tests were presented in a randomized order and completed on different days. Experimental trials were completed at the same time of day and separated by at least 48 h; all trials were completed within a 14-day period. Participants were instructed to stay well hydrated and to maintain their current diet and exercise patterns throughout the data collection period.
O2max. The parent study employed a within-subjects repeated measures design in which participants completed five different incremental exercise tests to volitional exhaustion. Incremental tests were presented in a randomized order and completed on different days. Experimental trials were completed at the same time of day and separated by at least 48 h; all trials were completed within a 14-day period. Participants were instructed to stay well hydrated and to maintain their current diet and exercise patterns throughout the data collection period.
Participants
Ten healthy, physically active, college-aged men were recruited from the campus community. Individuals were given a detailed account of the study and all participants provided written informed consent prior to the initiation of study procedures. All participants completed a medical history and received a medical evaluation from a health care provider prior to participation in the study. Exclusion criteria included diagnosed cardiorespiratory diseases, use of medication known to alter HR or metabolic rate, or orthopedic problems that interfered with performance of the tests. The study was approved by the college's Institutional Review Board.
Experimental trial
Participants fasted and abstained from caffeine and nicotine in the 4 h preceding the test and abstained from strenuous exercise and alcohol within 24 h of testing. Hydration status was assessed via urine specific gravity (Schueco Clinical Refractometer 5711-2020; Erma Inc, Tokyo, Japan) to ensure that participants were tested in a euhydrated state (USG ≤ 1.020) (Sawka et al. 2007). Height was measured prior to the first experimental trial using a stadiometer (Seca, Hanover, MD; accuracy ± 0.01 m). Body mass was measured prior to each experimental trial (Befour Inc., Saukville, WI; accuracy ± 0.1 kg). All participants had previous experience completing graded exercise tests to volitional exhaustion; details for each protocol were provided prior to each incremental test. Resting measurements were obtained in a thermoneutral laboratory (21.6 ± 1.2°C; 48.1 ± 6.8% relative humidity) before the incremental test. Participants were outfitted with a portable metabolic measurement system and HR monitor and were instructed to sit quietly for a 10-min period while resting HR and  O2 data were collected.
O2 data were collected.
Participants then completed one of five incremental protocols: Bruce, UCLA running, Wellness Fitness Initiative (WFI), Shuttle, and Cycle. Protocols were chosen to represent common modes used in clinical and performance exercise tests (running and cycling), different stage durations and workload increments within a mode, an occupationally relevant test (WFI), and a field test (Shuttle). The Bruce, UCLA, and WFI protocols were completed on a motorized treadmill (PPS Med; Woodway USA Inc., Waukesha, WI). The Shuttle run was administered in an indoor gymnasium and the Cycle protocol was performed on an electronically braked cycle ergometer (Velotron; RacerMate Inc., Seattle, WA). During all protocols, verbal encouragement was provided to promote maximal effort. Tests were terminated upon volitional exhaustion of the participant or the participant's inability to maintain the target cadence or speed.
The Bruce protocol (Bruce et al. 1973) included 3-min stages, with the first stage beginning at a gradient of 10% and a speed of 2.7 km·h−1. At the end of each stage the gradient increased by 2%; the speed increased to 4.0, 5.5, 6.8, 8.0, and 8.8 km·h−1 for the subsequent stages.
The UCLA running protocol consisted of 1-min stages. During the first 3 min, the gradient was held at 0% and the speed increased from 4.8 to 5.5 to 6.0 km·h−1. Between minutes 3 and 12, the treadmill gradient was set at 2% and speed was increased by 1.1 or 1.3 km·h−1 each minute until the maximum speed of 16.7 km·h−1 was reached. At the beginning of minute 12, the gradient was increased by 2% each minute while the treadmill speed remained constant at 16.7 km·h−1.
For the WFI (National Fire Protection Association [NFPA] 2006), the gradient was held at 0% and the speed at 4.8 km·h−1 for the first 3 min. The speed was then increased to 7.2 km·h−1 while the gradient remained at 0%. The treadmill gradient and speed were then alternately increased by 2% and 0.8 km·h−1, respectively, at the end of each minute.
The Cycle protocol began at a power output of 60 watts for 3 min. Thereafter, the work rate was increased by 40 watts (Heyward 2010) at the end of every 2-min stage. Target cadence was 60 revolutions per min.
For the Shuttle test (Léger et al. 1988), participants were required to run between two lines located 20 m apart at a set pace that was established using recorded signals. The test started at a speed of 8.5 km·h−1 and was increased by 0.5 km·h−1 every min. If the participant failed to cover the distance between signal emissions, a warning was given. If the participant failed to cover the distance on two consecutive lengths, the test was terminated.
Measurements
Oxygen uptake was measured continuously during the testing session using a portable metabolic system (Oxycon Mobile; Care Fusion, Yorba Linda, CA). Before each testing session, ambient temperature and pressure, delay, gas, and volume calibrations were performed. The Oxycon Mobile was worn on the back in a specially designed harness. Expired air was collected with a face mask connected to the flow sensor unit and sampling line of the Oxycon Mobile. Data were transmitted wirelessly to a personal computer. Breath-by-breath data were averaged over 15-sec intervals.
Heart rate was measured continuously throughout the testing session (Zephyr BioHarness BT2, Annapolis, MD). Following testing, HR data were downloaded to a laptop and stored for subsequent analysis. HR data were temporally aligned with  O2 data and the second-by-second data were averaged over 15-sec intervals.
O2 data and the second-by-second data were averaged over 15-sec intervals.
During each trial, the participant indicated his rating of perceived exertion (RPE) using the 6–20 Borg Scale (Borg 1982). Incremental tests were considered maximal if two of the following three criteria were met: (1) a plateau in oxygen uptake despite an increase in work rate, (2) respiratory exchange ratio (R) ≥1.1, and (3) a HR within 12 beats of age-predicted maximal HR (HRmax) (Plowman and Smith 2014).
Resting HR was identified as the lowest HR among the eight 15-sec intervals between minutes 7 and 9 of the rest period. The highest HR among all 15-sec intervals during the incremental test was considered HRmax. The HRindex was calculated using the following equation: HRindex = HRmax/HRrest. The HRindex was used to predict energy expenditure using the equation proposed by Wicks et al. (2011):
| (1) |
Predicted energy expenditure in METs was converted to mass-specific  O2 using the conversion factor of 3.5 mL·O2·kg−1·min−1 per 1 MET. The conversion factor was selected to correspond to the factor used by Wicks et al. (2011) when converting body mass-specific
O2 using the conversion factor of 3.5 mL·O2·kg−1·min−1 per 1 MET. The conversion factor was selected to correspond to the factor used by Wicks et al. (2011) when converting body mass-specific  O2 to METs in the development of the HRindex prediction model. The highest measured
O2 to METs in the development of the HRindex prediction model. The highest measured  O2max value among all 15-sec intervals during the incremental test was identified as the criterion
O2max value among all 15-sec intervals during the incremental test was identified as the criterion  O2max.
O2max.
Statistical analyses
Data are presented as mean ± SD unless indicated otherwise. A one-way (protocol) analysis of variance with repeated measures was used to detect differences in HRrest, HRmax, HRindex, and  O2max across the protocols. The accuracy of the
O2max across the protocols. The accuracy of the  O2max predictions was assessed by computing the bias (mean difference between predicted and measured
O2max predictions was assessed by computing the bias (mean difference between predicted and measured  O2max) and 95% confidence intervals (CI) for each protocol and overall. If the CI did not include zero, predicted and measured
O2max) and 95% confidence intervals (CI) for each protocol and overall. If the CI did not include zero, predicted and measured  O2max were considered statistically different at an alpha level of 0.05. Precision of the predictions overall and for each protocol were assessed using the root mean squared error (RMSE) and the standard error of the estimate (SEE). The RMSE is the square root of the mean of the squared prediction errors (predicted
O2max were considered statistically different at an alpha level of 0.05. Precision of the predictions overall and for each protocol were assessed using the root mean squared error (RMSE) and the standard error of the estimate (SEE). The RMSE is the square root of the mean of the squared prediction errors (predicted  O2max − measured
O2max − measured  O2max) and expresses the total error of the prediction equation, which includes the variation due to the lack of association between two measurements quantified by the SEE (Lohman 1981). A Bland–Altman plot was constructed to depict the overall bias and display any systematic error in the prediction. Pearson product-moment correlation coefficients (r) were computed to describe the strength of the linear relationship between measured and predicted
O2max) and expresses the total error of the prediction equation, which includes the variation due to the lack of association between two measurements quantified by the SEE (Lohman 1981). A Bland–Altman plot was constructed to depict the overall bias and display any systematic error in the prediction. Pearson product-moment correlation coefficients (r) were computed to describe the strength of the linear relationship between measured and predicted  O2max. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL; software version 19). The level of statistical significance was set at P < 0.05.
O2max. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL; software version 19). The level of statistical significance was set at P < 0.05.
Results
Ten young, fit men (age 22 ± 2 year; height 1.76 ± 0.08 m; body mass 78.0 ± 8.5 kg; body mass index 25.2 ± 2.7 kg·m−2) completed the study. On average, participants engaged in regular aerobic physical activity for ∼40–45 min on 3 day·week−1. All incremental tests were considered maximal based on the attainment of at least two of the three established criteria described in the Methods section.
Heart rate and metabolic data are summarized in Table 1. There were no differences in HRrest (P = 0.091) or HRmax (P = 0.183) among trials. The HRindex was significantly lower for the Cycle compared with the Shuttle protocol (P = 0.002). No significant differences were detected for other HRindex contrasts, however, there was a trend for the HRindex to be lower for the Cycle than the UCLA protocol (P = 0.058). There was no difference in R among protocols (P = 0.053).  O2max was significantly greater for the Bruce (P = 0.004) and WFI (P = 0.026) protocols compared with the Cycle protocol.
O2max was significantly greater for the Bruce (P = 0.004) and WFI (P = 0.026) protocols compared with the Cycle protocol.
Table 1.
Heart rate, metabolic, and perceptual effort among protocols (N = 10).
| Variable | Bruce | UCLA | WFI | Shuttle | Cycle |
|---|---|---|---|---|---|
| HRrest (beats·min−1) | 62 ± 8 | 61 ± 7 | 62 ± 5 | 59 ± 6 | 65 ± 6 |
| HRmax (beats·min−1) | 187 ± 9 | 192 ± 12 | 192 ± 8 | 189 ± 11 | 186 ± 11 |
| HRindex | 3.0 ± 0.4 | 3.2 ± 0.4 | 3.1 ± 0.3 | 3.3 ± 0.4* | 2.9 ± 0.3 |
| RPEpeak | 19.1 ± 0.9 | 19.7 ± 0.5 | 19.6 ± 0.5 | 19.3 ± 1.0 | 19.3 ± 0.7 |
| Rpeak | 1.29 ± 0.06 | 1.27 ± 0.05 | 1.25 ± 0.08 | 1.23 ± 0.04 | 1.27 ± 0.05 |
 O2max (mL·kg−1·min−1) O2max (mL·kg−1·min−1) |
54.9 ± 7.5* | 52.2 ± 8.0 | 54.1 ± 6.8* | 52.9 ± 5.0 | 47.8 ± 8.3 |
Values are mean ± SD. HRrest, resting heart rate; HRmax, maximum heart rate; HRindex, HRmax/HRrest; RPE, rating of perceived exertion; R, respiratory exchange ratio;  O2max, maximal oxygen uptake; WFI, Wellness Fitness Initiative.
O2max, maximal oxygen uptake; WFI, Wellness Fitness Initiative.
P < 0.05 compared with the Cycle protocol for the given variable.
Figure 1 presents predicted versus measured  O2max for all trials. Table 2 provides a comparison of measured versus predicted
O2max for all trials. Table 2 provides a comparison of measured versus predicted  O2max, including prediction bias, RMSE, SEE and correlation between measured and predicted
O2max, including prediction bias, RMSE, SEE and correlation between measured and predicted  O2max. Over all trials, the prediction equation significantly underestimated
O2max. Over all trials, the prediction equation significantly underestimated  O2max by 5.1 ± 8.3 mL·kg−1·min−1 when compared with measured
O2max by 5.1 ± 8.3 mL·kg−1·min−1 when compared with measured  O2max (95% CI = −7.4, −2.7). The negative bias for all protocols indicated a consistent underestimation of
O2max (95% CI = −7.4, −2.7). The negative bias for all protocols indicated a consistent underestimation of  O2max on average by HRindex model, whereas a 95% CI that did not span zero for the Bruce and WFI protocols indicated a significant difference between predicted and measured
O2max on average by HRindex model, whereas a 95% CI that did not span zero for the Bruce and WFI protocols indicated a significant difference between predicted and measured  O2max. The RMSE was 9.6 mL·kg−1·min−1 overall and ranged from 7.6 (Shuttle) to 11.2 mL·kg−1·min−1 (Bruce) among the five protocols. The SEE was lowest for the Shuttle and highest for the Cycle protocol. Low to moderate correlations between measured and predicted
O2max. The RMSE was 9.6 mL·kg−1·min−1 overall and ranged from 7.6 (Shuttle) to 11.2 mL·kg−1·min−1 (Bruce) among the five protocols. The SEE was lowest for the Shuttle and highest for the Cycle protocol. Low to moderate correlations between measured and predicted  O2max were identified.
O2max were identified.
Figure 1.
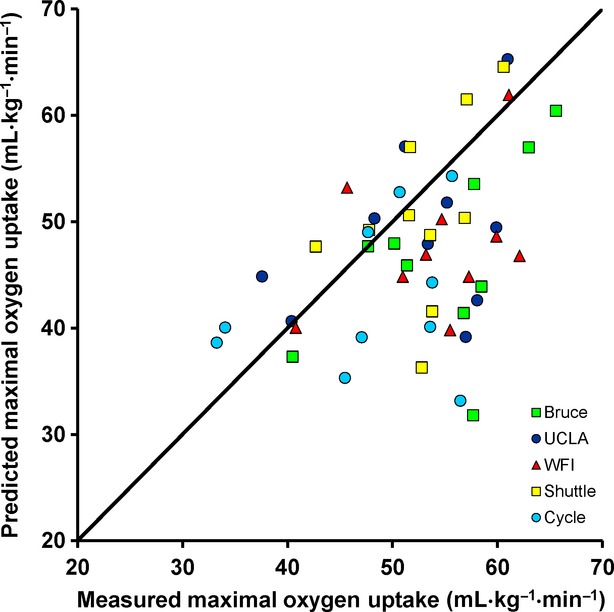
Scatter plot of predicted versus measured  O2max with points identified by protocol. The line of identity denotes perfect agreement.
O2max with points identified by protocol. The line of identity denotes perfect agreement.
Table 2.
Comparison of measured and predicted maximal oxygen uptake ( O2max).
O2max).
| Bias (95% CI) (mL·kg−1·min−1) | RMSE (mL·kg−1·min−1) | SEE (mL·kg−1·min−1) | r | |
|---|---|---|---|---|
| Bruce | −8.3 (−14.0, −2.6)* | 11.2 | 6.4 | 0.53 |
| UCLA | −3.3 (−9.7, 3.0) | 9.1 | 7.4 | 0.38 |
| WFI | −6.4 (−11.8, −1.1)* | 9.6 | 6.3 | 0.36 |
| Shuttle | −2.1 (−7.7, 3.4) | 7.6 | 4.5 | 0.45 |
| Cycle | −5.2 (−11.9, 1.6) | 10.3 | 8.0 | 0.27 |
| Overall | −5.1 (−7.4, −2.7)* | 9.6 | 6.7 | 0.42 |
N = 50 for Overall and N = 10 for all other protocols. WFI, Wellness Fitness Initiative; Bias, predicted  O2max – measured
O2max – measured  O2max; CI, confidence interval; RMSE, root mean squared error; SEE, standard error of the estimate; r, Pearson product-moment correlation.
O2max; CI, confidence interval; RMSE, root mean squared error; SEE, standard error of the estimate; r, Pearson product-moment correlation.
Predicted  O2max significantly different than measured
O2max significantly different than measured  O2max.
O2max.
The Bland–Altman plot (Fig. 2) displays the dispersion of the individual prediction errors and the overall bias and limits of agreement. The wide limits of agreement (11.5, −21.6 mL·kg−1·min−1) reflect the variability among the prediction errors. Table 3 presents the accuracy of predictions on an individual level, clearly showing that prediction accuracy varies considerably among participants as well as by protocol within participants.
Figure 2.
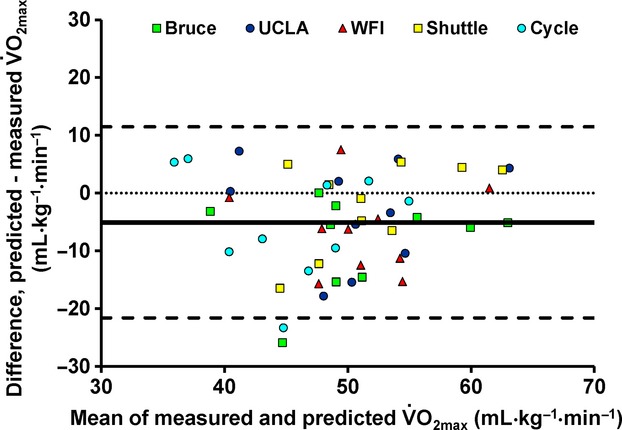
Bland–Altman plot of the prediction errors (predicted  O2max – measured
O2max – measured  O2max). The bias (solid line) and the limits of agreement (dashed lines; mean difference ± 1.96 SD) are displayed.
O2max). The bias (solid line) and the limits of agreement (dashed lines; mean difference ± 1.96 SD) are displayed.
Table 3.
Individual prediction errors (predicted  O2max − measured
O2max − measured  O2max) across all trials.
O2max) across all trials.
| Part # | Protocol | ||||
|---|---|---|---|---|---|
| Bruce | UCLA | WFI | Shuttle | Cycle | |
| 01 | −25.9 | 2.0 | −6.2 | −4.9 | −13.5 |
| 02 | 0.0 | 7.2 | 7.5 | 1.4 | 5.3 |
| 03 | −6.0 | −10.5 | −15.3 | −1.0 | −9.6 |
| 04 | −2.3 | −5.5 | −4.5 | −12.3 | −10.2 |
| 05 | −5.5 | −3.4 | −15.7 | 5.3 | −8.0 |
| 06 | −4.3 | 5.8 | −6.3 | 4.4 | 2.1 |
| 07 | −15.4 | −17.9 | −12.5 | −16.5 | −23.4 |
| 08 | −3.2 | 0.2 | −0.8 | 4.9 | 5.9 |
| 09 | −5.2 | 4.3 | 0.8 | 3.9 | −1.5 |
| 10 | −14.6 | −15.5 | −11.3 | −6.6 | 1.3 |
 O2max, maximal oxygen uptake; Part #, participant number; WFI, Wellness Fitness Initiative; units are mL·kg−1·min−1.
O2max, maximal oxygen uptake; Part #, participant number; WFI, Wellness Fitness Initiative; units are mL·kg−1·min−1.
Discussion
Across all test protocols, this study found that the HRindex prediction model significantly underestimated  O2max in aerobically fit, college-aged men. Furthermore, prediction accuracy was influenced by the incremental test protocol utilized.
O2max in aerobically fit, college-aged men. Furthermore, prediction accuracy was influenced by the incremental test protocol utilized.  O2max was significantly underpredicted for the Bruce and WFI protocols; however, no significant differences between estimated and measured
O2max was significantly underpredicted for the Bruce and WFI protocols; however, no significant differences between estimated and measured  O2max were found for the UCLA running, Shuttle, or Cycle protocols. In addition, accuracy of predictions at the individual level was highly variable for all protocols.
O2max were found for the UCLA running, Shuttle, or Cycle protocols. In addition, accuracy of predictions at the individual level was highly variable for all protocols.
CRF is a measure of interest to many clinicians, researchers, and other practitioners who perform graded exercise testing, and the use of prediction equations to estimate CRF is routinely employed, particularly in large-scale studies. In their development of the HRindex model, Wicks et al. (2011) identified published studies that reported measured values for HRrest, HRabsolute, and  O2 and extracted 220 data points that were group averages from 60 eligible exercise studies. The large dataset included diverse populations, different modes of exercise, and both submaximal and maximal data. Prediction models were developed to estimate energy expenditure over the range of 1–14 METs (
O2 and extracted 220 data points that were group averages from 60 eligible exercise studies. The large dataset included diverse populations, different modes of exercise, and both submaximal and maximal data. Prediction models were developed to estimate energy expenditure over the range of 1–14 METs ( O2max range: 3.5–49.0 mL·kg−1·min−1) using HR as a predictor, with HR expressed as either HRabsolute, HRnet (HRabsolute − HRrest) or HRindex. The researchers concluded that the best fit model employed the HRindex, which explained 99.1% of the variability in the data. Moreover, subgroup analysis, which included testing device (treadmill, cycle ergometer, other), indicated that the prediction equation was robust. Therefore, a single prediction equation, rather than protocol-specific or sex-specific equations, for the prediction of energy expenditure was proposed by Wicks et al. (2011). These researchers used data points based on group means rather than individual data point to develop the HRindex model, and it remains unclear how this might impact model performance. Furthermore, the HRindex prediction equation was not cross validated; therefore, subsequent performance of the model was uncertain. To our knowledge, no published studies have examined the accuracy of the HRindex prediction equation. In this study, the HRindex prediction equation was applied using five protocols that included three exercise types.
O2max range: 3.5–49.0 mL·kg−1·min−1) using HR as a predictor, with HR expressed as either HRabsolute, HRnet (HRabsolute − HRrest) or HRindex. The researchers concluded that the best fit model employed the HRindex, which explained 99.1% of the variability in the data. Moreover, subgroup analysis, which included testing device (treadmill, cycle ergometer, other), indicated that the prediction equation was robust. Therefore, a single prediction equation, rather than protocol-specific or sex-specific equations, for the prediction of energy expenditure was proposed by Wicks et al. (2011). These researchers used data points based on group means rather than individual data point to develop the HRindex model, and it remains unclear how this might impact model performance. Furthermore, the HRindex prediction equation was not cross validated; therefore, subsequent performance of the model was uncertain. To our knowledge, no published studies have examined the accuracy of the HRindex prediction equation. In this study, the HRindex prediction equation was applied using five protocols that included three exercise types.  O2max was significantly underestimated overall and a difference in prediction accuracy among protocols was found.
O2max was significantly underestimated overall and a difference in prediction accuracy among protocols was found.
In theory, assuming a uniform HRrest, the direct relationship between HRmax and  O2max in the HRindex model dictates that for estimates of
O2max in the HRindex model dictates that for estimates of  O2max to be the same for two protocols, HRmax and
O2max to be the same for two protocols, HRmax and  O2max must remain the same or change in a similar way between protocols. A review of several studies that compared cycling versus running or different treadmill protocols revealed that the effect of exercise protocol on
O2max must remain the same or change in a similar way between protocols. A review of several studies that compared cycling versus running or different treadmill protocols revealed that the effect of exercise protocol on  O2max corresponded to the effect of exercise protocol on HRmax in some studies (McArdle and Magel 1970; Miyamura et al. 1978; Pannier et al. 1980; Verstappen et al. 1982; Davies et al. 1984; Fernhall and Kohrt 1990) but not others (Hermansen and Saltin 1969; Faulkner et al. 1971; Froelicher et al. 1974; St Clair Gibson et al. 1999). Thus, a precise estimate of
O2max corresponded to the effect of exercise protocol on HRmax in some studies (McArdle and Magel 1970; Miyamura et al. 1978; Pannier et al. 1980; Verstappen et al. 1982; Davies et al. 1984; Fernhall and Kohrt 1990) but not others (Hermansen and Saltin 1969; Faulkner et al. 1971; Froelicher et al. 1974; St Clair Gibson et al. 1999). Thus, a precise estimate of  O2max using the HRindex model, which includes HRmax as a predictor, may be difficult to obtain across different protocols. Results from the present investigation support this point. As shown in Table 1, measured
O2max using the HRindex model, which includes HRmax as a predictor, may be difficult to obtain across different protocols. Results from the present investigation support this point. As shown in Table 1, measured  O2max was greater for the Bruce and WFI protocols than the Cycle protocol; however, HRmax did not differ among protocols. As the effect of protocol was not the same for HRmax and
O2max was greater for the Bruce and WFI protocols than the Cycle protocol; however, HRmax did not differ among protocols. As the effect of protocol was not the same for HRmax and  O2max, it was not surprising that differences between predicted and measured
O2max, it was not surprising that differences between predicted and measured  O2max were observed. Additionally, the combined effect of small nonsignificant differences in HRmax and HRrest likely led to the significantly lower HRindex for the Cycle than the Shuttle protocol. Accordingly, estimated
O2max were observed. Additionally, the combined effect of small nonsignificant differences in HRmax and HRrest likely led to the significantly lower HRindex for the Cycle than the Shuttle protocol. Accordingly, estimated  O2max followed the same pattern as the HRindex, which did not match measured
O2max followed the same pattern as the HRindex, which did not match measured  O2max.
O2max.
Wicks et al. (2011) developed the HRindex model using group averages, with 5–1909 participants contributing to a data point; therefore, the researchers were unable to establish the prediction error for an individual. Examination of the individual prediction errors in this study (Fig. 2 and Table 3) indicated a wide range of errors within all protocols. Moreover, the prediction errors displayed considerable variability in predictive accuracy among individuals across protocols. Uth et al. (2004) used the ratio of HRmax to HRrest (i.e., the HRindex) to estimate  O2max, but the researchers derived a prediction equation, which included a proportionality constant and the HRindex as factors, based on the Fick equation rather than regressing
O2max, but the researchers derived a prediction equation, which included a proportionality constant and the HRindex as factors, based on the Fick equation rather than regressing  O2max on HR as Wicks et al. (2011) did. In a group of 46 well-trained men (
O2max on HR as Wicks et al. (2011) did. In a group of 46 well-trained men ( O2max = 60.9 ± 5.5 mL·kg−1·min−1), Uth et al. (2004) determined the proportionality constant in one subgroup (n = 10) and then predicted
O2max = 60.9 ± 5.5 mL·kg−1·min−1), Uth et al. (2004) determined the proportionality constant in one subgroup (n = 10) and then predicted  O2max in the second subgroup (n = 36). The researchers reported a nonsignificant difference of 0.28 mL·kg−1·min−1 between measured and predicted
O2max in the second subgroup (n = 36). The researchers reported a nonsignificant difference of 0.28 mL·kg−1·min−1 between measured and predicted  O2max and an SEE of 2.7 mL·kg−1·min−1, indicating good agreement between measured and predicted
O2max and an SEE of 2.7 mL·kg−1·min−1, indicating good agreement between measured and predicted  O2max in the group of well-trained men. Validation studies of maximal performance tests based on time or work rate have reported a wide range of predictive accuracies, nevertheless, the predictive accuracy of commonly used equations (Foster et al. 1984; Storer et al. 1990; American College of Sports Medicine 2006; Heyward 2010) is higher than the accuracy noted for the HRindex in this study. Storer et al. (1990) reported an SEE of 2.57 mL·kg−1·min−1 for the prediction of
O2max in the group of well-trained men. Validation studies of maximal performance tests based on time or work rate have reported a wide range of predictive accuracies, nevertheless, the predictive accuracy of commonly used equations (Foster et al. 1984; Storer et al. 1990; American College of Sports Medicine 2006; Heyward 2010) is higher than the accuracy noted for the HRindex in this study. Storer et al. (1990) reported an SEE of 2.57 mL·kg−1·min−1 for the prediction of  O2max from body mass, work rate, and age in cycle ergometry using a sex-specific equation for men. A generalized prediction equation frequently used with the Bruce protocol has an SEE of 3.35 mL·kg−1·min−1 (Foster et al. 1984), which is considerably lower than the 6.4 mL·kg−1·min−1 identified in this study. In fact, this regression equation for the Bruce protocol, which uses test time to predict
O2max from body mass, work rate, and age in cycle ergometry using a sex-specific equation for men. A generalized prediction equation frequently used with the Bruce protocol has an SEE of 3.35 mL·kg−1·min−1 (Foster et al. 1984), which is considerably lower than the 6.4 mL·kg−1·min−1 identified in this study. In fact, this regression equation for the Bruce protocol, which uses test time to predict  O2max, produced accurate estimates of
O2max, produced accurate estimates of  O2max when applied to the data collected in this investigation (prediction bias = −2.6 ± 3.2 mL·kg−1·min−1; SEE = 3.3 mL·kg−1·min−1; r = 0.90).
O2max when applied to the data collected in this investigation (prediction bias = −2.6 ± 3.2 mL·kg−1·min−1; SEE = 3.3 mL·kg−1·min−1; r = 0.90).
There are several possible explanations for the underestimation of  O2max by the HRindex model and the high variability in the estimates of
O2max by the HRindex model and the high variability in the estimates of  O2max. One possible reason is that the participants in this study had a higher CRF on average than those in the model development study. For 72% of the incremental tests in this study, the
O2max. One possible reason is that the participants in this study had a higher CRF on average than those in the model development study. For 72% of the incremental tests in this study, the  O2max attained was higher than the 49 mL·kg−1·min−1 upper limit identified in development of the HRindex prediction model. It then follows that HRindex values in this study likely exceeded or were near the upper limit of those included as predictors by Wicks et al. (2011). However, Wicks et al. (2011) reported that the HRindex model accounted for fitness. Our results indicate that the HRindex model did not accurately predict
O2max attained was higher than the 49 mL·kg−1·min−1 upper limit identified in development of the HRindex prediction model. It then follows that HRindex values in this study likely exceeded or were near the upper limit of those included as predictors by Wicks et al. (2011). However, Wicks et al. (2011) reported that the HRindex model accounted for fitness. Our results indicate that the HRindex model did not accurately predict  O2max in young, fit men. Furthermore, this study found relatively large prediction errors (>7 mL·kg−1·min−1) in ∼30% of the trials where
O2max in young, fit men. Furthermore, this study found relatively large prediction errors (>7 mL·kg−1·min−1) in ∼30% of the trials where  O2max did not exceed 49 mL·kg−1·min−1, indicating that individual prediction errors may be substantial even within the scope of the prediction model.
O2max did not exceed 49 mL·kg−1·min−1, indicating that individual prediction errors may be substantial even within the scope of the prediction model.
Both HRmax and HRrest are predictors in the HRindex model; therefore, a difference in the measurement of these predictors could affect prediction accuracy. Only 20% of the studies included in the development of the HRindex model indicated the methods used to obtain HRrest. Moreover, among those studies providing details, procedures were vastly different, with rest periods between 2 and 90 min and inconsistency in the position of the participants (seated or supine). In this study, the method for obtaining HRrest was guided by the technology used and the potential application of the HRindex method in a typical cardiopulmonary exercise test setting where prediction of  O2max is the objective. Therefore, the measurement was obtained with the participant in a seated rather than supine position. Additionally, the use of the lowest 15-sec sampling interval was easily achieved using a HR monitor, and helped to ensure the obtainment of a HRrest value in a field study. The rest period of 7 min prior to obtaining the measurement was consistent with methods described for obtaining HRrest (American College of Sports Medicine 2008; Heyward 2010). In part, the underestimation of
O2max is the objective. Therefore, the measurement was obtained with the participant in a seated rather than supine position. Additionally, the use of the lowest 15-sec sampling interval was easily achieved using a HR monitor, and helped to ensure the obtainment of a HRrest value in a field study. The rest period of 7 min prior to obtaining the measurement was consistent with methods described for obtaining HRrest (American College of Sports Medicine 2008; Heyward 2010). In part, the underestimation of  O2max may be a consequence of the seated HRrest measurement, but this is not possible to ascertain because the methods for obtaining HRrest were unknown or inconsistent in the studies used to develop the HRindex model. Wicks et al. (2011) justifiably indicate that the measurement of HRrest needs to be standardized for the accurate prediction of the HRindex and
O2max may be a consequence of the seated HRrest measurement, but this is not possible to ascertain because the methods for obtaining HRrest were unknown or inconsistent in the studies used to develop the HRindex model. Wicks et al. (2011) justifiably indicate that the measurement of HRrest needs to be standardized for the accurate prediction of the HRindex and  O2. Notwithstanding standardization of the HRrest measurement, accuracy of individual level predictions using the HRindex model may be variable. Lee et al. (2010) used the HRindex to predict MET values of various submaximal activities in persons with paraplegia, and the group reported a substantially lower (∼23%) absolute error percentage when using prediction equations developed for each individual (individual calibration) compared with a single regression equation developed for all participants (group calibration) despite the use of a standardized procedure to determine HRrest. Previous research (Andrews 1971; Hiilloskorpi et al. 2003) suggests that the incorporation of HRrest in the predictor reduces but does not eliminate the interindividual differences when using HR to predict energy expenditure.
O2. Notwithstanding standardization of the HRrest measurement, accuracy of individual level predictions using the HRindex model may be variable. Lee et al. (2010) used the HRindex to predict MET values of various submaximal activities in persons with paraplegia, and the group reported a substantially lower (∼23%) absolute error percentage when using prediction equations developed for each individual (individual calibration) compared with a single regression equation developed for all participants (group calibration) despite the use of a standardized procedure to determine HRrest. Previous research (Andrews 1971; Hiilloskorpi et al. 2003) suggests that the incorporation of HRrest in the predictor reduces but does not eliminate the interindividual differences when using HR to predict energy expenditure.
The accuracy of  O2max estimates could have been influenced by differences in resting metabolic rate and the use of the standard conversion factor to convert METs to
O2max estimates could have been influenced by differences in resting metabolic rate and the use of the standard conversion factor to convert METs to  O2. This study used the established conversion factor of 3.5 mL·O2·kg−1·min−1 per 1 MET, which is the method used in the development of the HRindex model. Although this conversion factor is routinely used, research has shown that this value does not always equate to resting
O2. This study used the established conversion factor of 3.5 mL·O2·kg−1·min−1 per 1 MET, which is the method used in the development of the HRindex model. Although this conversion factor is routinely used, research has shown that this value does not always equate to resting  O2 (Byrne et al. 2005) and hence this may be a source of error within the HRindex model.
O2 (Byrne et al. 2005) and hence this may be a source of error within the HRindex model.
This study involved five incremental exercise tests conducted within a 14-day interval. Thus, day to day variability in measurements of HRmax, HRrest, and  O2max may have contributed to the variability in the predictions between exercise protocols. Day to day variability in HRmax is ∼2–4 beats·min−1 (Achten and Jeukendrup 2003). The standard deviation of HRrest (5–8 beats·min−1) in this study suggested considerable variability in this measure. Procedures had been implemented to limit the effect of factors that influence heart rate, but uncontrollable factors, such as stress level or sleep quality, may have contributed to within-participant variability. For repeated measurements of
O2max may have contributed to the variability in the predictions between exercise protocols. Day to day variability in HRmax is ∼2–4 beats·min−1 (Achten and Jeukendrup 2003). The standard deviation of HRrest (5–8 beats·min−1) in this study suggested considerable variability in this measure. Procedures had been implemented to limit the effect of factors that influence heart rate, but uncontrollable factors, such as stress level or sleep quality, may have contributed to within-participant variability. For repeated measurements of  O2max, studies have reported a coefficient of variation of 4–5% (Katch et al. 1982; Howley et al. 1995) and a reliability coefficient of 0.95 (Taylor et al. 1955). Thus, trial to trial variability in physiological measures, notably HRrest, could account for some variability in predictions.
O2max, studies have reported a coefficient of variation of 4–5% (Katch et al. 1982; Howley et al. 1995) and a reliability coefficient of 0.95 (Taylor et al. 1955). Thus, trial to trial variability in physiological measures, notably HRrest, could account for some variability in predictions.
The retrospective nature of the study resulted in several inherent limitations, namely the dataset was small and obtained on a homogeneous group, limiting statistical power and generalizability of findings. Protocols employed included different exercise types; however, the use of only protocols with established prediction equations would have permitted comparisons between the HRindex and protocol-specific equations. Additional research with larger, more heterogeneous groups is needed to further evaluate the performance of the HRindex prediction model.
Conclusions
The use of a simple predictor, such as a HRindex, to predict  O2max across different exercise protocols is an attractive possibility, and a recently published article (Wicks et al. 2011), which retrospectively analyzed a large number of published studies suggested that this may be possible. However, this study found that the HRindex prediction model significantly underestimated
O2max across different exercise protocols is an attractive possibility, and a recently published article (Wicks et al. 2011), which retrospectively analyzed a large number of published studies suggested that this may be possible. However, this study found that the HRindex prediction model significantly underestimated  O2max in young, fit men across different protocols. Furthermore, the incremental test protocol influenced prediction accuracy, with predicted
O2max in young, fit men across different protocols. Furthermore, the incremental test protocol influenced prediction accuracy, with predicted  O2max differing significantly from measured
O2max differing significantly from measured  O2max for the Bruce and WFI protocols but not the UCLA running, Shuttle or Cycle protocols. Despite the fact that no significant differences between measured and predicted
O2max for the Bruce and WFI protocols but not the UCLA running, Shuttle or Cycle protocols. Despite the fact that no significant differences between measured and predicted  O2max were found for three of the five protocols studied, examination of the individual data revealed large prediction errors among all protocols. Additionally, prediction accuracy across protocols varied considerably within individuals. Therefore, our results suggest caution is warranted when applying the HRindex prediction equation to estimate
O2max were found for three of the five protocols studied, examination of the individual data revealed large prediction errors among all protocols. Additionally, prediction accuracy across protocols varied considerably within individuals. Therefore, our results suggest caution is warranted when applying the HRindex prediction equation to estimate  O2max in young, fit men. The findings from this study are consistent with the view that prediction models often provide valid estimates on a group level, but the accuracy of individual estimates vary considerably.
O2max in young, fit men. The findings from this study are consistent with the view that prediction models often provide valid estimates on a group level, but the accuracy of individual estimates vary considerably.
Acknowledgments
The research presented in this study was performed as part of the UCLA PHASER Program, sponsored by the Department of Homeland Security Science and Technology Directorate. We express our thanks and appreciation to the Program Manager, Jalal Mapar, and all the members of the PHASER research group for their support during this research project. We are also appreciative of the willingness of subjects to give so generously of their time to support this work. The authors express their appreciation to Eric Hultquist and Wes Lefferts for their help in data collection.
Conflicts of Interest
C. B. C. has served as a consultant to CareFusion, the manufacturer of the Oxycon Mobile. The other coauthors have no conflicts of interest to declare.
References
- Achten J, Jeukendrup AE. Heart rate monitoring: applications and limitations. Sports Med. 2003;33:517–538. doi: 10.2165/00007256-200333070-00004. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. p. 366. [Google Scholar]
- American College of Sports Medicine. ACSM's health-related physical fitness assessment manual. 2nd ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2008. p. 208. [Google Scholar]
- Andrews RB. Net heart rate as a substitute for respiratory calorimetry. Am. J. Clin. Nutr. 1971;24:1139–1147. doi: 10.1093/ajcn/24.9.1139. [DOI] [PubMed] [Google Scholar]
- Asmussen E, Hemmingsen I. Determination of maximum working capacity at different ages in work with the legs or with the arms. Scand. J. Clin. Lab. Invest. 1958;10:67–71. doi: 10.3109/00365515809079920. [DOI] [PubMed] [Google Scholar]
- Astrand PO. Human physical fitness with special reference to sex and age. Physiol. Rev. 1956;36:307–335. doi: 10.1152/physrev.1956.36.3.307. [DOI] [PubMed] [Google Scholar]
- Astrand PO, Ryhming I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during sub-maximal work. J. Appl. Physiol. 1954;7:218–221. doi: 10.1152/jappl.1954.7.2.218. [DOI] [PubMed] [Google Scholar]
- Balke B, Ware RW. An experimental study of physical fitness of air force personnel. US Armed Forces Med. J. 1959;10:675–688. [PubMed] [Google Scholar]
- Blair S, Kohl H, Paffenbarger R, Clark D, Cooper K, Gibbons L. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- Borg G. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am. Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J. Appl. Physiol. 2005;99:1112–1119. doi: 10.1152/japplphysiol.00023.2004. [DOI] [PubMed] [Google Scholar]
- Cooper KH. A means of assessing maximal oxygen intake. Correlation between field and treadmill testing. JAMA. 1968;203:201–204. [PubMed] [Google Scholar]
- Cureton KJ, Sloniger MA, O'bannon JP, Black DM, Mccormack WP. A generalized equation for prediction of VO2peak from 1-mile run/walk performance. Med. Sci. Sports Exerc. 1995;27:445–451. [PubMed] [Google Scholar]
- Davies B, Daggett A, Jakeman P, Mulhall J. Maximum oxygen uptake utilising different treadmill protocols. Br. J. Sports Med. 1984;18:74–79. doi: 10.1136/bjsm.18.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner JA, Roberts DE, Elk RL, Conway J. Cardiovascular responses to submaximum and maximum effort cycling and running. J. Appl. Physiol. 1971;30:457–461. doi: 10.1152/jappl.1971.30.4.457. [DOI] [PubMed] [Google Scholar]
- Fernhall B, Kohrt W. The effect of training specificity on maximal and submaximal physiological responses to treadmill and cycle ergometry. J. Sports Med. Phys. Fitness. 1990;30:268–275. [PubMed] [Google Scholar]
- Foster C, Jackson AS, Pollock ML, Taylor MM, Hare J, Sennett SM, et al. Generalized equations for predicting functional capacity from treadmill performance. Am. Heart J. 1984;107:1229–1234. doi: 10.1016/0002-8703(84)90282-5. [DOI] [PubMed] [Google Scholar]
- Froelicher VF, Jr, Brammell H, Davis G, Noguera I, Stewart A, Lancaster MC. A comparison of three maximal treadmill exercise protocols. J. Appl. Physiol. 1974;36:720–725. doi: 10.1152/jappl.1974.36.6.720. [DOI] [PubMed] [Google Scholar]
- Hermansen L, Saltin B. Oxygen uptake during maximal treadmill and bicycle exercise. J. Appl. Physiol. 1969;26:31–37. doi: 10.1152/jappl.1969.26.1.31. [DOI] [PubMed] [Google Scholar]
- Heyward VH. Advanced fitness assessment and exercise prescription. Champaign, IL: Human Kinetics; 2010. p. 480. [Google Scholar]
- Hiilloskorpi HK, Pasanen ME, Fogelholm MG, Laukkanen RM, Manttari AT. Use of heart rate to predict energy expenditure from low to high activity levels. Int. J. Sports Med. 2003;24:332–336. doi: 10.1055/s-2003-40701. [DOI] [PubMed] [Google Scholar]
- Howley ET, Bassett DR, Welch HG. Criteria for maximal oxygen uptake: review and commentary. Med. Sci. Sports Exerc. 1995;27:1292–1301. [PubMed] [Google Scholar]
- Katch VL, Sady SS, Freedson P. Biological variability in maximum aerobic power. Med. Sci. Sports Exerc. 1982;14:21–25. doi: 10.1249/00005768-198201000-00004. [DOI] [PubMed] [Google Scholar]
- Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- Lee M, Weimo Z, Hedrick B, Fernhall B. Estimating MET values using the ratio of HR for persons with paraplegia. Med. Sci. Sports Exerc. 2010;42:985–990. doi: 10.1249/MSS.0b013e3181c0652b. [DOI] [PubMed] [Google Scholar]
- Lee DC, Sui X, Ortega FB, Kim YS, Church TS, Winett RA, et al. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. Br. J. Sports Med. 2011;45:504–510. doi: 10.1136/bjsm.2009.066209. [DOI] [PubMed] [Google Scholar]
- Léger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988;6:93–101. doi: 10.1080/02640418808729800. [DOI] [PubMed] [Google Scholar]
- Lohman TG. Skinfolds and body density and their relation to body fatness: a review. Hum. Biol. 1981;53:181–225. [PubMed] [Google Scholar]
- Margaria R, Aghemo P, Rovelli E. Indirect determination of maximal O2 consumption in man. J. Appl. Physiol. 1965;20:1070–1073. doi: 10.1152/jappl.1965.20.5.1070. [DOI] [PubMed] [Google Scholar]
- McArdle WD, Magel JR. Physical work capacity and maximum oxygen uptake in treadmill and bicycle exercise. Med. Sci. Sports. 1970;2:118–123. [PubMed] [Google Scholar]
- Miyamura M, Kitamura K, Yamada A, Matsui H. Cardiorespiratory responses to maximal treadmill and bicycle exercise in trained and untrained subjects. J. Sports Med. Phys. Fitness. 1978;18:25–32. [PubMed] [Google Scholar]
- National Fire Protection Association. NFPA 1582. Standard on comprehensive occupational medical program for fire departments. 2007 edition. Quincy, MA: NFPA; 2006. p. 66. [Google Scholar]
- Pannier JL, Vrijens J, Van Cauter C. Cardiorespiratory response to treadmill and bicycle exercise in runners. Eur. J. Appl. Physiol. 1980;43:243–251. doi: 10.1007/BF00421838. [DOI] [PubMed] [Google Scholar]
- Plowman SA, Smith DL. Exercise physiology for health, fitness, and performance. Philadelphia, PA: Lippincott Williams & Wilkins; 2014. p. 744. [Google Scholar]
- Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007;39:377–390. doi: 10.1249/mss.0b013e31802ca597. [DOI] [PubMed] [Google Scholar]
- Shephard RJ. Tests of maximum oxygen intake. A critical review. Sports Med. 1984;1:99–124. doi: 10.2165/00007256-198401020-00002. [DOI] [PubMed] [Google Scholar]
- St Clair Gibson A, Lambert MI, Hawley JA, Broomhead SA, Noakes TD. Measurement of maximal oxygen uptake from two different laboratory protocols in runners and squash players. Med. Sci. Sports Exerc. 1999;31:1226–1229. doi: 10.1097/00005768-199908000-00022. [DOI] [PubMed] [Google Scholar]
- Storer TW, Davis JA, Caiozzo VJ. Accurate prediction of VO2max in cycle ergometry. Med. Sci. Sports Exerc. 1990;22:704–712. doi: 10.1249/00005768-199010000-00024. [DOI] [PubMed] [Google Scholar]
- Taylor HL, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J. Appl. Physiol. 1955;8:73–80. doi: 10.1152/jappl.1955.8.1.73. [DOI] [PubMed] [Google Scholar]
- Uth N, Sørensen H, Overgaard K, Pedersen PK. Estimation of VO2max from the ratio between HRmax and HRrest–the heart rate ratio method. Eur. J. Appl. Physiol. 2004;91:111–115. doi: 10.1007/s00421-003-0988-y. [DOI] [PubMed] [Google Scholar]
- Verstappen FT, Huppertz RM, Snoeckx LH. Effect of training specificity on maximal treadmill and bicycle ergometer exercise. Int. J. Sports Med. 1982;3:43–46. doi: 10.1055/s-2008-1026061. [DOI] [PubMed] [Google Scholar]
- Wicks JR, Oldridge NB, Nielsen LK, Vickers CE. HR index-a simple method for the prediction of oxygen uptake. Med. Sci. Sports Exerc. 2011;43:2005–2012. doi: 10.1249/MSS.0b013e318217276e. [DOI] [PubMed] [Google Scholar]


