Abstract
We report a case of large iris melanocytoma in a child diagnosed by fine needle aspiration biopsy. In this interventional case report, cytologic features typical of melanocytoma were obtained by fine needle aspiration biopsy (FNAB). FNAB can be used in difficult diagnostic cases if a good sample is obtained, this technique has an accuracy of more than 99% in tumors larger than 3 mm; however, false-negative and false-positive results may be obtained. Its risk of local spread is very small, an advantage over incisional biopsy. The most common complication is intralesional hemorrhage and hyphema.
Keywords: Iris melanocytoma, Child, Fine needle aspiration biopsy, Iris tumor
Introduction
Zimmerman and Garron suggested the term “melanocytoma” to describe deeply pigmented tumor of the optic nerve head1 is an uncommon tumor of the uveal tract, which is generally regarded as benign, having the ability for invasion of local tissues.2 Classically it is described at the optic nerve head, but it is encountered less frequently at the ciliary body, and there are rare reports of occurrence in the iris, sclera, conjunctiva, and choroid. In some cases, iris or ciliary body melanocytoma can show progressive growth or even extrascleral involvement; this aspect makes clinical differentiation from malignant melanoma difficult.3 Moreover, iris melanocytoma has a peculiar tendency to undergo necrosis with shedding of pigment on the iris and trabecular meshwork,4 this can produce secondary glaucoma and heterochromia. Despite its benign nature, iris melanocytoma growth occurs in 23% of cases at 5 years and 48% of cases at 10 years.5 Malignant transformation is rare.
Case report
A 9 year-old girl was referred to the King Khaled Eye Specialist Hospital with the diagnosis of iris tumor in her left eye. For the past two months, she had experienced intermittent itching and redness in her left eye. On ophthalmic examination, the best uncorrected visual acuity was 20/20 in each eye. The intraocular pressures (IOP) were 13 mm Hg in the right eye and 20 mmHg in the left. The biomicroscopic examination of the right eye was within normal limits. The left eye had a dark brown lobulated lesion about 3 × 4 mm located in the lower nasal quadrant of the iris between 7 and 8 o’clock. It appeared to be solid, approached but did not involve the pupil. The peripheral part of the lesion is separated from the angle with the normal iris. Inferiorly there was another crescent like pigmented lesion at 6 o’clock. The surface of the iris has numerous small-pigmented lesions more concentrated around the lesion and disappears away from it. The mass seemed to be adhered to the peripheral posterior cornea (Fig. 1a). Extension of the lesion obstructed the gonioscopic view into the chamber angle between 7 and 8 o’clock. The remainder of the angle was open with a moderate amount of pigmentation covering the scleral spur and trabecular meshwork (Fig. 1b). There were moderate anterior chamber reaction 3 + cells, and 1 + flare with few pigment deposits on the posterior surface of the cornea. Ultrasound Biomicroscopy (UBM) showed a large homogeneous solid mass and a thickness of about 2.53 mm, the ciliary body was free from lesion, UBM was suggestive of iris melanoma (Fig. 1c). Uveitis work-up and systemic evaluation were unremarkable. Based on overall appearance and location malignancy could not be ruled out. Differential diagnosis included melanoma, nevus, melanocytoma and others. Fine-Needle Aspiration Biopsy (FNAB) as well as anterior chamber aqueous aspiration were performed and cytological smears of specimen showed highly pigmented plump polyhedral cells with abundant pigmented cytoplasm and round regular normal size nuclei and no evidence of pleomorphism, the cells showed low nuclear–cytoplasmic ratio (N/C ratio) (Fig. 2), the appearance was suggestive of iris melanocytoma.
Figure 1a.
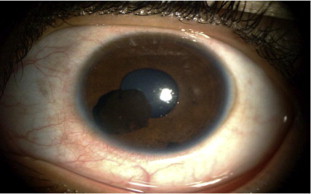
Picture of the left eye had a dark brown lobulated lesion about 3 4 mm located in the lower nasal quadrant of the iris between 7 and 8 o’clock. Inferiorly there was another crescent like lesion at 6 o’clock.
Figure 1b.

Extension of the iris lesion obstructing the gonioscopic view of the chamber angle between 7 and 8 o’clock. The remainder of the angle was open with a moderate amount of pigmentation covering the scleral spur and trabecular meshwork.
Figure 1c.
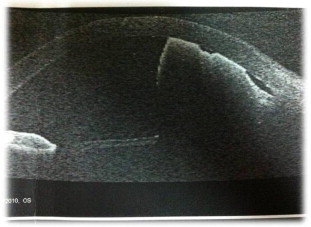
UBM showed a large homogeneous solid mass with a thickness of about 2.53 mm. The ciliary body was free from lesion.
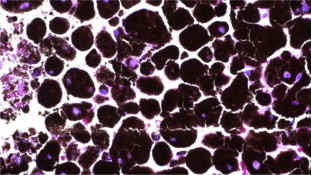
Figure 2.
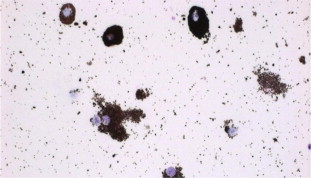
Direct smear of FNAB showing melanocytoma cells × 400 H&E.
Surgical technique for FNAB
The FNAB technique of the iris involves proper instrumentation, planning of tumor approach, handling of harvested cells, and preparation and interpretation of cytologic specimens. In our case clear corneal incision was made superionasally as paracentesis using 75 blade. Aqueous was aspirated with a 27 gauge cannula and viscoelastic substance was injected into the anterior chamber to form it and prevent any possible cells seed or bleeding that might occur. FNAB was done using a 25-gauge needle attached to a 3-ml syringe. Inferior clear corneal approach was selected for aspiration. Aspiration point was at the thickest portion of the tumor where the tumor was adhered to the cornea. A gentle sliding motion of the needle within the mass was performed to shave and loosen cells for aspiration. Aspiration of the 3-ml syringe was performed over 5 s to confirm that the needle was completely within the mass and not simply aspirating aqueous. Aspiration was maintained for a few seconds with the needle in the tumor and also as the needle was withdrawn from the eye. The needle was then removed slowly from the eye and bleeding occurred during the aspiration into the anterior chamber. The anterior chamber was refilled using balanced salt solution (BSS) after removing viscoelastic substance and stromal hydration was performed to the paracentesis site. There was very little aspiration material. The aspirated cells, located predominantly in the needle tip and wall of syringe, were flushed into the syringe using BSS. Immediately after collection, the sample was transported to the Cytology laboratory and was processed within 24 h of collection.
Clinical course
Recovery was satisfactory. On the first postoperative day, uncorrected visual acuity of the left eye was 20/100 with hyphema and blood clot in the anterior chamber with +3 reaction mainly pigment cells. There was a lot of pigmentation over the endothelium and along with needle track (Fig. 3a). Intraocular pressure was elevated immediately postoperative, but lowered to 16 mmHg with Timolol 0.5% twice daily. Prior to discharge IOP was 20 mmHg OS without treatment with resolving hyphema. Later on sector iridectomy was done to excise the lobulated lesion between 7 and 8 o’clock to avoid the risk of melanocytomalytic glaucoma. The other pigmented lesion at 6 o’clock was collected material of pigments and also all the diffuse pigments on the iris surface that were more abundant closer to the lesion and they aspirated easily with Simcoe needle (Fig. 3b). There was no residual iris tumor and no recurrence after 23 months of tumor removal with normal IOP without treatment. The best uncorrected visual acuity was 20/20 with quiet anterior chamber, and remaining pigments on the endothelium and along the corneal aspiration tract. The histopathologic appearance of the iris tissue was typical of melanocytoma arising within the iris stroma. The cells were polyhedral in shape with large melanin granules and regular uniform nuclei (Fig. 4), the diagnosis of iris melanocytoma was confirmed.
Figure 3a.

Post FNAB picture with hyphema, and blood clot around the lesion with pigmentation over the endothelium as well as the needle track.
Figure 3b.
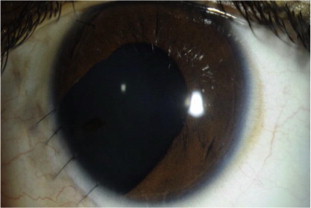
Slit-lamp appearance of the left eye after sector iridectomy showing complete excision of the iris lesions with some pigments along the aspiration tract.
Figure 4.
Histopathologic appearance of the non-cohesive melanocytoma cells of the lesion × 400 H&E.
Discussion
Iris melanocytoma is a rare variant of iris nevus with typical clinical and histopathologic features that may be of value in differentiating it from other nevi and melanomas. It presents as a darkly pigmented nodular mass with a mossy granular surface and no intrinsic vessels.6 The differential diagnosis of a pigmented tumor of the ciliary body and iris includes adenoma, adenocarcinoma, medulloepithelioma and iris epithelium pigment cyst, epithelial inclusion cyst, and most importantly, malignant melanoma. Although melanocytoma can usually be distinguished histopathologically, it can be difficult to differentiate clinically, especially from a malignant melanoma. Our patient has characteristic differentiating features such as color and diffuse pigmentation, although the pigmented condensation at 6 o’clock was thought to be a separate lesion. Fine needle aspiration biopsy is helpful in establishing the diagnosis and provides an efficient, economical, and relatively safe method without potential risk with better planning for excision, this was evident in our case which is similar to the one reported by El-Harazi et al.7 In a clinical study by Shields and associates of 200 patients referred for suspected iris melanoma, 158 patients (76%) were found to have lesions other than melanoma and these were termed as pseudomelanomas. The most common pseudomelanomas included iris cyst (38%) and iris nevus (31%). In that series, only one pseudomelanoma (0.5%) was an iris melanocytoma.8 Iris melanocytoma can undergo spontaneous necrosis with resultant pigment dispersion or shedding of melanocytoma cells and/or melanophages into the anterior chamber, causing secondary glaucoma or heterochromia.9 Macrophages that ingest pigment particles released from the necrotic tumor may cause secondary open-angle glaucoma by mechanically obstructing the trabecular meshwork. The term ‘melanocytomalytic glaucoma’ has been used in the literature to describe such a phenomenon.10 The anterior uveitis that is often present can also cause permanent damage of the aqueous outflow. Well-defined nodular melanocytomas can be successfully resected, eliminating the source of the pigment. Fine-needle aspiration biopsy can be done as an outpatient procedure and is safe and effective, it can be used in difficult diagnostic cases; this technique has an accuracy of more than 99%. Its risk of local spread is very small, an advantage over incisional biopsy. The most common complication is intralesional hemorrhage,6 that may have an effect and cause hyphema as it occurred in our case. The management of suspected iris melanocytoma is usually cautious observation. When noninvasive diagnostic techniques fail to establish the diagnosis or tumor growth is documented, fine-needle aspiration biopsy or local resection using iridectomy, iridogoniectomy, or iridogoniocyclectomy is performed.11 Local resection can also be used to treat secondary glaucoma caused by necrotic melanocytoma.12 In conclusion this case proves that iris melanocytoma can occur in young age group without significant symptoms and may cause condensed pigmented areas that may look like a tumor. High IOP may occur transiently following resection. Local resection can also be used to decrease the risk of secondary glaucoma caused by necrotic melanocytoma. FNAB is a good tool in the diagnosis of iris melanocytoma and anterior chamber tap might not be helpful. Recurrence of the tumor following resection has not been observed with good outcome.
Conflicts of interest
The authors declared that there is no conflicts of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Joffe L., Shields J.A., Osher R., Gass J.D.M. Clinical and follow-up studies of melanocytomas of the optic disc. Ophthalmology. 1979;86:1067–1068. doi: 10.1016/s0161-6420(79)35421-5. [DOI] [PubMed] [Google Scholar]
- 2.Zimmerman L.E. Melanocytes, melanocytic nevi and melanocytomas. Invest Ophthalmol. 1965;4:11–41. [PubMed] [Google Scholar]
- 3.Shields J.A., Eagle R.C., Jr., Shields C.L., Nelson L.B. Progressive growth of an iris melanocytoma in a child. Am J Ophthalmol. 2002;133:287–289. doi: 10.1016/s0002-9394(01)01305-8. [DOI] [PubMed] [Google Scholar]
- 4.Sagoo M.S., Mruthyunjaya P., Cree I., Luthert P.J., Hungerford J.L. Malignant transformation of iris melanocytoma to iris ring melanoma. Br J Ophthalmol. 2007;91:1571–1572. doi: 10.1136/bjo.2006.105858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shields C.L., Shields J.A., Materin M. Iris melanoma: risk factors for metastasis in 169 consecutive patients. Ophthalmology. 2001;108:172–178. doi: 10.1016/s0161-6420(00)00449-8. [DOI] [PubMed] [Google Scholar]
- 6.Demirci H., Mashayekhi A., Shields C.L., Eagle R.C., Jr., Shields J.A. Iris melanocytoma: clinical features and natural course in 47 cases. Am J Ophthalmol. 2005;139:468. doi: 10.1016/j.ajo.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 7.El-Harazi S.M., Kellaway J., Font R.L. Melanocytoma of the ciliary body diagnosed by fineneedle aspiration biopsy. Diagn Cytopathol. 2000 Jun;22(6):394–397. doi: 10.1002/(sici)1097-0339(200006)22:6<394::aid-dc13>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 8.Shields J.A., Sanborn G.E., Augsburger J.J. The differential diagnosis of malignant melanoma of the iris. A clinical study of 200 patients. Ophthalmology. 1983;90:716–720. doi: 10.1016/s0161-6420(83)34500-0. [DOI] [PubMed] [Google Scholar]
- 9.Al-Hinai A., Edelstein C., Burnier M.N., Jr. Unusual case of melanocytoma. Can J Ophthalmol. 2004;39:461e3. doi: 10.1016/s0008-4182(04)80020-6. [DOI] [PubMed] [Google Scholar]
- 10.Fineman M.S., Eagle R.C., Jr., Shields J.A. Melanocytomalytic glaucoma in eyes with necrotic iris melanocytoma. Ophthalmology. 1998;105:492e6. doi: 10.1016/S0161-6420(98)93033-0. [DOI] [PubMed] [Google Scholar]
- 11.Shields J.A., Shields C.L., Ehya H., Eagle R.C., De Potter P. Fine-needle aspiration biopsy of suspected intraocular tumors. The 1992 Urwick lecture. Ophthalmology. 1992;1993(100):1677–1684. doi: 10.1016/s0161-6420(93)31418-1. [DOI] [PubMed] [Google Scholar]
- 12.Shields J.A., Annesley W.H., Jr., Spaeth G.L. Necrotic melanocytoma of iris with secondary glaucoma. Am J Ophthalmol. 1977;84:826–829. doi: 10.1016/0002-9394(77)90505-0. [DOI] [PubMed] [Google Scholar]



