Abstract
Background:
For the past two decades, Acinetobacter spp. have emerged as an important pathogen globally in various infections.
Objectives:
This study was conducted to determine the frequency, risk factors, and antibiotic resistance pattern of Acinetobacter spp. from various clinical samples.
Materials and Methods:
This retrospective, hospital record–based, cross-sectional study included a total of 8749 clinical samples collected from patients at a tertiary care hospital in Odisha, India from July 2010 to December 2012. The samples were processed and identified by standard protocol. The Acinetobacter isolates were tested for antibiotic resistance by Kirby-Bauer disk diffusion method [according to the Clinical and Laboratory Standards Institute (CLSI) guidelines].
Results:
From 8749 clinical samples, 4589 (52.5%) yielded significant growth and only 137 (3%, 137/4589) Acinetobacter spp. were isolated. Maximum (56.9%) isolates were obtained from pus/swab, followed by blood (13.1%) and urine (12.4%). Elderly age, being inpatients, longer duration of stay in the hospital, associated co-morbidity, and invasive procedure were found to be significant risk factors in the setup investigated (P is less than 0.05). Out of 137 isolates, 75 (54.7%) were resistant to more than three classes of antibiotics (multidrug resistant) and 8 (5.8%) were resistant to all commonly used antibiotics (pan-drug resistant). Majority of the isolates were sensitive to imipenem, meropenem, and piperacillin/tazobactam, and showed resistance rates of 19%, 22%, and 23%, respectively. All eight pan-drug resistant isolates were 100% sensitive to colistin.
Conclusion:
This hospital-based epidemiological data will help to implement better infection control strategies and improve the knowledge of antibiotic resistance patterns in our region.
Keywords: Acinetobacter species, antibiotics, frequency, resistance, risk factors
INTRODUCTION
Members of the genus Acinetobacter are ubiquitous, free-living, and saprophytic bacilli that can be obtained easily from soil, water, food, and sewage.[1] These are aerobic, gram-negative, non-fermenter of glucose, and opportunistic pathogens that emerge as an important cause of hospital-acquired infections and intermittent outbreaks globally. Acinetobacter has undergone significant taxonomic modification over the last 30 years. Its most common and important representative is Acinetobacter baumannii, and the other species such as Acinetobacter lwoffii, Acinetobacter johnsonii, and Acinetobacter haemolyticus are rarely isolated from patients.[2] Its great capacity to survive in low-moist environment coupled with its ability to develop resistance to antimicrobial agents can increase the possibility of spreading in hospitals.[3]
The risk of colonization and subsequent infection are associated with factors such as the presence of underlying severe illnesses, long-term hospitalization, stays in intensive care units (ICUs), selective antimicrobial pressure, and invasive interventions such as use of mechanical ventilation or catheters.[4,5] The nosocomial infections caused by Acinetobacter include pneumonia, septicemia, wound sepsis, urinary tract infection, endocarditis, and meningitis.[6] In addition to infection among hospitalized patients, community-acquired Acinetobacter infection is increasingly reported.[7]
There is a significant difference in the behavior and spread of multi-drug resistant Acinetobacter spp. recovered various geographic locations.[8] Since several factors cause resistance in Acinetobacter spp., treatment of infections caused by this organism should be based on antibiotic susceptibility tests. Therefore, having information regarding the prevalence and pattern of bacterial resistance to these drugs is important.[9,10]
Keeping these above facts in view and due to the paucity of reports from Odisha, India, we analyzed the frequency, risk factors, and resistance pattern of Acinetobacter spp. that were isolated from different clinical samples in a tertiary care hospital in Odisha.
MATERIALS AND METHODS
Study area, population, and methodology
A retrospective, hospital record–based, cross-sectional study was carried out from July 2010 to December 2012 in the Department of Clinical Microbiology at a tertiary care hospital in Odisha. This 600-bedded hospital has three ICUs, one emergency ward, six medical and surgical wards, and outpatient departments (OPDs). A total of 8749 clinical samples like pus/swab, urine, sputum, blood, body fluid, tracheal aspirate, endotracheal tube, and intravenous (IV) catheter tips were collected from the patients and transferred to the laboratory without delay for further processing. A retrospective evaluation of patient's age, sex, co-morbidity (including diabetes mellitus, chronic obstructive pulmonary disease, asthma, neurologic impairment, congestive cardiac failure, end-stage renal disease, cancer, hepatitis and human immunodeficiency virus), admission into the hospital, duration of stay, and special invasive procedure conducted was carried out on the basis of the case record histories. A healthcare-associated infection or nosocomial infection is defined as a localized or systemic condition resulting from an adverse reaction to the presence of an infectious agent (s) or its toxin (s) that was not present on admission to the hospital. An infection is considered as nosocomial if all the elements of a site-specific infection criterion of Center of Disease Control and Prevention (CDC) were first present together on or after the 3rd hospital day (day of hospital admission is day 1).[11] Patient from whom Acinetobacter was isolated in the absence of a clinical disease suggesting colonization were not included in this study. The study was conducted after due approval was obtained from the institutional ethical committee.
The differences in the risk factors among patients infected with Acinetobacter spp. and patients suspected with bacterial infections were compared and investigated for significant risk factors in patients with these infections.
Sample processing and antibiogram
In the laboratory, all the collected samples were cultured aerobically on blood agar and MacConkey agar. Blood specimen was cultured in trypticase soy broth (TSB) and subcultured in blood agar and chocolate agar. The isolation, identification, and speciation were done according to the standard procedure.[12]
All isolates were tested for antimicrobial susceptibility testing by the standard Kirby-Bauer disk diffusion method according to Bauer et al.[13] The test organism was picked up with a sterile loop, suspended in peptone water, and incubated at 37°C for 2 h. The turbidity of the suspension was adjusted to 0.5 McFarland's standard [1.5 × 108 colony forming units (CFU)/ml]. It was then spread on the surface of a Mueller-Hinton agar (MHA) plate using sterile cotton swab. The following standard antibiotic disks were placed on the MHA plate: Ampicillin/sulbactam (10/10 mcg), ciprofloxacin (5 mcg), gentamicin (10 mcg), amikacin (30 mcg), tobramycin (10 mcg), ceftazidime (30 mcg), piperacillin/tazobactam (100/10 mcg), imipenem (10 mcg), meropenem (10 mcg), ofloxacin (5 mcg), cefepime (30 mcg), and colistin (10 mcg). The plate was incubated at 37°C overnight. The zone of inhibition were measured and interpreted according to the Clinical and Laboratory Standards Institute (CLSI) guidelines.[14] All dehydrated media and antibiotic disks were procured from Himedia Labs (Mumbai, India). In addition, the antibiotic potency of the disks was standardized against the reference strains of Escherichia coli ATCC 25922 as the negative control and A. baumannii ATCC 19606 as the positive control.
The isolate was considered as highly resistant when it was resistant to imipenem, amikacin, and ampicillin/sulbactam. Multidrug-resistant (MDR) Acinetobacter spp. are defined as those isolates resistant to more than three classes of antibiotics.[15] An isolate was classified as pan-resistant when it was resistant to all the commonly used antibiotics.[15]
Statistical analysis
The data were analyzed for mean, median and standard deviation, and P value (Chi-square with Yates’ correction and Fisher's exact test) by using GraphPad QuickCalcs (GraphPad Software Inc., La Jolla, CA, USA). Statistical significance was defined when the P value was less than 0.05.
RESULTS
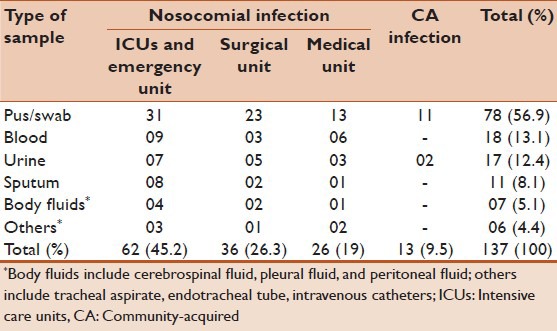
During the study period from July 2010 to December 2012, a total of 8749 clinical samples were aerobically cultured, of which 4589 (52.5%) yielded significant growth and rest of the samples [4160 (47.5%)] were either sterile or showed non-significant growth. From the 4589 growth-positive samples, a total of 137 (3%) Acinetobacter spp. were isolated. From the 137 isolates, majority [124 (90.5%)] were detected from inpatients (ICUs and emergency ward 45.2% and surgical ward 26.3%, followed by medicine ward 19%) and the rest [13 (9.5%)] were isolated from outpatients (community-acquired infection). Majority of the Acinetobacter spp. were isolated from pus/swab samples (56.9%), followed by blood (13.1%), urine (12.4%), sputum (8.1%), and body fluids (5.1%) [Table 1].
Table 1.
Distribution of Acinetobacter spp. based on mode of acquisition of infection and in various clinical samples (N=137)
A. baumannii was the main species responsible for 109 (79.6%) of the infections, followed by A. lwoffii [17 (12.4%)], and the remaining 11 (8%) were caused by other Acinetobacter species. The mean age of patients infected with Acinetobacter spp. was 38.58 years (median 39, standard deviation ± 16.44, 95% confidence intervals 35.37-41.8, range 3-85 years). The gender (male:female) ratio was 1.08:1. Acinetobacter infection was significantly observed among inpatients and the elderly (≥55 years), was associated with co-morbidity and longer duration of stay in the hospital (≥7 days), and was found in those who had undergone any invasive procedure (P was less than 0.05) [Table 2].
Table 2.
Risk factors for Acinetobacter spp. infection among patients attended a tertiary care hospital, South Odisha, India (N=8749)
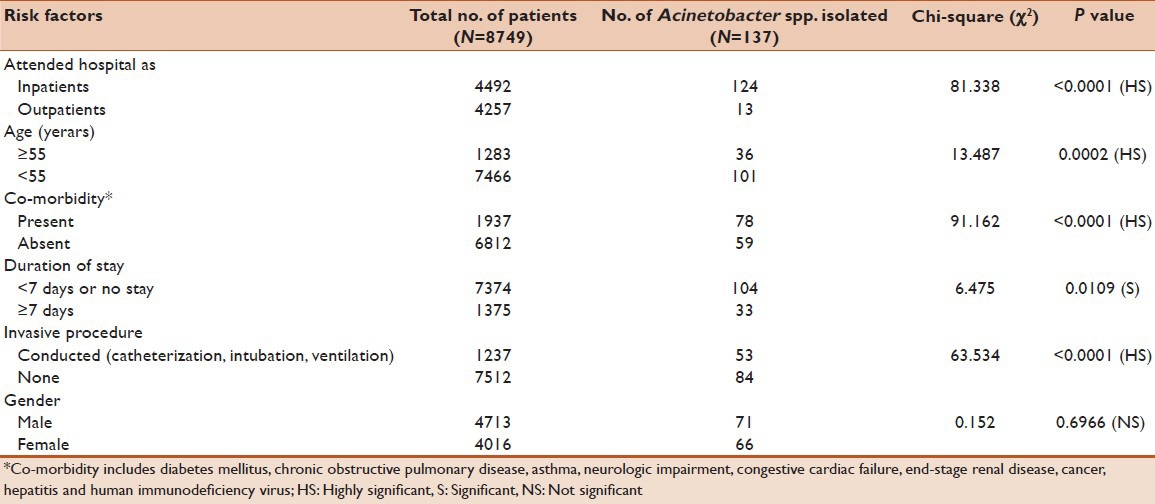
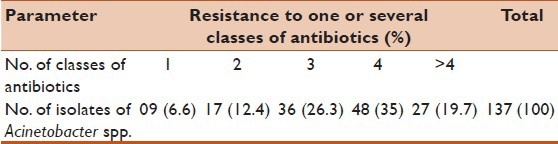
Table 3 shows the frequency of multidrug resistance among Acinetobacter spp. Out of the 137 isolates, 75 (54.7%) were MDR and only 8 (5.8%) were pan-drug resistant (PDR).
Table 3.
Frequency of multidrug resistance in Acinetobacter spp. (N=137)
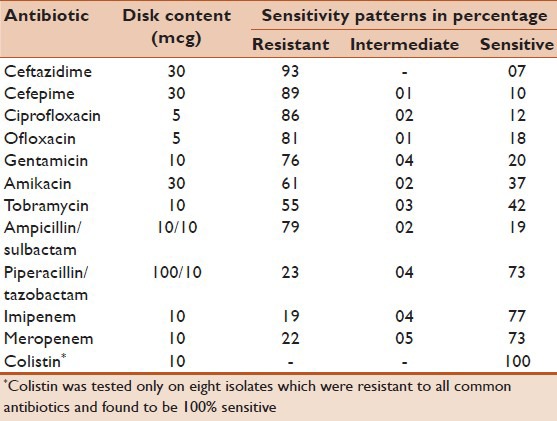
In the present study, most of the Acinetobacter spp. were highly resistant to ceftazidime (93%), cefepime (89%), ciprofloxacin (86%), ofloxacin (81%), ampicillin/sulbactam (79%), gentamicin (76%), amikacin (61%), and tobramycin (55%). The low resistant patterns of imipenem (19%), meropenem (22%), and piperacillin/tazobactam (23%) indicate that they are effective drugs. All eight (5.8%) PDR isolates were 100% sensitive to colistin [Table 4].
Table 4.
Frequency of antibiotic resistance in Acinetobacter spp. (N = 137)
DISCUSSION
Acinetobacter spp. are the second most common non-fermenting bacteria after Pseudomonas species that are isolated from human specimens, especially among nosocomial infections.[16] In recent years, this species has emerged as the causative agent of important nosocomial infections in the ICUs and emergency unit, which is probably related to the increasingly invasive diagnostic procedures used, the greater quantity of broad-spectrum antimicrobials used, and prolonged duration of stay in the hospital. Development of resistance against antimicrobials is a major problem in the treatment of Acinetobacter infections. Although they are considered as pathogen of mild virulence, they can rapidly acquire resistance.[17]
In our study, from 4589 clinical isolates, only 137 (3%) Acinetobacter spp. were obtained. Similar prevalence of 4.5% of the total organisms isolated was reported by Rit et al. in a tertiary care hospital in West Bengal, India.[18] In comparison, higher prevalence rates of 14% and 9.6% among hospital isolates were observed by Mostofi et al. in Tehran, Iran and Joshi et al. in Pune, India, respectively.[19,20] Acinetobacter normally inhabits soil and water and has also been isolated from foods and animals. In humans, Acinetobacter can colonize skin, wounds, respiratory and gastrointestinal tracts.[21] It is a pathogen of tropical and humid environment, but some species can survive environmental desiccation for weeks, a characteristic that promotes transmission through fomite contamination in hospitals.[22]
We isolated Acinetobacter from various clinical samples including blood, urine, body fluids, tracheal aspirate, endotracheal tubes, intravenous catheters, and other samples, but most commonly from pus/swab (56.9%). Similar findings were obtained by Chakraborty et al. in West Bengal.[23] Lone et al. in Srinagar, India reported that majority (39.6%) of the Acinetobacter isolates were obtained from urine, followed by pus and wound exudates (29.5%).[24]
Overall, in the present study, the significant risk factors for Acinetobacter infection were age ≥55 years, admission in the hospital as inpatients, longer (≥7 days) duration of stay in the hospital, having undergone any invasive procedures like catheterization, intubation, and mechanical ventilation, and with underlying co-morbid conditions, i.e., diabetes mellitus, chronic obstructive pulmonary disease, asthma, neurologic impairment, congestive cardiac failure, end-stage renal disease, cancer, hepatitis and human immunodeficiency virus (P ≤ 0.05). A longer hospital stay in a high-risk unit, use of mechanical ventilation, admission as inpatient into the ICUs, and underlying co-morbid conditions have been identified as the risk factors in previous studies as well.[15,24,25]
Our study revealed that majority (54.7%) of the isolates were MDR Acinetobacter spp., and among them, eight isolates were PDR. The other studies conducted by Bhattacharyya et al. in West Bengal and Mostofi et al. in Tehran reported the MDR isolates to be 29% and 54%, respectively.[19,26] Acinetobacter is ubiquitous in the hospital setting. Its ability to survive for long periods coupled with its ability to demonstrate a number of antimicrobial resistance genes has made Acinetobacter a successful hospital pathogen.[3]
Most of the patients who were admitted in our hospital had previously attended primary and secondary care hospitals and usually received combination of β-lactam antibiotics like third- and fourth-generation cephalosporins (i.e., ceftazidime, ceftriaxone, and cefepime) along with aminoglycosides (i.e., gentamicin and amikacin) or fluoroquinolones (ciprofloxacin, ofloxacin, and levofloxacin). Thus, majority of the isolates in our study were resistant to commonly used antibiotics such as ceftazidime, cefepime, gentamicin, amikacin, tobramycin, ciprofloxacin, ofloxacin, and ampicillin/sulbactam. This means MDR isolates are increasing day by day, probably due to indiscriminate use of these antibiotics in healthcare settings. It is re-emphasized that broad-spectrum antibiotics should be used with caution. We found that imipenem, meropenem, and piperacillin/tazobactam were the most potent antibiotics against this pathogen, although the resistance rates for these drugs were 19%, 22%, and 23%, respectively. The resistance pattern observed by us was similar to those described in previous studies.[18,23] Mostofi et al. in their study had reported tobramycin (26%) was the least resistant drug followed by meropenem (31%) and piperacillin/tazobactam (40%), but imipenem (76%) showed high resistance to Acinetobacter spp.[19] Differences observed between the studies could be due to the methods and the resistance patterns that are influenced by the environmental factors and the antimicrobial patterns used. The lower resistance rate of Acinetobacter spp. to carbapenems may be due to their recent introduction, i.e., in the year 2004, for use in our hospital. Higher cost of these drugs is also responsible for their restricted use. Although antibiotic resistance is a worldwide concern, it is first and foremost a local problem – selection for and amplification of resistant members of a species that are occurring in individual hospitals and communities, which can then spread worldwide.[27] There are many measures that may impact on antimicrobial resistance; reducing and restricting the use of antimicrobials to only those situations where they are warranted, at proper dose and for the proper duration is the most appropriate solution.[28] Thus, hospitals, as the primary incubators of antimicrobial-resistant pathogens, carry the highest responsibility for proper stewardship of our existing antimicrobial resources.
Carbapenems have been the drug of choice for treating Acinetobacter infections, but unfortunately, carbapenem-resistant Acinetobacter spp. due to carbapenemase enzyme is becoming common worldwide.[29] Of the β-lactamases, those with carbapenemase activity are the most concerning for drug resistance and include the serine oxacillinase (belonging to Ambler class D OXA type) and the metallo-β-lactamases (Ambler class B).[30]
Colistin was investigated in eight PDR Acinetobacter isolates in our laboratory and all of them were found to be susceptible. Colistin (polymyxin E) and tigecycline are new alternatives in the treatment of Acinetobacter species. Similar to our findings, Shareek et al. studied 44 isolates of A. baumannii and found that all were sensitive to colistin.[31] Taneja et al. in Chandigarh, India studied 224 A. baumannii isolates, out of which 50 (22.3%) isolates were resistant to carbapenems. The significant finding in their study was that eight (3.5%) isolates were resistant to both colistin and tigecycline.[32] Various authors have reported the resistance rate to colistin between 1.8% and 2%,[33,34] while resistance to tigecycline varies from being nonexistent to 66%.[35,36] We did not find any Acinetobacter isolate being resistant to colistin, which may be due to its selective use only in case of carbapenem-resistant gram-negative bacteria. In our hospital, tigecycline is not used routinely for treatment of Acinetobacter infections; so, we usually do not perform antibiogram using tigecycline disk.
CONCLUSION
We found 54.7% of Acinetobacter isolates were MDR and most of these isolates were sensitive to carbapenems and piperacillin/tazobactam. All eight PDR isolates were sensitive to colistin. Elderly age, being inpatients, longer duration of stay, associated co-morbidity, and invasive procedure were found to be the risk factors in the setup investigated. To avoid resistance, antibiotics should be used judiciously and empirical antibiotic therapy should be determined for each hospital according to the resistance rates of that center. This should be regulated according to antibiogram results. Increasing carbapenem resistance rates in Acinetobacter spp. leads to usage of new alternative antibiotics like colistin and tigecycline.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dougari HJ, Ndakidemi PA, Human IS, Benade S. Virulence factors and antibiotic susceptibility among verotoxic non O157: H7 Escherichia coli isolates obtained from water and waste water samples in Cape Town, South Africa. Afr J Biotechnol. 2011;10:14160–8. [Google Scholar]
- 2.Peleg AP, Seifert H, Paterson DL. Acinetobacter baumannii Emergence of a successful Pathogen. Clin Microbiol Rev. 2008;21:538–82. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu Yu, Yang Q, Xu Xw, Kong HS, Xu GY, G BY. Typing and characterization of carbapenems resistant Acinetobacter calcoaceticus – baumannii complex in a Chinese hospital. J Med Microbiol. 2004;53:653–6. doi: 10.1099/jmm.0.05513-0. [DOI] [PubMed] [Google Scholar]
- 4.Falagas ME, Karveli EA. The changing global epidemiology of Acinetobacter baumannii infections: A development with major public health implications. Clin Microbiol Infect. 2007;13:117–9. doi: 10.1111/j.1469-0691.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- 5.Fournier PE, Richet H. The epidemiology and control of Acinetobacter baumannii in health care fascilities. Clin Infect Dis. 2006;42:692–9. doi: 10.1086/500202. [DOI] [PubMed] [Google Scholar]
- 6.Towner KJ. Clinical importance and antibiotic resistance of Acinetobacter spp. J Med Microbiol. 1997;6:186–97. doi: 10.1099/00222615-46-9-721. [DOI] [PubMed] [Google Scholar]
- 7.Leung WS, Chu CM, Tsang KY, Lo FH, Ho PL. Fulminant community-acquired Acinetobacter baumannii pneumonia as a distinct clinical syndrome. Chest. 2006;129:102–9. doi: 10.1378/chest.129.1.102. [DOI] [PubMed] [Google Scholar]
- 8.Houang ET, Chu YW, Leung CM, Chu KY, Berlau J, Ng KC, et al. Epidemiology and infection control implication of Acinetobacter spp. in Hong Kong. J Clin Microbiol. 2001;39:228–34. doi: 10.1128/JCM.39.1.228-234.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halstead DC, Abid J, Dowzicky MJ. Antimicrobial susceptibility among Acinetobacter calcoaceticus-baumannii complex and Enterobacteriaceae collected as a part of yhe tigecycline evaluation and surveillance trail. J Infect. 2007;55:49–57. doi: 10.1016/j.jinf.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 10.Scott P, Deye G, Srinivasan A, Murray C, Moran K, Hulten E, et al. An outbreak of multidrug-resistant Acinetobacter baumannii-calcoaceticus complex infection in the US military health care system associated with military operations in Iraq. Clin Infect Dis. 2007;44:1577–84. doi: 10.1086/518170. [DOI] [PubMed] [Google Scholar]
- 11.www.cdc.gov [Internet]. CDC/NHSN Surveillance Definition of Healthcare-Associated Infection and Criteria for Specific Types of Infections in the Acute Care Setting; c2013. [Last updated on 2013 April; cited on 2013 April 28]. Available from: http://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf .
- 12.Collee JG, Miles RS, Watt B. Tests for identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and Mc Cartney Practical Medical Microbiology. 14th ed. Singapore: Churchill Livingstone; 2006. pp. 131–49. [Google Scholar]
- 13.Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45:493–6. [PubMed] [Google Scholar]
- 14.CLSI document M100-S19. Wayne; PA: USA: Clinical and Laboratory Standards Institute; 2009. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: Nineteenth Informational Supplement. [Google Scholar]
- 15.Dent LL, Marshall DR, Pratap S, Hulette RB. Multidrug resistant Acinetobacter baumannii: A descriptive study in a city hospital. BMC Infect Dis. 2010;10:196. doi: 10.1186/1471-2334-10-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Getchell-White SI, Donowitz LG, Gröschel DH. The inanimate environment of an intensive care unit as a potential source of nosocomial bacteria: Evidence for long survival of Acinetobacter calcoaceticus. Infect Control Hosp Epidemiol. 1989;10:402–7. doi: 10.1086/646061. [DOI] [PubMed] [Google Scholar]
- 17.Appleman MD, Belzberg H, Citron DM, Heseltine PN, Yellin AE, Murray J, et al. In vitro activities of nontraditional antimicrobials against multiresistant Acinetobacter baumannii strains isolated in an intensive care unit outbreak. Antimicrob Agents Chemother. 2000;44:1035–40. doi: 10.1128/aac.44.4.1035-1040.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rit K, Saha R. Multidrug-resistant Acinetobacter infection and their susceptibility patterns in a tertiary care hospital. Niger Med J. 2012;53:126–8. doi: 10.4103/0300-1652.104379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mostofi S, Mirnejad R, Masjedian F. Multi-drug resistance in Acinetobacter baumannii strains isolated from clinical specimens from three hospitals in Tehran-Iran. Afr J Microbiol Res. 2011;5:3579–82. [Google Scholar]
- 20.Joshi SG, Litake GM, Satpute MG, Telang NV, Ghole VS, Niphadkar KB. Clinical and demographic features of infection caused by Acinetobacter species. Indian J Med Sci. 2006;60:351–60. [PubMed] [Google Scholar]
- 21.Albrecht MC, Griffith ME, Murray CK, Chung KK, Horvath EE, Ward JA, et al. Impact of Acinetobacter infection on the mortality of burn patients. J Am Coll Surg. 2006;203:546–50. doi: 10.1016/j.jamcollsurg.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Bernards AT, Harinck HI, Dijkshoom L, van der Reijden TJ, van den Broek PJ. Persistant Acinetobacter baumannii? Look inside your medical equipment. Infect Control Hosp Epidemiol. 2004;25:1002–4. doi: 10.1086/502335. [DOI] [PubMed] [Google Scholar]
- 23.Chakraborty B, Banerjee D, Chakraborty B. Acinetobacter baumannii: No more a choosy intruder? Indian J Med Sci. 2011;65:344–8. [PubMed] [Google Scholar]
- 24.Lone R, Shah A, Kadri SM, Lone S, Faisal S. Nosocomial Multi-Drug-Resistant Acinetobacter Infections – Clinical Findings, Risk Factors and Demographic Characteristics. Bangladesh J Med Microbiol. 2009;3:34–8. [Google Scholar]
- 25.Agoda A, Zarrelli R, Barllitta M, Anzaldi A, Di Popolo A, Mattaliano A. Alert surveillance of intensive care unit acquired Acinetobacter infection in a Sicillian hospital. Clin Microbiol Infect. 2006;12:241–7. doi: 10.1111/j.1469-0691.2005.01339.x. [DOI] [PubMed] [Google Scholar]
- 26.Bhattacharyya S, Bhattacharyya I, Rit K, Mukhopadhyay PK, Dey JB, Ganguly U, et al. Antibiogram of Acinetobacter spp. isolated from various clinical specimens in a tertiary care hospital, West Bengal, India. Biomed Res. 2013;24:43–6. [Google Scholar]
- 27.O’Brien TF. Emergence, spread, and environmental effect of anti-microbial resistance: How use of an antimicrobial anywhere can increase resistance to any microbial anywhere else. Clin Infect Dis. 2002;34:S78–84. doi: 10.1086/340244. [DOI] [PubMed] [Google Scholar]
- 28.MacDougall C, Polk RE. Antimicrobial Stewardship Programs in Health Care Systems. Clin Microbiol Rev. 2005;18:638–56. doi: 10.1128/CMR.18.4.638-656.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Towner KJ. Acinetobacter: An old friend, but a new enemy. J Hosp Infect. 2009;73:355–63. doi: 10.1016/j.jhin.2009.03.032. [DOI] [PubMed] [Google Scholar]
- 30.Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-beta-lactamases: The quiet before the storm? Clin Microbiol Rev. 2005;18:306–25. doi: 10.1128/CMR.18.2.306-325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shareek PS, Sureshkumar D, Ramagopalakrishnan S, Ramasubramanian V, Abdul Ghafur K, Thirunarayanan MA. Antibiotic sensitivity pattern of blood isolates of Acinetobacter species in a tertiary care hospital: A rectrospective analysis. Am J Infect Dis. 2012;8:65–9. [Google Scholar]
- 32.Taneja N, Singh G, Singh M, Sharma M. Emergence of tigecycline and colistin resistant Acinetobacter baumannii in patients with complicated urinary tract infections in north India. Indian J Med Res. 2011;133:681–4. [PMC free article] [PubMed] [Google Scholar]
- 33.Duenas Diez AI, Bratos Perez MA, Eiros Bouza JM, Almaraz Gomez A, Gutierrez Rodriguez P, Miguel Gomez MA, et al. Susceptibility of the Acinetobacter calcoaceticus-A. baumannii complex to imipenem, meropenem, sulbactam and colistin. Int J Antimicrob Agents. 2004;23:487–93. doi: 10.1016/j.ijantimicag.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 34.Henwood CJ, Gatward T, Warner M, James D, Stockdale MW, Spence RP, et al. Antibiotic resistance among clinical isolates of Acinetobacter in the UK, and in vitro evaluation of tigecycline (GAR-936) J Antimicrob Chemother. 2002;49:479–87. doi: 10.1093/jac/49.3.479. [DOI] [PubMed] [Google Scholar]
- 35.Mezzatesta ML, Trovato G, Gona F, Nicolosi VM, Nicolosi D, Carattoli A, et al. In vitro activity of tigecycline and comparators against carbapenem-susceptible and resistant Acinetobacter baumannii clinical isolates in Italy. Ann Clin Microbiol Antimicrob. 2008;7:4. doi: 10.1186/1476-0711-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Navon-Venezia S, Leavitt A, Carmeli Y. High tigecycline resistance in multidrug-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2007;59:772–4. doi: 10.1093/jac/dkm018. [DOI] [PubMed] [Google Scholar]