Abstract
Background and Aims:
Pediatric index of mortality (PIM) 2 score is one of the severity scoring systems being used for predicting outcome of patients admitted to intensive care units (ICUs). The aim of the present study was to evaluate the usefulness of PIM2 score in predicting mortality in a tertiary care pediatric ICU (PICU) and to assess the associated factors in predicting mortality such as presence of shock, need for assisted ventilation and Glasgow coma scale <8.
Materials and Methods:
This was a prospective observation study done at tertiary care PICU from May 2011 to July 2011. Consecutive 119 patients admitted to PICU (aged 1 month to 12 years) were enrolled in the study. PIM2 scoring was done for all patients. The outcome was recorded as death or discharge. The associated factors for mortality were analyzed with SPSS 17.
Results:
PIM2 score discriminated between death and survival at a 99.8 cut-off, with area under receiver operating characteristic curve 0.843 with 95% confidence interval (CI) (0.765, 0.903). Most patients were referred late to this hospital, which explains higher death rate (46.2%), lesser length of hospital stay (mean 2.98 days) in the mortality group, and increased rate of mechanical ventilation (68.1%). Presence of shock was independently associated with mortality, as evidenced by binary logistic regression.
Conclusion:
PIM2 score discriminated well between survivors and death at PICU. Presence of shock was significantly associated with mortality.
Keywords: Mortality, pediatric index of mortality 2 score, shock, ventilation
Introduction
Many illness severity scoring systems are being used for predicting the outcome of patients admitted to pediatric intensive care units (PICU) and this has been constantly validated.[1] Although it is difficult to predict outcome of intensive care unit (ICU) patients accurately, these severity scoring systems may prognosticate groups of patients with similar presentations of the illness.[2] These risk-adjusted measures use logistic regression models to obtain an equation that describes the relationship between predictor variables and the probability of death.[3] The pediatric index of mortality (PIM) 2 score was introduced by Shann in 1997 (updated in 2003) to predict the outcome of children admitted to PICUs. Most of the severity scoring systems were designed in the West and need to be validated in India.
This study aims to evaluate the usefulness of PIM 2 score in predicting mortality in an Indian tertiary care PICU and to assess the associated factors in predicting mortality such as presence of shock, need for assisted ventilation and Glasgow coma scale <8.
Materials and Methods
This study was a prospective observational study done at a tertiary care PICU, which was a 537-bed teaching hospital with 15 intensive care beds catering mainly to medical illness (92.5%). The study period was from May 2011 to July 2011. With an average PICU mortality rate of 30-40%, an expected sensitivity of 85% and an allowable error of 5%, the sample size was calculated to be 119. Institutional ethical committee approval was obtained prior to undertaking the study. Informed written consent was obtained from parents of all participating children. Consecutive 119 children aged 1 month to 12 years admitted at PICU, who met with study criteria, were enrolled. Inclusion criteria: All consecutive patients admitted at PICU who were aged between 1 month and 12 years.
PIM2 scoring, which involves both clinical and laboratory data, was done once within 1 h of admission to PICU using a structured data collection form.
Demographic data such as age and gender were recorded. PIM 2 score consists of ten variables. The variables were elective admission to PICU, recovery post procedure, cardiac bypass, high-risk diagnosis, low-risk diagnosis, no response of pupils to bright light (>3 mm and both fixed), mechanical ventilation (at anytime during the first hour in PICU), systolic blood pressure (mmHg), base excess (mmHg) (arterial or capillary blood), and FiO2 *100/PaO2 (mmHg). All these ten parameters were recorded for each patient. Arterial blood gas analysis was done within 1 h of PICU admission and base excess, PaO2 were recorded by pediatric resident. The associated factors in predicting mortality such as presence of shock, need for mechanical ventilation, and Glasgow coma scale were also recorded. Any patient with tachycardia and signs of poor end organ perfusion, as defined by poor peripheral pulses with normal central pulses, prolonged capillary refill or flash refill, altered sensorium, cool extremities, and decreased urine output was considered to have “presence of shock.” Glasgow coma scale <8 was considered as low Glasgow coma scale. The length of stay in PICU was recorded. The patients were followed-up throughout their stay in PICU and during the hospital stay to record their final outcome. The final outcome was recorded as “discharged” or “death.”
PIM 2 score consists of ten variables. Yes or no response for these variables were scored as 1 or 0. These were entered into the system (www.sfar.org/scores2/pim22.html) for calculation of predicted mortality rate. The system computes the predicted mortality rate based on standard methods using logistic regression equation.[4,5]
PIM2 = [0.01395*(PaO2-120)] + [3.0791*Pupil sign] + [0.2888*(FiO2 *100/PaO2)] + [0.104* base] + [1.3352* mechanical ventilation] – [0.9282* elective admission] – [1.0244* recovery] + [0.7507*cardiac bypass] – [1.6829* high risk diagnosis] – [1.5770* low risk diagnosis] – [4.8841].
Predicted death rate = exponential (PIM2)/1 + exponential (PIM2).
A receiver operating characteristic (ROC) curve was constructed using statistical package “med calc.” The area under curve reflects the discriminatory performance of PIM2 score.
The associated factors such as presence of shock, need for ventilation, and low Glasgow coma scale were analyzed along with predicted death rate by using SPSS version 17 to determine their association with mortality. Univariate and multivariate analysis (binary logistic regression) was performed. The P value was calculated with 95% confidence interval (CI).
Results
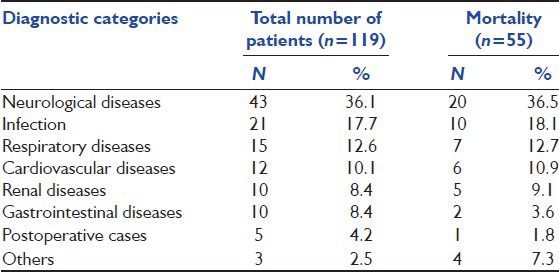
During the study period, consecutive 119 patients admitted at PICU, who met with the study criteria were studied. Table 1 shows demographic data and length of stay. Most common diagnostic categories and mortality pattern are shown in Table 2. In the study group, 58.82% were infants. The ratio of male to female in this study was 1.1:1. Neurological diseases contributed to 36.4% mortality, followed by infections 18.1% and respiratory diseases 12.7%. The average duration of stay in the PICU was 3.5 days (S.D = 2.64). The mean hospital stay for those who died was 2.98 days (S.D = 3.45) and those who were discharged was 3.95 days (S.D = 1.56)
Table 1.
Demographic data and length of stay
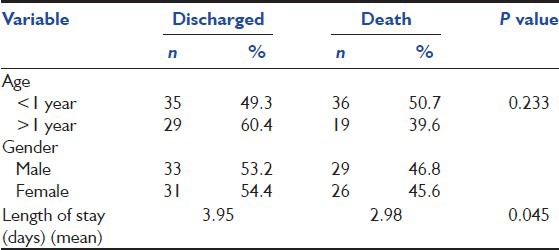
Table 2.
Diagnostic categories and mortality pattern
The mean predicted death rate was 92.24 (S.D = 19.91). The mean predicted death rate for those who were discharged was 88.87 (S.D = 20.05). The mean predicted death rate for those who died was 96.14 (S.D = 19.98). The observed death rate was 46.21% (n = 55). The death rate predicted by PIM2 score was 68.00% (n = 82).
Mortality risk was found to be increasing with increase in the predicted death rate. When the predicted death rate was <90, mortality risk was 7.1%, and, while the predicted death rate was 90-99, the risk increased to 50%. When the predicted death rate was >99, mortality raised to 51.7%.
Receiver operating characteristic curve
To determine the cut-off of predicted death rate at which it predicts mortality optimally, ROC curve was constructed. The best cut-off value at which sensitivity and specificity were optimal was 99.8.
The area under the ROC curve was 0.843, with 95% CI being 0.765 to 0.903 [Figure 1]. The best cut-off of predicted death rate was at 99.8, with a sensitivity of 98.2%, specificity of 65.6%, and positive predictive value of 71.1.
Figure 1.
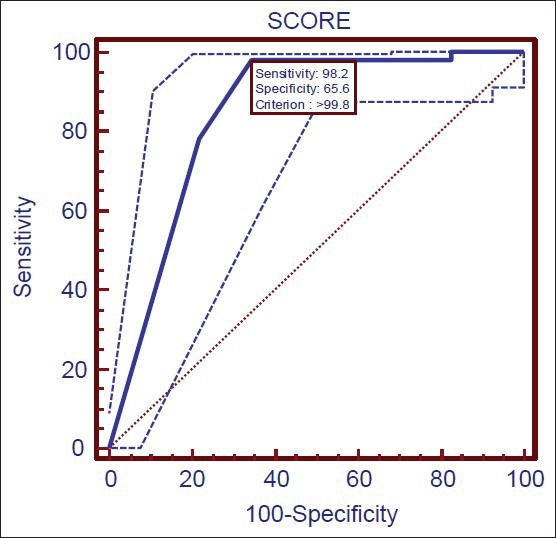
Receiver operating characteristic curve. The discrimination of PIM2 score between death and survival was good at 99.8 cut-off, reflected by area under ROC, which was 0.843 (95% CI: 0.765, 0.903)
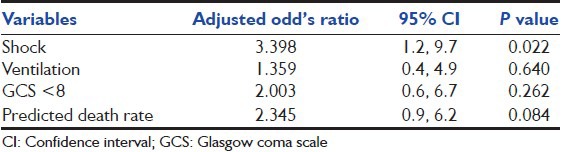
The risk factors such as age <1 year, Glasgow coma scale <8, presence of shock, and need of mechanical ventilation, were analyzed along with predicted death rate to find out statistical significance in their association with mortality. Out of 119 patients, 81 (68%) were mechanically ventilated. All the variables, except age <1 year, were found to be statistically significant [Table 3]. These risk factors were further analyzed using binary logistic regression model, of which, presence of shock was found to be independent association with mortality [Table 4].
Table 3.
Univariate analysis for factors associated with mortality
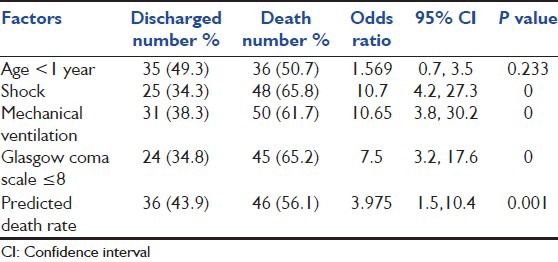
Table 4.
Multivariate analysis and mortality
Discussion
In this study done at tertiary care PICU, we found that the discrimination of PIM2 score between death and survival was good at 99.8 cut-off, reflected by area under ROC curve, which was 0.843 (95% CI: 0.765, 0.903). Hariharan showed that PIM2 score had good discrimination with area under ROC being 0.82 (95% CI: 0.72-0.92) in a PICU of a developing country.[6] PIM2 score was a good predictor of mortality in this study and is comparable to the results by Slater[4] and Eulmesekian,[7] who showed that PIM2 discriminated between death and survival well with area under the ROC curve 0.90 (95% CI: 0.89-0.92).
Because the sensitivity of PIM2 score at 99.8 cut-off was 98.2%, it can be used as a screening tool for assessing severity of illness of children admitted in PICU. The negative predictive value of the PIM2 score at 99.8 cut-off was found to be 97.7%. This helps identify children who have more chances of survival, which in turn helps in counseling parents of sick children admitted to PICU. The low specificity (65.6%) of PIM2 score denotes that not all patients with high predicted death rate may die. This reflects that effective interventions at PICU reduce mortality of those who have high predicted death rate at the time of admission, and, thereby, indicate good performance of PICU.
In contrast to other scores like PRISM used in PICU, which is performed at 24 h of PICU admission,[8] PIM2 score is done within 1 hour of PICU admission, resulting in early identification of severity of illness and stratification of children for necessary intervention.[9]
The data required for calculation of this score are easy to collect and non-proprietary. Since the data are collected at “Point-of-Care,” risk stratification can be done and mortality risk can be calculated at an early stage after ICU admission.[10]
The only limitation of this study was that the disease referral pattern and treatment facilities available reflects existing condition in our geographical area and is not applicable to other areas.
Conclusions
PIM2 score discriminated well between survival and death at PICU of this tertiary pediatric care hospital
Interventions have an impact on outcome, despite higher predicted death rate
As the PIM2 score can be done at earliest part of patient management, this will be very useful in counseling of parents
Presence of shock was significantly associated with mortality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Marik PE, Varon J. Severity scoring and outcome assessment. Computerized predictive models and scoring systems. Crit Care Clin. 1999;15:633–46. doi: 10.1016/s0749-0704(05)70076-2. [DOI] [PubMed] [Google Scholar]
- 2.Rogers J, Fuller HD. Use of daily Acute Physiology and Chronic Health Evaluation (APACHE) II scores to predict individual patient survival rate. Crit Care Med. 1994;22:1402–5. doi: 10.1097/00003246-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Wolfler A, Silvani P, Musicco M, Salvo I Italian Pediatric Sepsis Study (SISPe) Group. Pediatric Index of Mortality 2 score in Italy: A multicenter, prospective, observational study. Intensive Care Med. 2007;33:1407–13. doi: 10.1007/s00134-007-0694-z. [DOI] [PubMed] [Google Scholar]
- 4.Slater A, Shann F, Pearson G Paediatric Index of Mortality (PIM) Study Group. PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29:278–85. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 5.DiCarlo J, Frankel LR. Scoring systems and predictors of mortality. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: Saunders Publishers; 2007. p. 387. [Google Scholar]
- 6.Hariharan S, Krishnamurthy K, Grannum D. Validation of Pediatric Index of Mortality-2 scoring system in a pediatric intensive care unit, Barbados. J Trop Pediatr. 2011;57:9–13. doi: 10.1093/tropej/fmq031. [DOI] [PubMed] [Google Scholar]
- 7.Eulmesekian PG, Perez A, Minces PG, Ferrero H. Validation of pediatric index of mortality 2 (PIM2) in a single pediatric intensive care unit of Argentina. Pediatr Crit Care Med. 2007;8:54–7. doi: 10.1097/01.pcc.0000256619.78382.93. [DOI] [PubMed] [Google Scholar]
- 8.Martha VF, Garcia PC, Piva JP, Einloft PR, Bruno F, Rampon V. Comparison of two prognostic scores (PRISM and PIM) at a pediatric intensive care unit. J Pediatr (Rio J) 2005;81:259–64. [PubMed] [Google Scholar]
- 9.Qureshi AU, Ali AS, Ahmad TM. Comparison of three prognostic scores (PRISM, PELOD and PIM 2) at pediatric intensive care unit under Pakistani circumstances. J Ayub Med Coll Abbottabad. 2007;19:49–53. [PubMed] [Google Scholar]
- 10.Tibby SM, Taylor D, Festa M, Hanna S, Hatherill M, Jones G, et al. A comparison of three scoring systems for mortality risk among retrieved intensive care patients. Arch Dis Child. 2002;87:421–5. doi: 10.1136/adc.87.5.421. [DOI] [PMC free article] [PubMed] [Google Scholar]


