Abstract
Elizabethkingia meningoseptica, a ubiquitous gram-negative aerobic bacillus, is an emerging hospital acquired pathogen in patients on dialysis. It has been isolated in the hospital environment in water supplies, disinfectants, and medical devices. We present here an analysis of eight healthcare-acquired infections with this organism in adults. To the best of our our knowledge, this is the first report of infections with this organism in patients on hemodialysis.
Materials and Methods:
Over a 6-month period, eight patients were infected with E. meningoseptica in our hospital. These patients had bacteremia and lower respiratory tract infection. All these patients were on on mechanical ventilation and undergoing bedside hemodialysis in the intensive care unit (ICU). Environmental surveillance was done to detect the possible source.
Results:
These patients had a common denominator of bedside hemodialysis, and use of broad-spectrum antibiotics. E. meningoseptica was isolated from the water and sink of the ICU.
Conclusion:
E. meningoseptica is emerging as a nosocomial pathogen among patients on hemodialysis. Its unusual resistance pattern coupled with inherent resistance to colistin makes this organism difficult to treat unless susceptibility patterns are available. Isolation of this organism in handwash sink and water is a significant finding as they have been reported to survive in chlorinated water. Disinfecting the sinks and using filtered water for hand washing in critical areas may help in preventing infections with this organism.
Keywords: Colistin resistance, Elizabethkingia meningoseptica, hemodialysis
Introduction
Elizabethkingia meningoseptica is increasingly being recognized as a pathogen in hospitalized patients. It is a gram-negative, nonfermenting, nonmotile, oxidase positive bacilli growing on enriched media only.
It has been isolated from hospital water supplies, sinks, taps, saline solution used for flushing procedures, disinfectants, and medical devices, including feeding tubes, arterial catheters, and respirators. Environmental studies have revealed that the organism can survive in chlorine-treated municipal water supplies, often colonizing sink basins and taps, intubation tubes, humidifiers, incubators for newborns, ice chests and syringes, and has become a potential reservoir for infections in the hospital environment.[1,2,4]
In newborns, meningitis is the most common disease caused by this organism. Bacteremia and pneumonia are the other common manifestations in neonates. Infections usually affect premature infants and often occur as outbreaks.[5,6] Prematurity is a primary risk factor for E. meningosepticum infection. It has been implicated in meningitis, endocarditis, cellulitis, abdominal infection, wound infection, sinusitis, epididymitis, dialysis associated peritonitis, septic arthritis, and eye infections in severely immunocompromised patients such as end-stage hepatic and renal disease, extensive burns, and acquired immune deficiency syndrome, as well as community-acquired necrotizing fasciitis, pneumonia, and bacteremia.[7,8,9,10] Treatment for E. meningosepticum infections should be based on the mininimum inhibitory concentration (MIC) results from susceptibility tests.[11] Elizabethkingia spp. are resistant to multiple antibiotics, especially to β-lactams. Many possess two different types of β-lactamases, namely class A extended-spectrum β-lactamases and class B metallo-β-lactamases (MBLs); the latter confer resistance to carbapenems, which are widely used to treat infections caused by multidrug-resistant gram-negative bacteria. Two types of MBL, BlaB and GOB, have been identified in isolates of E. meningosepticum. They are constitutively resistant to multiple antibiotic classes and has unusual resistance patterns and mechanisms.[12,13,14]
Aim
A retrospective analysis of patients with this infection in our hospital and to identify the possible source of E. meningoseptica in our hospital.
Materials and Methods
Over a 6-month period, eight patients were infected with E. meningoseptica in our hospital. These patients had bacteremia and lower respiratory tract infection, attributable to ventilator-associated pneumonia.
All these patients were on mechanical ventilation and bedside hemodialysis in the intensive care unit (ICU).
Environmental surveillance swabs were collected from sinks, faucets, dialysis tubings, irrigation systems, airway humidifier vents and tubings, patient beds and dialysis machines.
Samples from the water source of the ICU and the Dialysis unit were also tested.
Hospital environmental swabs and water samples were inoculated into 5 mL trypticase soy broth and incubated for 48 hrs at 35-37°C. After 48 hrs, it was subculture on the blood agar and MacConkey agar plates and incubated for 18-24 h at 35-37°C. Moist grey, slightly hemolytic colonies on blood agar were picked up. Once confirmed as oxidase positive, further identification and susceptibility tests were done on the automated system (Vitek 2). The sensitivity of the organisms to colistin and vancomycin was also checked.
Results
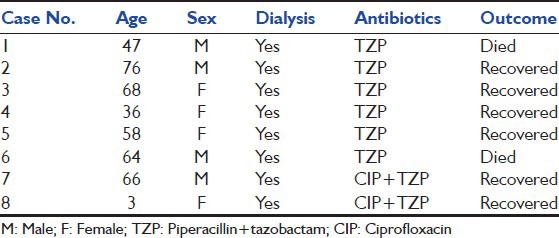
Eight cases of E. meningoseptica infections were reported in our ICU from December 2011 to June 2012. Seven patients were admitted with due to infection located in Cirrhosis of Liver (one case), Urosepsis (three cases), Dengue (two cases), ARDS (one case) and one patient was admitted for coronary artery bypass grafting. The isolates were from blood[6] and respiratory secretions.[2] The common factors among these patients were mechanical ventilation and bedside hemodialysis. The possible risk factors for colonization or infection by E. meningoseptica were evaluated [Table 1]. Of these patients, two died and the rest recovered [Table 2].
Table 1.
Frequency of possible risk factors in study patients (n=8)
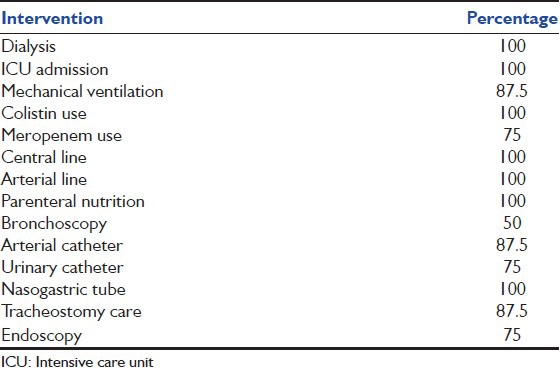
Table 2.
Outcome of the patients with Elizabethkingia meningoseptica infection (n=8)
All these patients were on colistin for multidrug-resistant bacterial infections.
Hospital environmental sampling of sixty-three swabs and thirty-five water samples was performed between April 2012 and June 2012. Water used for hand washing in the ICU and one swab from the handwash sink were the only two sources from which E. meningoseptica was isolated by environmental surveillance.[15]
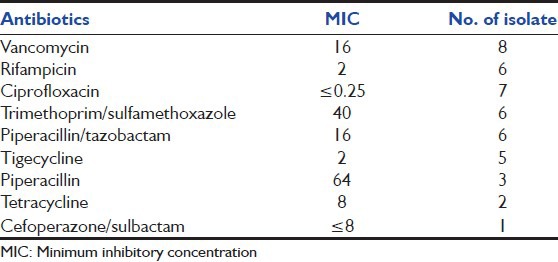
The antibiotic susceptibility pattern of the eight clinical isolates of E. meningoseptica was done on Vitek 2 [Table 3].
Table 3.
Minimum inhibitory concentrations of antibiotics tested for Elizabethkingia menigoseptica
Discussion
E. meningoseptica has been documented as a pathogen among immunocompetent neonates, but our study suggests that adult patients on mechanical ventilation and bedside hemodialysis may be more prone to this infection.
There are very few reports of E. meningoseptica infection in dialysis patients, few published from Asian countries. There are no reports of E. meningoseptica infection among patients on dialysis from India. As per our knowledge, this is the first such study on E. meningoseptica. Eight patients over a period of 6 months acquired E. meningoseptica infection in the hospital.
As compared to other studies where E. meningoseptica was a late infection, approximately after 50-70 days after admission to hospital,[16] in our study, the time interval between the admission of a patient to hospital and infection with E. meningoseptica was an average of 5 days (3-7 days).
The possible explanation for this early bacteraemia could be the presence of the organism in the tap water used for hand washing. One possible explanation for early bacteremia in the study population is the use of contaminated water for hand washing by healthcare workers. Other possibilty could be the early use of broad spectrum anitibiotics including Colistin.
E. meningoseptica has a strong predilection for extremes of age. Our patients were aged between 50 and 60 years.
In patients with bacteremia, check blood cultures performed to exclude contamination or colonization were found positive again for the organism. In patients who had pneumonia E. meningoseptica was isolated from bronchoalveolar lavage fluid.
Infections with E. meningoseptica were generally associated with a poor outcome, with a cumulative mortality of 33% among postneonates.[17]
In our study, patients had relatively lower mortality (25%) and the reason may be early detection and effective antibiotic therapy.
Patients with E. meningoseptica bacteremia have poor prognosis and use of inappropriate antibiotics further complicate the situation. All these patients had infection with multidrug resistant organisms for which colistin was being used prior to acquiring E. meningoseptica infection. The organism was resistant to most antimicrobial agents tested and developed resistance to others during treatment. Clinical and Laboratory standards Institute (CLSI) breakpoints for this organism are still not established, making the choice of antibiotic very difficult for the microbiologists as well as the clinicians. The mortality in the above-mentioned patients could also be attributed to comorbid conditions and underlying disease.
Most frequently isolated pathogen in these patients was Multi drug resistant (MDR) pseudomonas and MDR klebsiella. Pseudomonas was only sensitive to colistin and klebsiella sensitive to only colistin and tigecycline. Colistin had the strongest association with E. meningoseptica in these patients.
Colistin seems to have acted as a selective factor that allowed E. meningoseptica to emerge in the hospital. E. meningoseptica has unusual resistance patterns and mechanisms. E. meningoseptica are resistant to multiple antibiotics, especially to β-lactams. However, they show a moderate susceptibility to Piperacillin. They are also resistant to many antimicrobial classes commonly used to treat infections caused by gram-negative bacteria (aminoglycosides, chloramphenicol) but are often susceptible to agents generally used to treat infections caused by gram-positive bacteria (rifampicin, quinolones, vancomycin, trimethoprim-sulfamethoxazole). This gram-negative bacillus is vancomycin sensitive and colistin-resistant.
In our study, sensitivity rates of E. meningoseptica isolates to the antibiotics were found to be (100%) to vancomycin, (100%) to rifampicin, (87.5%) to ciprofloxacin, (75%) to trimethoprim-sulfamethoxazole, (75%) to piperacillin/tazobactam, (62.5%) to tigecycline, (37.5%) to piperacillin, (25%) to tetracycline, and (12.5%) to cefoperazone/sulbactam. Vancomycin has been previously recommended as the drug of choice for the treatment of neonatal meningitis due to E. meningoseptica.[16] However, the high MICs (16 μg/mL) of vancomycin for the organisms as demonstrated in our study as well as those of others[18] first indicate that vancomycin should not be considered the drug of choice. On the contrary, this study confirms the better activity of ciprofloxacin against E. meningoseptica infection, as has been seen in other studies.[3,19] In this study, patients were treated with a combination of ciprofloxacin with either piperacillin/tazobactam or trimethoprim-sulfamethoxazole. Two of our eight cases died despite treatment. Tigecycline, tetracycline, and rifampicin may be good alternatives as found in the susceptibility patterns in our study.
As the organism is resistant to chlorination, water from hand wash sink of the ICU was one of the environmental source in our hospital. E. meningoseptica infection was seen only in patients who were undergoing bedside hemodialysis. In addition, general infection control practices among the dialysis technicians were inconsistent, particularly hand washing and following aseptic.
E. meningosepticum often colonizes sink basins and taps, and has become a potential reservoir for infections in the hospital environment. This population of patients may become colonized after acquiring the organism from the healthcare worker and infection may occur subsequently.[20] Once microbiologist suspects this infection, clinician should immediately be informed so that appropriate antibiotic changes may be instituted early.
Clinicians need to be aware of this organism as a potential pathogen and initiate early therapy when preliminary report is informed to them.
Active infection control measures like regularly inspecting the hospital water tanks, water surveillance, and hyperchlorinating the water might be required for controlling infection with this challenging bacteria.
Further studies are required to define the epidemiology, risk factors and antimicrobial resistance patterns associated with this organism.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ceyhan M, Yildirim I, Tekeli A, Yurdakok M, Us E, Altun B, et al. A Chryseobacterium meningosepticum outbreak observed in 3 clusters involving both neonatal and non-neonatal pediatric patients. Am J Infect Control. 2008;36:453–7. doi: 10.1016/j.ajic.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Bloch KC, Nadarajah R, Jacobs R. Chryseobacterium meningosepticum: An emerging pathogen among immunocompromised adults. Report of 6 cases and literature review. Medicine (Baltimore) 1997;76:30–41. doi: 10.1097/00005792-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Chiu CH, Waddingdon M, Greenberg D, Schreckenberger PC, Carnahan AM. Atypical Chryseobacterium meningosepticum and meningitis and sepsis in newborns and the immunocompromised, Taiwan. Emerg Infect Dis. 2000;6:481–6. doi: 10.3201/eid0605.000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoque SN, Graham J, Kaufmann ME, Tabaqchali S. Chryseobacterium (Flavobacterium) meningosepticum outbreak associated with colonization of water taps in a neonatal intensive care unit. J Hosp Infect. 2001;47:188–92. doi: 10.1053/jhin.2000.0908. [DOI] [PubMed] [Google Scholar]
- 5.du Moulin GC. Airway colonization by Flavobacterium in an intensive care unit. J Clin Microbiol. 1979;10:155–60. doi: 10.1128/jcm.10.2.155-160.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nulens E, Bussels B, Bols A, Gordts B, van Landuyt HW. Recurrent bacteremia by Elizabethkingae indologenes in an oncology patient with a totally implanted intravenous device. Clin Microbiol Infect. 2001;7:391–3. doi: 10.1046/j.1198-743x.2001.00273.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee CH, Lin WC, Chia JH, Su LH, Chien C, Mao AH, et al. Community- acquired osteomyelitis caused by Chryseobacterium meningosepticum: Case report and literature review. Diagn Microbiol Infect Dis. 2008;60:89–93. doi: 10.1016/j.diagmicrobio.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Adachi A, Mori T, Simizu T, Yokoyama A, Takayama N, Ikeda Y, et al. Chryseobacterium meningosepticum septicemia in a recipient of allogeneic cord blood transplantation. Scand J Infect Dis. 2004;36:539–40. doi: 10.1080/00365540410020587. [DOI] [PubMed] [Google Scholar]
- 9.Kirby JT, Sader HS, Walsh TR, Jones RN. Antimicrobial susceptibility and epidemiology of a worldwide collection of Chryseobacterium spp: Report from the SENTRY antimicrobial surveillance program (1997-2001) J Clin Microbiol. 2004;42:445–8. doi: 10.1128/JCM.42.1.445-448.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Güngör S, Ozen M, Akinci A, Durmaz R. A Chryseobacterium meningosepticum outbreak in a neonatal ward. Infect Control Hosp Epidemiol. 2003;24:613–7. doi: 10.1086/502261. [DOI] [PubMed] [Google Scholar]
- 11.Maraki S, Scoulica E, Manoura A, Papageorgiou N, Giannakopoulou C, Galanakis E. A Chryseobacterium meningosepticum colonization outbreak in a neonatal intensive care unit. Eur J Clin Microbiol Infect Dis. 2009;28:1415–9. doi: 10.1007/s10096-009-0797-2. [DOI] [PubMed] [Google Scholar]
- 12.Bellais S, Poire L, Naas T, Girlich D, Nordmann P. Genetic biochemical analysis and distribution of the Ambler class A-lactamase CME-2, responsible for extended spectrum cephalosporin resistance in Elizabethkingae (Flavobacterium) meningosepticum. Antimicrob Agents Chemother. 2000;44:1–9. doi: 10.1128/aac.44.1.1-9.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steinberg JP, Burd EM. Other gram-negative and gram-variable bacilli. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. Philadelphia: Churchill Livingstone Elsevier; 2010. pp. 3015–33. [Google Scholar]
- 14.Chen GX, Zhang RH, Zhou W. Heterogeneity of metallo-β-lactamases in clinical isolates of Elizabethkingae meningosepticum from Hangzhou China. J Antimicrob Chemother. 2006;57:750–2. doi: 10.1093/jac/dkl019. [DOI] [PubMed] [Google Scholar]
- 15.Amer MZ, Bandey M, Bukhari A, Nemenqani D. Neonatal meningitis which was caused by Elizabethkingia meningoseptica in Saudi Arabia. J Infect Dev Ctries. 2011;5:745–7. doi: 10.3855/jidc.1570. [DOI] [PubMed] [Google Scholar]
- 16.Pereira GH, de Oliveira Garcia D, Abboud CS, et al. Nosocomial infections caused by Elizabethkingia meningoseptica: An emergent pathogen. Braz J Infec Dis. 2013;17:606–9. doi: 10.1016/j.bjid.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawley HB, Gump DW. Vancomycin therapy of bacterial meningitis. Am J Dis Child. 1973;126:261–4. doi: 10.1001/archpedi.1973.02110190231025. [DOI] [PubMed] [Google Scholar]
- 18.Chang JC, Hsueh PR, Wu JJ, Ho SW, Hsieh WC, Luh KT. Antimicrobial susceptibility of flavobacteria as determined by agar dilution and disk diffusion methods. Antimicrob Agents Chemother. 1997;41:1301–6. doi: 10.1128/aac.41.6.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Husson MO, Izard D, Bouillet L, Lecherc H. Comparative in-vitro activity of ciprofloxacin against nonfermentors. J Antimicrob Chemother. 1985;15:457–62. doi: 10.1093/jac/15.4.457. [DOI] [PubMed] [Google Scholar]
- 20.Martin K, Crisp C, Jurgensen JH. San Diego, Calif, USA: Abstract M52 in Proceedings of the Program and Abstracts of the 5th Annual meeting of the Society for Healthcare Epidemiology of America (SHEA); 1995. Outbreak of Flavobacterium meningosepticum in a surgical intensive care unit (SICU) [Google Scholar]


