Abstract
Background:
Diagnosis of cervical spine injury (CSI) is difficult in patients with an altered level of consciousness as a result of a traumatic brain injury (TBI). Patients with TBI and older adults are at increased risk for CSI. This study examined the various risk factors for CSI among trauma patients with TBI and whether adults who were older (≥55 years) were at higher risk for CSI when they sustained a fall-related TBI.
Materials and Methods:
Data used was the 2007 National Trauma Data Bank (NTDB), National Sample Project (NSP) for adults who sustained a TBI. This dataset contains 2007 admission records from 82 level I and II trauma centers. Logistic regression was used to identify potential risk factors for CSI and to test for interaction between age and injury mechanism. Additional model variables included gender, race, Glasgow Coma Score, multiple severe injuries, hypotension and respiratory distress.
Results:
An analysis of the NTDB NSP identified 187,709 adults with TBI, of which 16,078 were diagnosed with a concomitant CSI. In motor vehicle traffic injuries, the older age group had significantly higher odds of CSI (odds ratio [OR] = 1.26 [1.15-1.39]). In fall-related injuries the older age group did not have a higher odds of CSI compared to the younger age group. Skull/face fracture, other spine fracture/dislocation, upper limb injury, thorax injury, and hypotension were significantly associated with CSI. Pelvic injuries had an inverse association with CSI (OR = 0.60 [0.54-0.67]). Black had significantly higher odds of CSI compared to Whites (OR = 1.25 [1.07-1.46]).
Conclusion:
The identification of associated injuries and factors may assist physicians in evaluating CSI in patients with TBI.
Keywords: Cervical spine injury, injury mechanism, older adults, risk factors, traumatic brain injury
INTRODUCTION
The diagnosis of cervical spine injury (CSI) can be difficult in patients with multiple injuries and/or an altered level of consciousness. This difficulty can lead to a delayed or missed diagnosis of CSI.[1,2] One study revealed that the rate of overlooked CSI among traumatic brain injury (TBI) cases with a Glasgow Coma Scale (GCS) score of 8 or lower was 10.5% in 1991 and 2.3% during the years 1994-2003.[3] Due to altered level of consciousness these patients were often unable to report their neck pain. In addition, a thorough neurological examination was difficult because CSI was often associated with other acute polytrauma with life-threatening conditions, pharmacologic influences, paralysis, and alcohol.[1,4]
The optimal strategy for CSI evaluation is under debate, and existing guidelines have undergone rapid changes over the past decade. In 2000, the Eastern Association for the Surgery of Trauma (EAST) recommended anterior view cervical spine plain radiographs and supplemental computed tomography (CT) images should be reviewed.[5] If X-rays and CT images are normal, flexion/extension lateral cervical spine fluoroscopy may be necessary for a complete evaluation of the cervical spine.[5] In the 2009 version of the EAST guidelines,[6] axial CT was recommended for the evaluation of the cervical spine in patients with altered mental status. The guidelines indicated that plain radiographs do not contribute any additional information to CT.[6] Despite these guidelines, the clinical clearance of CSI is not easy and missed injuries and/or delays in diagnosis still occur. Delay in detecting CSI can lead to more damage to the spinal cord and resultant neurologic deficits due to failure to properly immobilize the patient.
Increased risk of CSI among patients with TBIs has been reported.[7] The reported incidence of CSI among patients with TBI ranges from 1.7% to 8%.[3,8,9,10] Several factors associated with CSI among patients with TBI or other injuries have been reported. Age, GCS, injury mechanism, thoracolumbosacral spine fracture, limb fracture, facial fracture, and hypotension were factors associated with CSI as identified from 41,142 TBI cases whose GCS scores were 8 or less.[3] In recognition that severe trauma can include CSI, an analysis of 8,401 motor vehicle pedestrian injuries revealed that age, severe head trauma (abbreviated injury scale [AIS] > 3), severe chest trauma (AIS > 3), pelvic fracture, and femur fracture were associated with CSI.[11] Another study revealed that GCS, motorcycle accident, and skull base fracture were associated with CSI among TBI cases where GCS was 12 or lower.[9] However, there has not been a study, which investigates CSI using nationally representative trauma data.
Older adults are especially susceptible to the risk of CSI. In a study of CSI patient's, mortality was found to be 60 times more likely in patients age 65 and older compared to patients between ages 40 and 64.[12] An increasing proportion of older adults with the spinal cord injury has also been reported over time. The proportion of patients who were age 65 or older and had CSI increased from 4.8% during 1973 to 1979 to 12.1% during 2000 to 2003 according to records of the Model Spinal Cord Injury System facilities in the US.[13] Older adults may have degenerative changes such as spondylosis, canal stenosis, and ossification of ligaments in the cervical spine. These conditions create vulnerabilities to CSI caused by low energy mechanisms, such as falls from standing height.[14,15] In CSI patients who were age 65 or older, 21.4% had spondylosis and 16.7% had cervical canal stenosis, and falls were the cause of the CSI in 71.5% of these patients.[12]
Among older adults falls is common mechanism of injury for TBI and CSI. More than 30% of adults age 70 or older fall each year.[16] Falls have been shown to be the primary cause of spinal cord injury in patients who were over age 61.[13] Among people aged 65 or older, fall-related TBI death and hospitalizations have increased with age.[17] An increasing proportion of population over 65 years old, combined with a higher risk for fall injury in this age group and degenerative changes of the spine among older adults may lead to an increase in overall CSI.[18]
There are challenges in diagnosing CSI among TBI patients and a risk of delayed diagnosis. The primary purpose was to describe potential risk factors associated with CSI among trauma patients with TBI. The secondary purpose was to investigate the interaction between age and injury mechanism and to examine whether older adults are at increased risk for CSI when they sustain a fall-related TBI.
MATERIALS AND METHODS
Data from the 2007, National Trauma Data Bank (NTDB), National Sample Project (NSP) was used to identify patients for this retrospective cross sectional study.[19] The NTDB NSP is a stratified sample of trauma centers (TCs) that includes data from 47 level I and 35 level II TCs with the intent to produce nationally representative estimates of level I and II TCs activity. The strata were based on NTDB participation, trauma level, and region and can be reviewed in this publication.[19] The weighting of the NTDB NSP was based on a total of the 453 level I and II TCs.[20]
The 2007 NTDB NSP contains 148,270 total unweighted trauma records for all ages. TBI is caused by a bump, blow or jolt to the head or a penetrating head injury that disrupts the normal functioning of the brain. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes 800-801, 803-804, 850-854.1, 950.1-950.3, 995.55, and 959.01 were used in this study to define TBI, which is consistent with the definition used by the Centers for Disease Control and Prevention (CDC).[21] Cases that were excluded from this study were those without an ICD-9-CM diagnosis code or age information, those declared dead on arrival with minimal or no resuscitation attempt and those younger than 18 years old. The outcome variable was CSI that included cervical spine fracture, dislocation and/or spinal cord injury without fracture or dislocation. The ICD-9-CM codes used to identify CSI were: 805.00-805.18, 806.00-806.19, 839.00-839.18, and 952.00-952.09.[3]
Age, sex, race, mechanism of injury, total GCS at emergency department (ED), injury severity score (ISS), concomitant skull, and face fractures (vault, base or face fractures), other spine fracture and/or dislocation (i.e., thoracic, lumber, sacrum or coccyx), upper extremity fracture and/or dislocation (upper extremity injury), lower extremity fracture and/or dislocation (lower extremity injury), pelvic fracture and/or dislocation (pelvic injury), thorax fracture and/or dislocation (thorax injury), hypotension in ED and respiratory distress in ED were evaluated as potential risk factors. Consistent with the guidelines for field triage of injured patients published by the CDC, hypotension was defined as systolic blood pressure lower than 90 mmHg, and respiratory distress was defined as fewer than 10 or more than 29 breaths/min.[22]
The risk of death in adults due to injury increases after age 55 years;[22] thus, age was categorized into two levels: 18-54 years old and 55 years or older. Race was categorized into 4 groups: White, Black, Asian, and other. Mechanisms of injury included were “motor vehicle traffic (MVT),” “falls,” “assault,” “struck by and against,” and “other and unspecified” based on the external cause codes.[20] Three GCS categories were defined: (severe: ≤8), (moderate: 9-12) and (mild: 13-15).[2,23,24]
A descriptive analysis was carried out in order to understand the proportions of CSI by demographic variables. A univariate analysis was carried out with potential risk factors (age, sex, race, injury mechanism, GCS category, ISS, skull/face fracture, other spine fracture/dislocation, upper extremity injury, lower extremity injury, pelvic injury, thorax injury, hypotension and respiratory distress), and then logistic regression models were run to identify the risk factors for CSIs. The interaction between age and injury mechanism was assessed using a likelihood ratio test. Odds ratio (OR) for CSI and corresponding 95% confidence interval (CI) was calculated. Statistical analysis was performed using the SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
The 2007 NTDB NSP contained 148,270 records, which represented 630,645 weighted trauma cases. Of the 630,645 cases, three cases (0.0005%) did not have a diagnosis code, 976 (0.15%) were declared dead on arrival and 79,432 (12.60%) cases were younger than 18 years old or age was missing. Among the remaining 550,313 trauma cases, 187,709 (34.1%) had TBI and were included in this study. The proportion of CSI among those TBI cases among the study population was 8.6% and significantly higher than in trauma cases without TBI (8.6% vs. 5.9%, Wald χ2 = 42.76, P < 0.001).
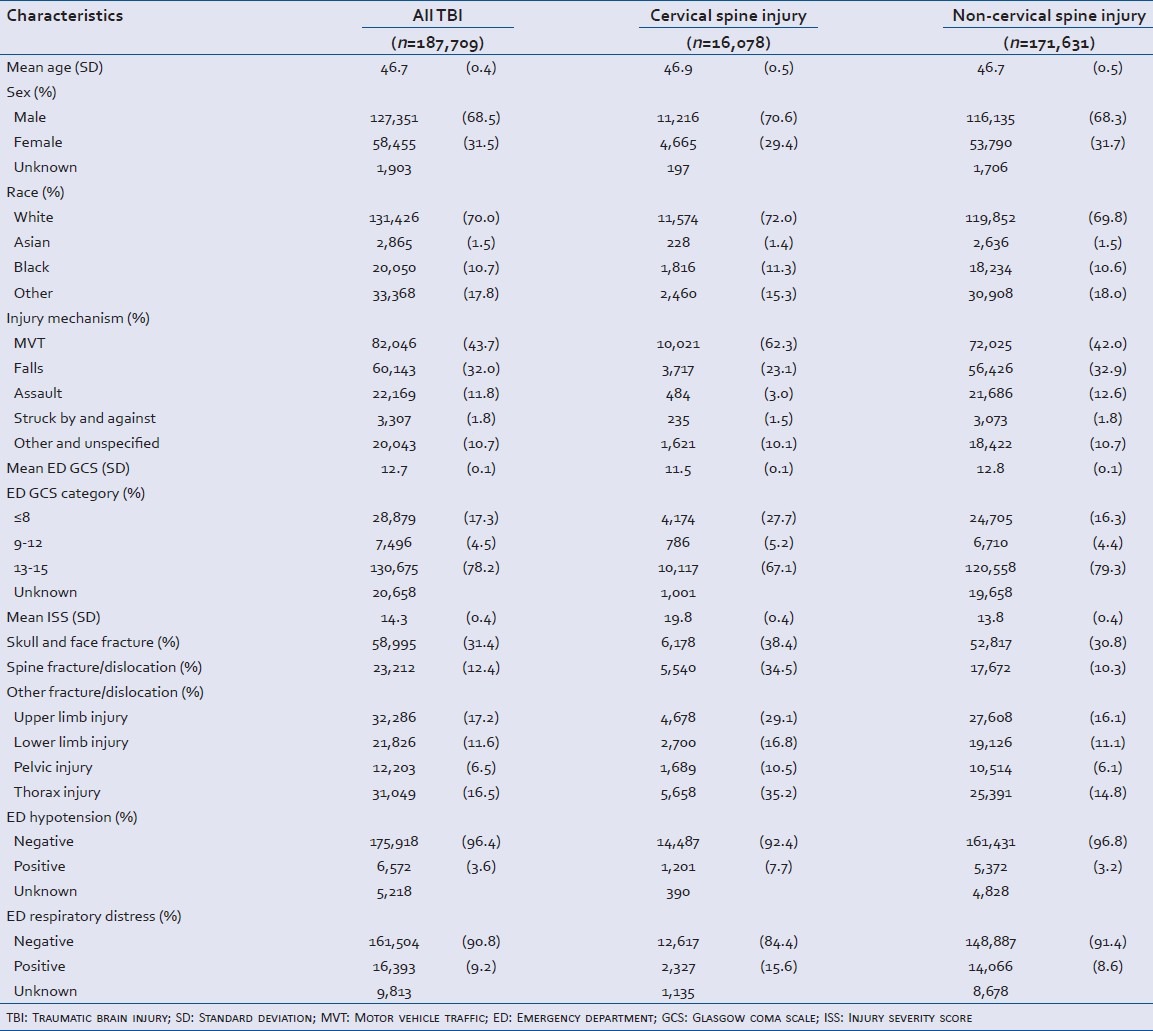
Characteristics of TBI cases in the present study are shown in Table 1. Among these TBI cases, the mean age was 46.7 years, 69% were males, and 70% were White. Nearly, 44% had MVT and 32% had fall-related injuries and the mean GCS was 12.7 and mean ISS was 14.3. Among these TBI patients, 31% had skull/face fractures. Nearly, 12% had other spine fracture/dislocation, 17% had upper limb injury, 12% had lower limb injury, 7% had pelvic injury, and 17% had thorax injury. Among them 3.6% had hypotension and 9.2% had respiratory distress.
Table 1.
Characteristics of traumatic brain injury cases (n=187,709), National Trauma Data Bank, National Sample Project, 2007
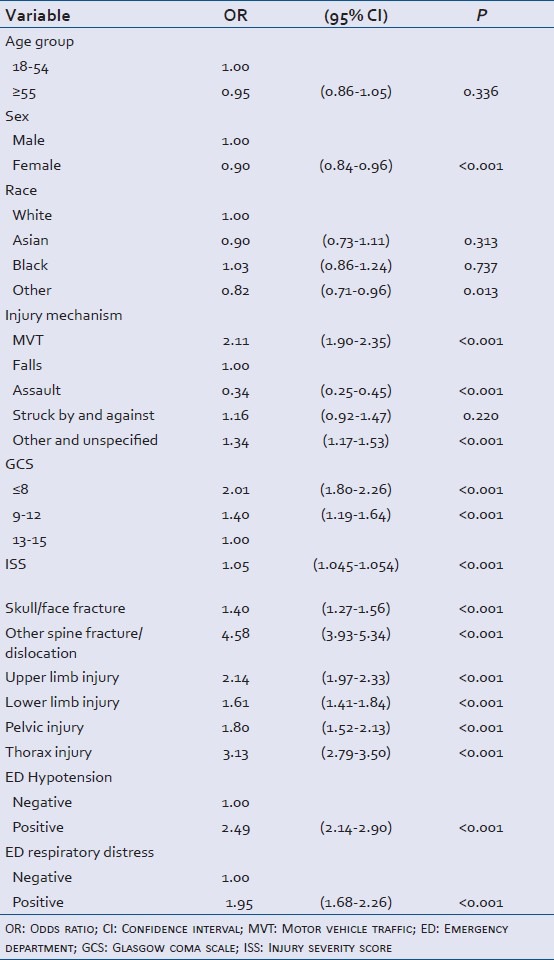
Age group was not significant in univariate analysis [Table 2]. Females had a significantly lower odds of CSI than males (OR = 0.90, 95% CI [0.84, 0.96]). Other races had significantly a lower odds of CSI than Whites (OR = 0.82, 95% CI [0.71, 0.96]). Patients with MVT injuries had significantly a higher odds of CSI compared to falls (OR = 2.11, 95% CI [1.90, 2.35]). The assault mechanisms of injury had a significantly lower odds of CSI compared to falls (OR = 0.34, 95% CI [0.25, 0.45]). Other and unspecified mechanisms had significantly a higher odds of CSI compared to falls (OR = 1.34, 95% CI [1.17, 1.53]). GCS score 8 or lower and GCS score 9-12 categories had a significantly higher OR compared to GCS 13-15 (OR = 2.01, 95% CI [1.80, 2.26] in GCS 8 or lower; OR = 1.40, 95% CI [1.19, 1.64] in GCS 9-12). Higher ISS was associated with a significantly higher odds of CSI (OR = 1.05, 95% CI [1.05, 1.05]). Skull/face fracture (OR = 1.40, 95% CI [1.27, 1.56]), other spine fracture/dislocation (OR = 4.58, 95% CI [3.93, 5.34]), upper limb injury (OR = 2.14, 95% CI [1.97, 2.33]), lower limb injury (OR = 1.61, 95% CI [1.41, 1.84]), pelvic injury (OR = 1.80, 95% CI [1.52, 2.13]), and thorax injury (OR = 3.13, 95% CI [2.79, 3.50]) were all associated with a significantly higher OR of CSI. Those who had hypotension or respiratory distress had a significantly higher OR of CSI (OR = 2.49, 95% CI [2.14, 2.90] in hypotension; OR = 1.95, 95% CI [1.68, 2.26] in respiratory distress).
Table 2.
Univariate analysis of the association between the potential risk factors and cervical spine injury among traumatic brain injury cases (n=187,709), National Trauma Data Bank, National Sample Project, 2007
A logistic regression model was fitted with the following variables: Age group, sex, race, injury mechanism, GCS categories, skull/face fractures, other spine fracture/dislocation, upper limb injury, lower limb injury, pelvic injury, thorax injury, hypotension, and respiratory distress to identify independent risk factors for CSI controlling for other risk factors.
There was significant interaction between the age and injury mechanism (χ2 = 29.22, P < 0.001). The results from the model with interaction of age with injury mechanisms are shown in Table 3. For injury mechanism, MVT had a significantly higher odds of CSI compared to falls in both age groups (adjusted OR [aOR] = 1.49, 95% CI [1.19, 1.85] in younger (18-54 years); aOR = 1.63, 95% CI [1.44, 1.84] in older [≥55 years]). Assault had significantly a lower OR of CSI compared to falls in both age groups (aOR = 0.33, 95% CI [0.25, 0.45] in younger; aOR = 0.35, 95% CI [0.18, 0.68] in older). “Struck by and against” and “other and unspecified” had a significantly higher OR of CSI compared to falls only in the older age group (aOR = 1.93, 95% CI [1.13, 3.28] for “struck by and against; aOR = 1.25, 95% CI [1.02, 1.52] for “other and unspecified"). Among patients with the MVT, the older age group had a significantly higher OR of CSI (aOR = 1.26, 95% CI [1.15, 1.39]) compared to the younger group. There were no significant differences in odds of CSI between the younger and older age groups for the mechanisms of injury of falls and assault. The older age group had a significantly higher odds of CSI with the “struck by and against” (aOR = 2.57, 95% CI [1.44, 4.57]).
Table 3.
Multiple logistic regression analysis of the association between potential risk factors and cervical spine injury among traumatic brain injury cases (n=187,709), National Trauma Data Bank, National Sample Project, 2007
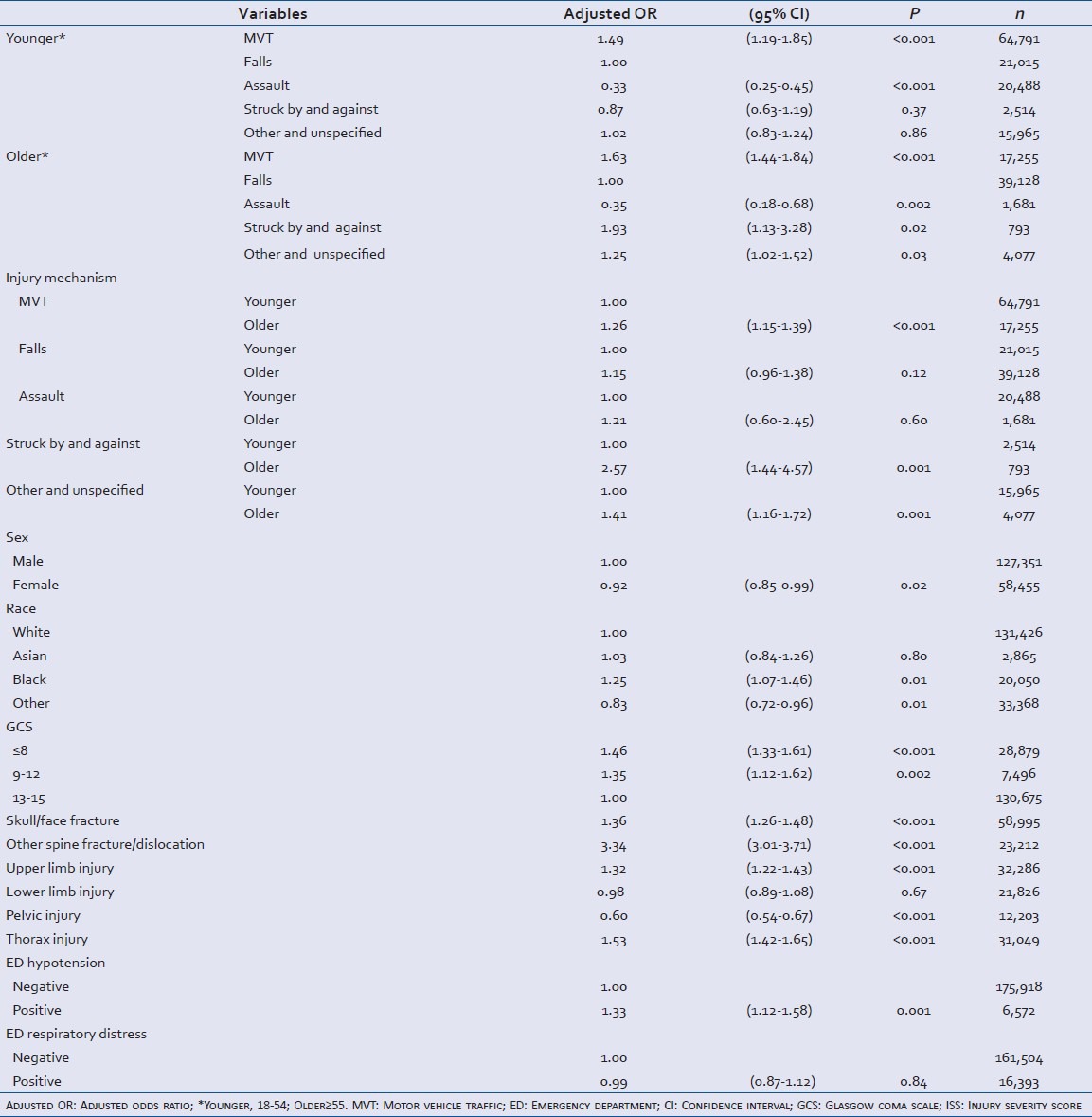
Females had significantly a lower OR of CSI (aOR = 0.92, 95% CI [0.85, 0.99]). Black had significantly higher odds of CSI compared to Whites (aOR = 1.25, 95% CI [1.07, 1.46]). The “other race” category had a significantly lower OR of CSI compared to Whites (aOR = 0.83, 95% CI [0.72, 0.96]). A GCS score of 8 or lower (aOR = 1.46, 95% CI [1.33, 1.61]) and GCS sore 9-12 (aOR = 1.35, 95% CI [1.12, 1.62]) were associated with a significantly higher OR of CSI compared to GCS 13-15. Skull/face fractures (aOR = 1.36, 95% CI [1.26, 1.48]), other spine fracture/dislocation (aOR = 3.34, 95% CI [3.01, 3.71]), upper limb injury (aOR = 1.32, 95% CI [1.22, 1.43], thorax injury (aOR = 1.53, 95% CI [1.42, 1.65]) were all associated with a higher odds of CSI. Cases with pelvic injuries had a significantly lower odds of CSI than cases without pelvic injuries (aOR = 0.60, 95% CI [0.54, 0.67]). Lower limb injury did not have a significant association with CSI. Hypotension was associated with a significantly higher odds of CSI (aOR = 1.33, 95% CI [1.12, 1.58]). Respiratory distress was not a significant predictor of CSI.
DISCUSSION
GCS, skull/face fractures, other spine fracture/dislocation, upper limb injury, thorax injury, and hypotension were significantly associated with CSI among cases with TBI, which is consistent with former studies.[3,9] These results, which emerged from nationally representative data may assist physicians in an ED in identifying TBI patients at higher risk for CSI and consider further tests for cervical spine protection.
Patients with pelvic injuries had significantly lower odds of CSI when controlling for other variables. This result is contrary to the literature where pelvic fracture increased incidence of CSI among pedestrians hit by automobiles regardless of brain injury.[11] In the current study, lower spine fracture/dislocation was associated with higher odds of CSI and hence it is interesting that fracture and/or dislocation of pelvis, which is adjacent to lumbar spine was associated with decreased odds of CSI. A pelvic injury may absorb energy and have protective effects against a CSI. Further biomechanical studies are needed to explore this finding.
Among TBI patients in this study, Black had significantly higher odds of CSI compared to Whites. Race was identified as a risk factor for CSI. The National Emergency X-Radiography Utilization Study (NEXUS) collected demographic information on all patients with blunt trauma who underwent cervical spine radiography in the participating EDs. These authors reported that the risk for CSI was the highest among Whites and the lowest among African American patients.[25] The difference could be the result of study design and sampling because the NEXUS study population consisted of patients who underwent radiography at the discretion of the treating physician. Furthermore, the sample used in the present study consisted of patients who were taken to level I or level II TCs, suggesting that these patients may be more seriously injured than the patients in the NEXUS study. Future studies should also examine differences between the races by controlling for other variables such as personal protective devices (i.e., seat belts or helmets).
Lower GCS was associated with higher odds of CSI among TBI cases. The practice of using GCS as a severity indicator can be inaccurate because of patient sedation, pharmacological influences, paralysis, alcohol and/or intubation. In future studies, a model controlling for overall ISS needs to be compared a model controlling for GCS to determine effectiveness of the two severity measures.
There was an overall interaction between age and injury mechanism. There was a difference in the effect of age between the MVT injury and fall-related injury. Older patients had significantly higher odds of CSI in MVT injury but in injuries with falls, the effect of age was not significant. However, it is possible that a diagnosis of CSI was missed, because of a low energy mechanism type injury. Mild CSI in older adults who may have a TBI can be missed initially because they may not be able to describe their symptoms or they may have some physical impairment. In such a scenario, these individuals would be underrepresented in the NTDB NSP.
This study revealed various risk factors for CSI among TBI cases and the interaction between age and injury mechanisms, which may help physicians to identify the patient at higher risk of CSI. The results from this study using the NTDB NSP allow for more generalizability than studies using the data from a single or even several TCs.
Limitations
Because data collected for the NTDB NSP were reported by each TC voluntarily, the data may not be random. Data for this study were from trauma registries, so detailed descriptions of CSI were not available.
Personal protective devices also impact CSI risk. Seat belt use has been reported to be associated with lower odds of CSI in MVT injury.[26] Controlling for the use of protective devices might affect the association between other risk factors [Tables 2 and 3] and CSI. However, use of personal protective devices was not examined in the present study because only 7,669 records out of 148,270 contained information about protective devices. Improved reporting of the use of personal protective devices will lead to better future studies.
Arguably, hypotension or respiratory distress caused by CSI might have been reversed by emergency medical service (EMS) personnel at the scene. In addition, hypotension or respiratory distress identified in the pre-hospital setting could alert health-care providers to the potential risk of CSI. However, systolic blood pressure and respiratory rate measurements in ED were used rather than those provided by EMS in this study because systolic blood pressure and respiratory rate in EMS were missing in 50% of records.
CONCLUSIONS
Among TBI patients, the older age group had significantly higher odds of CSI compared to the younger age group in MVT injuries. Pelvic injuries had an inverse association with CSI. Skull/face fractures, other spine fracture/dislocation, upper limb injury, thorax injury, and hypotension were all associated with higher odds of CSI. There was significant difference across race categories in odds of CSI: Higher in Black patients. These factors associated with CSI may assist physicians in evaluating CSI among TBI patients with an altered level of consciousness. Higher risk patients for CSI include older adults who suffer a TBI from MVT injury or TBI patients with other injuries in upper limbs or thorax.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
ACKNOWLEDGMENT
We gratefully acknowledge the editorial advice and information received by Jeneita Bell, MD. Her assistance helped produce a more detailed manuscript.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Platzer P, Hauswirth N, Jaindl M, Chatwani S, Vecsei V, Gaebler C. Delayed or missed diagnosis of cervical spine injuries. J Trauma. 2006;61:150–5. doi: 10.1097/01.ta.0000196673.58429.2a. [DOI] [PubMed] [Google Scholar]
- 2.Demetriades D, Charalambides K, Chahwan S, Hanpeter D, Alo K, Velmahos G, et al. Nonskeletal cervical spine injuries: Epidemiology and diagnostic pitfalls. J Trauma. 2000;48:724–7. doi: 10.1097/00005373-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Piatt JH., Jr Detected and overlooked cervical spine injury among comatose trauma patients: From the Pennsylvania trauma outcomes study. Neurosurg Focus. 2005;19:E6. doi: 10.3171/foc.2005.19.4.7. [DOI] [PubMed] [Google Scholar]
- 4.Laurer H, Maier B, Saman AE, Lehnert M, Wyen H, Marzi I. Distribution of spinal and associated injuries in multiple trauma patients. Eur J Trauma Emerg Surg. 2007;33:476–81. doi: 10.1007/s00068-007-7124-3. [DOI] [PubMed] [Google Scholar]
- 5.Marion D, Domeier R, Dunham CM, Luchette F, Haid R, & Erwood SC. Determination of cervical spine stability in trauma patients (update of the 1997 EAST cervical spine clearance document) East Assoc Surg Trauma (EAST) 2000:1–9. [Google Scholar]
- 6.Como JJ, Diaz JJ, Dunham CM, Chiu WC, Duane TM, Capella JM, et al. Practice management guidelines for identification of cervical spine injuries following trauma: Update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. 2009;67:651–9. doi: 10.1097/TA.0b013e3181ae583b. [DOI] [PubMed] [Google Scholar]
- 7.Hills MW, Deane SA. Head injury and facial injury: Is there an increased risk of cervical spine injury? J Trauma. 1993;34:549–53. [PubMed] [Google Scholar]
- 8.Holly LT, Kelly DF, Counelis GJ, Blinman T, McArthur DL, Cryer HG. Cervical spine trauma associated with moderate and severe head injury: Incidence, risk factors, and injury characteristics. J Neurosurg. 2002;96(Suppl 3):285–91. doi: 10.3171/spi.2002.96.3.0285. [DOI] [PubMed] [Google Scholar]
- 9.Tian HL, Guo Y, Hu J, Rong BY, Wang G, Gao WW, et al. Clinical characterization of comatose patients with cervical spine injury and traumatic brain injury. J Trauma. 2009;67:1305–10. doi: 10.1097/TA.0b013e31819db57c. [DOI] [PubMed] [Google Scholar]
- 10.Bayless P, Ray VG. Incidence of cervical spine injuries in association with blunt head trauma. Am J Emerg Med. 1989;7:139–42. doi: 10.1016/0735-6757(89)90125-3. [DOI] [PubMed] [Google Scholar]
- 11.Yanar H, Demetriades D, Hadjizacharia P, Nomoto S, Salim A, Inaba K, et al. Pedestrians injured by automobiles: Risk factors for cervical spine injuries. J Am Coll Surg. 2007;205:794–9. doi: 10.1016/j.jamcollsurg.2007.06.280. [DOI] [PubMed] [Google Scholar]
- 12.Spivak JM, Weiss MA, Cotler JM, Call M. Cervical spine injuries in patients 65 and older. Spine (Phila Pa 1976) 1994;19:2302–6. doi: 10.1097/00007632-199410150-00009. [DOI] [PubMed] [Google Scholar]
- 13.Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Arch Phys Med Rehabil. 2004;85:1740–8. doi: 10.1016/j.apmr.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 14.Nakae R, Onda H, Yokobori S, Araki T, Fuse A, Toda S, et al. Clinical analysis of spinal cord injury with or without cervical ossification of the posterior longitudinal ligament, spondylosis, and canal stenosis in elderly head injury patients. Neurol Med Chir (Tokyo) 2010;50:461–5. doi: 10.2176/nmc.50.461. [DOI] [PubMed] [Google Scholar]
- 15.Lomoschitz FM, Blackmore CC, Mirza SK, Mann FA. Cervical spine injuries in patients 65 years old and older: Epidemiologic analysis regarding the effects of age and injury mechanism on distribution, type, and stability of injuries. AJR Am J Roentgenol. 2002;178:573–7. doi: 10.2214/ajr.178.3.1780573. [DOI] [PubMed] [Google Scholar]
- 16.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–6. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 17.Thomas KE, Stevens JA, Sarmiento K, Wald MM. Fall-related traumatic brain injury deaths and hospitalizations among older adults — United States, 2005. J Safety Res. 2008;39:269–72. doi: 10.1016/j.jsr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 18.He W, Sengupta M, Velkoff VA, DeBarros KA. Washington, DC: US Government Printing Office; 2005. 65+ in the United States: Current population report. US Census Bureau. [Google Scholar]
- 19.The American College of Surgeons. Creation of the National Sample National Sample Project of the National Trauma Data Bank (NTDB) 2007. [Cited 2012 Aug 1]. Available from: http://www.facs.org/trauma/nsp/samplecreation.pdf .
- 20.Goble S, Neal M, Clark DE, Nathens AB, Annest JL, Faul M, et al. Creating a nationally representative sample of patients from trauma centers. J Trauma. 2009;67:637–42. doi: 10.1097/TA.0b013e3181b84294. [DOI] [PubMed] [Google Scholar]
- 21.Faul M, Xu L, Wald MM, Coronado VG. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths, 2002-2006. [Google Scholar]
- 22.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, et al. Guidelines for field triage of injured patients: Recommendations of the National expert panel on field triage, 2011. MMWR Recomm Rep. 2012;61:1–20. [PubMed] [Google Scholar]
- 23.Esselman PC, Uomoto JM. Classification of the spectrum of mild traumatic brain injury. Brain Inj. 1995;9:417–24. doi: 10.3109/02699059509005782. [DOI] [PubMed] [Google Scholar]
- 24.Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT, et al. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25:719–38. doi: 10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lowery DW, Wald MM, Browne BJ, Tigges S, Hoffman JR, Mower WR, et al. Epidemiology of cervical spine injury victims. Ann Emerg Med. 2001;38:12–6. doi: 10.1067/mem.2001.116149. [DOI] [PubMed] [Google Scholar]
- 26.Thompson WL, Stiell IG, Clement CM, Brison RJ, Canadian C. Association of injury mechanism with the risk of cervical spine fractures. Journal of the Canadian Association of Emergency Physicians. 2009;11:14. doi: 10.1017/s1481803500010873. [DOI] [PubMed] [Google Scholar]


