Abstract
Background:
In the context of inadequacy of neurology workforce in India, it is important to understand factors that post-graduate medical students consider for and against choosing neurology as their career option. Understanding these factors will help in planning strategies to encourage students to pursue a career in neurology. At present, there is a paucity of studies addressing this issue in India.
Aims and Objectives:
(1) To analyze factors, which post-graduate students consider for and against choosing neurology as a career specialty. (2) To access the level and quality of neurology exposure in the current MBBS and MD curricula.
Materials and Methods:
Statewide questionnaire based study was conducted in the state of Maharashtra for students eligible to take DM neurology entrance examination (MD Medicine and MD Pediatrics).
Results:
In this survey, 243 students were enrolled. Factors bringing students to neurology were - intellectual challenge and logical reasoning (72%), inspired by role model teachers (63%), better quality-of-life (51%) and scope for independent practice without expensive infrastructure (48%). Factors preventing students from taking neurology were - perception that most neurological diseases are degenerative (78%), neurology is mainly an academic specialty (40%), neurophobia (43%) and lack of procedures (57%). Inadequate exposure and resultant lack of self-confidence were common (31%, 70-80%). 84% of the students felt the need for a short term certification course in neurology after MD.
Conclusions:
To attract more students to neurology, “role model” teachers of neurology could interact and teach students extensively. Neurologists’ efforts to shed their diagnostician's image and to shift their focus to therapeutics will help change the image of neurology. Out-patient neurology clinics should be incorporated early in the student's career. Procedures attract students; hence, they should be made conversant with procedures and interventions. Increasing the level of neurological exposure in our current MBBS and MD curriculum is necessary. A case could be made for consideration of short certification course in neurology for physicians.
Key Words: Career, neurology, postgraduate, students
Introduction
Neurology took roots in India almost six decades ago.[1,2] Even after 62 years of establishment of Neurological Society of India[1] and later, the Indian Academy of Neurology, there are less than 1000 Neurologists in our country with a ratio of one Neurologist/1,250,000 Indians.[3] In face of this inadequacy, knowledge base of neurological disorders has progressed very rapidly and sub specialties have evolved. With these changes, it is clear that for the maintenance and adequate functioning of future neurology health-care system in India, there is an urgent need to increase the neurology workforce.[4] In this context, it is essential to assess factors determining career choices of our young post-graduate MD students. A systematic search of PubMed articles revealed lacunae in Indian studies assessing students’ attitudes and perceptions toward neurology as their career option. This study was undertaken to analyze and understand various factors, which students consider for and against choosing neurology as their career specialty after MD. The analysis of factors influencing career choice can be used to modify student desires, medical education curricula and job satisfaction of prospective Neurologists, to better match population needs.[5,6]
Materials and Methods
Design and participants
We conducted a statewide questionnaire based prospective study in the state of Maharashtra. Total of 243 postgraduate medical student with 179 males and 64 females, who are currently enrolled for MD (Internal Medicine) and MD (Pediatrics) degree course in various medical colleges under Maharashtra University of Health Sciences were included in this study. As per the data available from websites of Ministry of Health and Family Welfare, Medical Council of India (MCI) and Directorate of Medical Education and Research there are approximately 500 seats of MD Internal Medicine and MD Pediatrics in the state of Maharashtra and our sample represents approximately 49% of this population. We included MD (Internal Medicine) as well as MD (Pediatrics) as students of both these specialties are further eligible for DM (Neurology).
Materials
A structured 13-item questionnaire was designed to examine the student's attitude toward neurology as their future career option. Questionnaire was administered in English language and validation of the questionnaire was done by using standard procedure on proportionate sample size. Questions were designed to get insight in to various reasons and factors to consider or reject neurology as their career, the level of neurological exposure they got during their graduation and post-graduation, confidence in handling common neurological problems and ways to improve their neurological skills and exposure.
Procedure
Survey was conducted by a single observer visiting medicine and pediatrics department of various medical colleges of Mumbai, Pune, Sholapur, Miraj and Thane district. Self-administered questionnaire was given to students who were present at the time of visit. Before inclusion into the study, all participants were assured that taking part in this study is voluntary and their anonymity was guaranteed.
Results
Of 243 students enrolled in our study, 179 (74%) were males and 64 (26%) were females. While all students wanted to specialize in one of the six available specialties (Neurology, Cardiology, Gastroenterology, Endocrinology, Hemato-oncology and Nephrology), 19% of the students chose neurology as their first career choice, additional 16% kept neurology as 2nd choice and 18% considered neurology to be the their last career option. Result of assessment of reasons for students opting for neurology as their career are documented in Figure 1 and analysis of factors that take students away from neurology are documented in Figure 2.
Figure 1.
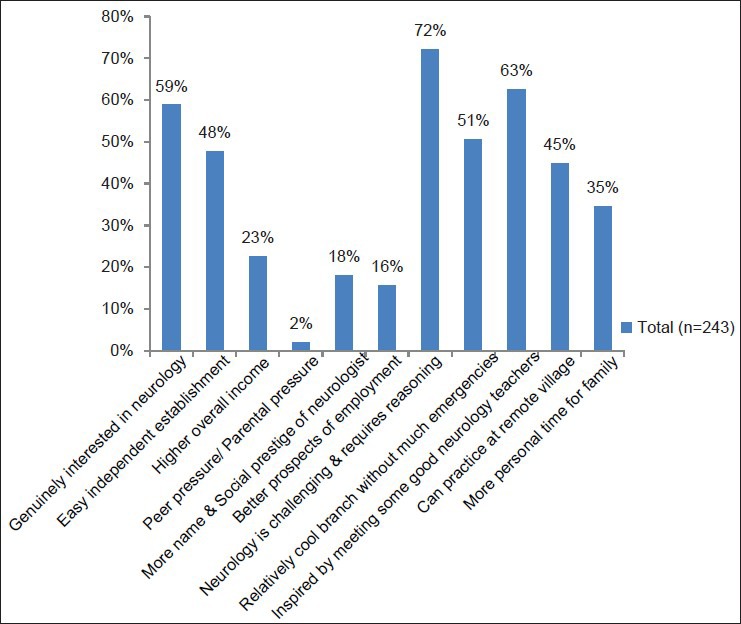
Factors for choosing neurology as career option
Figure 2.
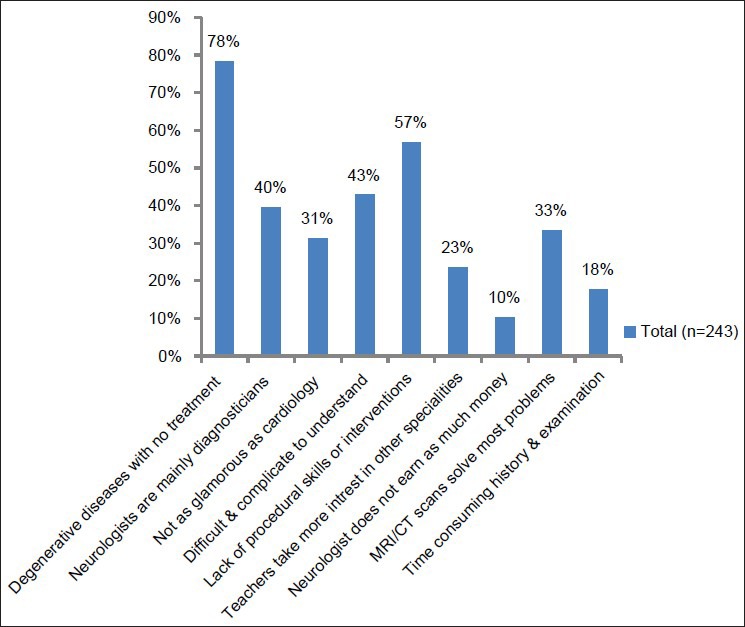
Factors for not choosing neurology as a career option
When the two groups of students (neurology as 1st option and as the last option) were contrasted, the challenge that neurology posed was of importance (89%) and scored over the limited reversibility of neurological disorders. And reverse was the perception in those wanting to stay away from the neurology.
Around, 60% of students reported insufficient neurology exposure in various conferences and continuing medical education programs that they have attended. Nearly, one-third of students (31%) also felt that exposure to neurology was below average in our current MBBS and MD curriculum.
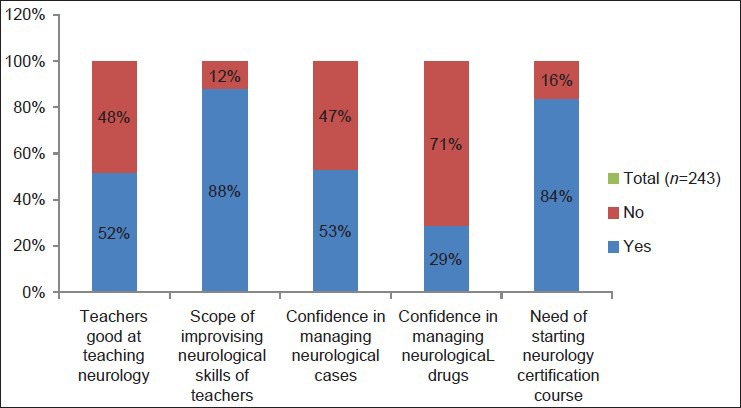
Response to open labeled questions for evaluating the level and quality of neurological exposure given to students in their MBBS and MD curriculum are given in Figure 3. For starting short-term (12 months) certification course in neurology after post-graduation, 84% of the students felt it will be very useful to them for better understanding and management of neurological cases.
Figure 3.
Level of neurological exposure and teaching during MBBS and MD curriculum
Discussion
Neurology was the first career option in 19% of students, suggesting that neurology is generally well-regarded by students.
Analyzing the factors that bring them to neurology reveal two prominent reasons, namely, intellectual challenge and logical reasoning that is the basis of neurology (72%) and role model impact (63%). Students were inspired and developed an interest in neurology after coming in contact with or listening to famous neurology teachers. Both these factors have consistently been shown to be of importance to residents for choosing their specialty.[7,8] Jan and Fida point out that students who have been taught by a qualified Pediatric Neurologist are more likely to view this specialty as interesting and challenging and considered it as their future career option. In a study by Gaucher and Thabut teaching was the determinant for specialty choice in 74% of the students. In this study, interestingly, the teacher did not belong to the university campus in almost half instances.[9] Hence, teaching of students by “role model” Neurologists is one factor that should be seriously looked into to promote students for taking neurology as a career.
Literature suggests that most medical students make their specialty career choices quite early in their medical training mostly during third and 4th year clinical rotation of MBBS.[10] Hence, neurology is at a disadvantage, because MBBS students hardly ever come in contact with neurology faculty. The neurology exposure in our current MBBS and MD curriculum and in CME programs was considered as inadequate by 30-60% of students. Hence, early exposure to neurology needs to be promoted.
Other important reasons for considering neurology were controllable life-style with better quality-of-life (51%) in neurology as compared with other specialties, family time (35%) and rapid establishment of independent practice without expensive infrastructure (48%). Interestingly, above mentioned considerations superseded income and prestige issues. These findings match entirely with that of Schwartz et al., who found these factors uniformly affecting all specialties.[11] In our study, almost half of the students felt that better quality-of-life as one of the important factor for entering this specialty, but we are likely to lose this attraction very soon. Our Neurologists are already overburdened with patient care with just 1100 qualified Neurologist (approximate) to look after population of more than 1 billion[4] and this workload is likely to rise exponentially with gross inadequacy of institutes providing neurology training in our country.[3,12] Hence, there is an urgent need for increasing the training facilities in neurology to maintain job satisfaction of our doctors.
It is interesting that 16% of participants considered neurology as their second choice. This group of students can be attracted toward neurology further if some of the reasons that are preventing them from keeping neurology as their first choice can be addressed.
On analyzing the factors preventing students from taking neurology as their career, it was striking that students (78%) perceived neurological diseases as degenerative, without concrete treatment options. This seems to be direct reflection of lack of exposure to out-patient neurology. Patients with rare syndromes and degenerative disease with severe locomotor or cognitive disabilities get admitted in neurology wards. And, it is these patients on whom our students learn the art of history taking and practice clinical skills, but along with this probably they also make subconscious impression that most of the neurological disorders are untreatable.[13] Common neurological diseases such as headaches, vertigo, epilepsy and neuropathy are often treated only on the out-patient basis with good treatment response. Since under graduates and in many institutes even post-graduates hardly ever get the chance to see profile and treatment response of patients in neurology out-patient clinics, this greener side of neurology goes unappreciated. So, there is a need to expose students to outpatient clinics, early in their medical career when they are more impressionable.
Other major culprits in deterring students away from neurology were the perceptions that neurology is an academic specialty and Neurologists are mainly diagnosticians (40%). The Neurologist's image in the students’ mind seems to be that described by British Medical Journal editor “brilliant forgetful man with bulging cranium who adores diagnosis and rare syndromes and most importantly never bothers about treatment.”[14] This image of Neurologist, to some extent, is enhanced by its ranks taking pride and cherishing their image as professionals on whose opinion others depend.[13] In last decade, tremendous growth and development has taken place in the field of neurology, in particular neuroimmunology and neurogenetics, which has widened the therapeutic umbrella of disease modifications, cure and possibly prevention of diseases for the Neurologists.[12] It is high time that we actively shed this image of being diagnosticians and shift our focus to available therapeutic options in interactions with students.
Neurophobia[15] among students, i.e., perception that neurology is a difficult and complicated subject to understand (43%) is a common problem world-wide that pushes students away from this specialty.[13] Neurologists are partially responsible in perpetuating this myth that neurology is a specialty “for which only young Einsteins need apply”.[13,16] Ridsdale et al. pointed to the fact that neurophobia begins quite early in the medical career of students. Authors attributed this to the bombardment of information of basic neurosciences and neuroanatomy in such details that turns the students “off,” particularly at a time when they have no exposure to clinical neurology.[13] Furthermore, minute details of basic neurosciences are often irrelevant to clinical neurology.[17] Menken M in his editorial affirms Morris B Bender's suggestion that our teaching approach from basic neurosciences to clinical neurology is becoming dysfunctional and consideration should be given to develop a new approach where neurology exposure to student starts with clinical signs and phenomenology following, which explanations and reasons to save that phenomenon comes.[18] Hence, there is need to design a teaching model that allows more effective integration of basic neurosciences with that of clinical neurology with stress on most basic and simple concepts, introducing clinical neurology exposure in early years of medical studies.
At present, the subject of neurology is covered by non-neurologists in most medical colleges, which students find inadequate. In our study, 48% of the students thought that their teachers are not as good in teaching clinical neurology as they are in other specialties and 88% of the students suggested that there is scope for improvisation of neurological skills of their teaching faculty. Schon et al. have raised this point of amount, type and quality of teaching that is given to a student is one of the reasons for neurophobia.[19] Thus, improved interaction between medical graduates and qualified neurologists needs to be bolstered.
Schwartz et al. observed that procedure related specialties were increasingly being chosen by students in United States in the previous two decades[11] and at present, Indian students are following the same track. In our study, lack of procedural skills was an important reason (57%) for not considering neurology as career. Hence, there is a need to give medical students some exposure of routine procedures done by Neurologists, i.e., electroencephalography and nerve conduction studies. While most of the postgraduates are very much aware of electrocardiography, echocardiography and endoscopy, but they hardly know or learn anything about neurophysiological procedures done in our labs. Hence, provision should be made in our teaching curriculum where students can be taught few basic concepts about these procedures at some point in their medical education. Subspecialties like interventional neurology, having procedures both diagnostic (digital subtraction angiography) and therapeutic (intra-arterial thrombolysis) for stroke and other vascular disorders, are evolving speedily and will attract students. The turf battle between Neurologists, Neuroradiologists and Cardiologists for these procedures needs to be sorted out, to give neurology candidates a fair chance to enhance their procedural skills. Other common procedures routinely done by Neurologist such as botulinum toxin injection for various movement disorders, nerve and muscle biopsy along with neuropathology exposure, lumbar puncture also need to be highlighted and demonstrated to students during their neurology rotations.
In our survey, self-assessment of neurological exposure and confidence in managing neurological cases was dismal. Up to one-third of the students (31%) thought that the level of neurological exposure given to them for managing common neurological cases and emergencies during their MBBS and MD curriculum was below average. Majority of the students (70-80%) felt they have not been taught enough about neurological drugs during MBBS pharmacology and they are not as confident in handling various neurological drugs as they are with drugs used in other specialties. Even in various conferences and CME's they attend, the level of neurological exposure was inadequate (67%). Consequently almost half of the students (47%) admitted that they are not confident in managing neurological cases. These findings match with other available studies[19,20] and have far reaching implications. In India, at present 90% of neurological cases are taken care by general physicians and it is very important to ensure good clinical neurology exposure to those who do not become Neurologists.
At present, there are only few institutes that provide structured neurology training, which is recognized by MCI with a limited intake capacity of approximately 100-150/year.[3,12] Therefore, already deficient neurology workforce in India is growing very slowly and there is a need for increasing interaction between Neurologists and general physicians and increasing the number of post-graduate registrations for neurology training. Organizing continuing medical education at regular interval and increasing the neurological exposure in various conferences students attend is one possible way of increasing their confidence in handling neurological disorders. 84% of students felt that starting a short-term (12 months) certification course in neurology will help them. Serious consideration should be given to these feasible options for looking after the neurological needs of our huge population and to further develop neurology work force in India.
Conclusions
Students should attend neurology out-patient clinics to get a positive perspective of treatable neurology
Procedures attract students. Hence, they should be told about available neurophysiological procedures and interventional neurology early in their careers
To attract more students toward neurology, students need to interact with “Role model” teachers in neurology
Neurologists should make active efforts to be perceived as therapeuticians and not only diagnosticians
Neurophobia may be countered by teaching only limited and relevant concepts basic neuroanatomy and neurophysiology as applicable to clinical neurology
Level of neurology exposure in our current MBBS and MD curricula and in various post-graduate conferences needs to be widened
Integrating practicing Neurologists in the teaching faculty in places where neurology departments do not exist
Serious consideration should be given to starting a short-term (12 months) certification course in neurology
Neurologist's interaction with practicing physicians needs to be enhanced.
Limitations of study
This study has enrolled students from a single state (Maharashtra). A larger series and similar type of studies from other states will be necessary for further exposition of this subject at the national level.
Acknowledgments
The authors wish to thank Dr. R. Bhagwat, Dr. Shrikant Deshmukh, Dr. Y. K. Amdekar and Dr. R. D. Khare for help in the collection of data.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Jagjit CS. History of Indian academy of neurology. In: Srinivas HV, editor. A Saga of Indian Neurology Reflections of Former Presidents. Bangalore: Aditi Enterprises; 2011. pp. xix–xx. [Google Scholar]
- 2.Wadia NH. Introduction to Indian neurology. In: Wadia NH, editor. Textbook – Neurological Practice: An Indian Perspective. 1st ed. New Delhi: Elsevier; 2005. p. 3. [Google Scholar]
- 3.Gourie-Devi M. Organization of neurology services in India: Unmet needs and the way forward. Neurol India. 2008;56:4–12. doi: 10.4103/0028-3886.39304. [DOI] [PubMed] [Google Scholar]
- 4.Khadilkar SV, Wagh S. Practice patterns of neurology in India: Fewer hands, more work. Neurol India. 2007;55:27–30. doi: 10.4103/0028-3886.30423. [DOI] [PubMed] [Google Scholar]
- 5.Lefevre JH, Roupret M, Kerneis S, Karila L. Career choices of medical students: A national survey of 1780 students. Med Educ. 2010;44:603–12. doi: 10.1111/j.1365-2923.2010.03707.x. [DOI] [PubMed] [Google Scholar]
- 6.van der Horst K, Siegrist M, Orlow P, Giger M. Residents’ reasons for specialty choice: Influence of gender, time, patient and career. Med Educ. 2010;44:595–602. doi: 10.1111/j.1365-2923.2010.03631.x. [DOI] [PubMed] [Google Scholar]
- 7.Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300:1154–64. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]
- 8.Jan MM, Fida NM. Attitudes of medical students toward pediatric neurology. Pediatr Neurol. 2002;27:106–10. doi: 10.1016/s0887-8994(02)00386-7. [DOI] [PubMed] [Google Scholar]
- 9.Gaucher S, Thabut D. Medical specialty choice: What impact of teaching? Results of a survey of two medical schools. Presse Med. 2013;42(4 Pt 1):e89–95. doi: 10.1016/j.lpm.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Johnson AL, Sharma J, Chinchilli VM, Emery SE, McCollister Evarts C, Floyd MW, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94:e78. doi: 10.2106/JBJS.K.00826. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz RW, Jarecky RK, Strodel WE, Haley JV, Young B, Griffen WO., Jr Controllable lifestyle: A new factor in career choice by medical students. Acad Med. 1989;64:606–9. [PubMed] [Google Scholar]
- 12.Khadilkar SV. Neurology: The scenario in India. J Assoc Physicians India. 2012;60:42–4. [PubMed] [Google Scholar]
- 13.Ridsdale L, Massey R, Clark L. Preventing neurophobia in medical students, and so future doctors. Pract Neurol. 2007;7:116–23. [PubMed] [Google Scholar]
- 14.Anonymous, Neurology for the masses. BMJ. 1999;319:A. [PMC free article] [PubMed] [Google Scholar]
- 15.Jozefowicz RF. Neurophobia: The fear of neurology among medical students. Arch Neurol. 1994;51:328–9. doi: 10.1001/archneur.1994.00540160018003. [DOI] [PubMed] [Google Scholar]
- 16.Lim EC, Seet RC. Demystifying neurology: Preventing ‘neurophobia’ among medical students. Nat Clin Pract Neurol. 2008;4:462–3. doi: 10.1038/ncpneuro0849. [DOI] [PubMed] [Google Scholar]
- 17.Haines DE, Hutchins JB, Lynch JC. Medical neurobiology: Do we teach neurobiology in a format that is relevant to the clinical setting? Anat Rec. 2002;269:99–106. doi: 10.1002/ar.10073. [DOI] [PubMed] [Google Scholar]
- 18.Menken M. Demystifying neurology. BMJ. 2002;324:1469–70. doi: 10.1136/bmj.324.7352.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schon F, Hart P, Fernandez C. Is clinical neurology really so difficult? J Neurol Neurosurg Psychiatry. 2002;72:557–9. doi: 10.1136/jnnp.72.5.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flanagan E, Walsh C, Tubridy N. ‘Neurophobia’ – Attitudes of medical students and doctors in Ireland to neurological teaching. Eur J Neurol. 2007;14:1109–12. doi: 10.1111/j.1468-1331.2007.01911.x. [DOI] [PubMed] [Google Scholar]


