Abstract
We discuss the clinical and imaging perspective in a case of a 78-year-old male who developed slurring of speech and ataxia acute in onset for the last 3 days. During his hospital stay, he developed multiple episodes of focal seizures without secondary generalization involving the angle of mouth on the right side. The patient had ataxia and positive cerebellar signs. In the past, the patient was treated for amoebic liver abscess and had undergone percutaneous aspiration of abscess. The patient was prescribed oral metronidazole and was discharged. This time, the patient underwent magnetic resonance imaging examination, which revealed lesion highly suggestive of metronidazole-induced encephalopathy. The offending drug was discontinued immediately after which the patient improved clinically. A follow-up scan was performed after 12 days and showed complete resolution of lesions.
Key Words: Diffusion-weighted imaging, fluid-attenuated inversion-recovery, metronidazole-induced encephalopathy, magnetic resonance imaging
Introduction
Metronidazole is a common antimicrobial agent used in the treatment of anaerobic and protozoal infections. The common adverse drug reactions to metronidazole include nausea, vomiting, epigastric pain, metallic taste, diarrhea and rash. In very rare instances, the drug is implicated in serious neurologic side-effects, including peripheral neuropathy, ataxia, dysarthria, seizures and encephalopathy.[1] Brain lesions of patients clinically diagnosed to have metronidazole-induced encephalopathy (MIE) were typically located at the cerebellar dentate nucleus, midbrain, dorsal pons, medulla and splenium of the corpus callosum.[2] We present a case of a 78-year-old male who was prescribed metronidazole at a dose of 800 mg three times daily for 6 weeks. The patient eventually developed neurologic manifestations compatible with encephalopathy. The magnetic resonance imaging (MRI) findings were highly suggestive of MIE. Upon discontinuation of metronidazole, the patient showed clinical improvement. A follow-up MRI as early as 12 days showed resolution of the lesions.
Case Report
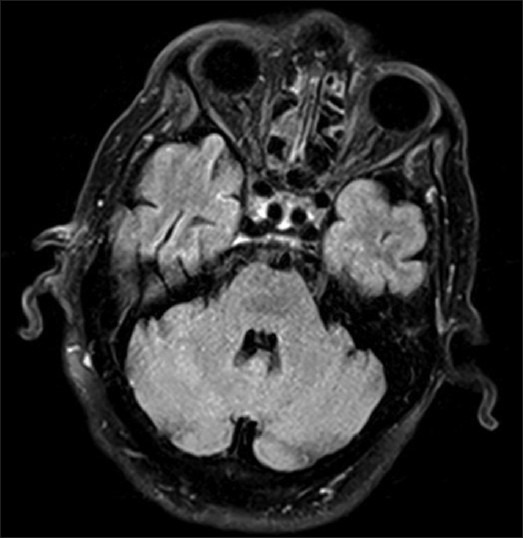
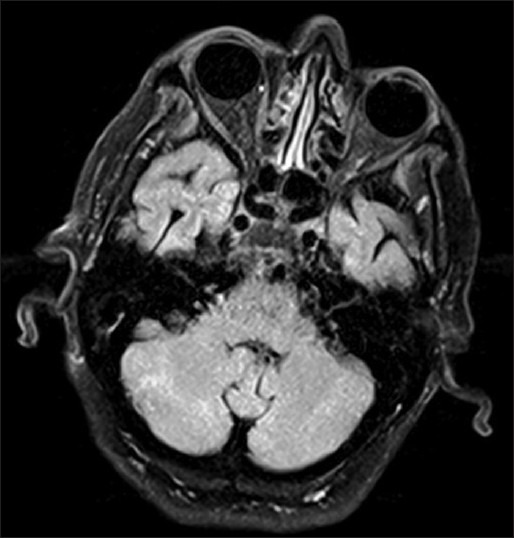
We discuss the case of a 78-year-old male who developed slurring of speech and ataxia acute in onset for the last 3 days. During the hospital stay, he developed multiple episodes of focal seizures without secondary generalization involving the angle of mouth on the right side. The patient complained of headache not associated with vertigo, tinnitus or visual complaints. There was no recent history of toxin exposure or trauma. Five weeks prior to admission, the patient was admitted for amoebic liver abscess. He underwent percutaneous aspiration of abscess. The patient was prescribed oral metronidazole 800 mg thrice daily for 6 weeks and was discharged. At the time of admission, he had taken the drug for 5 weeks (35 days). On examination, the patient was well oriented. Sensory motor and cranial nerve examination were unremarkable. The patient had cerebellar signs in the form of ataxia dysdiadochokinesia and impaired co-ordination in both the upper and the lower limbs. Reflexes were within normal limits. The patient underwent MRI examination, which revealed symmetrical areas of altered signal intensity, appearing hyperintense on T2-weighted and fluid-attenuated inversion-recovery (FLAIR) images involving the dentate nuclei, dorsal pons and midbrain [Figures 1 and 2]. Diffusion-weighted/apparent diffusion coefficient (ADC) mapping was suggestive of T2 shine through due to cytotoxic edema rather than restricted diffusion [Figures 3 and 4]. Given the history of metronidazole and characteristic distribution of lesions on MRI, the patient was diagnosed as a case of MIE. The offending drug was discontinued immediately, after which the patient improved clinically. A follow-up scan was performed after 12 days, which showed complete resolution of the lesions [Figures 5 and 6].
Figure 1.
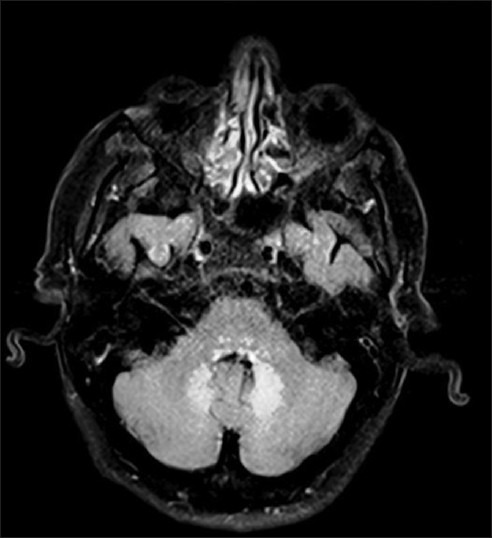
Axial fluid-attenuated inversion-recovery image shows hyperintense signal in characteristic bilateral dentate nuclei
Figure 2.
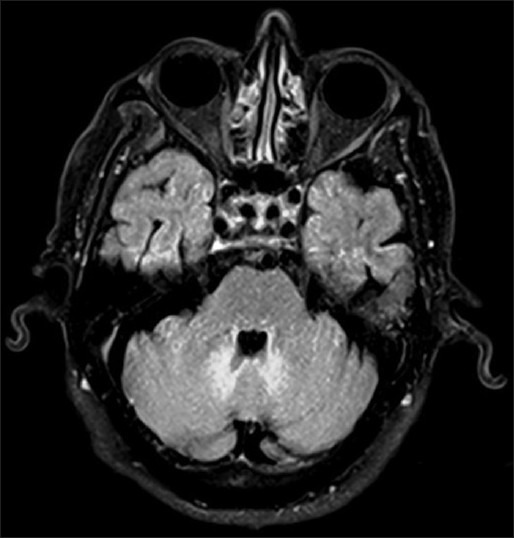
Axial fluid-attenuated inversion-recovery image shows hyperintense signal in bilateral vermis and tonsillar region
Figure 3.
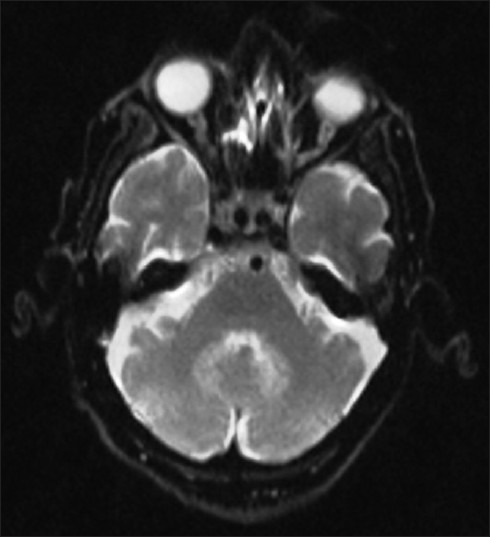
Corresponding diffusion weighted imaging shows hyperintense signal in dentate nuclei
Figure 4.
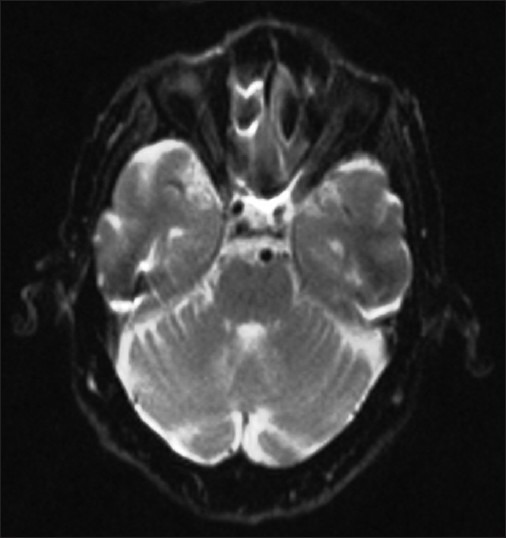
Diffusion weighted imaging showing hyperintense signal in vemis and tonsillar region
Figure 5.
Follow-up scanning after 12 days at same level shows complete resolution of lesions
Figure 6.
Follow-up scanning after 12 days at level of tonsils shows complete resolution of lesions
Discussion
The mechanism of metronidazole toxicity has not been elucidated. The signal intensity changes observed on the diffusion-weighted images most likely represent interstitial edema. Ahmed et al.[3] speculated that, because of the reversibility of the MRI changes, the cause of the changes associated with acute toxic insult were most likely due to “axonal swelling with increased water content” And not demyelination. Proposed mechanisms include binding of metronidazole to RNA, DNA and inhibitory neurotransmitters, as well as inducing both vasogenic and cytotoxic edema.[4] The typical locations of lesions by MRI in patients with MIE are the cerebellar dentate nuclei, midbrain (tectum, red nucleus, tegmentum around periaqueductal gray matter), dorsal pons, dorsal medulla and corpus callosum (splenium). These were always bilateral and symmetric. FLAIR and diffusion weighted imaging (DWI) was performed in our patient, and demonstrated increased signal intensity on T2 and FLAIR sequences and isotropic DW images. ADC maps demonstrated an increase in the ADCs corresponding to the areas of abnormal DW image signal intensity, suggestive of T2 shine through. Follow-up MRI performed after 12 days showed absence of identifiable signal intensity abnormality on the DW images and normalization of the ADC values. The quantitative ADC maps confirm that the observed high DWI signal intensity is due to vasogenic edema with associated increased ADC values, not restricted diffusion, which would suggest an ischemic process.[5] Ahmed et al.[3] first described the imaging findings of metronidazole toxicity in a 45-year-old woman who developed nausea, vomiting, vertigo, dysarthria and confusion after consuming 35 g metronidazole over a 30-day course of therapy. Horlen et al.[6] reported imaging findings of presumed metronidazole toxicity in a 35-year-old male patient with liver cirrhosis who had consumed greater than 60 g metronidazole over a 55-day period and developed clinical symptoms consistent with metronidazole toxicity. Our patient consumed 84 g metronidazole over a period of 35 days. In each of the cases, including ours, the symptoms rapidly normalized following cessation of metronidazole therapy. The rapidity with which the signal intensity abnormality resolves remains to be elucidated. To the best of our knowledge, earliest follow-up MRI was obtained after 12 days in our case. The duration of treatment with metronidazole before cerebellar symptoms manifest is variable, ranging from 28 days to 3 months,[1,2] and cumulative doses range from 25 g to 90 g.[1,2] In our patient, the symptoms developed at a dose of 84 g. Patients usually experience complete resolution of the symptoms after discontinuation of metronidazole, sometimes within a few days. Our patient's symptoms and signs resolved within days of stopping metronidazole. The MRI changes also resolved, thereby implicating the drug as the causative agent. The differential diagnosis of T2 hyperintense, bilaterally symmetrical dentate nuclei includes methyl bromide intoxication, maple syrup urine disease and enteroviral encephalomyelitis.[7,8,9]
Conclusions
MIE is a rare subacute cerebellar syndrome. Its diagnosis requires a high index of suspicion. Withdrawal of the offending metronidazole drug is the only definitive treatment for MIE as the condition is a form of drug intoxication. MRI is complementary in this entirely clinical diagnosis. How early the lesions resolve on follow-up imaging is uncertain. No definitive dosage of drug can be estimated as toxicity has been reported at low as well as at high doses.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Kim KH, Choi JW, Lee JY, Kim TD, Paek JH, Lee EJ, et al. Two cases of metronidazole-induced encephalopathy. Korean J Gastroenterol. 2005;45:195–200. [PubMed] [Google Scholar]
- 2.Kim E, Na DG, Kim EY, Kim JH, Son KR, Chang KH. MR imaging of metronidazole-induced encephalopathy: Lesion distribution and diffusion-weighted imaging findings. AJNR Am J Neuroradiol. 2007;28:1652–8. doi: 10.3174/ajnr.A0655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed A, Loes DJ, Bressler EL. Reversible magnetic resonance imaging findings in metronidazole-induced encephalopathy. Neurology. 1995;45:588–9. doi: 10.1212/wnl.45.3.588. [DOI] [PubMed] [Google Scholar]
- 4.Kusumi RK, Plouffe JF, Wyatt RH, Fass RJ. Central nervous system toxicity associated with metronidazole therapy. Ann Intern Med. 1980;93:59–60. doi: 10.7326/0003-4819-93-1-59. [DOI] [PubMed] [Google Scholar]
- 5.Lee SS, Cha SH, Lee SY, Song CJ. Reversible inferior colliculus lesion in metronidazole-induced encephalopathy: Magnetic resonance findings on diffusion-weighted and fluid attenuated inversion recovery imaging. J Comput Assist Tomogr. 2009;33:305–8. doi: 10.1097/RCT.0b013e31817e6f58. [DOI] [PubMed] [Google Scholar]
- 6.Horlen CK, Seifert CF, Malouf CS. Toxic metronidazole-induced MRI changes. Ann Pharmacother. 2000;34:1273–5. doi: 10.1345/aph.10028. [DOI] [PubMed] [Google Scholar]
- 7.Geyer HL, Schaumburg HH, Herskovitz S. Methyl bromide intoxication causes reversible symmetric brainstem and cerebellar MRI lesions. Neurology. 2005;64:1279–81. doi: 10.1212/01.WNL.0000156835.12492.30. [DOI] [PubMed] [Google Scholar]
- 8.Jan W, Zimmerman RA, Wang ZJ, Berry GT, Kaplan PB, Kaye EM. MR diffusion imaging and MR spectroscopy of maple syrup urine disease during acute metabolic decompensation. Neuroradiology. 2003;45:393–9. doi: 10.1007/s00234-003-0955-7. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman RD. MR imaging findings of enteroviral encephalomyelitis: An outbreak in Taiwan. AJNR Am J Neuroradiol. 1999;20:1775–6. [PMC free article] [PubMed] [Google Scholar]


