Abstract
Objective:
The objective of this study was to compare the occurrence and severity of behavioral and psychological symptoms of dementia (BPSD) between vascular dementia (VaD) and vascular cognitive impairment-no dementia (VCI-ND).
Materials and Methods:
Consecutive patients presenting with cognitive impairment at least 3 months after an ischemic stroke and with a Hachinski Ischemic Score ≥4 were included. VaD was diagnosed as per National Institute of Neurological Disorders and Stroke – Association Internationale pour la Recherche et l’Enseignement en Neurosciences criteria for probable VaD and VCI-ND on the lines of the Canadian study of health and aging. The severity of cognitive impairment and the behavioral/psychological symptoms were studied by means of the clinical dementia rating scale and the neuropsychiatric inventory (NPI) respectively.
Results:
All patients with VaD and 89% of those with VCI-ND had at least one BPSD. The mean no. of symptoms per patient and the total NPI scores were higher in VaD than in VCI-ND. Apathy and night-time behavior disturbances were significantly more common and severe in VaD.
Conclusions:
BPSD are very common both in VCI-ND and in VaD. The profile of BPSD is similar in both groups, albeit more severe in VaD. The net burden of BPSD is higher in VaD as compared to VCI-ND.
Key Words: Behavioral and psychological symptoms, neuropsychiatric inventory, vascular cognitive impairment, vascular cognitive impairment-no dementia, vascular dementia
Introduction
As part of the natural history of dementia, most patients experience changes in mood, perception, thought and personality. These phenomena are common and are a source of both patient distress and caregiver burden. These neuropsychiatric symptoms have been designated “behavioral and psychological symptoms of dementia” (BPSD) by the International Psychogeriatric Association.[1] Alleviation of most of these behavioral and psychological symptoms is feasible, especially if diagnosed early. BPSD lead to lower levels of cognitive functioning and their treatment may improve the functional status and quality-of-life of patients with dementia.[2]
Vascular cognitive impairment (VCI) is a concept encompassing the entire spectrum of cognitive impairment arising due to vascular brain insults. Apart from frank cases of vascular dementia (VaD), there exists a subgroup of patients with cerebrovascular disease who demonstrate cognitive deficits not fulfilling the traditional definitions of dementia. This subgroup has been designated “Vascular cognitive impairment-no dementia (VCI-ND).”
VCI includes VaD, VCI-ND and cases of mixed dementia (VaD + features of Alzheimer disease [AD]). VCI-ND may be considered to be the prodromal stage of VaD, with nearly 50% cases of VCI-ND observed to progress to dementia over 5 years.[3] The literature dealing with BPSD in VCI is scant as compared to AD. Most of the existing work deals only with VaD. In the light of the concept of the continuum of VCI, it is imperative to study the profile of BPSD in VCI-ND. With this end in view, this study was conceptualised.
Aim
The purpose of this study was to compare the occurrence and severity of behavioral and psychological symptoms between VaD and VCI-ND.
Materials and Methods
This was a prospective, observational study approved by the Institutional Ethics Committee. Patients presenting to the inpatient or outpatient clinics of the Department of Neurology in a Tertiary Care Teaching Hospital in New Delhi between March 2011 and August 2012, at least 3 months after a stroke were interrogated regarding the occurrence of any cognitive problems in the presence of a reliable caregiver. Patients with aphasia severe enough to preclude further cognitive evaluation, those with hepatic, renal or thyroid disease and those already on antidepressants, anxiolytics, antipsychotics, anti-dementia drugs or cognition enhancers, were excluded. Patients with cognitive complaints after stroke and scoring ≥4 on the Hachinski ischaemic score[4] were included after taking written and informed consent.
A detailed neurological examination including higher mental function assessment was done. Cognitive domains such as attention, language, memory, executive function, visuospatial function, praxis and calculation were evaluated using appropriate clinical methods. Magnetic resonance imaging of the brain, incorporating T1, T2, fluid attenuated inversion recovery, diffusion weighted images, apparent diffusion coefficient maps and gradient-echo sequences was carried out for each patient. Cases with intracerebral hemorrhage were excluded. Patients who fulfilled the National Institute of Neurological Disorders and Stroke — Association Internationale pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN) “probable VaD” criteria were diagnosed as having VaD.[5] Patients with cognitive deficits of vascular etiology, but not fulfilling the NINDS-AIREN or the Diagnostic and Statistical Manual of Mental Disorders-Fourth edition (DSM-IV) criteria, but demonstrating difficulties in any two of: Doing household chores, managing money, feeding self, dressing and incontinence, were diagnosed as VCI-ND, on the lines of the Canadian study of health and aging.[6] The clinical dementia rating scale (CDR) score[7] was calculated for each patient. Behavioral and psychological symptoms were evaluated on the basis of the neuropsychiatric inventory (NPI)[8] in the presence of a reliable caregiver. The individual domain scores for each of the 12 neuropsychiatric symptoms were obtained by calculating the product of the frequency and severity scores of each symptom. The sum of these domain scores yielded the total NPI score for each patient.
Statistical analysis
The mean age and educational status and the mean no. of neuropsychiatric symptoms per patient, between the VaD and VCI-ND groups were compared using the unpaired t-test while the gender distribution and frequency of occurrence of individual neuropsychiatric symptoms were compared by the Chi-square test. The domain scores of individual symptoms and the total NPI scores were compared between these groups by means of the Mann-Whitney U test. Correlations between the CDR score and the number of neuropsychiatric symptoms or the NPI score (individual domain scores and total NPI scores) were obtained by calculating Spearman correlation coefficients. A P ≤ 0.05 was considered to be statistically significant.
Results
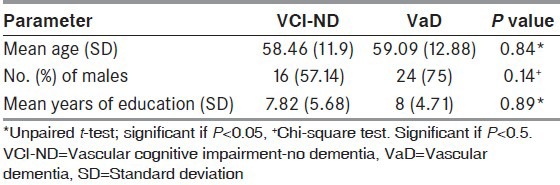
A total of 60 patients with VCI were studied. The mean age and years of education for the entire group were 58.8 (±12.03) and 8 (±5.14) years respectively while the male:female ratio was 2:1.32 (53.3%) patients were diagnosed as having VaD, whereas 28 (46.6%) patients were classified as VCI-ND. No case of mixed dementia was found. The age, gender distribution and educational status of both VaD and VCI-ND groups were comparable [Table 1]. The median CDR score of the VCI-ND group was 0.5 and that of the VaD group was 2.
Table 1.
Demographic parameters of the VCI-ND and VaD groups
Frequency of BPSD in the two groups
Overall, 57 (95%) patients had at least one neuropsychiatric symptom on the NPI. At least one behavioral/psychological symptom on the NPI was found in all patients with VaD and in 89% of those with VCI-ND. The mean number of symptoms per patient on the NPI in the VaD group was 4.87 (standard deviation [SD]: 1.64; range: 2-8), which was significantly higher than that in the VCI-ND group (Mean: 3; SD: 2.15; range: 0-8); (P = 0.0003). There was a significant positive correlation between the CDR score and the number of symptoms per patient (r = 0.58, P = 0.001).
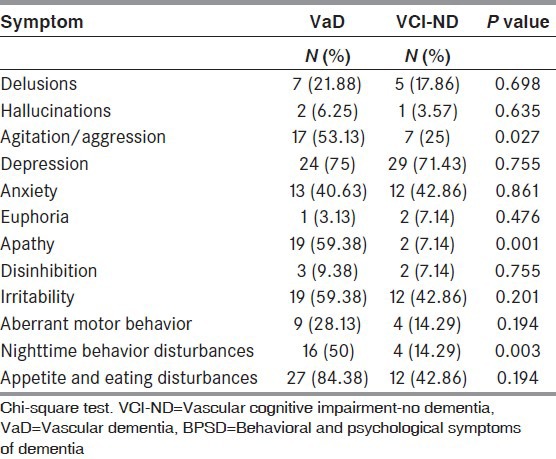
In the VaD group, appetite and eating disorders constituted the commonest symptom (84.38%), followed by depression (75%), irritability and apathy (59.38% each), agitation/aggression (53.15%), night-time behavior disturbances (50%), anxiety (40.63%), aberrant motor behavior (28.13%) and delusions (21.88%). Hallucinations, disinhibition and euphoria were the least common symptoms, being encountered in less than 10% cases each. On the other hand, in VCI-ND, depression was the predominant symptom (71.43%), followed by irritability, appetite disturbances and anxiety (42.86% each). These were followed by agitation/aggression (25%), delusions (17.86%), aberrant motor behavior and night-time behavior disturbances (14.29% each). Apathy, euphoria, disinhibition and hallucinations were infrequently encountered.
Between the two groups, most symptoms were commoner in VaD, the differences being significant only in the domains of apathy, night-time behavior disturbances and agitation/aggression. (P = 0.001, 0.003 and 0.027 respectively) [Table 2]. Only anxiety and euphoria were commoner in VCI-ND, but the differences were insignificant.
Table 2.
Comparison of the frequency of various BPSD between VaD and VCI-ND groups
Comparison of severity of BPSD between the two groups
Between the VaD and VCI-ND groups, the domain scores for each symptom except euphoria were found to be higher in the VaD group [Figure 1]. The difference was statistically significant in the domains of apathy, night-time behavior and appetite. (P = 0.0002, 0.01, 0.003 respectively). The median total NPI score was found to be significantly higher in the VaD group than in VCI-ND (32.5 vs. 13; P = 0.00013).
Figure 1.
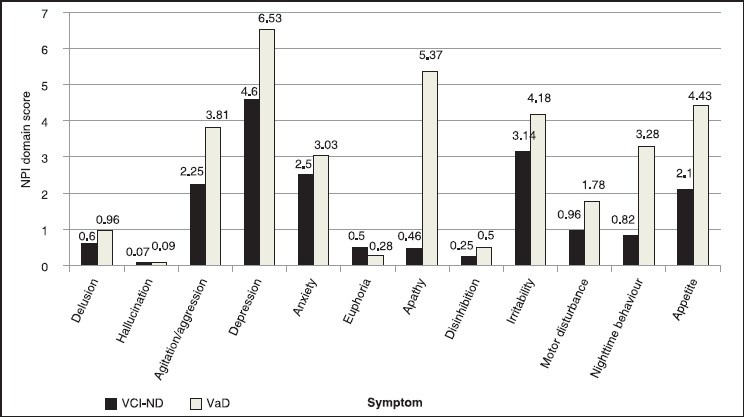
Comparison of the mean neuropsychiatric inventory domain scores of each symptom between vascular dementia and vascular cognitive impairment-no dementia groups: Note: Although the mean scores have been depicted in this graph, the Mann-Whitney U test for non-parametric data has been used to determine statistical significance
The total NPI score correlated positively and significantly with the CDR score. (r = 0.598; P = 0.001).
Discussion
A diagnosis of VaD by most accepted criteria mandates the documentation of memory impairment. However, several patients have cognitive dysfunction attributable to vascular brain insults where memory may not be impaired as commonly as other domains like executive function. VaD; therefore, is only the tip of the iceberg of the broader concept of VCI. Diagnosis of VCI in earlier stages is crucial as appropriate therapeutic measures if instituted early, have been found to thwart the progression to dementia.[9] The concept of VCI-ND becomes important in this scenario and may be considered analogous to the construct of “mild cognitive impairment” in the setting of AD.
VCI-ND has been found to be very common, especially in the elderly. VCI-ND was observed to be the commonest subtype of VCI in a Canadian population aged 65-84 years.[10] A study from Japan found the prevalence of VCI-ND to be as high as 8.5% in the total population.[11] Wentzel et al., reported that half the individuals in their study who met criteria for VCI-ND developed dementia over a 5 year follow-up.[3] However, in a given cohort of individuals with VCI, the proportion of cases being diagnosed as VCI-ND depends on the criteria employed to diagnose dementia. More stringent criteria like the NINDS-AIREN criteria for VaD lead to more patients being diagnosed as VCI-ND as compared to the situation where more liberal criteria are used. In the present study, VaD was diagnosed on the basis of the NINDS-AIREN criteria.
There is a dearth of studies contrasting the neuropsychological and neuropsychiatric profiles of VCI-ND and VaD. Nyenhuis et al., reported that deficits in immediate memory, psychomotor speed and depression, which had previously been described in VaD also occurred in VCI-ND. On the basis of this similarity of cognitive and behavioral deficits, they further supported the hypothesis that VCI-ND and VaD were points on a continuum.[12] Based on the above hypothesis, it would not be wrong to hypothesise that the pattern of neuropsychiatric symptoms in these two groups too would be similar.
In the present study, a significantly higher number of neuropsychiatric symptoms occurred per patient in VaD, though the frequency of occurrence of most symptoms between these groups was similar. Apathy, agitation and night-time behavioral disturbances were significantly less common in VCI-ND. In a previous study by Chiu et al., at least one neuropsychiatric symptom was reported by 85% and 92% of their VCI-ND and VaD patients respectively. The frequency of apathy, agitation, aberrant motor behavior and hallucinations was found to be significantly lower in their VCI-ND group.[13] These findings are in good agreement with those of the present study.
Apathy, appetite and nighttime behavior disturbances were found to be significantly more severe in the VaD group. The total NPI score was also significantly higher in this group. Chiu et al., also found similar results with respect to apathy and total NPI scores in VaD as compared to VCI-ND. In addition, hallucinations, agitation and aberrant motor behavior were found to be more severe in their VaD group.[13]
In a similar study, comparing the prevalence of neuropsychiatric symptoms across the declining memory continuum in AD (i.e., normal controls, subjective cognitive impairment, mild cognitive impairment and mild AD), the prevalence of BPSD was found to be higher at the higher end of the spectrum, i.e., mild AD. The total NPI scores also were found to increase along the continuum. Agitation, apathy and aberrant motor behavior were significantly commoner in AD than in the other groups.[14]
Various previous studies have demonstrated a good correlation between the severity of BPSD and the degree of cognitive impairment in VaD.[15,16] The present finding of a greater burden of BPSD in VaD than in VCI-ND is in agreement with these observations.
Judging by the above findings, it seems that both the number of symptoms per patient and the net burden of BPSD as reflected by the total NPI scores may increase with increasing degrees of cognitive impairment in VCI, though, head to head, the frequency of individual symptoms is nearly identical in VaD and VCI-ND. Apathy and night-time behavior disturbances as neuropsychiatric symptoms in VCI deserve attention as they may significantly increase both in frequency and severity with an increase in degrees of cognitive impairment.
Limitations of the study
This study has certain limitations, the chief one being a relatively small sample size. Secondly, the question arises as to which instruments are the most ideal to study the cognitive and behavioral profile of patients with VCI. There is no straightforward answer to this. Most instruments have been designed with a focus on AD and each one has its own limitations. For example, the CDR scale has a disproportionate emphasis on memory impairment. Comparison between studies on VCI is made difficult owing to the variety of instruments used to study cognition and behavior. In the present study, the CDR and NPI were chosen on the lines of previous similar studies on the subject.[13,17,18] Thirdly, in the light of the paucity of data regarding the applicability of the NPI in the Indian population, it would have been worthwhile to compare the NPI scores of a cohort of normal individuals with those of the study group, especially with those of patients with VCI-ND. This was not done.
In spite of these limitations, our findings have clinical relevance. That the pattern of BPSD in VCI-ND is similar, albeit milder, is well in accordance with the present concept of VCI-ND being an earlier point than VAD on the continuum of VCI. In the earlier stages of VCI, the cognitive deficits may be so mild as to be overlooked by both the patient and the family. Behavioral symptoms like depression; however, may be present even in these stages. Late-life depression must be investigated thoroughly for sinister etiologies like incipient dementia. At present, the therapeutic armamentarium against dementia is limited. Early diagnosis and management of BPSD in patients with dementia has the potential to improve the quality-of-life of both patients and caregivers. Further, in the later stages of dementia, when the burden of BPSD is expected to be higher, patient and the caregivers may require more professional assistance.
To conclude, the profile of BPSD in VCI-ND and VaD is similar. Depression is common irrespective of the severity of cognitive impairment. The frequency and severity of apathy and night-time behavior disturbances and the net burden of BPSD are higher in the later stages of VCI. Diagnosis and management of BPSD in the early stages of VCI is crucial.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Finkel SI, Costa e Silva J, Cohen G, Miller S, Sartorius N. Behavioral and psychological signs and symptoms of dementia: A consensus statement on current knowledge and implications for research and treatment. Int Psychogeriatr. 1996;8(Suppl 3):497–500. doi: 10.1017/s1041610297003943. [DOI] [PubMed] [Google Scholar]
- 2.Brody JA. An epidemiologist views senile dementia — Facts and fragments. Am J Epidemiol. 1982;115:155–62. doi: 10.1093/oxfordjournals.aje.a113286. [DOI] [PubMed] [Google Scholar]
- 3.Wentzel C, Rockwood K, MacKnight C, Hachinski V, Hogan DB, Feldman H, et al. Progression of impairment in patients with vascular cognitive impairment without dementia. Neurology. 2001;57:714–6. doi: 10.1212/wnl.57.4.714. [DOI] [PubMed] [Google Scholar]
- 4.Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32:632–7. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- 5.Román GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, et al. Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250–60. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 6.Ingles JL, Wentzel C, Fisk JD, Rockwood K. Neuropsychological predictors of incident dementia in patients with vascular cognitive impairment, without dementia. Stroke. 2002;33:1999–2002. doi: 10.1161/01.str.0000024433.36590.1b. [DOI] [PubMed] [Google Scholar]
- 7.Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 8.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–14. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 9.Devasenapathy A, Hachinski VC. Vascular Cognitive Impairment. Curr Treat Options Neurol. 2000;2:61–72. doi: 10.1007/s11940-000-0024-z. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K, Wentzel C, Hachinski V, Hogan DB, MacKnight C, McDowell I. Prevalence and outcomes of vascular cognitive impairment. Vascular Cognitive Impairment Investigators of the Canadian Study of Health and Aging. Neurology. 2000;54:447–51. doi: 10.1212/wnl.54.2.447. [DOI] [PubMed] [Google Scholar]
- 11.Ishii H, Meguro K, Yamaguchi S, Ishikawa H, Yamadori A. Prevalence and cognitive performances of vascular cognitive impairment no dementia in Japan: The Osaki-Tajiri Project. Eur J Neurol. 2007;14:609–16. doi: 10.1111/j.1468-1331.2007.01781.x. [DOI] [PubMed] [Google Scholar]
- 12.Nyenhuis DL, Gorelick PB, Geenen EJ, Smith CA, Gencheva E, Freels S, et al. The pattern of neuropsychological deficits in Vascular Cognitive Impairment-No Dementia (Vascular CIND) Clin Neuropsychol. 2004;18:41–9. doi: 10.1080/13854040490507145. [DOI] [PubMed] [Google Scholar]
- 13.Chiu PY, Liu CH, Tsai CH. Neuropsychiatric manifestations in vascular cognitive impairment patients with and without dementia. Acta Neurol Taiwan. 2007;16:86–91. [PubMed] [Google Scholar]
- 14.Zhang M, Wang H, Li T, Yu X. Prevalence of Neuropsychiatric Symptoms across the Declining Memory Continuum: An Observational Study in a Memory Clinic Setting. Dement Geriatr Cogn Dis Extra. 2012;2:200–8. doi: 10.1159/000338410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson C, Brodaty H, Trollor J, Sachdev P. Behavioral and psychological symptoms associated with dementia subtype and severity. Int Psychogeriatr. 2010;22:300–5. doi: 10.1017/S1041610209991220. [DOI] [PubMed] [Google Scholar]
- 16.Kim JM, Lyons D, Shin IS, Yoon JS. Differences in the behavioral and psychological symptoms between Alzheimer's disease and vascular dementia: Are the different pharmacologic treatment strategies justifiable? Hum Psychopharmacol. 2003;18:215–20. doi: 10.1002/hup.466. [DOI] [PubMed] [Google Scholar]
- 17.Fuh JL, Wang SJ, Cummings JL. Neuropsychiatric profiles in patients with Alzheimer's disease and vascular dementia. J Neurol Neurosurg Psychiatry. 2005;76:1337–41. doi: 10.1136/jnnp.2004.056408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Staekenborg SS, Su T, van Straaten EC, Lane R, Scheltens P, Barkhof F, et al. Behavioural and psychological symptoms in vascular dementia; differences between small- and large-vessel disease. J Neurol Neurosurg Psychiatry. 2010;81:547–51. doi: 10.1136/jnnp.2009.187500. [DOI] [PubMed] [Google Scholar]


