Abstract
Subdural empyema is an uncommon clinical entity. The first case of Porphyromonas gingivalis subdural empyema is reported. We report a case of 34-year-old male who presented with subdural empyema and sinusitis. Through the utilization of polymerase chain reaction (PCR) tests on subdural pus, we were able to confirm the diagnosis and institute appropriate treatment. Early surgical intervention and intravenous antibiotics meant that the patient recovered fully. Infections caused by P. gingivalis should be considered in differential diagnoses of central nervous system (CNS) abscesses or subdural empyema especially in patients with precedent periodontal diseases and sinusitis.
Key Words: Porphyromonas gingivalis, subdural empyema, periodontal disease
Introduction
Subdural empyema is an uncommon clinical entity and accounts for approximately 13-23% of all intracranial infections.[1] Young male patients in the second or third decade are most commonly affected.[2] Subdural empyema is a collection of pus between dura mater and arachnoid mater.[1] It develops most commonly as a consequence of ear or sinus infection. Other causes include cranial osteomyelitis, penetrating head trauma or neurosurgery and hematogenous spread from a remote source.[3] Aerobic and anaerobic streptococci, Haemophilus influenzae, Staphylococcus aureus, and S. epidermidis are the most commonly identified organisms.[4,5] In this report, we present an adult patient who developed subdural empyema due to Porphyromonas gingivalis.
Case Report
A 34-year-old male was admitted to Thammasat University Hospital, Thailand with 1 day of high fever, severe headache, photophobia, left hemiparesis, and repeated vomiting. He had had rhinorrhea, sore throat, facial pain, and low grade fever 2 weeks earlier and was treated with a short course of oral antibiotics.
On admission, he was alert and oriented. The patient had a temperature of 39°C, heart rate of 120 beats/min, and blood pressure of 130/90 mmHg. Neurological examination revealed nuchal rigidity and left hemiparesis grade 3 (medical research council scale). He had left facial weakness, upper motor neuron type with purulent nasal discharge, nasal turbinate swelling, and frontal sinus tenderness. His blood profile showed leukocytosis of 23,700 cells/mm3 with 95% neutrophils. His basic metabolic panel showed normal electrolytes, glucose, liver, and renal function. Computed tomography (CT) of the brain revealed crescent-shaped hypodense to isodense lesion at right frontal convexity and along right falx cerebri with 0.6 cm in maximal thickness at right frontal lobe suggestive of subdural effusion. The CT additionally revealed opacification at both frontal sinuses, both ethmoid sinuses and left maxillary sinus suggestive of sinusitis. A magnetic resonance imaging (MRI) was obtained and showed thin subdural collection over right hemispheric convexity and right interhemispheric fissure causing subfalcian brain herniation to the left for about 8 mm with bilateral frontal, ethmoid, and left maxillary sinusitis [Figure 1].
Figure 1.
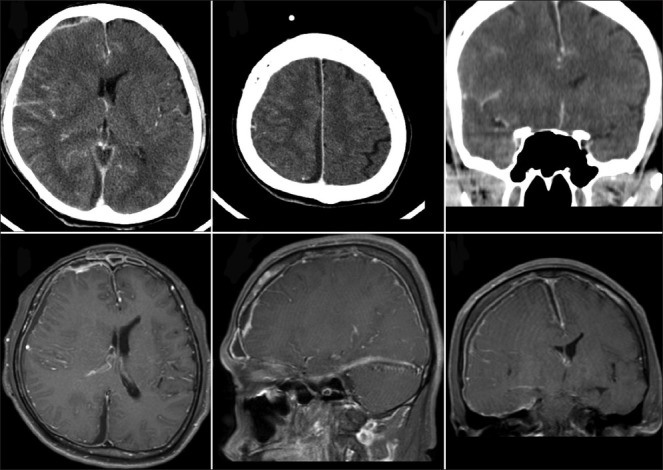
Subdural empyema at right frontal convexity and along right side falx cerebri, about 0.6 cm in maximal thickness at right frontal lobe. Minimal brain swelling and effacement of adjacent cortical sulci and right lateral ventricle with shifting of midline structures to the left about 0.2 cm. Opacification at both frontal sinuses, ethmoid, and left maxillary sinuses
He was diagnosed with subdural empyema and started on intravenous ceftriaxone 4 g daily divided every 12 h and metronidazole 1.5 g daily divided every 8 h and were continued for 6 weeks without dose adjustment. He received supportive care with neurosurgical consultation. On the 2nd day of admission he developed increased left hemiparesis (from grade 3 to grade 0) and his consciousness level deteriorated. Right frontoparietal craniectomy was performed. Antiepileptic drugs were started. Seizure prophylaxis was started as intravenous dilantin 300 mg daily divided every 8 h. Yellowish purulent material with a total volume of 100 ml was drained and sent for microbiological examination. No organisms were isolated in aerobic pus culture. Polymerase chain reaction (PCR) molecular identification for bacteria isolated Porphyromonas gingivalis. The 16S rRNA sequences of the genus Porphyromonas were selected from the taxonomy database of the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/Taxonomy/taxonomyhome.html/). The sequence of the forward primer, was 5’-GCGCTCAACGTTCAGCC-3’ (base pairs 612-628); the sequence of the reverse primer was 5’-CACGAATTCCGCCTGC-3’ (base pairs 664-679); and the sequence of the Taqman probe, was 5’-CACTGAACTCAAGCCCGGCAGTTTCAA-3’ (base pairs 634-660).[6] Patient regained full consciousness 2 days after the surgery. Bilateral anterior ethmoidectomy and bilateral frontal sinectomy were also performed. On 15th day of admission, his consciousness deteriorated. MRI showed subdural empyema along bilateral falx cerebri and right parieto-temporo-occipital region. A second craniotomy was done and drainage tubes were placed at posterior midline parietal and occipital area, a total of 100 ml of yellow purulent material was drained. Patient gradually improved and was discharged after 6 weeks of the intravenous antibiotics. Dental consultations revealed no dental or root canal abscesses, no further work up for periodontal disease were carried out. At the time of discharge, his motor power was 5/5 with normal mental status. No signs of recurrent infection were detected on the follow-up 1 month after discharge [Figure 2].
Figure 2.
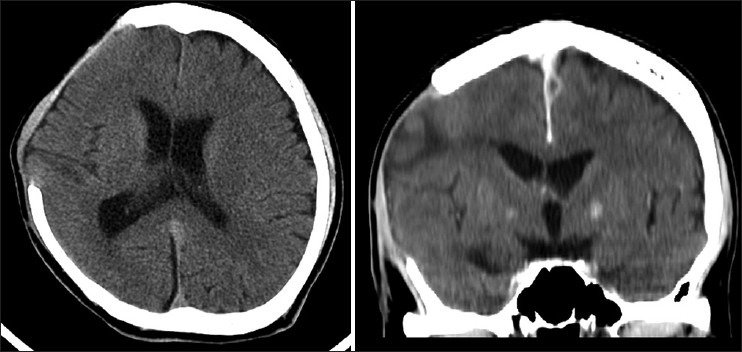
Subdural collection over right hemispheric convexity and right interhemispheric fissure, most pronounced collection of 0.7 cm thickness at right frontal convexity near right frontal sinus. Mass effect of right subdural collection causing subfalcial brain herniation to the left side about 0.8 cm
Discussion
P. gingivalis is black-pigmented non-motile gram-negative bacteria and requires anaerobic conditions for growth.[7] This organism works with other microbes to generate a biofilm in the subgingival layer.[8] P. gingivalis is the species highly associated with chronic periodontitis and can be detected in up to 85% of the disease sites.[9] P. gingivalis is native only to the oral cavity and has not yet been identified from extra-oral sources in patients with P. gingivalis periodontitis.[10,11] The reported extra-oral infections are rare and include chronic sinusitis, paranasal infected mucocele, tonsillitis, peritonsillar abscesses, pleuropulmonary infection, thoracic empyema, lung abscess, chronic suppurative otitis media, gas gangrene, perforated appendix and appendicitis.[8]
Subdural empyema occurs commonly in children and young adults.[2,12] It is often associated with sinusitis and otitis media.[2,12] The most common organism associated with subdural empyema is Streptococcus pneumoniae.[12,13] To our knowledge, this reported case is the first case caused by P. gingivalis in the literature. Generally, central nervous system (CNS) infections caused by P. gingivalis are extremely rare. There have been two previously reported cases of P gingivalis associated CNS infection in the literature. The first case was a patient with brain abscess developed after dental infection caused by P. gingivalis.[14] The organism was identified in the cerebrospinal fluid (CSF). Treatment required intravenous, intrathecal and intraventricular antibiotics, ventricular drainage and tooth extraction. The second patient had cavernous sinus thrombophlebitis caused by P. gingivalis with abscess formation extending to the orbital cavity.[15] There was no prior trauma or obvious oral or pharyngeal infections in this case. The patient was successfully treated with surgical drainage and intravenous antibiotics.
According to the two reported cases and our case, risk factors associated with CNS infections are unknown. However, the infections were most likely associated with precedent dental or sinus infections caused by P. gingivalis. Molecular diagnosis using PCR technique can be helpful in identification of the pathogen given the difficulties in cultivation process of this bacteria in anaerobic conditions.[16] Because of the broad susceptibility to antibiotics of P. gingivalis, all beta-lactam antibiotics with good CNS penetration and metronidazole are treatment options for the CNS infections.[17] The duration of therapy should be at least 6 weeks, but also depends on the resolution of the infections. Overall treatment outcomes according to these three reported cases are good.
This is the first documented case of subdural empyema due to P. gingivalis. Infections caused by P. gingivalis should be considered in differential diagnoses of CNS abscesses or subdural empyema especially in patients with precedent periodontal diseases and sinusitis. Molecular identification using PCR technique could aid the definite diagnosis as this anaerobic bacterium is difficult to grow. Combination therapy with surgical drainage of the infected site and appropriate antibiotic therapy is the key for success and good outcomes.
Ethical approval
This case report is approved by the Ethics committee expedite review at the Thammasat University, Thailand.
Acknowledgement
This work was supported by the National Research University Project of Thailand Office of Higher Education Commission.
Footnotes
Source of Support: National Research University Project of Thailand Office of Higher Education Commission
Conflict of Interest: None declared
References
- 1.Youmans JR. Philadelphia: Saunders; 1996. Neurological surger: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical problems. [Google Scholar]
- 2.Nathoo N, Nadvi SS, van Dellen JR, Gouws E. Intracranial subdural empyemas in the era of computed tomography: A review of 699 cases. Neurosurgery. 1999;44:529–35. doi: 10.1097/00006123-199903000-00055. [DOI] [PubMed] [Google Scholar]
- 3.Hlavin ML, Kaminski HJ, Fenstermaker RA, White RJ. Intracranial suppuration: A modern decade of postoperative subdural empyema and epidural abscess. Neurosurgery. 1994;34:974–80. doi: 10.1227/00006123-199406000-00004. [DOI] [PubMed] [Google Scholar]
- 4.De Louvois J, Hurley R, Gortvai P. Treatment of cerebral abscesses. Br Med J. 1977;2:1284–5. doi: 10.1136/bmj.2.6097.1284-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Louvois J, Gortvai P, Hurley R. Antibiotic treatment of abscesses of the central nervous system. Br Med J. 1977;2:985–7. doi: 10.1136/bmj.2.6093.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boutaga K, van Winkelhoff AJ, Vandenbroucke-Grauls CM, Savelkoul PH. Comparison of real-time PCR and culture for detection of Porphyromonas gingivalis in subgingival plaque samples. J Clinical Microbiol. 2003;41:4950–4. doi: 10.1128/JCM.41.11.4950-4954.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bostanci N, Belibasakis GN. Porphyromonas gingivalis: An invasive and evasive opportunistic oral pathogen. FEMS Microbiol Lett. 2012;333:1–9. doi: 10.1111/j.1574-6968.2012.02579.x. [DOI] [PubMed] [Google Scholar]
- 8.Pflughoeft KJ, Versalovic J. Human microbiome in health and disease. Annu Rev Pathol. 2012:99–122. doi: 10.1146/annurev-pathol-011811-132421. [DOI] [PubMed] [Google Scholar]
- 9.Yang HW, Huang YF, Chou MY. Occurrence of Porphyromonas gingivalis and Tannerella forsythensis in periodontally diseased and healthy subjects. J Periodontol. 2004;75:1077–83. doi: 10.1902/jop.2004.75.8.1077. [DOI] [PubMed] [Google Scholar]
- 10.van Winkelhoff AJ, Slots J. Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in nonoral infections. Periodontol 2000. 1999;20:122–35. doi: 10.1111/j.1600-0757.1999.tb00160.x. [DOI] [PubMed] [Google Scholar]
- 11.Okuda K, Fukumoto Y, Takazoe I. Enumeration of cultivable black-pigmented Bacteroides species in human subgingival dental plaque and fecal samples. Oral Microbiol Immunol. 1988;3:28–31. doi: 10.1111/j.1399-302x.1988.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 12.Wu TJ, Chiu NC, Huang FY. Subdural empyema in children--20-year experience in a medical center. J Microbiol Immunol Infect. 2008;41:62–7. [PubMed] [Google Scholar]
- 13.Jim KK, Brouwer MC, van der Ende A, van de Beek D. Subdural empyema in bacterial meningitis. Neurology. 2012;79:2133–9. doi: 10.1212/WNL.0b013e3182752d0e. [DOI] [PubMed] [Google Scholar]
- 14.Iida Y, Honda K, Suzuki T, Matsukawa S, Kawai T, Shimahara T, et al. Brain abscess in which Porphyromonas gingivalis was detected in cerebrospinal fluid. Br J Oral Maxillofac Surg. 2004;42:180. doi: 10.1016/S0266-4356(03)00190-6. [DOI] [PubMed] [Google Scholar]
- 15.Ito E, Saito K, Nagatani T, Teranishi M, Aimi Y, Wakabayashi T. Cavernous sinus thrombophlebitis caused by Porphyromonas gingivalis with abscess formation extending to the orbital cavity. Case report. Neurol Med Chir (Tokyo) 2009;49:370–3. doi: 10.2176/nmc.49.370. [DOI] [PubMed] [Google Scholar]
- 16.Al Masalma M, Lonjon M, Richet H, Roche PH, Drancourt M, Raoult D, et al. Metagenomic analysis of brain abscesses identifies specific bacterial associations. Clinical Infect Dis. 2012;54:202–10. doi: 10.1093/cid/cir797. [DOI] [PubMed] [Google Scholar]
- 17.Andres MT, Chung WO, Roberts MC, Fierro JF. Antimicrobial susceptibilities of Porphyromonas gingivalis, Prevotella intermedia, and Prevotella nigrescens spp. isolated in Spain. Antimicrob Agents Chemother. 1998;42:3022–3. doi: 10.1128/aac.42.11.3022. [DOI] [PMC free article] [PubMed] [Google Scholar]


