Abstract
Background:
RTIs/STIs present a huge burden of disease, adversely impact reproductive health, and cause suffering for both men and women with consequences more devastating and widespread among women. These infections often go undiagnosed and untreated.
Objectives:
1) To identify the most common reported symptoms of RTI/STI among married women aged 15-44 years in an urban population of Ludhiana. 2) To identify important risk factors associated with symptoms of RTI/STI in the study population.
Materials and Methods:
A cross-sectional study was carried out among married women aged 15-44 years in an urban area in Ludhiana, using the WHO-Syndromic Approach for diagnosis and management of RTIs/STIs. The sample consisted of 260 eligible women obtained by systematic random sampling, from amongst those residing in the population served by one MPHW (F).
Results:
The prevalence of symptoms suggestive of RTIs/STIs in the study population was found to be 17.3%. The most common symptoms reported by the women sufferers were urinary (dysuria 57.8%, frequent urination 53.3%), followed by dyspareunia (26.7%), unusual vaginal discharge (24.4%) and vaginal itching (22.2%). Age 35-44 years, gravidity >4, education high school/above, joint families, history of abortion, and using ordinary cloth during menstruation were found to be significant risk factors. 64.4% of those with symptoms were untreated, 68.7% of those treated reported partial relief, most of those treated preferred private doctors, and the partners were not treated.
Keywords: Prevalence, reproductive tract infections, sexually transmitted infections, women of reproductive age group, syndromic diagnosis
INTRODUCTION
Reproductive tract infections (RTIs) including sexually transmitted infections (STIs) present a huge burden of disease and adversely impact reproductive health. They cause suffering for both men and women around the world, but their consequences are far more devastating and widespread among women. These infections often go undiagnosed and untreated. About 40% of women in India are estimated to have RTI/STI at any given point of time, but only 1% completes the full treatment of both partners.[1] The World Health Organization (WHO) recommends the syndromic approach for the diagnosis and management of RTIs/STIs,[2] through which a health worker at the most peripheral level without using laboratory support, can diagnose RTIs and prescribe treatment or advise referral of the patient.[3] With this methodology, a study in Punjab found the prevalence of RTIs/STIs in “eligible women” (usual residents, currently married, aged 15-44 years, whose marriage was consummated) to be 27.8% (rural 27.8%, urban 27.9%) as women who reported at least one symptom of RTI/STI.[4] Due to paucity of population based studies in this part of the state on this important public health problem, the present study was undertaken.
Aims and objectives
To estimate the prevalence of the symptoms suggestive of RTIs/STIs reported among married women aged 15-44 years in an urban population of Ludhiana
To identify major demographic and socio-economic risk factors associated with RTIs/STIs in the study population.
MATERIALS AND METHODS
Study period: 2 months (16th May 2011-15th July 2011).
Study design: Cross-sectional, descriptive study.
Study population: “Eligible Women” in 4,566 population covered by one female multi-purpose health worker (MPHW-F), in an urban area of Ludhiana.
Sample size: Taking 28% as the prevalence of RTI/STIs among urban eligible women in Punjab,[4] the minimum sample size required at 95% confidence limits and 10% allowable error, was 1030. This being too large a sample for a medical student to study in the short span of theIndian Council of Medical Research Short-term Studentship (ICMR-STS) Project, the minimum sample size required with 20% allowable error was taken, which was 257. A One-third sample (one in three) of the 774 eligible women in the study population, i.e., 257, obtained by systematic random sampling method, was planned to be studied. The actual number of women studied was 260.
Data collection and analysis
Institutional Research and Ethics Committee approval for the study was obtained before commencement. The respondents were visited in their homes by the student investigator, accompanied by the MPHW-F. After obtaining signed informed consent from the respondent, information was obtained on a pre-designed questionnaire. The respondents were interviewed by the student investigator with the help of the MPHW-F to assist in communicating with the respondents in the local language (Punjabi/Hindi). In addition to demographic and socio-economic details of the respondents, information was obtained regarding the presence of symptoms of RTIs/STIs as per the WHO syndromic approach protocol. RTI/STI was said to be present if the respondent reported the presence of at least one of the symptoms. The data was analysed by proportions, using Epi Info version-6 software.[5] Chi-square test was applied where applicable.
RESULTS
The most common symptoms of RTI/STI reported by the respondents were pain on urination (57.8%), followed by frequent urination (53.3%), pain during sexual intercourse (26.7%), unusual vaginal discharge (24.4%) and vaginal itching (22.2%). Urethral discharge, genital sore and lower abdominal pain were reported by 4.4% respondents while no one had painful inguinal lymphadenopathy.
Table 1 shows the prevalence of symptoms suggestive of RTI/STI in relation to some biological and reproductive factors. The prevalence of RTI/STI, based upon the presence of one or more symptom reported by the respondent, was found to be 17.3% in the women studied. It was highest (22.6%) in the 35-44 years old and 11.8% in the 25-34 years old. None of the youngest eligible women (15-24 years old) had any symptoms suggestive of RTI/STI. The differences were statistically significant (P = 0.024)
Table 1.
Prevalence of symptoms suggestive of RTI/STI in relation to some biological and reproductive factors
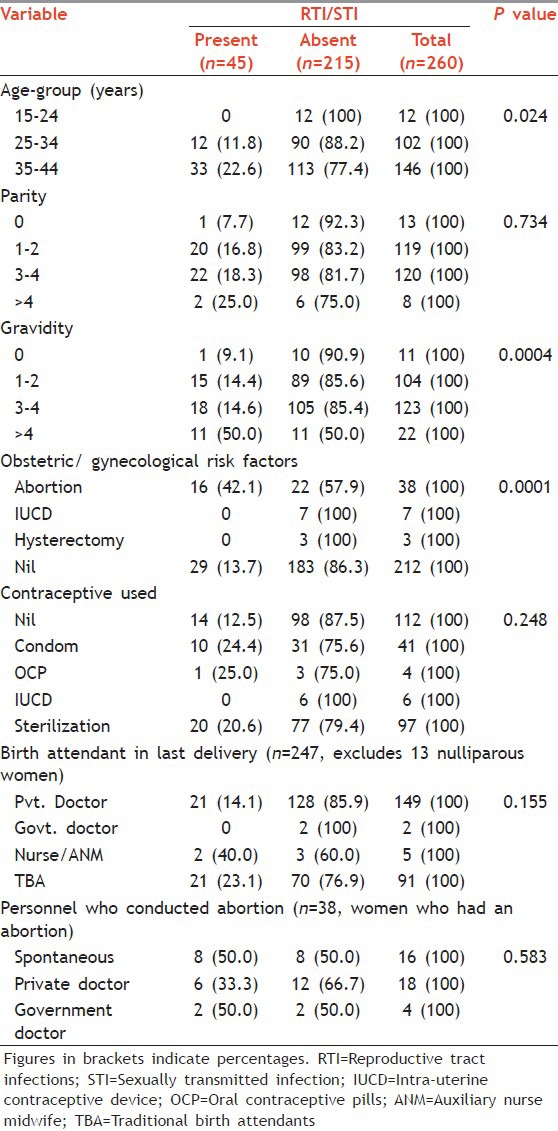
The prevalence of the symptoms increased with parity, with the prevalence being lowest (7.7%) in the nulliparous and highest (25.0%) in the multiparous with parity >4. The prevalence was 16.8% in those with parity 1-2 and 18.3% in those with parity 3-4. However, the differences were statistically not significant (P = 0.734).
The prevalence increased with gravidity, being highest (50.0%) in those with gravidity >4 and lowest (9.1%) in the nulligravida. It was similar, 14.4% and 14.6%, respectively, in those with gravidity 1-2 and 3-4. The differences were statistically highly significant (P = 0.0004).
The prevalence was highest (42.1%) in those who had a history of the previous abortion and 13.7% in those who had none of the risk factors of abortion, hysterectomy or intrauterine contraceptive device (IUCD) use. There were only seven IUCD users and three women who had a hysterectomy and none of them had symptoms suggestive of RTI/STI. The differences were statistically highly significant (P = 0.0001). Those who had a history of abortion were at significantly higher risk of RTI/STI symptoms as compared with those who had none of the risk factors of abortion, hysterectomy or IUCD-use [OR: 4.59 (95% CI: 2.02-10.42)].
The prevalence of symptoms suggestive of RTI/STI was similar (25.0% and 24.4%, respectively), in users of oral contraceptive pills and condom users, 20.6% in sterilized women and 12.5% in those who didn’t use any contraceptives. However, the differences were statistically not significant (P = 0.248).
The prevalence of the symptoms was found to be highest (40.0%) in those who had their last delivery conducted by a nurse/auxiliary nurse midwife (ANM), but the numbers were very small (total five deliveries conducted by nurse/ANM). Only two deliveries were conducted by a government doctor and none of these respondents reported symptoms of RTI/STI. The prevalence of the symptoms was 23.1% and 14.1% in women who had been last delivered by traditional birth attendants (TBAs) and private doctor, respectively. The differences were statistically not significant (P = 0.155).
The prevalence of the symptoms was 50.0% in women who had suffered a spontaneous abortion and 33.3% in those who had abortion performed by a private doctor. There were only four women who had abortion performed by a government doctor and two of them reported symptoms of RTI/STI. However, the differences were statistically not significant (P = 0.583).
Table 2 shows the prevalence of RTI/STI in relation to some socio-economic factors. The prevalence of RTI/STI was highest (46.1%) in those with education high school or above, followed by the illiterate (20.0%), 13.7% in those with primary level education and 12.9% in those with education up to matric. The differences were statistically significant (P = 0.023).
Table 2.
Prevalence of symptoms suggestive of RTI/STI in relation to some socio-economic factors
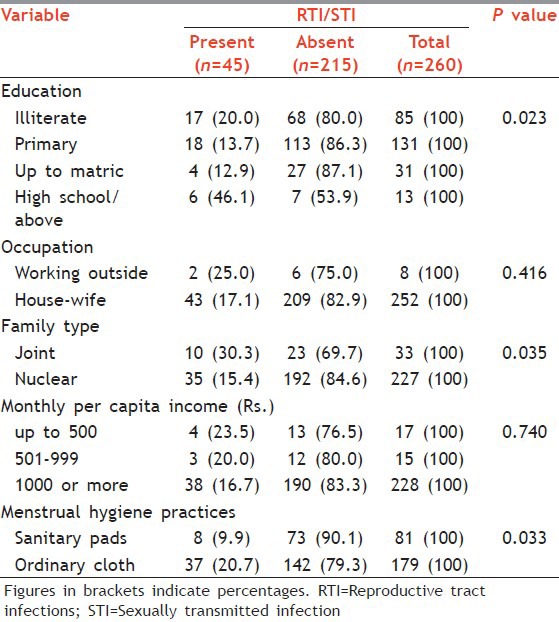
There were only eight women in the sample who were working outside and 2 (25.0%) of them reported symptoms suggestive of RTI/STI. In the 252 housewives, the prevalence of RTI/STI was 17.1%. However, the differences were statistically not significant (P = 0.416).
The prevalence of symptoms of RTI/STI was 30.3% in those living in joint families and 15.4% in those living in nuclear families. The differences were statistically significant (P = 0.035). Those living in joint families had significantly higher risk of having symptoms of RTI/STI, with OR: 2.39 (95% CI: 0.96-5.83).
The prevalence of the symptoms decreased with increasing monthly per capita income (MPCI). It was highest (23.5%) in the poorest (those with MPCI of ≤Rs. 500), 20.0% in those with MPCI Rs 501-999 and 16.7% in those with MPCI ≥ Rs. 1000. However, the differences were statistically not significant (P = 0.740).
The prevalence of the symptoms was higher (20.7%) in those who used ordinary cloth during menstruation as compared with those who used sanitary pads (9.9%) and the differences were statistically significant (P = 0.033), with OR: 2.38 (95% CI: 1.00-5.86).
Treatment-seeking behavior of those who reported symptoms of RTI/STI (n = 45, table deleted): 29 (64.4%) of the 45 women who reported symptoms suggestive of RTIs/STIs did not receive any treatment, 10 (22.2%) took treatment from a private practitioner, 5 (11.1%) opted for “desi” medicines and only one respondent sufferer (2.2%) took treatment from a government doctor. Out of 16 women who took treatment of any kind, only 3 (18.7%) reported complete relief, 11 (68.7%) reported partial relief while 2 (12.5%) reported no relief from the treatment they had received. None of the partners of the 45 women who reported symptoms suggestive of RTIs/STIs received treatment.
DISCUSSION
The prevalence of symptoms suggestive of RTIs/STIs in the study population (17.3%) is low as compared with the country as a whole (40%)[1] and to what is found in other studies in India, 27% in urban women of Agra district of Uttar Pradesh,[6] 35.6% in reproductive age women living in urban slums of Tirupati, Andhra Pradesh,[7] 32% in urban women in Sundergarh district of Orissa[8] and 27.8% in Punjab.[4] This suggests that many women in the study population may be asymptomatic or have symptoms that are considered “normal” for women. This is further suggested by the fact that the majority of the women sufferers under study (64.4%) did not seek any treatment.
The most common symptoms reported by the women sufferers under study were urinary (dysuria 57.8%, frequent urination 53.3%), followed by dyspareunia (26.7%), unusual vaginal discharge (24.4%) and vaginal itching (22.2%). Dysuria and frequent micturition are symptoms also associated with urinary tract infection, which could not be ruled out in the present community-based study without further laboratory investigation. Moreover, some dysuria can also occur due to dehydration and, as this study was carried out during the peak summer months, this aspect could also not be ruled out. Other Indian studies,[6,7,8,9] have reported the commonest symptom of RTIs/STIs to be vaginal discharge, followed by lower abdominal pain.
The prevalence of the symptoms were highest in the 35-44 years old, in those with gravidity >4, those with higher education (high school/above), those living in joint families, those with a history of abortion and those who used ordinary cloth during menstruation. For all these factors, the differences were found to be statistically significant. No statistically significant relationship was established between RTIs/STIs and parity, occupation, income, birth attendant in last delivery, personnel who conducted the abortion and contraceptive use. Bhawsar et al.[4] also found the prevalence of RTIs/STIs among women in Punjab to be significantly higher in those with history of abortions; however, contrary to our study, they found the prevalence to be highest in the 15-19 years old and lowest in those aged 30+, highest in those with no children, the illiterate, in those with low standard of living and in the tubectomized. Sri Devi and Swarnalatha[7] reported significantly higher prevalence of RTIs/STIs in the 20-24 years old, those living in joint families, the unskilled workers, the poorest, those with no or one live birth, in those using IUCD, in those whose delivery was conducted by a family member or TBA and in those who used ordinary cloth during menstruation. Nandan et al.[6] reported the highest prevalence of RTIs/STIs in the 25-34 years old, in those having 1-2 children and the illiterate. The reason for the higher prevalence of symptoms suggestive of STI/RTI found in those with higher education level (high school/above) in our study, contrary to the findings of other researchers,[4,5] may be because of a small sample size, there being only 13 women in this category in the sample studied. The higher prevalence of the symptoms found in those living in joint families is in agreement with the findings of Sri Devi and Swarnalatha[7] and may be because women in joint families generally have less privacy and decision-making power, affecting their treatment-seeking opportunities.
The majority (64.4%) of the respondents with symptoms did not seek any treatment. Of those who did seek treatment, 81.2% had partial or no relief and none of the respondents reported treatment of a partner. The preferred source of treatment was a private practitioner, followed by “desi” medicines. Women suffer from reproductive morbidities for a long time because of the prevailing “culture of silence.”[10] Many women believe that reproductive health problems (discharge or pain) are simply “women's fate” and therefore not a condition for which they should seek medical help. Moreover, women are generally reluctant to discuss their genital health problems with their husbands or health providers.[11] According to a national level study during September 2004-October 2005, the health seeking behavior among the general population of India showed that for STI/RTI treatment people preferred non-modern medicine (74%) over modern medicine qualified practitioners (12%) while 14% did not seek treatment.[12] Our findings are similar to those of Bhawsar et al.[4] who also found that most of the women (54.6%) with symptoms of RTI/STI in Punjab did not receive treatment, 28.2% opted to be treated by a private doctor and only 6.2% by a government doctor. Sri Devi and Swarnalatha,[7] however, found government doctor to be the preferred source of treatment for RTI/STI by majority (76.7%) of women, with 39.5% reporting partial and 57.2% reporting complete relief and 90.7% reporting no partner treatment. RTI is a common, but neglected health problem in women during their reproductive age.
CONCLUSIONS
The prevalence of symptoms suggestive of RTIs/STIs among married women of reproductive age in the study population was found to be 17.3%, which is low as compared with the prevalence reported in other studies. The most common symptoms reported by the women sufferers were urinary (dysuria 57.8%, frequent urination 53.3%), followed by dyspareunia (26.7%), unusual vaginal discharge (24.4%) and vaginal itching (22.2%). Age 35-44 years, gravidity >4, higher education (high school/above), joint families, history of abortion and using repeatedly-washed cloths during menstruation were found to be a significant risk factors for RTIs/STIs in the study population. Nearly, 64.4% of those with symptoms were untreated, showing that the majority of women bear the brunt of RTIs/STIs silently without seeking treatment. Those who do get treated mostly prefer private doctors and their partners do not get treated at all.
Recommendations
The treatment and control of RTIs/STIs needs to be part of the primary health-care. Grass-root level health workers should be trained to identify RTIs/STIs through the syndrome approach. They need to educate women about reproductive health issues and encourage them to seek treatment for their problems and also encourage their partners to get treated at the same time. They should be able to affect behavior changes that are conducive to maintenance of reproductive health.
ACKNOWLEDGMENT
The authors gratefully acknowledge the support of ICMR (STS-2012) for this study.
Footnotes
Source of Support: ICMR (STS-2012)
Conflict of Interest: None declared.
REFERENCES
- 1.New Delhi: National AIDS Control Organization; 2007. GOI, MOHFW. National Guidelines on Prevention, Management and Control of Reproductive Tract Infections Including Sexually Transmitted Infections. [Google Scholar]
- 2.Introducing STI Syndromic Case Management. 2nd ed. Geneva: World Health Organization; 2007. WHO. Training Modules for the Syndromic Management of Sexually Transmitted Infections. Module 2. [Google Scholar]
- 3.Simplified RTI and STI Treatment Guidelines. New Delhi: National AIDS Control Organization; 1999. GOI, MOHFW. [Google Scholar]
- 4.Bhawsar RD, Singh JP, Khanna A. Determinants of RTIs/STIs among women in Punjab and their health seeking behaviour. Indian J Fam Welf. 2005;51:24–34. [Google Scholar]
- 5.Dean AG, Dean JA, Coulombier D, Brendel KA, Smith DC, Burton AH, et al. Epi Info Version 6: A word processing, database and statistics program for epidemiology on microcomputers. Centers for Disease Control and Prevention, Atlanta, Georgia, U.S.A. 1994 [Google Scholar]
- 6.Nandan D, Misra SK, Sharma A, Jain M. Estimation of prevalence of RTI's/STD's among women of reproductive age group in district Agra. Indian J Community Med. 2002;27:110–3. [Google Scholar]
- 7.Sri Devi B, Swarnalatha N. Prevalence of RTI/STI among reproductive age women (15-49 years) in urban slums of Tirupati Town, Andhra Pradesh. Health Popul Perspect Issues. 2007;30:56–70. [Google Scholar]
- 8.Panda SC, Sarangi L, Bebartta D, Parida S, Panigrahi OP. Prevalence of RTI/STI among women of reproductive age in district Sundergarh (Orissa) [Last accessed on 2011 May 16];Indian J Pract Doct. 2007 4 Available from: http://www.indmedica.com/journals.php? journalid=3 & issueid=94 . [Google Scholar]
- 9.Pawanarkar J, Chopra K. Prevalence of lower reproductive tract infection in infertile women. Health Popul Perspect Issues. 2004;27:67–75. [Google Scholar]
- 10.Luthra UK, Mehta S, Bhargava NC. Reproductive tract infections in India: The need for comprehensive reproductive health policy and programs. In: Germain A, Holmes KK, Piot P, et al., editors. Reproductive Tract Infections. New York: Plenum Press; 1992. pp. 317–42. [Google Scholar]
- 11.Patel BC, Khan ME. Reproductive health problems of women in rural Uttar Pradesh: Observations from a community survey. Soc Change. 1996;26:245–70. [Google Scholar]
- 12.New Delhi: National AIDS Control Organization; 2007. GOI, MOHFW, NACO. Operational guidelines for strengthening STI/RTI services; p. 28. [Google Scholar]


