Abstract
Purpose
Many studies have reported on the use of narrow band imaging (NBI) colonoscopy to differentiate neoplastic from non-neoplastic colorectal polyps. It has potential to replace pathological diagnosis of diminutive polyps. We aimed to perform a systematic review and meta-analysis on the real-time diagnostic operating characteristics of NBI colonoscopy.
Methods
We searched PubMed, SCOPUS and Cochrane databases and abstracts. We used a two-level bivariate meta-analysis following a random effects model to summarise the data and fit hierarchical summary receiver-operating characteristic (HSROC) curves. The area under the HSROC curve serves as an indicator of the diagnostic test strength. We calculated summary sensitivity, specificity and negative predictive value (NPV). We assessed agreement of surveillance interval recommendations based on endoscopic diagnosis compared to pathology.
Results
For NBI diagnosis of colorectal polyps, the area under the HSROC curve was 0.92 (95% CI 0.90 to 0.94), based on 28 studies involving 6280 polyps in 4053 patients. The overall sensitivity was 91.0% (95% CI 87.6% to 93.5%) and specificity was 82.6% (95% CI 79.0% to 85.7%). In eight studies (n=2146 polyps) that used high-confidence diagnostic predictions, sensitivity was 93.8% and specificity was 83.3%. The NPVs exceeded 90% when 60% or less of all polyps were neoplastic. Surveillance intervals based on endoscopic diagnosis agreed with those based on pathology in 92.6% of patients (95% CI 87.9% to 96.3%).
Conclusions
NBI diagnosis of colorectal polyps is highly accurate—the area under the HSROC curve exceeds 0.90. High-confidence predictions provide >90% sensitivity and NPV. It shows high potential for real-time endoscopic diagnosis.
Keywords: Colonic Polyps, Colorectal Neoplasia, Colorectal Cancer Screening, Meta-Analysis, Colonoscopy
Significance of this study.
What is already known about this subject?
Pathological evaluation for polyps found at colonoscopy for colorectal cancer screening is expensive.
Narrow band imaging (NBI) makes neoplastic polyps appear darker, aiding in their differentiation from non-neoplastic lesions.
Many studies have evaluated the performance of endoscopic diagnosis with NBI compared with pathology.
What are the new findings?
Real-time endoscopic diagnosis of colorectal polyps is a highly accurate test, with the area under the summary receiver operator curve exceeding >0.90.
Surveillance intervals dictated by endoscopic diagnosis agree with pathology-directed surveillance intervals in more than 90% of patients.
How might it impact on clinical practice in the foreseeable future?
Endoscopists may move toward endoscopic diagnosis of colorectal polyps, forgoing pathological evaluation, particularly in high-confidence predictions.
Endoscopic diagnosis holds promise for making colonoscopy more cost effective and efficient by potentially avoiding the need for pathological examination.
Introduction
Colonoscopy with polypectomy is considered effective at preventing colorectal cancer deaths.1 However, its expense makes it potentially less cost effective than other screening methods.2 All polyps, even diminutive polyps that rarely harbour dysplasia,3 are routinely sent for pathological evaluation, and this can incur major costs.4 Pathology diagnoses are needed to determine the patient's interval to the next surveillance colonoscopy.5 Real-time endoscopic diagnosis, in which endoscopists diagnose polyp histology at the moment of identification, may have similar diagnostic operating characteristics as pathological evaluation at a significantly reduced cost.
Narrow band imaging (NBI) technology highlights the increased vasculature of neoplastic tissue and makes neoplastic polyps appear darker than surrounding mucosa. This allows for improved differentiation of polyps compared with that using white light.6 As such, an international classification to distinguish neoplasms such as adenomas from non-neoplasms such as hyperplastic polyps with the use of NBI has been developed and validated (figure 1).7 Real-time differentiation has been proposed as part of a ‘resect and discard’ strategy in which diminutive (≤5 mm) neoplastic polyps are resected without pathological evaluation, and diminutive rectosigmoid non-neoplastic polyps are left in situ.8 Such a strategy could allow for surveillance intervals to be communicated to the patient on the day of colonoscopy, and confer substantial cost savings by avoiding pathology and endoscopy fees.4 9 It could also decrease unnecessary polypectomy, a risk factor for major colonoscopy-related complications such as perforation and bleeding.10
Figure 1.
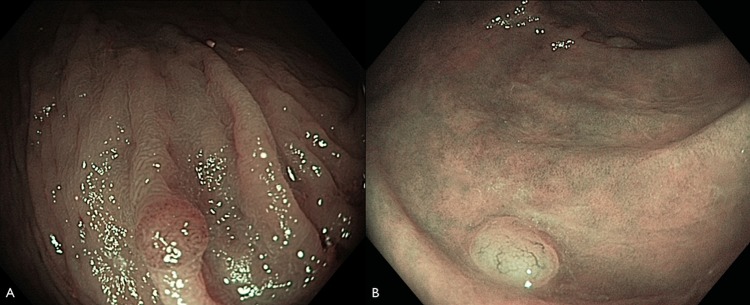
Endoscopic image with narrow band imaging of diminutive colorectal polyps. (A) Adenoma and (B) non-neoplastic polyp.
The potential for applying the ‘resect and discard’ strategy to clinical use depends to a large extent on the accuracy of real-time endoscopic diagnosis. Numerous prospective studies have compared endoscopic diagnosis of polyps with NBI to a reference standard of histology. These data are valuable to allow us to understand its diagnostic operating characteristics, which, in turn, could provide insights of its potentials for clinical use. The aim of this study was to carry out a systematic review and meta-analysis on the real-time performance of endoscopic diagnosis.
Methods
Search strategy and study selection
We (TK and SM) conducted a computerised literature search of the PubMed, SCOPUS (including EMBASE) and Cochrane Library databases up to June 2012. In addition, we searched the abstracts of conference proceedings of Digestive Diseases Week and American College of Gastroenterology. We designed the search queries with a biomedical research librarian to capture all articles related to NBI and colonoscopy. Studies in PubMed were identified with the terms narrow band or optical filter combined with the set operator AND with studies identified with the MeSH terms colonoscopy, colonic neoplasms or colonic polyps or with words beginning with colorect, adenoma, colonoscop or polyp. Studies in SCOPUS were identified with the terms narrow band or optical filter combined with the set operator AND with words beginning with colorect, adenoma, colonoscop or polyp. The electronic archives of conference proceedings were searched using the term narrow band, and abstracts that included this term were reviewed in detail for potential inclusion. We subsequently manually searched the citations from published reviews. Following the initial search, we identified articles for appropriateness, and performed a detailed full text assessment of potentially relevant studies.
We included studies that prospectively evaluated patients undergoing colonoscopy during which endoscopists used NBI to make a real-time prediction of polyp histology (neoplastic or non-neoplastic), and compared this with histology as the reference standard. We excluded studies that primarily analysed still images to predict polyp histology; those that included patients with inflammatory bowel disease, hereditary nonpolyposis colorectal cancer or familial polyposis syndromes; as well as those primarily designed as a retrospective study, review, editorial or meta-analysis. We translated papers that were not written in English. We discussed and resolved disagreement between investigators. Our protocol is available by request.
Data extraction
We extracted data independently onto standardised paper forms. We constructed 2×2 tables that contained the number of polyps found to be true positives (neoplastic polyps that were endoscopically predicted to be neoplastic), true negatives (non-neoplastic polyps that were endoscopically predicted to be non-neoplastic), false positives (non-neoplastic polyps that were endoscopically predicted to be neoplastic) and false negatives (neoplastic polyps that were endoscopically predicted to be non-neoplastic). When possible, additional 2×2 tables were constructed for polyps ≤5 mm, 6–9 mm and ≥10 mm, and high-confidence and low-confidence predictions. In general, a real-time diagnosis was described as high confidence when the polyp had endoscopic features strongly suggestive of its pathology, and the endoscopist could make a clinical management and surveillance decision based on his or her endoscopic diagnosis. We contacted study authors when there were insufficient published data to construct the 2×2 table for all results. In addition, the following data were extracted for each trial, when available: period of enrolment, number of endoscopists who individually performed colonoscopies on patients in the cohort, number of these who were expert endoscopists, total number of patients enrolled, number of patients with polyps examined by NBI for accuracy data, inclusion and exclusion criteria for participants; patient data including age, sex and indication for colonoscopy; size criterion for polyps examined for real-time diagnosis; polyp location, size and shape by Paris classification11; and histology. We also extracted the diagnostic criteria used to differentiate neoplasms from non-neoplasms, and the features of the diagnostic modalities used, including NBI LUCERA or EXERA processor systems, high definition or high resolution, and the use of optical or digital magnification. Expert endoscopists were defined as those attending endoscopists with significant experience performing colonoscopy and using NBI.
Study quality assessment
To assess study quality and potential for bias, we used the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool.12 We rated the quality of key study design characteristics such as prespecified inclusion and exclusion criteria, defined diagnostic criteria, blinding of endoscopists to the pathological diagnosis, description of a reference standard and the inclusion of all patients in the analysis.
Statistical methods
We performed a bivariate meta-analysis using a linear mixed model approach to calculate summary estimates of sensitivity, specificity, positive likelihood ratio and negative likelihood ratio, and to fit a hierarchical summary receiver-operating characteristic (HSROC) curve.13 14 We used summary estimates of sensitivity and specificity to estimate the negative and positive predictive values when neoplasms accounted for 60%, 50%, 40% and 30% of all polyps based on prior published values.3 15 16 We performed prespecified subgroup analyses for published studies alone, diminutive polyps, high-confidence predictions, diminutive high-confidence predictions, diagnoses with NBI LUCERA and EXERA systems. To perform a sensitivity analysis, we performed subgroup analyses for high-quality and highest-quality studies, which were not prespecified. We calculated the area under the HSROC curve for the main analysis and subgroup analyses. We used random effects to calculate summary estimates for feasibility of high-confidence diagnoses and assessed agreement of surveillance interval recommendations based on endoscopic diagnosis compared with those based on the pathological diagnosis. We used Stata V.11 to perform the calculations.
Results
Eligible studies
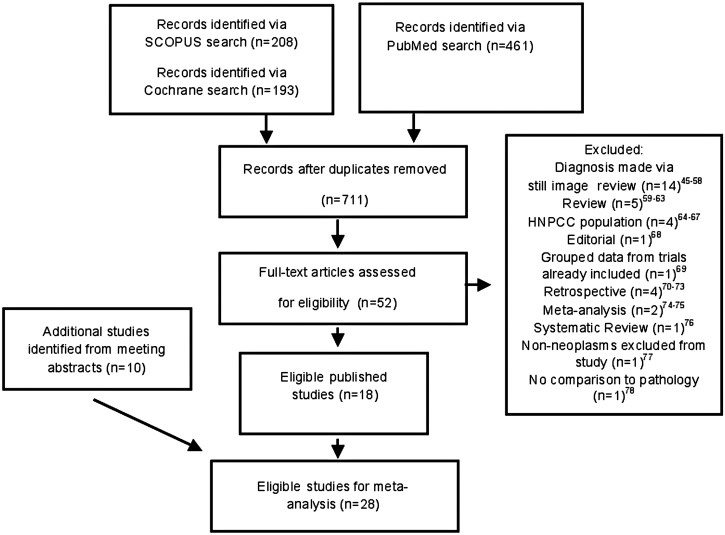
Twenty-eight studies consisting of 18 full published papers6 17–33 and 10 abstracts34–43 fulfilled the study inclusion criteria and were analysed. These 28 studies were selected from 711 screened citations. We excluded 658 citations based on the title and abstract. Of the 52 articles selected for full text review, 14 were excluded as they had predicted polyp histology based on still images,44–57 5 were review articles,58–62 4 were excluded because they involved a hereditary nonpolyposis colorectal cancer population,63–66 and 11 exclusions were based on other criteria67–77 (figure 2). Eventually, we identified 18 papers and 14 abstracts that met eligibility criteria. Four abstracts78–81 with a total of 541 polyps (359 patients) were subsequently excluded for missing data despite contacting the investigators.
Figure 2.
Flow chart of the search strategy and selected studies.
Study characteristics
The 28 studies included a total of 6280 polyps that were diagnosed in 4053 patients. The characteristics of the included studies are listed in table 1. Fourteen studies were performed in the USA, seven in Asia, six in Europe and one in Australia. Twenty studies used the EXERA; eight used the LUCERA systems of NBI. The criteria used for prediction of polyp histology varied: six used Kudo pit pattern classification, four used the Narrow Band Imaging International Colorectal Endoscopic (NICE) classification, and others used less defined criteria of polyp colour or vascular pattern. Overall, 63% of all polyps analysed were neoplastic—the range was from 38% to 89%.
Table 1.
Study characteristics
| Study, year | Study no. | Country | Diagnostic modality | Diagnostic criteria | Endoscopists number | No. of experts | Patients analysed | Polyps analysed | No. of neoplasms/No. of non-neoplasms | Polyps, n (%) with high confidence predictions |
|---|---|---|---|---|---|---|---|---|---|---|
| Buchner et al (2010)17 | 1 | USA | Exera | Kudo | 2 | 2 | 75 | 41 | 25/16 | |
| Henry et al (2010)19 | 2 | USA | Exera | Sano-Emura | 1 | 1 | 52 | 126 | 67/59 | |
| Hirata et al (2007)69 | 3 | Japan | Lucera | Brown hue | 2 | 2 | 99 | 148 | 132/16 | |
| Ignjatovic et al (2009)20 | 4 | UK | Lucera | Vascular pattern intensity | 4 | 2 | 130 | 169 | 129/40 | * |
| Lee et al (2011)21 | 5 | South Korea | Lucera | Mucosal pattern and vascular density | 1 | 1 | 142 | 156 | 80/76 | 125 (80.1%) |
| Machida et al (2004)23 | 6 | Japan | Lucera | Kudo | 2 | 2 | 34 | 43 | 34/9 | |
| Rastogi et al (2009)24 | 7 | USA | Exera | Type A: HP | 1 | 1 | 101 | 236 | 143/93 | |
| Type B: TA | ||||||||||
| Rastogi et al (2011)6 | 8 | USA | Exera | Type A: HP | 6 | 6 | 134 | 384 | 147/237 | |
| Type B: TA | ||||||||||
| Rex (2009)22 | 9 | USA | Exera | Pre NICE* | 1 | 1 | 136 | 451 | 230/221 | 368 (81.6%) |
| Rogart et al (2008)26 | 10 | USA | Exera | Vascular density, modified Kudo | 4 | 4 | 302 | 265 | 129/134 | |
| Rotondano et al (2011)27 | 11 | Italy | Lucera | Kudo | 3 | 3 | 94 | 281 | 141/140 | |
| Sakamoto et al (2012)28 | 12 | Japan | Lucera | Sano | 1 | 1 | 80 | 116 | 52/42 | |
| Sano et al (2009)29 | 13 | Japan | Lucera | Sano | 1 | 1 | 92 | 150 | 111/39 | |
| Shahid et al (2011)30 | 14 | USA | Exera | Sano | 1 | 1 | 65 | 130 | 58/72 | |
| Singh et al (2011)31 | 15 | Australia | Exera | Sano | 1 | 1 | 32 | 50 | 30/20 | 50 (100%) |
| Zhou et al (2011)32 | 16 | China | Lucera | Kudo and Sano | 1 | 1 | 118 | 109 | 67/42 | |
| Ren (2012)25 | 17 | China | Exera | Yoshiki | 1 | 1 | 75 | 116 | 52/42 | |
| Kuiper et al (2012)33 | 18 | The Netherlands | Exera | Kudo | 3 | 0 | 108 | 281 | 141/140 | 231 (82.2%) |
| Abstracts | ||||||||||
| Coe et al (2012)43 | 19 | USA | Exera | NICE | 6 | 6 | 300 | 260 | 152/108 | |
| Hewett and Rex (2010)36 | 20 | USA | Exera | Pre NICE* | 1 | 1 | 225 | 235 | 38/197 | |
| Kaltenbach et al (2011)38 | 21 | USA | Exera | NICE | 2 | 2 | 220 | 236 | 146/90 | 178 (75.4%) |
| Kaltenbach et al (2012)39 | 22 | USA | Exera | NICE | 5 | 5 | 311 | 338 | 233/105 | 246 (72.8%) |
| Matthew et al (2008)34 | 23 | USA | Exera | Reported patterns | 1 | 0 | 100 | 231 | 106/125 | |
| Occhipinti et al (2011)37 | 24 | Italy | Exera | Kudo | 5 | 5 | 93 | 220 | 120/100 | |
| Pohl et al (2012)40 | 25 | USA | Exera | NICE | 10 | NR | 608 | 948 | 528/420 | 770 (81.3%) |
| Radaelli et al (2011)41 | 26 | Italy | Exera | NR | NR | all | 197 | 354 | 233/121 | 354* |
| Ringold et al (2008)35 | 27 | USA | Exera | ‘Cerebriform’ | 4 | 4 | 55 | 93 | 56/37 | |
| Yague et al (2011)42 | 28 | Spain | Exera | Vascular patterns | 1 | 1 | 75 | 215 | 107/108 | |
*Information on the number of polyps predicted with low confidence was not provided.
NICE, Narrow Band Imaging International Colorectal Endoscopic Classification. This classification system includes criteria on polyp colour, vessels and surface pattern; NR, not reported; Pre NICE, classification systems based on similar criteria that preceded NICE.
Quality assessment
In general, the included studies met most of the quality criteria (table 2). However, in many studies it was not clear whether a consecutive or random sample of patients was enrolled, and whether all patients were included in the analysis, both of which might have introduced bias.
Table 2.
The quality assessment of diagnostic accuracy studies-2 tool for quality assessment of the included studies
| Author | DOM1A1 | DOM1A2 | DOM1A3 | DOM 1A4 | DOM1B | DOM2A1 | DOM 2A2 | DOM 2A3 | DOM 2B | DOM 3A1 | DOM 3A2 | DOM 3A3 | DOM 3B | DOM 4A1 | DOM 4A2 | DOM4A3 | DOM4A4 | DOM 4A5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Buchner et al17 | Y | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | U | Y | Y | Y | L |
| Henry et al19 | Y | Y | Y | L | L | Y | Y | L | L | Y | U | U | U | Y | Y | Y | Y | L |
| Hirata et al69 | U | Y | U | U | H | Y | Y | L | U | Y | Y | L | L | Y | Y | Y | U | U |
| Ignjatovic et al20 | Y | Y | Y | L | H | Y | Y | L | L | Y | Y | L | L | U | Y | Y | N | L |
| Lee et al21 | Y | Y | Y | L | L | Y | Y | L | U | Y | Y | L | L | Y | Y | Y | Y | L |
| Machida et al23 | U | Y | U | U | U | Y | Y | L | L | Y | U | U | L | Y | Y | U | U | U |
| Rastogi et al24 | U | Y | Y | U | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Rastogi et al6 | U | Y | Y | U | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | N | U |
| Rex22 | U | Y | U | U | U | Y | Y | L | L | Y | Y | L | L | U | Y | Y | U | U |
| Rogart et al26 | Y | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | U | Y | Y | U | U |
| Rotondano et al27 | U | Y | Y | L | L | Y | Y | L | H | Y | Y | L | L | Y | Y | Y | Y | L |
| Sakamoto et al28 | Y | Y | U | U | L | Y | Y | H | H | Y | Y | L | L | U | Y | Y | Y | L |
| Sano et al29 | Y | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | U | Y | Y | Y | L |
| Shahid et al30 | Y | Y | U | U | L | Y | Y | L | L | Y | Y | L | L | U | Y | Y | U | U |
| Singh et al31 | U | Y | Y | U | L | Y | Y | L | L | Y | Y | L | L | U | Y | Y | Y | L |
| Zhou et al32 | U | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Ren25 | U | Y | Y | U | L | Y | Y | L | L | Y | U | U | L | Y | Y | Y | N | U |
| Kuiper et al33 | U | Y | Y | U | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Abstracts | ||||||||||||||||||
| Coe et al43 | U | Y | U | U | L | Y | Y | L | L | Y | Y | L | L | Y | Y | U | Y | L |
| Hewett et al15 | U | Y | U | U | U | Y | U | U | L | Y | Y | L | L | Y | Y | Y | N | U |
| Kaltenbach et al38 | Y | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Kaltenbach et al39 | Y | Y | Y | L | L | Y | Y | L | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Matthew et al34 | Y | Y | Y | L | L | Y | U | U | L | Y | U | U | L | U | Y | Y | Y | L |
| Occhipinti et al37 | Y | Y | U | U | L | Y | Y | L | L | Y | U | L | L | Y | Y | Y | U | U |
| Pohl et al40 | U | Y | U | U | L | Y | Y | L | L | Y | U | U | L | Y | Y | Y | U | U |
| Radaelli et al41 | Y | Y | Y | L | L | Y | U | U | L | Y | Y | L | L | Y | Y | Y | Y | L |
| Ringold et al35 | U | Y | Y | U | L | Y | Y | L | L | Y | U | U | L | U | Y | Y | U | U |
| Yague et al42 | U | Y | U | U | L | Y | Y | L | L | Y | U | U | U | Y | Y | Y | U | U |
DOM, domain; DOM1A1, consecutive or random sample of patients enrolled; DOM1A2, case–control design avoided; DOM1A3, study avoided inappropriate exclusions; DOM1A4, selection of patients introduced bias; DOM1B, concern that included patients do not match the review question; DOM2A1, index test results interpreted without knowledge of results of reference standard; DOM2A2, prespecified threshold used; DOM2A3, could the conduct of index test have introduced bias; Dom2B, concern that index test conduct or interpretation differ from review question; DOM3A1, reference standard correctly classifies condition; DOM3A2, reference standard results interpreted independently from index test results; DOM3A3, could the reference standard, its conduct, or its interpretation have introduced bias; DOM3B, concern that target condition defined by reference standard does not match review question; DOM4A1, appropriate interval between index test and reference standard; DOM4A2, all patients received the reference standard; DOM4A3, patients received the same reference standard; DOM4A4, all patients included in the analysis; DOM4A5, could the patient flow have introduced bias; H, high; L, low; N, no; U, unclear; Y, yes.
Diagnostic performance of NBI diagnosis
Endoscopic diagnosis of colorectal polyps with NBI showed highly accurate diagnostic performance—the area under the HSROC curve was 0.92 (95% CI 0.90 to 0.94) (figure 3). For high-confidence predictions alone reported by eight studies, the area under the HSROC curve was 0.95 (95% CI 0.93 to 0.97), and for high-confidence predictions of diminutive polyps, the area under the HSROC curve was 0.92 (95% CI 0.92 to 0.96) (figure 4).
Figure 3.
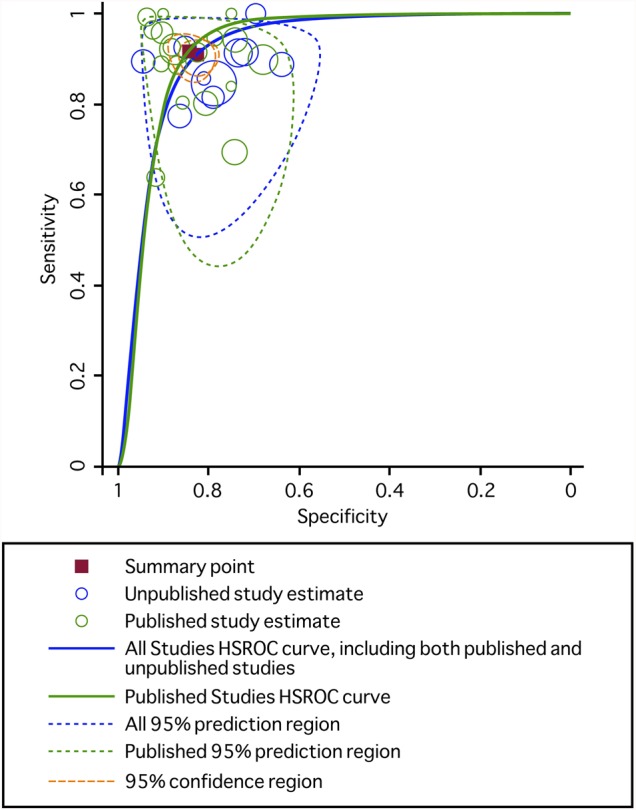
Hierarchical summary receiver-operating characteristic (HSROC) curve for the diagnostic performance of narrow band imaging to diagnose neoplastic and non-neoplastic polyps among all studies (blue line) and among published studies (green line). The size of the circles indicates the weight of the individual studies. The summary sensitivity and specificity is shown with a yellow square and the 95% confidence region is plotted. For all studies, the area under the HSROC curve was 0.92 (95% CI 0.90 to 0.94); for published studies, the area under the HSROC curve was 0.93 (0.90 to 0.95).
Figure 4.
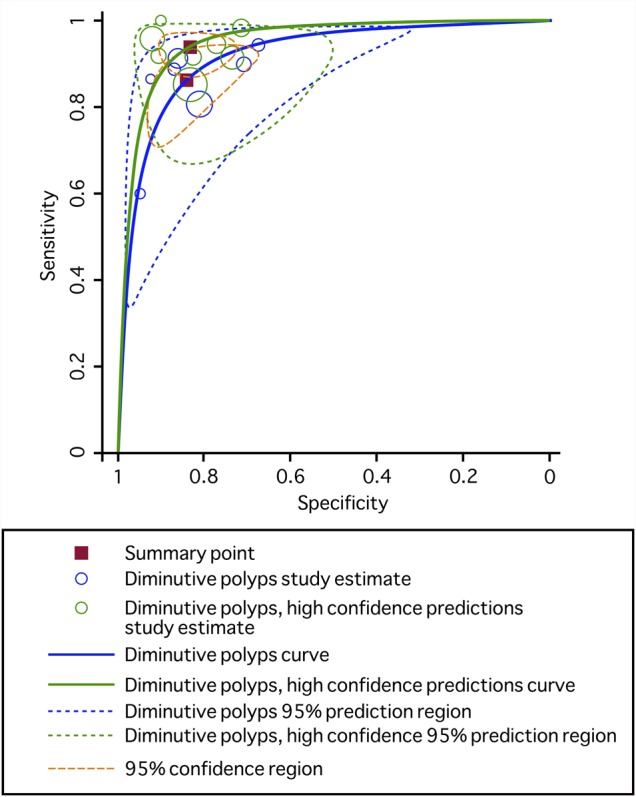
Hierarchical summary receiver-operating characteristic (HSROC) curve for the diagnostic performance of narrow band imaging to diagnose diminutive polyps (blue line) and diminutive polyps that were diagnosed with high confidence (green line). For high-confidence predictions of diminutive polyps, area under the HSROC curve was 0.94 (95% CI 0.92 to 0.96).
The main results are presented in table 3. The overall sensitivity of NBI diagnosis was 91.0% (95% CI 87.6% to 93.5%) and specificity was 82.6% (95% CI 79.0% to 85.7%) compared with histology. In six studies (n=1567 polyps) that provided information on high-confidence and low-confidence predictions, a high-confidence prediction was made in 77% of polyps (95% CI 73.3% to 80.7%). In eight studies (n=2146 polyps) that provided information on high-confidence predictions, the sensitivity and specificity for diagnosis made with high confidence was 93.8% and 83.3%, respectively. The sensitivity and specificity of diagnosis of diminutive polyps, made with high confidence was 93.4% (95% CI 87.4% to 96.7%) and 84.0% (95% CI 76.6% to 89.3%), respectively. The negative predictive values (NPVs) overall were 86.0%, 90.1%, 93.2% and 95.5% and for high-confidence predictions improved to 90.0%, 93.0%, 95.3% and 96.9% when neoplasms account for 60%, 50%, 40% and 30% of all polyps, respectively.
Table 3.
Diagnostic accuracy of endoscopic diagnosis with NBI to distinguish between neoplastic and non-neoplastic colorectal neoplasms
| Summary estimates (95% CI) | Likelihood ratio (95% CI) | |||||
|---|---|---|---|---|---|---|
| Study characteristics | No. of studies (no. of polyps) | Sens | Spec | LR+ | LR− | Area under HSROC curve (95% CI) |
| All | 28 (6280) | 91.0 (87.6 to 93.5) | 82.6 (79.0 to 85.7) | 5.2 (4.3 to 6.4) | 0.11 (0.08 to 0.15) | 0.92 (0.90 to 0.94) |
| Published manuscripts | 18 (3212) | 91.7 (87.1 to 97.4) | 84.5 (80.4 to 87.9) | 5.9 (4.6 to 7.6) | 0.10 (0.06–0.16) | 0.93 (0.90–0.95) |
| High-confidence predictions20–22 31 38–41 | 8 (2146) | 93.8 (90.1 to 96.2) | 83.3 (77.1 to 88.1) | 5.6 (4.0 to 7.8) | 0.07 (0.05 to 0.12) | 0.95 (0.93 to 0.97) |
| Polyps ≤5 mm19 21 22 30 38 39 | 7 (1942) | 86.3 (78.4 to 91.7) | 84.1 (75.5 to 90.1) | 5.4 (3.6 to 8.2) | 0.16 (0.11 to 0.25) | 0.92 (0.89 to 0.94) |
| High-confidence predictions for polyps ≤5 mm21 22 38–40 | 5 (1350) | 93.4 (87.4 to 96.7) | 84.0 (76.6 to 89.3) | 5.8 (4.0 to 8.6) | 0.08 (0.04 to 0.15) | 0.94 (0.92 to 0.96) |
| Exera | 20 (5148) | 89.4 (85.0 to 92.6) | 81.6 (77.3 to 85.2) | 4.9 (3.9 to 6.0) | 0.13 (0.09 to 0.18) | 0.91 (0.89 to 0.94) |
| Lucera | 8 (1132) | 94.0 (88.7 to 96.9) | 86.0 (81.1 to 89.8) | 6.7 (4.9 to 9.2) | 0.07 (0.04 to 0.13) | 0.95 (0.93 to 0.97) |
| Highest-quality studies17 29 32 38 39 | 5 (826) | 91.5 (86.0 to 94.8) | 87.2 (74.7 to 94.1) | 7.2 (3.4 to 15.0) | 0.10 (0.06 to 0.16) | 0.95 (0.93 to 0.97) |
| High-quality studies17 21 24 26 29 31–33 38 39 41 43 | 12 (2428) | 88.3 (83.6 to 91.8) | 85.3 (80.3 to 89.2) | 6.0 (4.3 to 8.4) | 0.14 (0.09 to 0.20) | 0.93 (0.91 to 0.95) |
HSROC, hierarchical summary receiver-operating characteristic; NBI, narrow band imaging.
The likelihood ratio synthesis gave an overall LR+ of 5.2 (95% CI 4.3 to 6.4) and LR− of 0.11 (95% CI 0.08 to 0.15). Results were similar when limited to published papers, and improved for high-confidence and diminutive polyps.
Surveillance intervals based on NBI diagnosis
Seven studies—three papers20 22 33 and four abstracts38–41—reported surveillance intervals based on endoscopic diagnosis. Overall, surveillance intervals based on endoscopic diagnosis were the same as those based on formal pathology in 92.6% of patients (95% CI 87.9% to 96.3%). There was statistically significant heterogeneity in the agreement rates across studies (p=4×10−8 for Q statistic). If we exclude the studies by Radaelli et al41 and Kuiper et al,33 who reported significantly less agreement at 83.2% and 81.4%, respectively, heterogeneity is not significant (p=0.28 for Q statistic) and the surveillance intervals agree in 95.5% of patients (95% CI 93.9% to 96.9%). Among the six studies that reported whether endoscopically directed intervals were shorter or longer than those directed by pathology,20 22 33 38 39 41 39 patients (3.0%) were prescribed shorter intervals and 35 patients (2.7%) were prescribed longer intervals (figure 5).
Figure 5.
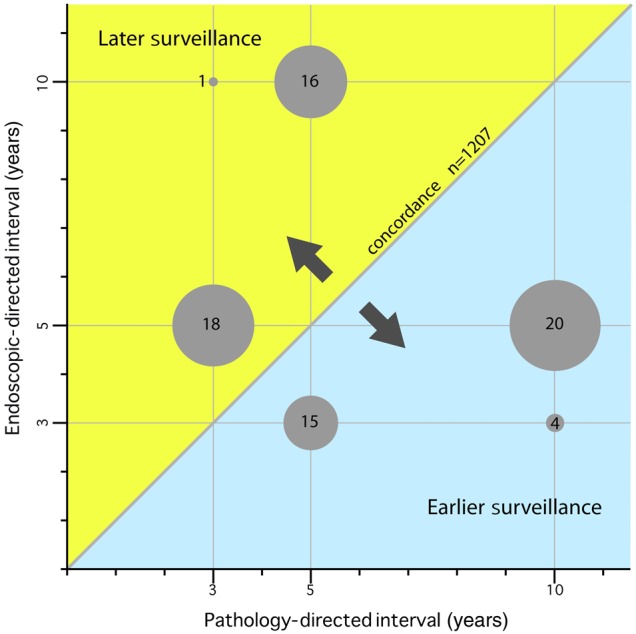
Disagreement between endoscopically directed and pathology directed surveillance intervals. Each dot represents patients whose endoscopic-directed surveillance interval differed from that dictated by the pathological assessment. Discordant intervals in 22 patients in the study by Pohl et al40 are not plotted, as this information was not reported.
Sensitivity analysis
We performed sensitivity analyses with five studies rated of the highest quality (all risk for bias low) and 12 of high quality (all risk for bias low or low except one which was unknown). Diagnostic operating characteristics were similar compared with all results (table 3, figure 6).
Figure 6.
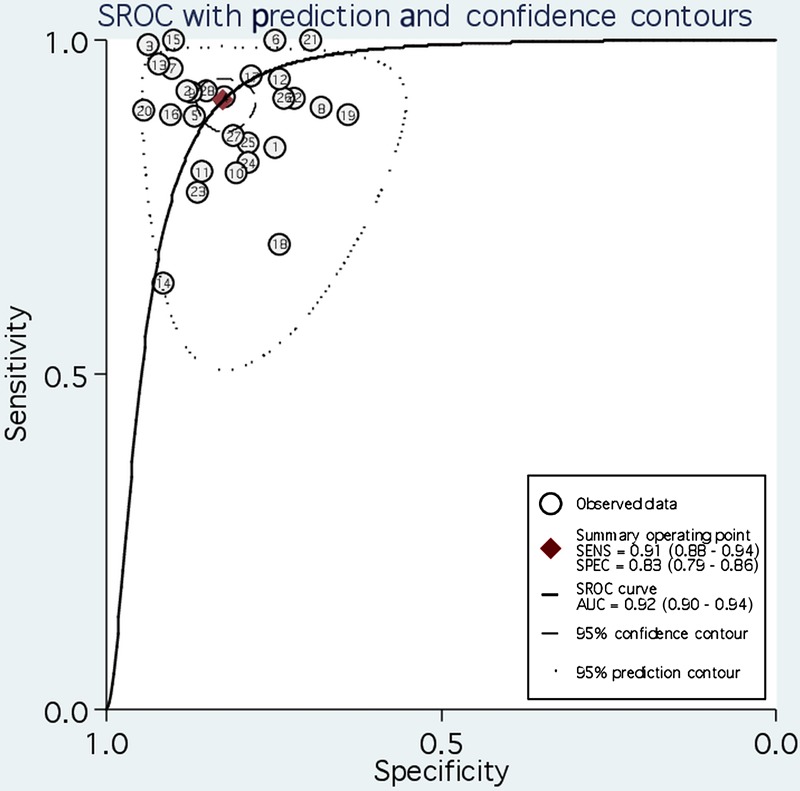
Sensitivities and specificities of individual studies (see study numbers, table 1) plotted with the hierarchical summary receiver-operating characteristic (SROC) curve.
Discussion
The findings of this meta-analysis suggest that real-time endoscopic diagnosis of colorectal polyps performed using NBI has a high diagnostic performance, with an area under the HSROC curve exceeding 0.90. Endoscopic diagnosis correctly characterised 91% of neoplasms and 83% of non-neoplastic polyps, and these numbers improved with high-confidence predictions to 94% and 83%, respectively, though the improvement was not statistically significant.
To our knowledge, this is the first meta-analysis to solely assess diagnosis of colorectal polyps using NBI in real time, which is the closest to simulate actual practice, rather than using still images as well. We included published papers and abstracts, since a substantial portion of this literature is recent and may not yet be fully published. Our use of a two-level statistical approach with the bivariate meta-analysis and HSROC curve analyses following a random effects model allows test stringency and test accuracy to vary across studies.82 This technique allows researchers to avoid misleading conclusions that can occur when estimates of test sensitivity and specificity are simply pooled or averaged. Our analysis is the largest to address the topic; a prior meta-analysis by Wu et al74 included only 11 prospective studies, 6 of which differentiated polyps based on still images. The only real-time diagnosis study75 in a meta-analysis by van den Broek et al77 excluded non-neoplastic polyps from its analysis.
Our study addresses the standards set forth by the American Society of Gastrointestinal Endoscopy (ASGE) for the ‘resect and discard’ strategy. The ASGE has proposed that, for endoscopically diagnosed adenomas ≤5 mm in size to be resected and discarded without pathologic assessment, endoscopic diagnosis should provide a ≥90% agreement in assignment of post-polypectomy surveillance intervals compared with decisions based on pathology.83 The summary agreement was 92.6% in our study, supporting the clinical use of such a strategy.
Our results also relate to the ‘diagnose and leave in’ strategy of leaving endoscopically predicted diminutive non-neoplastic recto-sigmoid polyps in situ without resection. The ASGE recommended that to implement such a policy, endoscopic diagnosis should provide ≥90% NPV when used with high confidence.83 Our calculated NPV for high-confidence NBI diagnosis, derived using the summary sensitivity and specificity, meets this requirement when neoplastic polyps account for less than 60% of all polyps. This is true in prior studies that have reported polyp findings in the entire and recto-sigmoid colon. Lieberman et al3 found that 50% of 3744 diminutive polyps were neoplastic using a large database of colonoscopies performed at academic and private practices. Pickhardt et al16 found that 36.5% of 977 diminutive polyps were neoplastic; Hewett et al15 found that only 20% of 235 rectosigmoid diminutive polyps were neoplastic.
The rationale for real-time histology of colorectal polyps is based on the literature that diminutive polyps rarely harbour advanced histology such as villous features, high-grade dysplasia or cancer,3 and that pathologists are 85–95% accurate in polyp histology characterisation.84 85 Nonetheless, shifting colorectal polyp diagnosis from the traditional gold standard pathology to endoscopy is likely to cause much reservation across the field in regards to accountability, particularly in the strategy of forgoing resection. The importance of high-quality photo documentation of the polyp, in lieu of a pathology slide, must be underscored. The high-resolution polyp image should be permanently stored with the procedure report and accessible in the future as the reference to support the endoscopists’ assessment and clinical decision when subjected to quality review.
The agreement of surveillance intervals is important. In theory, longer surveillance intervals could allow for progression of neoplasia in high-risk individuals before follow-up while inappropriately short surveillance intervals could result in unnecessary colonoscopy, making the strategy less cost effective. In our study, when endoscopy-directed surveillance intervals disagreed with those dictated by pathology, roughly half the recommended longer follow-up and the other half, earlier follow-up. The majority of studies that reported surveillance intervals met the threshold of concordance for high-confidence predictions suggested by the ASGE. There were two exceptions that contributed to between-study heterogeneity. Kuiper and coauthors’ study,33 which uniquely focused on non-academic endoscopists, suggests they may have diminished accuracy compared with experts and require more or continued learning to achieve and sustain high performance. However, it is difficult to draw such a conclusion from a single study. The second study by Radaelli et al41 assesses expert endoscopists and it is unclear from the abstract why they had relatively worse agreement with histology than the other studies.
Recent evidence suggests that serrated polyps with features of larger size, sessile serrated polyp histology, cytologic dysplasia and location in the proximal colon may have a higher risk of colorectal cancer. As such, guidelines for colonoscopy surveillance after screening and polypectomy have recently been updated to stratify serrated lesions.5 The consensus recommended that a sessile serrated polyp larger than 9 mm and a sessile serrated polyp with cytological dysplasia should be managed like a high-risk adenoma; and serrated polyps that are less than 10 mm and do not have cytological dysplasia can be managed like a low-risk adenoma. Current endoscopic classification systems for the differentiation of polyp histology, however, do not address how to distinguish sessile serrated polyps from hyperplastic lesions, mainly due to the high inter-observer variability for their pathological diagnosis, and consequent lack of a reference standard. In the future, serrated polyps will need to be formally studied and integrated into the real-time histology strategy.
Our results reflect the important use of confidence levels. The highest performance of real-time NBI diagnosis of colorectal polyps was achieved when the diagnosis was made with high confidence—the area under the HSROC curve was 0.95 (95% CI 0.93 to 0.97) for polyps of any size, and 0.92 (95% CI 0.92 to 0.96) for diminutive ones. This compares to the overall area under the HSROC curve of 0.92 (95% CI 0.90 to 0.94). The use of objective validated criteria for the endoscopic differentiation of colorectal polyp histology can guide the physician in determining the confidence level. For example, a high-confidence diagnosis can be made if the polyp has one or more features as described in the classification and no features associated with the other polyp histology. If features are not present, then a low-confidence diagnosis can be made, and the polyp submitted for pathological assessment.
We analysed data of over 6000 polyps among 4053 patients who spanned four continents. Nonetheless, the main limitation to our study is that of generalisability. Most studies were performed with expert endoscopists who used variable classification methods to differentiate adenomas from non-neoplastic polyps. The results could be widely generalised if non-experts can readily learn endoscopic diagnosis; only preliminary studies exist, and results are mixed.33 57 86–88 Furthermore, the recent publication of validated international criteria specifically developed for colorectal polyps differentiation using NBI7 holds promise for making endoscopic diagnosis more standardised and less operator dependent. Teaching tools such as videos88 and computer modules86 may be important in the initial and continued training of endoscopists on polyp differentiation.
The exact number of NBI procedures needed to achieve proficiency in optical diagnosis is currently unknown. We identified two studies that address the potential learning curve for real-time endoscopic diagnosis. In Rogart et al's26 series of 265 polyps in 131 patients, three of four endoscopists significantly improved their accuracy in the second half of the study compared with the first from 74% to 87%, respectively. In that study, endoscopists received feedback every 2 weeks about the accuracy of their endoscopic diagnosis. This suggests that with frequent feedback among experienced endoscopists, significant gains in accuracy can be attained in a relatively short amount of time. The other study was a single endoscopist study, which showed higher accuracy for polyps evaluated in the second half of study than the first. The difference however was not statistically significant.24
Another potential limitation is publication bias. We searched for information included in meeting abstracts. We cannot totally exclude that some studies with poor diagnostic performance may have remained unpublished and not even presented in major meetings. However, these studies would have to be large to change substantially the results of the meta-analysis.
In conclusion, we found that endoscopic diagnosis with NBI is an accurate test to differentiate neoplastic from non-neoplastic polyps, with an area under the HSROC curve exceeding 0.90. Its sensitivity for diagnosing adenomatous and other neoplastic polyps is >90%, as is the agreement between endoscopically derived and histologically derived surveillance intervals. Its NPV is high as long as neoplasms account for <60% of polyps. Endoscopic diagnostic performances are highest with high-confidence predictions.
Acknowledgments
The authors would like to thank Christopher Stave, MLS, for his design of the search terms for the systematic review and Aparna Motiwala for her assistance with the database.
Footnotes
Contributors: SM, TK, JPAI and RS contributed to the study's concept and design. SM, TK and JPAI designed the protocol and data collection tools, and SM and TK performed the search and extracted data. EE, SM and TK analysed the data. SM drafted the manuscript, which was revised by all coauthors. All authors accepted the final version of the manuscript. TK is guarantor.
Competing interests: RS and TK: Olympus research support and consultancy; RS: Olympus speaker's fees.
Provenance and peer review: Not commissioned; externally peer reviewed.
Open Access: This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
References
- 1.Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frazier AL, Colditz GA, Fuchs CS, et al. Cost-effectiveness of screening for colorectal cancer in the general population. JAMA 2000;284:1954–61 [DOI] [PubMed] [Google Scholar]
- 3.Lieberman D, Moravec M, Holub J, et al. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology 2008;135:1100–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol 2010;8:865–9, 9 e1–3 [DOI] [PubMed] [Google Scholar]
- 5.Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US multi-society task force on colorectal cancer. Gastroenterology 2012;143:844–57 [DOI] [PubMed] [Google Scholar]
- 6.Rastogi A, Early DS, Gupta N, et al. Randomized, controlled trial of standard-definition white-light, high-definition white-light, and narrow-band imaging colonoscopy for the detection of colon polyps and prediction of polyp histology. Gastrointest Endosc 2011;74:593–602 [DOI] [PubMed] [Google Scholar]
- 7.Hewett DG, Kaltenbach T, Sano Y, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology 2012;143:599–607 e1 [DOI] [PubMed] [Google Scholar]
- 8.Rex DK. Reducing costs of colon polyp management. Lancet Oncol 2009;10:1135–6 [DOI] [PubMed] [Google Scholar]
- 9.Kessler WR, Imperiale TF, Klein RW, et al. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy 2011;43:683–91 [DOI] [PubMed] [Google Scholar]
- 10.Levin TR, Zhao W, Conell C, et al. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med 2006;145:880–6 [DOI] [PubMed] [Google Scholar]
- 11.The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58(6 Suppl):S3–43 [DOI] [PubMed] [Google Scholar]
- 12.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36 [DOI] [PubMed] [Google Scholar]
- 13.Chu H, Cole SR. Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol 2006;59:1331–2; author reply 1332–3 [DOI] [PubMed] [Google Scholar]
- 14.Wang F, Gatsonis CA. Hierarchical models for ROC curve summary measures: design and analysis of multi-reader, multi-modality studies of medical tests. Stat Med 2008;27:243–56 [DOI] [PubMed] [Google Scholar]
- 15.Hewett DG, Huffman ME, Rex DK. Leaving distal colorectal hyperplastic polyps in place can be achieved with high accuracy by using narrow-band imaging: an observational study. Gastrointest Endosc 2012;76:374–80 [DOI] [PubMed] [Google Scholar]
- 16.Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med 2003;349:2191–200 [DOI] [PubMed] [Google Scholar]
- 17.Buchner AM, Shahid MW, Heckman MG, et al. Comparison of probe-based confocal laser endomicroscopy with virtual chromoendoscopy for classification of colon polyps. Gastroenterology 2010;138:834–42 [DOI] [PubMed] [Google Scholar]
- 18.Hirata M, Tanaka S, Oka S, et al. Magnifying endoscopy with narrow band imaging for diagnosis of colorectal tumors. Gastrointest Endosc 2007;65:988–95 [DOI] [PubMed] [Google Scholar]
- 19.Henry ZH, Yeaton P, Shami VM, et al. Meshed capillary vessels found on narrow-band imaging without optical magnification effectively identifies colorectal neoplasia: a North American validation of the Japanese experience. Gastrointest Endosc 2010;72:118–26 [DOI] [PubMed] [Google Scholar]
- 20.Ignjatovic A, East JE, Suzuki N, et al. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): a prospective cohort study. Lancet Oncol 2009;10:1171–8 [DOI] [PubMed] [Google Scholar]
- 21.Lee CK, Lee SH, Hwangbo Y. Narrow-band imaging versus I-Scan for the real-time histological prediction of diminutive colonic polyps: a prospective comparative study by using the simple unified endoscopic classification. Gastrointest Endosc 2011;74:603–9 [DOI] [PubMed] [Google Scholar]
- 22.Rex DK. Narrow-band imaging without optical magnification for histologic analysis of colorectal polyps. Gastroenterology 2009;136:1174–81 [DOI] [PubMed] [Google Scholar]
- 23.Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy 2004;36:1094–8 [DOI] [PubMed] [Google Scholar]
- 24.Rastogi A, Keighley J, Singh V, et al. High accuracy of narrow band imaging without magnification for the real-time characterization of polyp histology and its comparison with high-definition white light colonoscopy: a prospective study. Am J Gastroenterol 2009;104:2422–30 [DOI] [PubMed] [Google Scholar]
- 25.Ren JJX. Narrow-band imaging of meshed capillary vessels for differential diagnosis of colorectal lesions. World Chin J Digestol 2012;20:473–8 [Google Scholar]
- 26.Rogart JN, Jain D, Siddiqui UD, et al. Narrow-band imaging without high magnification to differentiate polyps during real-time colonoscopy: improvement with experience. Gastrointest Endosc 2008;68:1136–45 [DOI] [PubMed] [Google Scholar]
- 27.Rotondano G, Bianco MA, Sansone S, et al. Trimodal endoscopic imaging for the detection and differentiation of colorectal adenomas: a prospective single-centre clinical evaluation. Int J Colorectal Dis 2011:1–6 [DOI] [PubMed] [Google Scholar]
- 28.Sakamoto T, Matsuda T, Aoki T, et al. Time saving with narrow-band imaging for distinguishing between neoplastic and non-neoplastic small colorectal lesions. J Gastroenterol Hepatol 2012;27:351–5 [DOI] [PubMed] [Google Scholar]
- 29.Sano Y, Ikematsu H, Fu KI, et al. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointest Endosc 2009;69:278–83 [DOI] [PubMed] [Google Scholar]
- 30.Shahid MW, Buchner AM, Heckman MG, et al. Diagnostic accuracy of probe-based confocal laser endomicroscopy and narrow band imaging for small colorectal polyps: a feasibility study. Am J Gastroenterol 2012;107:231–9 [DOI] [PubMed] [Google Scholar]
- 31.Singh R, Nordeen N, Mei SL, et al. West meets East: preliminary results of narrow band imaging with optical magnification in the diagnosis of colorectal lesions: a multicenter Australian study using the modified Sano's classification. Dig Endosc 2011;23(Suppl 1):126–30 [DOI] [PubMed] [Google Scholar]
- 32.Zhou QJ, Yang JM, Fei BY, et al. Narrow-band imaging endoscopy with and without magnification in diagnosis of colorectal neoplasia. World J Gastroenterol 2011;17:666–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuiper T, Marsman WA, Jansen JM, et al. Accuracy for optical diagnosis of small colorectal polyps in nonacademic settings. Clin Gastroenterol Hepatol 2012;10:1016–20 [DOI] [PubMed] [Google Scholar]
- 34.Mathew A, Ramirez F, Gilani M. In vivo prediction of polyp histology using high definition/magnification and narrow band imaging [abstract]. Am J Gastroenterol 2008;102(Suppl 2):S264–5 [409] [Google Scholar]
- 35.Ringold D, Sikka S, Sayuk G, et al. High-definition white light and high-contrast narrow band imaging at standard magnification to predict polyp histology: an in-vivo study [abstract]. Gastrointest Endosc 2008;67:AB132–3 [S1423] [Google Scholar]
- 36.Hewett DG, Rex D. Accuracy of predicting distal colorectal histology in real-time using narrow band imaging without optical magnification [abstract]. Gastrointest Endosc 2010;71:AB200 [S1582] [Google Scholar]
- 37.Occhipinti P, Saettone S, Quaglia A, et al. Accuracy of predicting polyps histology using narrow band imaging (NBI) with magnification in routine clinical practice [abstract]. Gastrointest Endosc 2011;73:AB444 [Tu1550] [Google Scholar]
- 38.Kaltenbach T, Hewett D, Rex D, et al. Resect and discard strategy in real-time colonoscopy using the validated Narrow Band Imaging International Colorectal Endoscopic (NICE) Classification provides accurate surveillance interval recommendations [abstract]. Am J Gastroenterol 2011;106(Suppl 2):S167 [428] [Google Scholar]
- 39.Kaltenbach T, Rastogi A, Rouse RV, et al. The VALID colonoscopy study—results of a multicenter prospective randomized controlled trial on real time colorectal polyp diagnosis using narrow band imaging (NBI) [abstract]. Gastrointest Endosc 2012;75(Suppl 4):AB151 [569] [Google Scholar]
- 40.Pohl H, Bensen S, Berk B, et al. Real time diminutive polyp diagnosis accurately determines colonoscopy surveillance interval in clinical practice [abstract]. Gastrointest Endosc 2012;75(Suppl 4):AB151 [570] [Google Scholar]
- 41.Radaelli F, Paggi S, Imperiali G, et al. The impact of a ‘resect and discard’ strategy on surveillance times after colorectal polypectomy: preliminary data of a prospective study [abstract]. Am J Gastroenterol 2011;106(Suppl 2):S542 [1414] [Google Scholar]
- 42.Yague A, Pereda T, Cid-Mañas J, et al. High definition NBI without optical magnification for real-time characterization of small colon polyps: a prospective study compared to white light endoscopy [abstract]. Gastrointest Endosc 2011;73(Suppl 4):AB306 [Su1565] [Google Scholar]
- 43.Coe S, Almansa C, Crook J, et al. Accuracy of in vivo colorectal polyp discrimination using dual focus high definition narrow band imaging colonoscopy: a randomized controlled trial; preliminary results. Gastroentest Endosc 2012;75(4S):AB172 [916] [Google Scholar]
- 44.Chiu HM, Chang CY, Chen CC, et al. A prospective comparative study of narrow-band imaging, chromoendoscopy, and conventional colonoscopy in the diagnosis of colorectal neoplasia. Gut 2007;56:373–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chang CC, Hsieh CR, Lou HY, et al. Comparative study of conventional colonoscopy, magnifying chromoendoscopy, and magnifying narrow-band imaging systems in the differential diagnosis of small colonic polyps between trainee and experienced endoscopist. Int J Colorectal Dis 2009;24:1413–19 [DOI] [PubMed] [Google Scholar]
- 46.Gross S, Trautwein C, Behrens A, et al. Computer-based classification of small colorectal polyps by using narrow-band imaging with optical magnification. Gastrointest Endosc 2011;74:1354–9 [DOI] [PubMed] [Google Scholar]
- 47.Okamoto Y, Watanabe H, Tominaga K, et al. Evaluation of microvessels in colorectal tumors by narrow band imaging magnification: including comparison with magnifying chromoendoscopy. Dig Dis Sci 2011;56:532–8 [DOI] [PubMed] [Google Scholar]
- 48.Rastogi A, Bansal A, Wani S, et al. Narrow-band imaging colonoscopy—a pilot feasibility study for the detection of polyps and correlation of surface patterns with polyp histologic diagnosis. Gastrointest Endosc 2008;67:280–6 [DOI] [PubMed] [Google Scholar]
- 49.Su MY, Hsu CM, Ho YP, et al. Comparative study of conventional colonoscopy, chromoendoscopy, and narrow-band imaging systems in differential diagnosis of neoplastic and nonneoplastic colonic polyps. Am J Gastroenterol 2006;101:2711–16 [DOI] [PubMed] [Google Scholar]
- 50.Takemura Y, Yoshida S, Tanaka S, et al. Computer-aided system for predicting the histology of colorectal tumors by using narrow-band imaging magnifying colonoscopy (with video). Gastrointest Endosc 2012;75:179–85 [DOI] [PubMed] [Google Scholar]
- 51.Tischendorf JJ, Gross S, Winograd R, et al. Computer-aided classification of colorectal polyps based on vascular patterns: a pilot study. Endoscopy 2010;42:203–7 [DOI] [PubMed] [Google Scholar]
- 52.Tischendorf JJW, Schirin-Sokhan R, Streetz K, et al. Value of magnifying endoscopy in classifying colorectal polyps based on vascular pattern. Endoscopy 2010;42:22–7 [DOI] [PubMed] [Google Scholar]
- 53.Tischendorf JJ, Wasmuth HE, Koch A, et al. Value of magnifying chromoendoscopy and narrow band imaging (NBI) in classifying colorectal polyps: a prospective controlled study. Endoscopy 2007;39:1092–6 [DOI] [PubMed] [Google Scholar]
- 54.Wada Y, Kudo Se,, Kashida H, et al. Diagnosis of colorectal lesions with the magnifying narrow-band imaging system. Gastrointest Endosc 2009;70:522–31 [DOI] [PubMed] [Google Scholar]
- 55.Wada Y, Kashida H, Kudo SE, et al. Diagnostic accuracy of pit pattern and vascular pattern analyses in colorectal lesions. Dig Endosc 2010;22:192–9 [DOI] [PubMed] [Google Scholar]
- 56.Wada Y, Kudo SE, Misawa M, et al Vascular pattern classification of colorectal lesions with narrow band imaging magnifying endoscopy. Dig Endosc 2011;23(Suppl. 1):106–11 [DOI] [PubMed] [Google Scholar]
- 57.Higashi R, Uraoka T, Kato J, et al. Diagnostic accuracy of narrow-band imaging and pit pattern analysis significantly improved for less-experienced endoscopists after an expanded training program. Gastrointest Endosc 2010;72:127–35 [DOI] [PubMed] [Google Scholar]
- 58.Iwatate M, Ikumoto T, Sano Y, et al. Diagnosis of neoplastic and non-neoplastic lesions and prediction of submucosal invasion of early cancer during colonoscopy. Rev Colomb Gastroenterol 2011;26:43–57 [Google Scholar]
- 59.Coe SG, Wallace MB. Management of small and diminutive colorectal polyps: a review of the literature. Minerva Gastroenterol Dietol 2011;57:167–76 [PubMed] [Google Scholar]
- 60.DaCosta RS, Wilson BC, Marcon NE. Optical techniques for the endoscopic detection of dysplastic colonic lesions. Curr Opin Gastroenterol 2005;21:70–9 [PubMed] [Google Scholar]
- 61.Chiu HM, Wang HP, Wu MS, et al. The clinical efficacy and future perspective of narrow band imaging for the diagnosis of colorectal neoplasm. Dig Endosc 2011;23(Suppl 1):116–19 [DOI] [PubMed] [Google Scholar]
- 62.Bernstein M. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Dis Colon Rectum 2009;52:1355–6 [DOI] [PubMed] [Google Scholar]
- 63.East JE, Suzuki N, Bassett P, et al. Narrow band imaging with magnification for the characterization of small and diminutive colonic polyps: pit pattern and vascular pattern intensity. Endoscopy 2008;40:811–17 [DOI] [PubMed] [Google Scholar]
- 64.van den Broek FJC, Fockens P, Van Eeden S, et al. Clinical evaluation of endoscopic trimodal imaging for the detection and differentiation of colonic polyps. Clin Gastroenterol Hepatol 2009;7:288–95 [DOI] [PubMed] [Google Scholar]
- 65.Kuiper T, van den Broek FJ, Naber AH, et al. Endoscopic trimodal imaging detects colonic neoplasia as well as standard video endoscopy. Gastroenterology 2011;140:1887–94 [DOI] [PubMed] [Google Scholar]
- 66.Kuiper T, van den Broek FJ, van Eeden S, et al. Feasibility and accuracy of confocal endomicroscopy in comparison with narrow-band imaging and chromoendoscopy for the differentiation of colorectal lesions. Am J Gastroenterol 2012;107:543–50 [DOI] [PubMed] [Google Scholar]
- 67.Fichera A. A prospective comparative study of narrow band imaging, chromoendoscopy, and conventional colonoscopy in the diagnosis of colorectal neoplasia: commentary. Dis Colon Rectum 2008;51:618 [Google Scholar]
- 68.Gupta N, Bansal A, Rao D, et al. Accuracy of in vivo optical diagnosis of colon polyp histology by narrow-band imaging in predicting colonoscopy surveillance intervals. Gastrointest Endosc 2012;75:494–502 [DOI] [PubMed] [Google Scholar]
- 69.Hirata M, Tanaka S, Oka S, et al. Evaluation of microvessels in colorectal tumors by narrow band imaging magnification. Gastrointest Endosc 2007;66:945–52 [DOI] [PubMed] [Google Scholar]
- 70.Kanao H, Tanaka S, Oka S, et al. Narrow-band imaging magnification predicts the histology and invasion depth of colorectal tumors. Gastrointest Endosc 2009; 69(3 Pt 2):631–6 [DOI] [PubMed] [Google Scholar]
- 71.Chen CH, Wu KL, Hu ML, et al. Is a biopsy necessary for colon polyps suitable for polypectomy when performing a colonoscopy? Chang Gung Med J 2011;34:506–11 [PubMed] [Google Scholar]
- 72.Gross S, Stehle T, Behrens A, et al., eds. A comparison of blood vessel features and local binary patterns for colorectal polyp classification. Proc SPIE 7260, Medical Imaging: Computer-Aided Diagnosis, 2009 [Google Scholar]
- 73.Kobayashi Y, Hayashino Y, Jackson JL, et al. Diagnostic performance of chromoendoscopy and narrow band imaging for colonic neoplasms: a meta-analysis. Colorectal Dis 2012;14:18–28 [DOI] [PubMed] [Google Scholar]
- 74.Wu L, Li Y, Li Z, et al. The diagnostic accuracy of narrow-band imaging for the differentiation of neoplastic from non-neoplastic colorectal polyps: a meta-analysis. Colorectal Dis. 2013;15:3–12 [DOI] [PubMed] [Google Scholar]
- 75.Katagiri A, Fu KI, Sano Y, et al. Narrow band imaging with magnifying colonoscopy as diagnostic tool for predicting histology of early colorectal neoplasia. Aliment Pharmacol Ther 2008;27:1269–74 [DOI] [PubMed] [Google Scholar]
- 76.Tanaka S, Oka S, Hirata M, et al. Pit pattern diagnosis for colorectal neoplasia using narrow band imaging magnification. Dig Endosc 2006;18(Suppl 1):S52–S6 [Google Scholar]
- 77.van den Broek FJ, Reitsma JB, Curvers WL, et al. Systematic review of narrow-band imaging for the detection and differentiation of neoplastic and nonneoplastic lesions in the colon (with videos). Gastrointest Endosc 2009;69:124–35 [DOI] [PubMed] [Google Scholar]
- 78.Dekker D, Kara M, Cohen C, et al. Detection and classification of adenomas using high resolution endoscopy, video autofluorescence imaging and narrow band imaging incorporated in one colonoscope [abstract]. Gastroenterology 2006;130(4, Suppl 2):A310 [M1137] [Google Scholar]
- 79.Shin S, Song J, Lee K, et al. The effectiveness of narrow band imaging magnification for differential diagnosis of colorectal tumor [abstract]. Gastrointest Endosc 2010;71(Suppl 5):AB317 [T1591] [Google Scholar]
- 80.Fuchs CS, Scholz T, Heil U, et al. Chromoendoscopy with pit pattern classification allows to characterize flat neoplastic changes better than narrow band imaging (NBI) with vascular pattern [abstract]. Gastrointest Endosc 2011;73(Suppl 4):AB381 [Mo1543] [Google Scholar]
- 81.Krishnan S, Cheney C, Anastopoulos T, et al. Prospective validation of modified narrow band imaging criteria for predicting polyp histology in routine clinical practice [abstract]. Gastrointest Endosc 2012;75(Suppl 4):AB151–2 [571] [Google Scholar]
- 82.Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 2001;20:2865–4 [DOI] [PubMed] [Google Scholar]
- 83.Rex DK, Kahi C, O'Brien M, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc 2011;73:419–22 [DOI] [PubMed] [Google Scholar]
- 84.Cross SS, Betmouni S, Burton JL, et al. What levels of agreement can be expected between histopathologists assigning cases to discrete nominal categories? A study of the diagnosis of hyperplastic and adenomatous colorectal polyps. Mod Pathol 2000;13:941–4 [DOI] [PubMed] [Google Scholar]
- 85.Wu ML, Dry SM, Lassman CR. Deeper examination of negative colorectal biopsies. Am J Clin Pathol 2002;117:424–8 [DOI] [PubMed] [Google Scholar]
- 86.Ignjatovic A, Thomas-Gibson S, East JE, et al. Development and validation of a training module on the use of narrow-band imaging in differentiation of small adenomas from hyperplastic colorectal polyps. Gastrointest Endosc 2011;73:128–33 [DOI] [PubMed] [Google Scholar]
- 87.Ladabaum U, Fioritto A, Paik J, et al. A standardized learning module improves the accuracy of ex-vivo endoscopic diagnosis of polyp histology with narrow band imaging by community-based endoscopists [abstract]. Gastrointest Endosc 2012;75(Suppl 4):AB 152 [572] [Google Scholar]
- 88.Rastogi A, Rao D, Gupta N, et al. Impact of a computer based teaching module on characterization of diminutive colon polyps using narrow band imaging (NBI) by non-experts in academics and community practice: a video based study [abstract ] Gastrointest Endosc 2012;75(Suppl 4):AB152–3 [DOI] [PubMed] [Google Scholar]