Abstract
Background: Toxoplasmosis is a common parasitic infection in human around the world and can cause life-threatening encephalitis in human immunodeficiency virus (HIV) infected host. The aim of this study was to assess the frequency of toxoplasma infection in illicit drug users (IDUs) with and without HIV infection in Iran.
Methods: This study was carried out on 84 IDUs (42 HIV positive as case group and 42 HIV negative subjects as control group) from 2008 to 2009. Serum samples were tested for T. gondii IgG antibodies by Enzym linked immunosorbant assay (ELISA). Based on the company brochure kit, the test was defined positive if the antibody titer was 3 IU/ml or more. The data from these two groups were collected and analyzed.
Results: The mean age of HIV positive cases was 34.4±8.6 and for HIV negative cases was 35.9±9.3 year. The mean age and distribution of sex in both groups were equal. The frequency of toxoplasma-IgG in HIV positive and HIV negative was 73.8% and 81%, respectively (p=0.19).
Conclusion: The results show that prevalence of toxoplasmosis infection in the illicit drug users with HIV positive or negative is equal.
Key Words: HIV, Toxoplasma antibody, Illicit drug user.
Toxoplasmosis caused by T.gondii, a protozoan parasite is a common parasitic infection in human worldwide (1). The seroprovalence rate of toxoplasmosis ranges in the countries with different socioeconomics and climate condition, from 30% to 75% (2-4). The highest seroprevalence rates up to 55.7% have been reported in Iran (5, 6). While the infection in immunocompetent individuals is mostly subclinical, T.gondii can cause life threatening diseases such as severe central nervous system (CNS) infection in immunocompromised patients especially the human immunodeficiency virus (HIV) infected host (1, 7).
It is estimated that at least 20% of all HIV infected patients with latent toxoplasmosis develop toxoplasmic encephalitis (1). In Iran, as well as in the other parts of the world, T.gondii infection in the HIV infected patients remains the most challenging problem in managing this population (8-10).
In order to plan a proper approach for the prevention of CNS infection, it is necessary to know the toxoplasma antibody among the HIV infected people. In Iran, HIV infection mostly occurs in illicit drug users who share injection equipment (11). To the best of our knowledge, there are limited studies on toxoplasmosis seroprevalence among the HIV infected and non-HIV infected illicit drug users in the country (8-10). We undertook a prospective case control seroprevalence study on toxoplasmosis in HIV positive and HIV negative IDUs to assess T.gondii infection in this high risk population in Ahvaz, Southwest Iran.
Materials
This case control study was conducted on 84 subjects including 42 HIV infected as case group and 42 HIV negative subjects as control group. The samples were obtained from illicit drug users referred to the drug addict treatment centers in Ahvaz from 2008 to 2009. The cases were randomly selected from documented HIV positive subjects registered in Khuzestan Health Center (KHC) affiliated to Ahvaz Joundishapur University of Medical Sciences (AJUMS) based on 2 positive ELISA and a positive confirmatory Western blot test for HIV. Controls also were randomly selected from illicit drug users with negative results for HIV tests registered in KHC.
A total of 82 serum samples were tested at the Pasteur Laboratory in Ahvaz. Blood samples were collected and sera separated and frozen at -20˚C until use. T. gondii immunoglobulin G (IgG) antibodies were detected by ELISA method using commercial kit (Roche, Germany) with 99.5% sensitivity and 98.5% specificity. In accordance with the manufacturer’s instructions, T. gondii IgG was defined as positive if the antibody titer was 3 IU/ml or more. The toxoplasma and HIV infection related data of the studied cases were collected by using an epidemiological sheet for variables such as age, sex, and toxoplasma/HIV infection. The study was approved by the Infectious and Tropical Diseases Research Cente of Joundishapur University of Medical Sciences, Ahvaz, Iran.
The Ethics Committee of the Research Deputy also approved this study. Finally, the data were analyzed in SPSS Version 16 system.
The frequency of toxoplasma antibodies in intravenous drug users (IDUs) with and without HIV infection was determined and compared.
Results
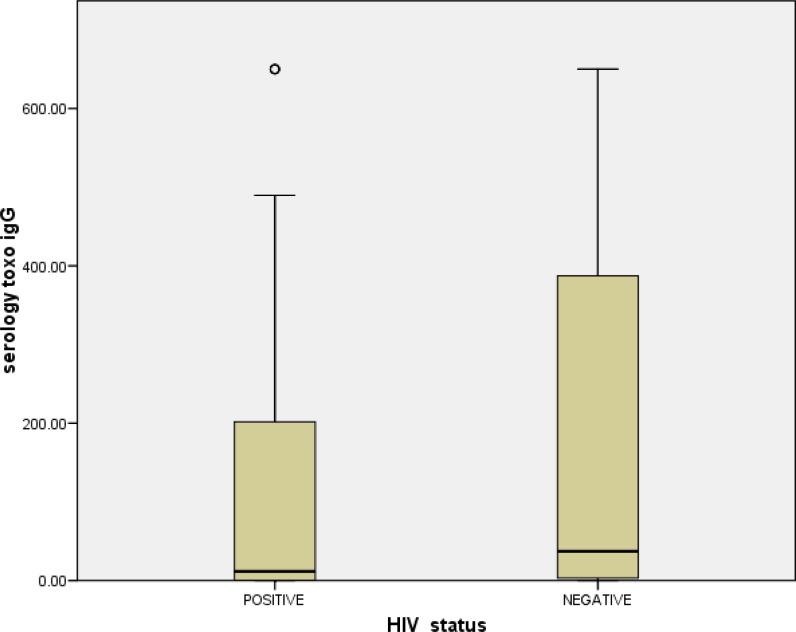
The mean age of HIV positive cases was 34.4±8.6 (ranged18-54 years) and for HIV negative cases was 35.9±9.3 years (ranged 19-59 years) (p>0.05). From 3 females in this study, 2 were HIV negative and 1 was HIV positive. The prevalence of Toxoplasma-IgG positive antibodies in HIV positive and HIV negative was 73.8% and 81%, respectively (table 1) (p=0.19). The mean antibodies titer of IgG in HIV positive and HIV negative was 138.81±26.27 and 185.84±31.13, respectively (figure 1). There was no significant difference in the serum levels of antibody titers between the HIV positive and HIV negative cases (p=0.35).
Table 1.
Comparison of Toxoplasma-IgG positivity between HIV positive and HIV negative cases
| HIVstatus |
Toxoplasma-IgG
|
P value | |
|---|---|---|---|
|
Positive
N (%) |
Negative
N (%) |
||
| Positive (n=42) | 31 (73.8) | 11 (26.2) | 0.19 |
| Negative (n=42) | 34 (80.9) | 8 (19.1) | |
Figure 1.
Mean±SD antibodies titer of IgG in HIV positive and HIV negative studied cases
Discussion
The present study showed that the seroprevalence rate of toxoplasma infection in HIV infected individuals was 73.8% which was higher than the rate previously reported except for one report from Ethiopia (12-16). A cross-sectional study in Malaysia showed that the seroprevalence rate of toxoplasmosis in HIV infected was found to be 21% (12). Kodym et al. reported this rate of 42% in HIV infected cases in Czech Republic and Natio et al. reported this rate to 5.4% in Japan and Sipore et al reported to 28.5% in Burkina Faso (13-15).
Davarpanah et al. reported that the seroprevalence rate of toxoplasmosis in HIV infected in Shiraz was 18.2%, Mohraz et al. reported this rate as 49.7% in Tehran and Shafiei et al. reported this rate as 38% in Mashhad (8-10). In our study, illicit drug users regardless to HIV infection had higher latent toxoplasma infection than the rates reported in other studies (8-10, 13-15). Our results are even higher than the results of Mohraz et al. with similar population in Iran (73.8% vs. 49.7%) (9).
The reason for these differences is not clear, but we believe that geographical variation, socioeconomic and lifestyle of the studied cases may effect on the prevalence of toxoplasmosis (1, 8). Although, toxoplasma infection mostly occurs via contaminated food, the illicit drug users because of their low health status, poverty, low nutritional status and perhaps other route of transmission are at higher risk of infection. According to official reports and published studies, the great majority of Iranian HIV infected individuals are illicit drug users with low socioeconomic and poor nutritional status (11, 17, 18).
The results of our study and the findings of other researchers revealed that HIV infection does not put the patients at a higher risk of toxoplasmosis. We believe that in the area such as the region of study, the patients acquired infection in their childhood and before HIV infection. The result of our study showed that the mean age in seropositive cases was similar to seronegative cases like the results of other researchers in Iran and other countries (8, 9, 13, 14). According to the results of this study, previous studies conducted in different areas of Iran and based on general health condition, toxoplasmosis should be considered as one of the most prevalent parasitic infectious diseases in Iranian HIV infected people as well as general population (19, 20).
There are several limitations to our study that should be considered in relation to the findings. First toxoplasma –IgG was tested for registered illicit drug users with previously known status of HIV infection rather than through a standardized serological survey. Second, the participants were limited to those referred to drug treatment centers and could not be real representative of general population .Third, nearly more than 95% infected studied cases were males and the statistical calculation related to gender may be considered with caution. In summary, the results of our study show that the prevalence of toxoplasmosis infection in the illicit drug users with HIV positive or negative is equal.
Acknowledgments
This study is a part of an assistant's thesis for medical specialty in infectious diseases field (No: u-88132), so the authors wish to thank Joundishapur Infectious and Tropical Diseases Research Center for supporting this study. We also thank Mr. Taei and Dr. Tarrahomi, the Chief of the HIV/AIDS Department of KHC for their kind assistance.
Funding: This study was funded by Joundishapur Infectious and Tropical Diseases Research Center, AJUMS.
Conflict of interest: None declared.
Ethical approval: Approved by the Ethics Committee of AJUMS Research Council.
References
- 1.Montoya JG, Kovacs JA, Remington JS. Toxoplasma gondii. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. Philadelphia: Churchill Livingstone ; 2012. pp. 3495–510. [Google Scholar]
- 2.McCabe RE, Remington JS. Toxoplasmosis: The time has now come. N Engl J Med. 1988;318:313–5. doi: 10.1056/NEJM198802043180509. [DOI] [PubMed] [Google Scholar]
- 3.Jones JL, Kruszon-Moran D, Wilson M, et al. Toxoplasma gondii infection in the United States: seroprevalence and risk factors. Am J Epidemiol. 2001;154:357–65. doi: 10.1093/aje/154.4.357. [DOI] [PubMed] [Google Scholar]
- 4.Jeannel D, Niel G, Costagliola D, et al. Epidemiology of toxoplasmosis among pregnant women in the Paris area. Int J Epidemiol. 1988;17:595–602. doi: 10.1093/ije/17.3.595. [DOI] [PubMed] [Google Scholar]
- 5.Ghorbani M, Edrisian GH, Asad N. Serological survey of toxoplasmosis in the northern part of Iran, using indirect fluorescent antibody technique. Trans R Soc Trop Med Hyg. 1978;72:369–71. doi: 10.1016/0035-9203(78)90129-3. [DOI] [PubMed] [Google Scholar]
- 6.Fallah M, Rabiee S, Matini M, Taherkhani H. Seroepidemiology of toxoplasmosis in primigravida women in Hamadan, Islamic Republic of Iran, 2004. East Mediterr Health J. 2008;14:163–71. [PubMed] [Google Scholar]
- 7.Luft BJ, Remington JS. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15:211–22. doi: 10.1093/clinids/15.2.211. [DOI] [PubMed] [Google Scholar]
- 8.Davarpanah MA, Mehrabani D, Neirami R, Ghahremanpoori M, Darvishi M. Toxoplasmosis in HIV/AIDS patients in Shiraz, southern Iran. Iran Red Crescent Med J. 2007;9:22–7. [Google Scholar]
- 9.Mohraz M, Mehrkhani F, Jam S, et al. Seroprevalence of Toxoplasmosis in HIV/AIDS patients in Iran. Acta Med Iran. 2011;49:213–8. [PubMed] [Google Scholar]
- 10.Shafie R, Riazi Z, Sarvghad MR, et al. Prevalence of IgG and IgM Anti-Toxoplasma gondii Antibodies in HIV Positive Patients in Northeast of Iran. Iran J Pathol. 2011;6:68–72. [Google Scholar]
- 11.Razzaghi EM, Movaghar AR, Green TC, Khoshnood K. Profile of risk: A qualitative study of injecting drug users in Tehran, Iran. Harm Reduct J. 2006;3:12. doi: 10.1186/1477-7517-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nissapatorn V, Kamarulzaman A, Init I, Tan LH, Rohela M, Norliza A, et al. Seroepidemiology of toxoplasmosis among HIV-infected patients and healthy blood donors. Med J Malaysia. 2002;57:304–10. [PubMed] [Google Scholar]
- 13.Kodym P, Hrda S, Machala L, et al. Prevalence and Incidence of Toxoplasma Infection in HIV-Positive Patients in the Czech Republic. J Eukaryote Microbiol. 2006;53:S160–1. doi: 10.1111/j.1550-7408.2006.00215.x. [DOI] [PubMed] [Google Scholar]
- 14.Natio T, Inui A, Kudo N, et al. Seroprevalence of IgG Anti-Toxoplasma Antibodies in Asymptomatic patients Infected with HIV in Japan. Intern Med. 2007;46:1149–50. doi: 10.2169/internalmedicine.46.6402. [DOI] [PubMed] [Google Scholar]
- 15.Simpore J, Savadogo A, Ilboudo D, et al. Toxoplasma gondii, HCV and HBV Seroprevalenceand Co-Infection Among HIV-Positive and –Negative Pregnant Women in Burkina Faso. J Med Virol. 2006;78:730–3. doi: 10.1002/jmv.20615. [DOI] [PubMed] [Google Scholar]
- 16.Shimelis T, Tebeje M, Tadesse E, Tegbaru B, Terefe A. Sero-prevalence of latent Toxoplasma gondii infection among HIV-infected and HIV-uninfected people in Addis Ababa, Ethiopia: A comparative cross-sectional study. BMC Research Notes. 2009;2 doi: 10.1186/1756-0500-2-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prevention Department of Welfare Organization. A summary report of drug related infectious disease in Iran. 2000. [Google Scholar]
- 18.Vazirian M, Nassirimanesh B, Zamani S, et al. Needle and syringe sharing practices of injecting drug users participating in an outreach HIV prevention program in Tehran, Iran: A cross-sectional study. Harm Reduct J. 2005;2:19. doi: 10.1186/1477-7517-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noorbakhsh S, Mamishi S, Rimaz S, Monavari SRH. Toxoplasmosis in primiparus pregnant women and their neonates. Iran J Pub Health. 2002;31:51–4. [Google Scholar]
- 20.Hattam G, Shamseddin A, Nikouee F. Seroprevalence of toxoplasmosis in high school girls in Fasa district, Iran. Iranian J Immunol. 2005;2:177–181. [Google Scholar]