Abstract
We examined the effects of RT on oral glucose tolerance test (OGTT)-derived indices of muscle insulin sensitivity, hepatic insulin resistance, β-cell function, and skeletal muscle proteins related to glucose transport in overweight/obese, sedentary young men. Twenty-eight participants [median body mass index (BMI) 30.9 kg/m2; age 22 yr] completed 12 wk of RT (3 sessions/wk) and were assessed for changes in OGTT-derived indices, resting metabolic rate, body composition, serum adipokines, and skeletal muscle protein content [hexokinase 2 (HK2), glucose transporter type 4 (GLUT4), RAC-β serine/threonine-protein kinase (AKT2), glycogen synthase kinase 3β, and insulin receptor substrate 1]. Individualized responses to RT were also evaluated. RT significantly improved insulin and glucose area under the curve (both P < 0.03). With the use of OGTT indices of insulin action, we noted improved muscle insulin sensitivity index (mISI; P = 0.03) and oral disposition index (P = 0.03). BMI, lean body mass (LBM), and relative strength also increased (all P < 0.03), as did skeletal muscle protein content of HK2, GLUT4, and AKT2 (26–33%; all P < 0.02). Hepatic insulin resistance index, adiponectin, leptin, and total amylin did not change. Further analysis demonstrated the presence of highly individualized responsiveness to RT for glucose tolerance and other outcomes. RT improved oral indices of muscle insulin sensitivity and β-cell function but not hepatic insulin resistance in overweight/obese young men. In addition to the increase in LBM, the improvements in insulin action may be due, in part, to increases in key insulin signaling proteins.
Keywords: insulin sensitivity, strength training, exercise, OGTT, glucose tolerance
in recent decades, type 2 diabetes has progressed into a major cause of preventable death, increasing from ∼1.5 million diagnosed in 1958 to ∼21 million in 2010 (11), with an estimated additional 7 million undiagnosed (4). Thus prevention of future type 2 diabetes and its primary clinical manifestation—cardiovascular disease—in young adults is a major public-health challenge. It is well established that aerobic exercise prevents type 2 diabetes (5, 41). Resistance training (RT) may be an additional viable, preventive strategy for type 2 diabetes (22, 36a), especially in obese subjects precluded from performing aerobic activities, as it improves whole-body insulin sensitivity and glucose tolerance [as reviewed by Roberts et al. (42)].
Generally, the euglycemic-hyperinsulinemic clamp (EHC) and frequently sampled intravenous glucose tolerance (FSIGT) test are the gold standard methods for estimation of insulin sensitivity and β-cell function. However, these methods are expensive, not simple to perform, and generally not practical in standard clinical practice. The oral glucose tolerance test (OGTT) is less expensive, and its simplicity allows for more widespread use. Recently, Abdul-Ghani et al. (1) validated OGTT-derived indices of muscle insulin sensitivity index (mISI) and hepatic insulin resistance index (IRI) with EHC data and oral disposition index (DI) (3, 40), an estimate of β-cell function. Estimates of the contribution of skeletal muscle and liver insulin sensitivity changes in response to RT are unknown. Furthermore, little is known about the underlying molecular mechanisms by which RT improves insulin sensitivity in skeletal muscle (42). Holten et al. (25) noted RT-induced increases in glucose transporter type 4 (GLUT4) protein content in subjects with type 2 diabetes and in insulin receptor, PKB-α/β, and glycogen synthase (GS) protein content in both controls and subjects with type 2 diabetes.
The present study was designed to investigate the effects of a high-intensity RT intervention (12 wk; 3 sessions/wk) in sedentary, overweight/obese young men on OGTT indices of mISI, hepatic IRI, and oral DI and changes in protein expression of proteins linked to improved glucose transport in skeletal muscle. Our primary hypothesis was that RT, due to its primary effects on skeletal muscle, would improve glucose tolerance through improvements in mISI rather than hepatic IRI, independent of weight loss.
METHODS
Study Participants
Thirty-six young-adult (ages 18–35), overweight/obese [body mass index (BMI) ≥ 27 kg/m2] men were enrolled in the RT group, of which 28 completed the study (26 with blood samples). Of the eight who dropped out of the study, six reported personal/time commitments, and two failed to attend their post-test visits after completing the intervention. At baseline, participants were sedentary (participated in light-intensity physical activities ≥2 times/wk) and did not exhibit any overt chronic disease symptoms, as indicated by a comprehensive screening history and physical examination. Potential participants who had: 1) documented cardiovascular disease, cardiac surgery, or any heart arrhythmia found on an ECG reading; 2) participated in a structured exercise, nutrition, or weight-loss program within the previous 6 mo; or 3) used tobacco products or medications that influence cardiovascular function, body composition, or insulin indices in the prior 6 mo were excluded from the study. Participants were instructed to maintain their normal ad libitum diet and normal activities of daily living. Pre- and postintervention assessments were made at wk 0 and 13, respectively. All of the study protocols were approved by the University of California, Los Angeles (UCLA), Institutional Review Board and were performed according to the Declaration of Helsinki.
RT Intervention and Muscular-Strength Testing
All training occurred at the John Wooden Recreation Center (UCLA). Participants in the RT group completed 12 wk of RT at three supervised sessions/wk, with each session lasting ∼1 h. The training overload was modified using a linear periodization model with three phases. During phase 1 (wk 1–2), participants completed two sets of 12–15 repetitions for each exercise at 100% of their approximated 12–15 repetition maximum (RM; i.e., participants were motivated to reach volitional fatigue/failure within 15 repetitions). In phase 2 (wk 3–7) participants completed three sets of eight–12 repetitions at 100% of their eight–12 RM, and in phase 3 (wk 8–12), participants completed six to eight repetitions at 100% of their six to eight RM. As participants adapted to the training overload, the weight was increased to maintain the prescribed training intensity. All participants trained on 3 nonconsecutive days/wk, cycling between two workout regimens. Workout I consisted of dumbbell (DB) squat, cable row, DB front lunge, DB row, barbell (BB) deadlift, DB triceps extension, and DB curl. Workout II included DB step-up, BB chest press, machine squat, DB overhead press, DB incline chest press, DB side raise, DB reverse fly, and abdominal crunches. A certified personal trainer led all training sessions with a maximum three-to-one participant-to-trainer ratio.
Maximal strength testing consisted of one RM (1-RM) lift for the BB bench press, 45° incline leg press, and machine-seated row. Participants first warmed up each muscle group by performing eight to 10 repetitions with weight equivalent to 40–60% of their estimated 1-RM. The weight was increased progressively while decreasing the repetitions until participants could safely attempt an estimated 1-RM for each exercise. A successful 1-RM occurred on the penultimate set, having failed their last set. Participants were allowed 3–4 min of rest between all sets. All participants performed two maximal strength tests, one immediately preceding the first training session and the second immediately preceding their penultimate training session. Relative strength measures were calculated by dividing each measure (in kg) by participant body weight (in kg).
Outpatient Visit Procedures
Measurements were taken from participants at baseline (pre-test) and on wk 13 (post-test), with each test period consisting of two outpatient visits. The first visit took place on a weekday at the UCLA Clinical and Translational Research Center (CTRC), followed by a same-week Saturday visit at the Gonda (Goldschmied) Diabetes Center (UCLA). To control for any acute effects of the training program caused by RT, the CTRC outpatient visit occurred ∼72 h after the last training session, and the subsequent Saturday visit was 96–120 h following the last training session. Before each visit, participants were reminded to: 1) avoid all moderate-to-vigorous physical activity 24 h before testing and 2) abstain from all food and drink (except water) for ∼12 h before each visit. Verbal confirmation of adherence to the aforementioned criteria was obtained immediately before all testing.
Outpatient visit, day 1.
The outpatient procedures began at 7:30 AM and typically lasted 3.5 h. A 12-lead ECG was administered as a safety measure and checked by a physician before allowing any participation in exercise testing/intervention. Height, weight, and waist circumference were measured in duplicate in all participants. Fasting blood samples were collected, and serum was separated and stored at −80°C until assayed. Subsequently, a 2-h OGTT was performed.
Outpatient visit, day 2.
Body composition was determined by a dual-energy X-ray absorptiometry scan (QDR 4500 fan beam X-ray densitometer; Hologic, Bedford, MA). Glycated hemoglobin A1c (HbA1c) was measured via a DCA Vantage analyzer (Siemens Medical Solutions USA, New York, NY), and a physical activity questionnaire [International Physical Activity Questionnaire (IPAQ)] was administered. Muscle biopsies from the left vastus lateralis muscle were performed.
Physical activity questionnaire.
Participants completed an IPAQ (self-administered, long form) to quantify the amount of routine physical activity performed in the week before each assessment. During the post-test visit, participants were instructed to exclude their intervention-specific physical activity when completing the questionnaire. In this validated questionnaire (19), participants self-reported the frequency (days/wk) and duration (h and min/day) of physical activity. Activity-specific (moderate, vigorous, or total activity) scores were calculated as continuous variables of metabolic equivalent task (MET) · min/wk.
Resting Energy Expenditure
Resting energy expenditure (REE; kcal/day) was measured by means of the Vmax Encore Metabolic Cart (CareFusion, Yorba Linda, CA) using the ventilated hood technique. After reaching steady state (approximately 10–15 min), oxygen consumption (l/min) and carbon dioxide production (l/min)—standardized for temperature, barometric pressure, and humidity—were measured at 1-min intervals for ∼5 min. REE was derived from the measured oxygen uptake and carbon dioxide output. Before each test, the calorimeter was calibrated with a reference gas mixture of 95% oxygen and 5% carbon dioxide.
Blood Chemistry Assays
Adiponectin was determined by ELISA (R&D Systems, Minneapolis, MN). Total amylin and leptin were determined using the Multiplex assay (EMD Millipore, Billerica, MA).
Glucose Tolerance
The participants completed a 2-h glucose tolerance (OGTT) using 75 g anhydrous glucose dissolved in water. Venous blood samples were obtained at baseline and every 30 min (−30, 0, 30, 60, 90, and 120, relative to glucose ingestion) and were assayed for glucose and insulin. Serum glucose was analyzed using the in vitro hexokinase method (Olympus AU400 Chemistry-Immuno Analyzer; Olympus America, Center Valley, PA). Serum insulin was measured by means of solid-phase, enzyme-labeled chemiluminescent immunometric assay (Immulite 2000; Diagnostic Products, Los Angeles, CA).
OGTT Calculations
Total and incremental areas under the glucose and insulin curves (tAUC and iAUC, respectively) were calculated by trapezoidal rule, with tAUC defined as the AUC subtracted from zero and iAUC as the AUC subtracted from the fasting glucose value. tAUC, from 0 to 120 min, was calculated for glucose [GtAUC(0–120)] and insulin [ItAUC(0–120)]. ISI was estimated by the Matsuda index, which strongly correlates with the rate of whole-body glucose disposal during the EHC (33).
Glucose production in postabsorptive states is determined predominately by hepatic glucose production (largely mediated by glucagon) and fasting insulin levels. Additionally, the acute rise in plasma glucose following a glucose load stimulates pancreatic β-cells to secrete insulin. This early period of hyperglycemia and hyperinsulinemia eventually suppresses hepatic glucose production, which reaches a nadir within 45 min, following ingestion of a glucose load in healthy individuals (18). In hepatic insulin-resistant individuals, suppression of endogenous glucose production is often impaired, resulting in higher plasma glucose during early stages of the OGTT (32). Therefore, the product of the glucose and insulin tAUCs during the first 30 min of the OGTT was used as an index of hepatic insulin resistance [hepatic IRI = GtAUC(0–30) × ItAUC(0–30)] (1). Hepatic IRI was subsequently divided by 1,000 for data presentation. This OGTT-derived index of hepatic IRI correlates strongly with the EHC estimate of hepatic IRI in subjects with both normal and impaired glucose tolerance (1).
The early insulin response [insulinogenic index (IGI)] was calculated as the ratio of the change in insulin to the change in glucose from 0 to 30 min [IiAUC(0–30)/GiAUC(0–30)] (3). β-Cell function was estimated by the oral DI (insulin secretion × insulin sensitivity) and was calculated as the product of OGTT-derived IGI and the Matsuda index (3). Measurements of oral DI have been validated against the FSIGT test (39).
During a glucose load, the concomitant rise in plasma glucose and insulin stimulates glucose disposal into skeletal muscle and other tissues, including brain and splanchnic areas (30). Because endogenous glucose production remains significantly unchanged during time 60–120 min of the OGTT (18), the decline from peak glucose to nadir during the OGTT is likely due to two factors: skeletal muscle response to insulin and the concurrent plasma insulin concentration. Therefore, skeletal mISI can be estimated as rate of decline in plasma glucose concentration from peak to nadir of the OGTT (dG/dt), divided by the mean plasma insulin concentration during time 30–120 min of the OGTT {Im; mISI = [(dG/dt ÷ Im) × −100], where −100 represents a constant that allows one to obtain numbers ranging from 0 to 10} (1).
Skeletal Muscle Tissue Collection
Skeletal muscle biopsies were taken from vastus lateralis muscle, 96–120 h following the last training session to avoid the potential effects of the last training session. After local anesthesia (1% lidocaine), tissue was procured using a 5-mm Bergstrom needle with applied suction (24), cleaned of nontarget tissues, flash frozen in liquid nitrogen, and stored at −80°C.
Western Blotting
Skeletal muscle (20–40 mg) was homogenized in ice-cold buffer [50 mmol/l HEPES, 150 mmol/l NaCl, 20 mmol/l Na4P2O7, 20 mmol/l β-glycerophosphate, 10 mmol/l NaF, 2 mmol/l Na3VO4, 1 mmol/l EDTA, 1 mmol/l EGTA, 1% (vol/vol) Nonidet P-40, 10% (vol/vol) glycerol, 2 mmol/l PMSF, 10 μg/ml leupeptin, 10 μg/ml aprotinin, and 3 mmol/l benzamidine]. Homogenates were rotated end over end at 4°C for 1 h and centrifuged (17,500 g; 4°C) for 30 min. Supernatant fractions were collected and protein concentrations determined using the bicinchoninic acid method (Pierce, Rockford, IL). Total protein content of relevant proteins was determined in muscle lysates by SDS-PAGE, followed by immunoblotting. Total protein levels of GLUT4 and insulin receptor substrate 1 (IRS1) were measured using antibodies from Pierce and EMD Millipore, respectively. Total protein levels of hexokinase 2 (HK2), RAC-β serine/threonine-protein kinase (AKT2), and GS kinase 3β (GSK3β) were measured using antibodies from Cell Signaling Technology (Beverly, MA).
Statistical Analyses
Nonparametric analyses were chosen for statistical inference due to the presence of non-normally distributed data and heteroscedasticity. The overall effects of the intervention were tested for evaluable participants, who completed both pre- and post-test visits. Significance was calculated using Wilcoxon signed-rank test, with P < 0.05 considered statistically significant. Confidence intervals were derived from bias-corrected bootstrap methods (100,000 permutations). Data were reported as median (interquartile range) unless stated otherwise. Significance for the OGTT was calculated by linear mixed model with Huber-White robust standard errors, and Bonferroni adjustment was used for multiple testing (α = 0.0125). Post hoc Spearman correlation analyses were used to determine the relationships between changes in muscle proteins and OGTT-derived indices. Statistical analyses were performed with the use of Stata Statistical Software 11.2 (StataCorp, College Station, TX).
RESULTS
Body Composition, Indirect Calorimetry, Strength, and Physical Activity
A total of 28 participants completed the pre- and post-test visits. Baseline anthropometrics, physical activity (via IPAQ), HbA1c, and fasting glucose and insulin of the eight participants who dropped out of the study following their pre-test visit were no different from that of the remaining 28 participants who completed the entire study (all P > 0.2). Twenty-five percent of participants reported Asian ethnicity, 35% Caucasian, and 35% Hispanic. Overall, participants who completed the intervention attended 99.7% of their scheduled training sessions.
We noted significant increases in BMI (P = 0.03), lean body mass (LBM; P < 0.0001), and REE (P = 0.02) and decreases in total fat mass (P = 0.002), trunk fat mass (P = 0.003), and total fat percent (P < 0.001; Table 1). Furthermore, relative 1-RM chest, leg, and row strength increased, along with a score of overall relative strength (all P < 0.0001). Moreover, IPAQ results indicated no changes in moderate (P = 1.00) or vigorous (P = 0.41) activity (as measured in MET·min/wk) outside of the training.
Table 1.
Body composition, strength measurements, and physical activity
| Median (25th–75th percentile) |
||||
|---|---|---|---|---|
| Outcomes | Pre-test | Post-test | Changes | P |
| Age, yr | 21.5 (20.0–23.0) | |||
| Height, m | 1.77 (1.73–1.81) | |||
| Weight, kg | 96.6 (90.0–103.5) | 97.1 (91.2–105.4) | 1.8 (−0.004 to 3.0) | 0.06 |
| BMI, kg/m2 | 30.9 (29.7–32.7) | 31.2 (30.3–32.7) | 0.39 (−0.18 to 0.96) | 0.03 |
| WC, cm | 103.3 (99.4–111.3) | 101.4 (96.8–108.7) | −0.55 (−2.3 to 0.85) | 0.24 |
| Total fat mass, kg | 27.9 (23.7–32.6) | 26.2 (20.5–30.1) | −1.0 (−2.9 to −0.44) | 0.002 |
| Total fat, % | 28.6 (26.3–31.2) | 26.2 (24.2–29.6) | −1.9 (−2.9 to −0.52) | <0.001 |
| Trunk fat mass, kg | 13.6 (11.6–16.9) | 12.8 (10.4–15.8) | −0.68 (−1.5 to −0.33) | 0.003 |
| Lean body mass, kg | 69.5 (64.7–72.8) | 70.9 (66.5–76.2) | 2.7 (2.0–3.4) | <0.0001 |
| REE, kcal/day | 1,924.0 (1,808.5–2,260.0) | 2,160.0 (2,013.5–2,372.0) | 131.0 (81.0–372.0) | 0.02 |
| 1-RM relative chest | 0.77 (0.58–0.85) | 0.88 (0.78–1.0) | 0.16 (0.13–0.20) | <0.0001 |
| 1-RM relative leg | 2.7 (2.4–3.1) | 3.5 (3.1–3.9) | 0.63 (0.54–0.94) | <0.0001 |
| 1 RM relative row | 0.83 (0.76–0.87) | 1.0 (0.90–1.1) | 0.16 (0.12–0.22) | <0.0001 |
| Relative strength score | 4.3 (3.8–4.8) | 5.3 (4.9–5.8) | 1.1 (0.87–1.3) | <0.0001 |
| Moderate, MET*min/wk−1 | 170.0 (0.0–500.0) | 190.0 (0.0–518.0) | 0.0 (0.0–555.0) | 1.0 |
| Vigorous, MET*min/wk−1 | 0.0 (0.0–540.0) | 27.5 (0.0–600.0) | 0.0 (0.0–1,440.0) | 0.41 |
| Total, MET · min−1 · wk−1 | 1,888.5 (1,054.1–2,760.8) | 1,659.5 (898.5–3,474.0) | −126.3 (−865.5 to 834.0) | 0.93 |
Significance was calculated using Wilcoxon signed-rank test. BMI, body mass index; WC, waist circumference; REE, resting energy expenditure; RM, repetition maximum; strength score, sum of all 3 strength measures; MET, metabolic equivalent of task; Total, sum of all activity.
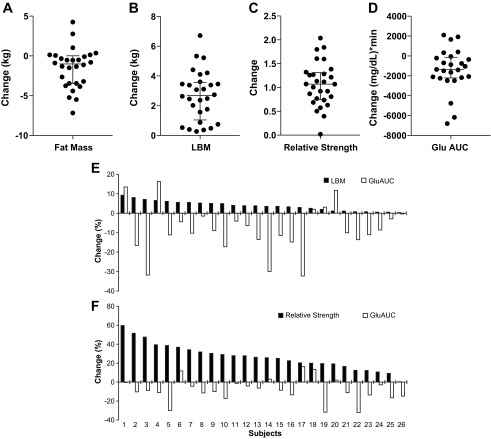
Glucose and Insulin Dynamics and Endocrine Response
A significant decrease in glucose (P = 0.004) and insulin AUC (P = 0.025) during the OGTT was observed after RT (Table 2). This drop was significant at OGTT time points—60 and 120 min for glucose and 90 and 120 min for insulin (all P < 0.01; Fig. 1, A and B). mISI and oral DI, an index of β-cell function, increased (both P = 0.03; Fig. 1C), whereas there were no significant changes in hepatic IRI (P = 0.67; Fig. 1C) or IGI (P = 0.27). No significant changes in adiponectin, leptin, and total amylin were detected (all P > 0.08; Table 2).
Table 2.
Glucose and insulin dynamics and endocrine panel
| Median (25th–75th percentile) |
Median (95% CI) | |||
|---|---|---|---|---|
| Outcomes | Pre-test | Post-test | Changes | P |
| HbA1c, % | 5.3 (5.2–5.6) | 5.3 (5.2–5.4) | 0.00 (−0.05 to 0.20) | 0.99 |
| Fasting glucose, mg/dl | 88.0 (85.5–93.9) | 90.0 (84.9–94.8) | 0.75 (−2.5 to 3.5) | 0.84 |
| 2-h Glucose, mg/dl | 111.0 (100.3–121.8) | 97.0 (87.8–113.0) | −13.5 (−19.0 to −1.5) | 0.005 |
| Glucose AUC, (mg/dl) · min | 14,812.5 (13,665.0–16,155.0) | 13,357.5 (12,195.0–14,745.0) | −1,357.5 (−2,062.5 to −325.5) | 0.004 |
| Fasting insulin, uIU/ml | 9.0 (5.5–12.0) | 9.0 (6.0–11.5) | 0.0 (−2.0 to 2.3) | 0.95 |
| 2-h Insulin, uIU/ml | 54.0 (36.0–82.0) | 35.0 (25.0–48.0) | −21.0 (−22.0 to −1.0) | <0.001 |
| Insulin AUC, (uIU/ml) · min | 7,008.8 (5,227.5–9,547.5) | 6,180.0 (4,395.0–9,345.0) | −1,042.5 (−1,252.5 to −367.5) | 0.025 |
| Hepatic IRI | 3,720.2 (2,186.4–6,574.4) | 4,301.6 (2,399.6–6,358.1) | −252.3 (−1,005.5 to 762.8) | 0.67 |
| Muscle ISI | 1.1 (0.71–1.3) | 1.4 (1.0–2.0) | 0.24 (0.05–0.64) | 0.03 |
| DI | 0.67 (0.47–0.79) | 0.78 (0.56–1.1) | 0.18 (−0.02 to 0.26) | 0.03 |
| IGI | 1.3 (0.90–1.7) | 1.4 (1.0–2.0) | 0.13 (−0.06 to 0.34) | 0.27 |
| Matsuda index | 0.49 (0.30–0.80) | 0.46 (0.37–0.87) | 0.07 (0.01–0.16) | 0.08 |
| Leptin, pM | 582.0 (326.5–1,070.0) | 449.5 (228.0–794.8) | −46.0 (−191.5 to 12.5) | 0.15 |
| Adiponectin, ng/ml | 32.3 (21.3–43.9) | 31.8 (18.6–40.6) | −1.3 (−3.9 to −0.47) | 0.08 |
| Total amylin, pmol/l | 17.2 (12.2–35.8) | 16.3 (12.3–27.0) | −1.6 (−4.0 to 2.8) | 0.19 |
Significance was calculated using Wilcoxon signed-rank test. Significance for the oral glucose tolerance test was calculated by linear mixed model with Huber-White robust SE and Bonferroni adjustment for multiple testing. CI, confidence interval; HbA1c, hemoglobin A1c; AUC, area under the curve; IRI, insulin resistance index; ISI, insulin sensitivity index; DI, disposition index; IGI, insulinogenic index.
Fig. 1.
Effects of resistance training (RT) on (A) glucose and (B) insulin levels during a 2-h oral glucose tolerance test. Data indicate significant reductions in time points—60 and 120 min for glucose and 90 and 120 min for insulin (n = 26). Bar graphs illustrate total glucose area under the curve (AUC) and insulin AUC, pre- and postintervention, for their respective curves. Data are presented as median and median absolute deviation (MAD). *P < 0.01. C: changes in muscle insulin sensitivity index (ISI), hepatic insulin resistance index (IRI), and oral disposition index (DI; *P < 0.05). D: effects of RT on protein content of glucose transporter type 4 (GLUT4), hexokinase 2 (HK2), insulin receptor substrate 1 (IRS1), glycogen synthase kinase 3β (GSK3β), and RAC-β serine/threonine-protein kinase (AKT2; *P < 0.02). Bar graphs present median and MAD for pre- and postintervention tests.
Skeletal Muscle Proteins
Figure 1D depicts the change in protein content of GLUT4, HK2, IRS1, GSK3β, and AKT2. Compared with the 27% increase in mISI, RT also resulted in median percent increases in HK2 (28%; P = 0.008), GLUT4 (26%; P = 0.02), and AKT2 (33%; P = 0.003) and no change in IRS1 or GSK3β. Exploratory correlations among skeletal muscle proteins and glucose AUC, insulin AUC, and OGTT-derived indices of mISI, hepatic IRI, and oral DI were not statistically significant.
Individual Responses
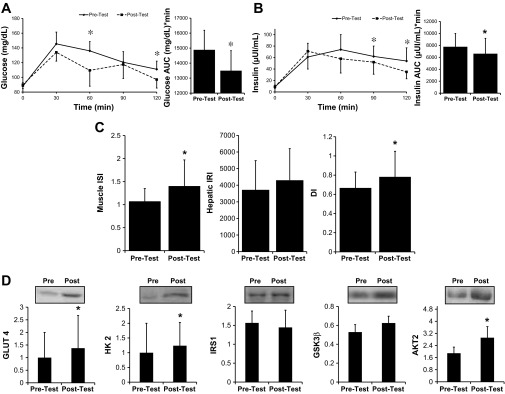
Figure 2 presents the change from pre- to post-test in each individual for fat mass (Fig. 2A), LBM (Fig. 2B), relative strength (Fig. 2C), and glucose AUC (Fig. 2D). Whereas all participants gained LBM and strength with the RT intervention, the degree of responsiveness was highly variable. Furthermore, although the majority of participants decreased fat mass and glucose AUC, this effect was not uniform, with a few participants exhibiting opposite responses. Figure 2, E and F, demonstrates the percent change in glucose AUC for each individual sorted by LBM or relative strength effect. Notably, the individualized effect of RT on glucose AUC was generally unrelated to the effect on either LBM or relative strength.
Fig. 2.
Individual responsiveness to 12-wk RT intervention presented as a change from pre-test values for fat mass (A), lean body mass (LBM; B), relative strength (C), and glucose AUC (Glu AUC; D) and also as a percent change sorted by LBM (E) and relative strength (F) compared with the effect on glucose AUC (glucose AUC vs. LBM Spearman correlation ρ = −0.11, P = 0.59; glucose AUC vs. relative strength ρ = 0.18, P = 0.39). A–D: data are presented as median and interquartile range.
DISCUSSION
Classically, insulin sensitivity has been estimated using the gold standard methods of the EHC and the FSIGT test. However, due to limitations in the ability to perform these tests clinically in a widespread fashion, alternative methods, such as the OGTT, have been used. Whereas the EHC estimates glucose disposal, and the FSIGT test estimates insulin secretion and β-cell function, the OGTT has been used to estimate glucose tolerance via AUCs or insulin action by the Matsuda index (33). One of the limitations of using the OGTT in clinical research studies has been the inability to quantify estimates of muscle and hepatic insulin sensitivity. In 2007, Abdul-Ghani et al. (1) published equations to estimate muscle and hepatic insulin sensitivity indices from the OGTT and validated these equations against the EHC. In addition, Abdul-Ghani and coworkers (3) estimated an index of oral DI validated with FSIGT testing, and others have validated similar estimates of insulin secretion and β-cell function from the FSIGT test (39, 40). Although it is well established that RT can improve glucose tolerance and whole-body insulin sensitivity (42), the effects of RT on the relative improvement in insulin sensitivity in different tissues are poorly understood. Given the simplicity of the OGTT, its ability to be used clinically, and the fact that it more closely mimics glucose and insulin dynamics of physiological conditions, we used these validated equations to estimate changes in mISI, hepatic IRI, and oral DI from an OGTT in response to a RT intervention in sedentary, overweight/obese young men.
The principal findings of the present study are: 1) RT improves OGTT-derived mISI and β-cell function but not hepatic IRI, suggesting that RT may preferentially affect insulin sensitivity in skeletal muscle; 2) mISI changes occur in combination with an increase in LBM and decreases in total and trunk fat mass but in the absence of weight loss; 3) RT increases protein content of proteins involved in muscle glucose transport (HK2, GLUT4, AKT2); and 4) RT effects demonstrate significant individual variability. These results support our primary hypothesis—that RT would improve mISI more than hepatic IRI, independent of weight loss—and suggest that RT may be a viable intervention to investigate for the prevention of type 2 diabetes.
One other study has estimated peripheral and hepatic insulin action after RT. Van Der Heijden et al. (47) noted no change in peripheral but a 24% improvement in hepatic insulin sensitivity with RT in youth. The differences in findings between this study and the present study may be due to a number of reasons: Hispanic ethnicity, which exhibits greater incidence of nonalcoholic fatty-liver disease (NAFLD) (44) and is associated with hepatic insulin resistance; glucose sampling techniques and index calculation; training volume (e.g., 2 days/wk compared with our 3 days/wk program); and/or dietary intake control. Kawaguchi et al. (29) demonstrated that a hybrid training of voluntary and electrical thigh-muscle contractions may decrease hepatic steatosis and insulin resistance (by fasting indices) in patients with NAFLD. Although Hallsworth et al. (23) also demonstrated a decrease in liver adiposity (by magnetic resonance) after 8 wk of RT in NAFLD patients, it is still unclear whether improvements in liver adiposity and glucose tolerance are directly related. In contrast to our study demonstrating an improvement in β-cell function, another study of RT in Hispanic youth by Shaibi et al. (45) noted no change in β-cell function. Ethnicity, age, and/or training volume (2 days/wk with a maximum 15 sets/session compared with our 3 days/wk program with as many as 24 sets/session) may again have contributed to this difference.
Glycemic control can also be assessed with HbA1c. Although several studies have demonstrated an improvement of HbA1c levels with RT (8–10, 21), others have shown no change (12, 16, 28). In general, HbA1c tends to decrease after RT in participants with type 2 diabetes. The lack of change in fasting glucose, insulin, or HbA1c in our study may be due to the fact that RT is unlikely to change HbA1c in participants without prediabetes or diabetes.
Accumulation of excess body fat results in secretion of proinflammatory cytokines and adipokines, which may be a possible mechanism by which obesity is associated with insulin resistance (38). In general, RT seems to have minimal effects on proinflammatory cytokines. In a companion paper (13), we noted that 12 wk of RT did not significantly affect a number of cytokines, including C-reactive protein, IL-8, and soluble adhesion molecules. The effect of RT on adipokines remains equivocal. In contrast to other studies that note an increase in adiponectin (35) and a decrease in leptin (31), our study resulted in no change in these adipokines. Interestingly, decreases in leptin and adiponectin were shown to be related to training intensity in elderly sedentary men (17). Muscle secretion of various myokines, such as IL-6, has also been suggested recently as possible regulators of inflammation and insulin sensitivity (36), but as with leptin and adiponectin, further investigation is needed to elucidate the role of RT on myokines and adipokines and their relationship to glucose tolerance and insulin sensitivity (35). We also measured amylin, which contributes to blood glucose regulation (48). Fasting amylin did not change, which is not surprising given that fasting levels of glucose and insulin also did not change.
Obesity is closely associated with type 2 diabetes, and weight loss is often emphasized as an important factor for improving insulin action. However, in our study, the effects of RT on mISI occurred in the absence of weight loss. Several studies also demonstrate that RT improves glucose tolerance or insulin sensitivity without altering body weight in: young (45, 47), obese, middle-aged (31), and older men (49); healthy, young (37), and postmenopausal (43) women; and subjects with type 2 diabetes (27, 28). Furthermore, these changes often occur without altering aerobic capacity (28, 31, 43). It is apparent that metabolic health improvement can occur independent of weight loss (20, 42), and more emphasis should be placed on lifestyle change, including increasing physical activity and exercise training.
Given that the increase in glucose clearance with RT appears to be explained by factors in addition to the increase in LBM, we also evaluated protein content of selected proteins involved in muscle glucose uptake and insulin signaling. As mentioned previously, RT may increase the content of proteins involved in insulin signaling toward increased glucose transport (25). In our study, we noted that protein expression of HK2 and GLUT4—two key regulators of insulin and contraction-induced glucose transport in skeletal muscle—was up-regulated following RT, thus potentially enabling a greater glucose flux across the plasma membrane. In addition, we observed a 33% increase in AKT2 expression, whereas expression of IRS1 and GSK3β did not change significantly following training. Some studies support the theory that improvements in glucose clearance with RT are predominately due to increases in LBM (i.e., increasing the sink for glucose disposal) (37, 46), whereas others note improvements even after controlling for changes in LBM (25, 28, 34). We found no correlations between the improvements in LBM (median increase of 4%) and protein content of HK2, GLUT4, and AKT2 and OGTT-derived indices (data not shown). Moreover, the improvements in glucose tolerance across participant LBM and strength improvements in this study were highly variable (Fig. 2, E and F, respectively). Thus improvements in glucose tolerance with RT are likely due to improvements in skeletal muscle quantity and quality; however, exact mechanisms still require elucidation (15). The lack of an obvious pattern among these results argues against the idea of solely a direct relationship between LBM and glucose tolerance and implies the existence of a more complex relationship, where changes in LBM, insulin signaling, and other potential factors, such as myocellular lipid changes, may contribute.
Another aspect that has been relatively underappreciated to date is the individual responsiveness to different forms of exercise training. In fact, responses to aerobic exercise training can be highly variable [see Fig. G.2.4 in the Physical Activity Guideline Advisory Committee Report (36a) and see Bouchard et al. (6)]. Boulé et al. (7) noted marked variability in improvements in intravenous glucose tolerance test-derived outcomes after 20 wk of cycle ergometer training. It is likely that individual responses to RT are also variable, and determination of this is important as we move toward individualizing exercise-training programs. For example, we noted relative strength increases ranging from 2% to 60% and increases in LBM from <1% to 9% (26). This occurred in conjunction with highly variable responsiveness for both fat mass (33% decrease to 13% increase) and glucose AUC (32% decrease to 16% increase) to 12 wk of RT. It is interesting to note that in the study by Van Der Heijden et al. (47), the peripheral insulin sensitivity response was highly variable, contributing to a nonsignificant outcome. Genetic variation (6), training motivation (i.e., effort), and other factors likely account for the spectrum of responses observed in our study.
In conclusion, RT appears to improve muscle insulin action and β-cell function, increases strength and LBM, and decreases total and trunk fat mass without weight loss in overweight/obese young-adult men. Whereas these findings are noted, study limitations include the lack of a control group, the lack of dietary control at the time of pre- and postintervention visits, and the gender-specific population. As regular participation in RT is associated with a lower risk of developing type 2 diabetes, independent of aerobic training (22), and reduces HbA1c compared with the effectiveness of metformin (14) in patients with type 2 diabetes (9), the present findings provide further evidence for RT as a potentially effective therapeutic option for the prevention of type 2 diabetes, especially for individuals who may be noncompliant with medications and/or unable to engage in aerobic exercise. Furthermore, given the simplicity and clinical use of the OGTT, future studies may consider potential use of OGTT-derived indices of insulin sensitivity in the early detection and management of metabolic disease.
GRANTS
Support for this work was provided by the American Heart Association (BGIA #0765139Y to C. K. Robers), National Heart, Lung, and Blood Institute (P50 HL105188 to C. K. Roberts), National Institute of Diabetes and Digestive and Kidney Diseases (DK090406 to C. K. Roberts), and National Center for Advancing Translational Sciences through UCLA Clinical and Translational Science Institute (CTSI) Grant UL1TR000124.
DISCLOSURES
C. K. Roberts is the guarantor of this work and as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Author contributions: D.M.C. and C.K.R. conception and design of research; D.M.C., E.P., N.B., B.K.L., D.L., and C.C.L. performed experiments; D.M.C., E.P., and C.K.R. interpreted results of experiments; D.M.C., M.M.L., and B.K.L. prepared figures; D.M.C. and C.K.R. drafted manuscript; D.M.C., E.P., M.M.L., N.B., C.C.L., and C.K.R. edited and revised manuscript; D.M.C., E.P., M.M.L., N.B., B.K.L., D.L., C.C.L., and C.K.R. approved final version of manuscript.
ACKNOWLEDGMENTS
We thank Shannon Krell, Samuel Kianmahd, Christopher S. Oh, Michael Katiraie, Claudia Lam, Madeleine Wilcox, Fanny Xu, Stacy Young, and Kristin Anderson (all from UCLA) and the entire Exercise and Metabolic Disease Research Laboratory team for their commitment to this study. We thank the dedicated nurses and staff of the UCLA Clinical and Translational Research Center (CTRC), Gonda (Goldschmied) Diabetes Center, and Diabetes and Endocrinology Research Center (DERC) and Elisa Terry and colleagues at the John Wooden Recreation Center. We also thank Xiao Chen, Phil Ender, and the UCLA Academic Technology Services Statistical Consulting Group for their statistical support. Furthermore, we thank all participants for their time and effort.
REFERENCES
- 1.Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo RA. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care 30: 89–94, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Abdul-Ghani MA, Williams K, DeFronzo RA, Stern M. What is the best predictor of future type 2 diabetes? Diabetes Care 30: 1544–1548, 2007 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association National Diabetes Fact Sheet, 2011 (Online). American Diabetes Association, Alexandria, VA: http://www.diabetes.org/diabetes-basics/diabetes-statistics/ [2012]. [Google Scholar]
- 5.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol 2: 1143–1211, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, Gagnon J, Perusse L, Leon AS, Rao DC. Familial aggregation of VO2 max response to exercise training: results from the HERITAGE Family Study. J Appl Physiol 87: 1003–1008, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Boulé NG, Weisnagel SJ, Lakka TA, Tremblay A, Bergman RN, Rankinen T, Leon AS, Skinner JS, Wilmore JH, Rao DC, Bouchard C. Effects of exercise training on glucose homeostasis: the HERITAGE Family Study. Diabetes Care 28: 108–114, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Brooks N, Layne JE, Gordon PL, Roubenoff R, Nelson ME, Castaneda-Sceppa C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci 4: 19–27, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castaneda C, Layne JE, Munoz-Orians L, Gordon PL, Walsmith J, Foldvari M, Roubenoff R, Tucker KL, Nelson ME. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care 25: 2335–2341, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Cauza E, Strehblow C, Metz-Schimmerl S, Strasser B, Hanusch-Enserer U, Kostner K, Dunstan D, Fasching P, Haber P. Effects of progressive strength training on muscle mass in type 2 diabetes mellitus patients determined by computed tomography. Wien Med Wochenschr 159: 141–147, 2009 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Diabetes Data & Trends. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/diabetes/statistics [2011]. [Google Scholar]
- 12.Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K, Mikus CR, Myers V, Nauta M, Rodarte RQ, Sparks L, Thompson A, Earnest CP. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA 304: 2253–2262, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Croymans DM, Krell SM, Oh CS, Katiraie M, Lam C, Harris RA, Roberts CK. Effects of resistance training on central blood pressure in obese young men. J Hum Hypertens. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 333: 541–549, 1995 [DOI] [PubMed] [Google Scholar]
- 15.Dela F, Kjaer M. Resistance training, insulin sensitivity and muscle function in the elderly. Essays Biochem 42: 75–88, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Dunstan DW, Puddey IB, Beilin LJ, Burke V, Morton AR, Stanton KG. Effects of a short-term circuit weight training program on glycaemic control in NIDDM. Diabetes Res Clin Pract 40: 53–61, 1998 [DOI] [PubMed] [Google Scholar]
- 17.Fatouros IG, Tournis S, Leontsini D, Jamurtas AZ, Sxina M, Thomakos P, Manousaki M, Douroudos I, Taxildaris K, Mitrakou A. Leptin and adiponectin responses in overweight inactive elderly following resistance training and detraining are intensity related. J Clin Endocrinol Metab 90: 5970–5977, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Ferrannini E, Bjorkman O, Reichard GA, Jr, Pilo A, Olsson M, Wahren J, DeFronzo RA. The disposal of an oral glucose load in healthy subjects. A quantitative study. Diabetes 34: 580–588, 1985 [DOI] [PubMed] [Google Scholar]
- 19.Fogelholm M, Malmberg J, Suni J, Santtila M, Kyrolainen H, Mantysaari M, Oja P. International Physical Activity Questionnaire: validity against fitness. Med Sci Sports Exerc 38: 753–760, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Gaesser GA, Angadi SS, Sawyer BJ. Exercise and diet, independent of weight loss, improve cardiometabolic risk profile in overweight and obese individuals. Phys Sportsmed 39: 87–97, 2011 [DOI] [PubMed] [Google Scholar]
- 21.Gordon PL, Vannier E, Hamada K, Layne J, Hurley BF, Roubenoff R, Castaneda-Sceppa C. Resistance training alters cytokine gene expression in skeletal muscle of adults with type 2 diabetes. Int J Immunopathol Pharmacol 19: 739–749, 2006 [DOI] [PubMed] [Google Scholar]
- 22.Grøntved A, Rimm EB, Willett WC, Andersen LB, Hu FB. A prospective study of weight training and risk of type 2 diabetes mellitus in men. Arch Intern Med 172: 1306–1312, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hallsworth K, Fattakhova G, Hollingsworth KG, Thoma C, Moore S, Taylor R, Day CP, Trenell MI. Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut 60: 1278–1283, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hennessey JV, Chromiak JA, Dellaventura S, Guertin J, Maclean DB. Increase in percutaneous muscle biopsy yield with a suction-enhancement technique. J Appl Physiol 82: 1739–1742, 1997 [DOI] [PubMed] [Google Scholar]
- 25.Holten MK, Zacho M, Gaster M, Juel C, Wojtaszewski JF, Dela F. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscle in patients with type 2 diabetes. Diabetes 53: 294–305, 2004 [DOI] [PubMed] [Google Scholar]
- 26.Hubal MJ, Gordish-Dressman H, Thompson PD, Price TB, Hoffman EP, Angelopoulos TJ, Gordon PM, Moyna NM, Pescatello LS, Visich PS, Zoeller RF, Seip RL, Clarkson PM. Variability in muscle size and strength gain after unilateral resistance training. Med Sci Sports Exerc 37: 964–972, 2005 [PubMed] [Google Scholar]
- 27.Ibanez J, Izquierdo M, Arguelles I, Forga L, Larrion JL, Garcia-Unciti M, Idoate F, Gorostiaga EM. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care 28: 662–667, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Ishii T, Yamakita T, Sato T, Tanaka S, Fujii S. Resistance training improves insulin sensitivity in NIDDM subjects without altering maximal oxygen uptake. Diabetes Care 21: 1353–1355, 1998 [DOI] [PubMed] [Google Scholar]
- 29.Kawaguchi T, Shiba N, Maeda T, Matsugaki T, Takano Y, Itou M, Sakata M, Taniguchi E, Nagata K, Sata M. Hybrid training of voluntary and electrical muscle contractions reduces steatosis, insulin resistance, and IL-6 levels in patients with NAFLD: a pilot study. J Gastroenterol 46: 746–757, 2011 [DOI] [PubMed] [Google Scholar]
- 30.Kelley D, Mitrakou A, Marsh H, Schwenk F, Benn J, Sonnenberg G, Arcangeli M, Aoki T, Sorensen J, Berger M, Sonksen P, Gerich J. Skeletal muscle glycolysis, oxidation, and storage of an oral glucose load. J Clin Invest 81: 1563–1571, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klimcakova E, Polak J, Moro C, Hejnova J, Majercik M, Viguerie N, Berlan M, Langin D, Stich V. Dynamic strength training improves insulin sensitivity without altering plasma levels and gene expression of adipokines in subcutaneous adipose tissue in obese men. J Clin Endocrinol Metab 91: 5107–5112, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Krssak M, Brehm A, Bernroider E, Anderwald C, Nowotny P, Dalla Man C, Cobelli C, Cline GW, Shulman GI, Waldhausl W, Roden M. Alterations in postprandial hepatic glycogen metabolism in type 2 diabetes. Diabetes 53: 3048–3056, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22: 1462–1470, 1999 [DOI] [PubMed] [Google Scholar]
- 34.Miller JP, Pratley RE, Goldberg AP, Gordon P, Rubin M, Treuth MS, Ryan AS, Hurley BF. Strength training increases insulin action in healthy 50- to 65-yr-old men. J Appl Physiol 77: 1122–1127, 1994 [DOI] [PubMed] [Google Scholar]
- 35.Olson TP, Dengel DR, Leon AS, Schmitz KH. Changes in inflammatory biomarkers following one-year of moderate resistance training in overweight women. Int J Obes 31: 996–1003, 2007 [DOI] [PubMed] [Google Scholar]
- 36.Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol 98: 1154–1162, 2005 [DOI] [PubMed] [Google Scholar]
- 36a.Physical Activity Guidelines Advisory Committee Physical Activity Guidelines Advisory Committee Report 2008. Washington, DC: U.S. Department of Health and Human Services, 2008 [DOI] [PubMed] [Google Scholar]
- 37.Poehlman ET, Dvorak RV, DeNino WF, Brochu M, Ades PA. Effects of resistance training and endurance training on insulin sensitivity in nonobese, young women: a controlled randomized trial. J Clin Endocrinol Metab 85: 2463–2468, 2000 [DOI] [PubMed] [Google Scholar]
- 38.Rabe K, Lehrke M, Parhofer KG, Broedl UC. Adipokines and insulin resistance. Mol Med 14: 741–751, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Retnakaran R, Qi Y, Goran MI, Hamilton JK. Evaluation of proposed oral disposition index measures in relation to the actual disposition index. Diabet Med 26: 1198–1203, 2009 [DOI] [PubMed] [Google Scholar]
- 40.Retnakaran R, Shen S, Hanley AJ, Vuksan V, Hamilton JK, Zinman B. Hyperbolic relationship between insulin secretion and sensitivity on oral glucose tolerance test. Obesity (Silver Spring) 16: 1901–1907, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Roberts CK, Barnard RJ. Effects of exercise and diet on chronic disease. J Appl Physiol 98: 3–30, 2005 [DOI] [PubMed] [Google Scholar]
- 42.Roberts CK, Hevener AL, Barnard RJ. Metabolic syndrome and insulin resistance: underlying casues and modification by exercise training. Compr Physiol 3: 1–58, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ryan AS, Pratley RE, Goldberg AP, Elahi D. Resistive training increases insulin action in postmenopausal women. J Gerontol A Biol Sci Med Sci 51: M199–M205, 1996 [DOI] [PubMed] [Google Scholar]
- 44.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics 118: 1388–1393, 2006 [DOI] [PubMed] [Google Scholar]
- 45.Shaibi GQ, Cruz ML, Ball GD, Weigensberg MJ, Salem GJ, Crespo NC, Goran MI. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc 38: 1208–1215, 2006 [DOI] [PubMed] [Google Scholar]
- 46.Takala TO, Nuutila P, Knuuti J, Luotolahti M, Yki-Jarvinen H. Insulin action on heart and skeletal muscle glucose uptake in weight lifters and endurance athletes. Am J Physiol Endocrinol Metab 276: E706–E711, 1999 [DOI] [PubMed] [Google Scholar]
- 47.Van Der Heijden G, Wang ZJ, Chu Z, Toffolo G, Manesso E, Sauer PJ, Sunehag AL. Strength exercise improves muscle mass and hepatic insulin sensitivity in obese youth. Med Sci Sports Exerc 42: 1973–1980, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Westermark P, Andersson A, Westermark GT. Islet amyloid polypeptide, islet amyloid, and diabetes mellitus. Physiol Rev 91: 795–826, 2011 [DOI] [PubMed] [Google Scholar]
- 49.Zachwieja JJ, Toffolo G, Cobelli C, Bier DM, Yarasheski KE. Resistance exercise and growth hormone administration in older men: effects on insulin sensitivity and secretion during a stable-label intravenous glucose tolerance test. Metabolism 45: 254–260, 1996 [DOI] [PubMed] [Google Scholar]