Abstract
Background:
Bow Hunter's syndrome/stroke is defined as symptomatic, vertebrobasilar insufficiency provoked by physiologic head rotation. It is a diagnostically challenging cause of posterior circulation stroke in children. While there have been prior reports of this rare disorder, we describe an exceptional case of pediatric Bow Hunter's stroke resulting from a near complete occlusion the right vertebral artery (VA) secondary to an anomalous spur emanating from the right occipital condyle. Surgical and endovascular options and approaches are also detailed herein.
Case Description:
A 16-year-old male presented with multiple posterior circulation ischemic strokes. A dynamic computerized tomography angiogram performed with the patient's head in a rotated position revealed a near complete occlusion of the V3 segment of the right VA from a bone spur arising from his occipital condyle. The spur caused a focal dissection of the distal right VA with associated thrombus. He was initially managed with a cervical collar, antiplatelet therapy with aspirin 81 mg and anticoagulation with coumadin (INR goal 2-3) for 3 months. Despite the management plan, he had a subsequent thromboembolic event and a right VA sacrifice with coil embolization was then performed. At the 3-month follow-up, the patient was doing well with no reports of any subsequent strokes.
Conclusion:
We report the first reported pediatric case of Bow Hunter's stroke due to dynamic right VA occlusion from an occipital condylar bone spur. The vascular compression from this spur led to a right VA dissection and thrombus formation and ultimately caused multiple posterior circulation thromboembolic strokes. Endovascular treatment options including vessel sacrifice should be considered in cases that have failed maximal medical management.
Keywords: Bow Hunter's syndrome, coil embolization, endovascular surgery, stroke, vertebral artery
INTRODUCTION
Bow Hunter's syndrome/stroke (BHS) is the clinical presentation of posterior circulation ischemia produced by reversible occlusion of the vertebral artery (VA) lumen during head rotation. The term BHS was coined by Sorensen in 1978 based on observations of a patient becoming symptomatic during archery.[12]
Overall, the incidence of BHS is rare, and there are about 60 reported cases in the literature. BHS usually presents with transient ischemia in the adult population, whereas stroke is the predominant clinical presentation in children. While acute ischemic stroke is rare in children, with an estimated incidence of 2.5 per 100,000,[4] posterior circulation stroke (PCS) represents an even smaller fraction of the total incidence. Notably, among males the incidence of pediatric stroke is higher; similarly, there is a higher percentage of PCS.[2,3,4]
Vertebral artery dissection (VAD) in children with BHS may be secondary to repetitive trauma or abrupt movements towards the extremes of the physiologic range of motion. VAD is a significant cause of thrombus formation and PCS. We report a rare case of BHS secondary to right VA occlusion from a right occipital condylar bone spur, which was treated successfully by endovascular management using coil embolization/vessel sacrifice of the VA.
CASE REPORT
A 16-year-old male presented with right-sided numbness, dysphagia, and right peripheral vision loss after working out during football practice. In the emergency room (ER) his right-sided visual field defect persisted, with anomia and alexia. He stated that he had experienced intermittent episodes and discreet events over the past year including weakness, numbness, and vision loss.
He had a computerized tomography scan of the head, which revealed areas of hypodensity in the left temporoparietal region suggestive of stroke. This finding was confirmed by magnetic resonance imaging, which revealed multiple strokes of different ages. Specifically, he had an acute stroke in the left temporoparietal region, along with subacute strokes in the right thalamus, spanning the corpus callosum and left cerebellum. The patient was then admitted to the pediatric intensive care unit (PICU) for observation and further workup. A cerebral angiogram revealed a focal dissection of the distal right VA with a small nonocclusive thrombus proximal to the dissection. The only suspicious event from the patient's history was a wrestling incident in the locker rooms a few days before the onset of stroke. He was followed by neurology and hematology/oncology, and had workups to rule out vasculitis, metabolic, hypercoagulable, and cardiac embolic sources, all of which were negative. Anticoagulation with enoxaparin was then initiated, and the patient was discharged home with instructions to avoid weight lifting and contact sports.
Approximately 3 months after his initial presentation and completing his 3-month course of anticoagulation with therapeutic enoxaparin, the patient experienced new transient neurological symptoms of headache, blurred vision, and confusion. Incidentally, he began weightlifting a week prior to the onset of his new symptoms. Magnetic resonance imaging of the brain revealed a subacute stroke in the left medial cerebellum, and a new area of encephalomalacia, suspicious for a stroke, in the parietal region near the vertex that occurred after his initial hospitalization. The patient was then admitted for further evaluation.
A dynamic cerebral angiogram was performed and revealed that the patient had a Bow Hunter's type phenomenon, with dynamic occlusion of the right VA in the chin up position looking to the left [Figure 1].
Figure 1.
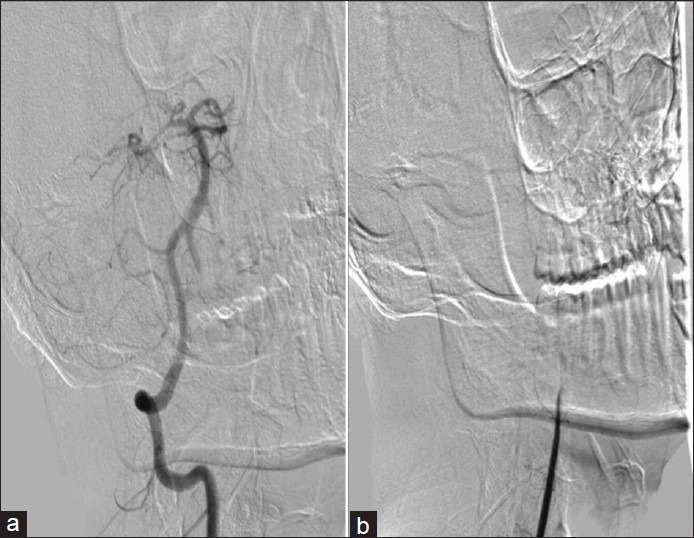
(a) Cerebral angiogram of the right vertebral artery showing a normal course and flow of the artery. (b) Dynamic right vertebral artery angiogram with the head turned showing complete flow obstruction
A dynamic computerized tomography angiogram performed with the patient's head in rotated position showed a near complete occlusion of the V3 segment of the right VA resulting from an anomalous spur emanating from his right occipital condyle that pinched off his VA between the C1 ring and this condylar spur [Figure 2]. This was determined to be the etiology of the dissection. Therefore, the patient was managed by neck immobilization via a cervical collar, and we initiated aspirin 81 mg and coumadin with an INR goal of 2-3. At this time, the plan was to allow the dissection flap to heal and then bring the patient back for elective surgical decompression of the condylar spur.
Figure 2.
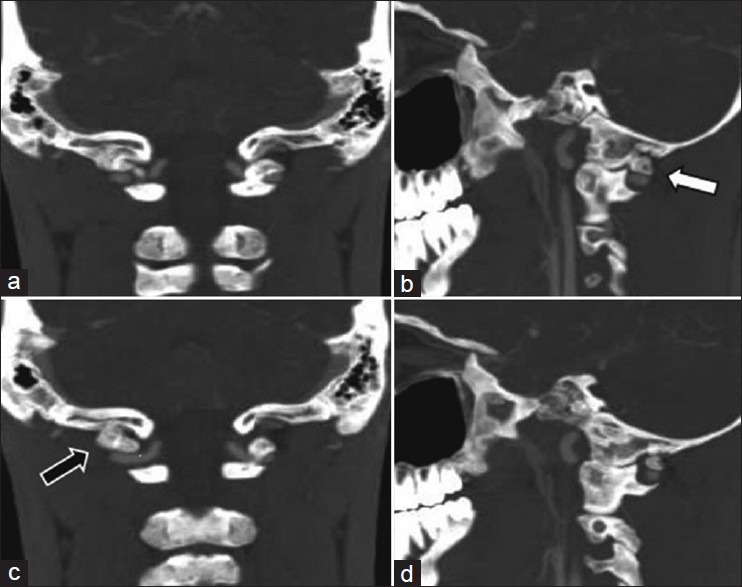
(a-d) Computerized tomography angiogram of the head and neck demonstrating both the aberrant right condylar bone spur (arrow) and its close proximity to the right vertebral artery
However, 2 weeks after the treatment modality of immobilization and pharmacotherapy, the patient presented with a transient ischemic attack. He reported right hemibody numbness and tingling. His INR at that point was subtherapeutic, first at 1.8 then at 1.6. A magnetic resonance imaging and magnetic resonance angiography of the head and neck revealed persistent narrowing of the V3 segment of the VA to 50%, with new strokes noted in the occipital lobe, right cerebellum, and a thrombus in the left P2-3 segment of the left posterior cerebral artery.
Since the patient had further thrombotic episodes due to the dissection, he was admitted and placed on 325 mg aspirin, clopidrogrel (300 mg load followed by 75 mg daily), and a heparin infusion. After a thorough discussion of all treatment options, including stenting of the artery, surgery to drill off the spur, or continued medical therapy, the decision was made to proceed with coil embolization/sacrifice of the right VA so as to prevent further thromboembolic events as well as to avoid the future need for surgical decompression of the anomalous occipital condyle process. The right VA was sacrificed with coil embolization and trapping of a 4 mm thrombus over the dissected segment [Figure 3]. The patient tolerated the procedure without complication and was subsequently discharged home.
Figure 3.
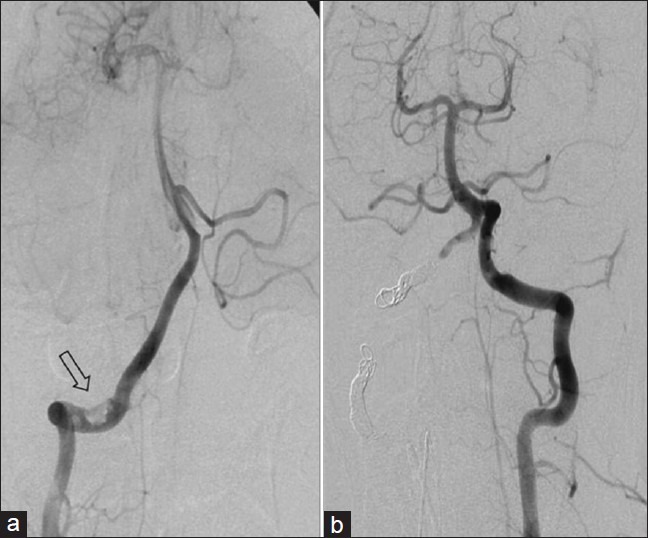
(a) Cerebral angiogram of the right vertebral artery demonstrating a dissection and associated thrombus (arrow) secondary to intermittent condylar bone spur compression. (b) Cerebral angiogram of the left vertebral artery. The right vertebral artery has been occluded with coil embolization both proximally and distally, trapping the thrombus. The right PICA is preserved through a right AICA-PICA variant
During his initial postoperative clinic visit, one week status-post right VA sacrifice, his cervical collar was discontinued. During his 5 week postoperative clinic visit, he reported no further episodes of seizures, paresthesias, headache, or neck pain. He was doing well on aspirin 81 mg with a plan to continue antiplatelet therapy indefinitely
Three months status-post right VA sacrifice, the patient had a baseline right homonymous hemianopsia and a mild nystagmus, especially with right lateral gaze, but was otherwise doing well and denied any symptoms. He had increased his level of activity and started weightlifting but was not cleared for contact sports.
DISCUSSION
Our case demonstrates the importance of maintaining a high clinical suspicion for the diagnosis of BHS. We described a very active 16-year-old male with a near complete occlusion of the right VA due to an anomalous spur off the right occipital condyle that resulted in a VA dissection and subsequent thromboembolic strokes.
A VA compression can occur at various levels, but it most commonly occurs at the atlanto–axial junction. This is as a result of the stretch that the VA undergoes between the foramen transversarium of C-1 and C-2 during head rotation.[11] In this case we describe a rare location of VA occlusion that occurred along the V3 segment of the VA as it exits the C-1 foramen transversarium.
Treatment options include medical therapy, surgical, and, more recently, endovascular management. The medical management option (neck immobilization and anticoagulation therapy for 3 months) was used initially in this case, but failed to prevent thromboembolic events. The long-term efficacy of medical management alone has not been reported. Due to the high morbidity and mortality associated with the risk of recurrent PCS, definitive treatment (endovascular versus surgical) should be recommended in such cases. We would like to note that our initial intention was to use medical therapy as a bridge to definitive surgical decompression.
Depending on the etiology of BHS, there are different treatment options available. When the contralateral VA is occluded, absent, markedly hypoplastic and/or ends in posterior inferior cerebellar artery (PICA), surgical decompression by way of freeing the affected vessel from the C1 transverse foramen is the most direct treatment option available. When severe stenosis of the contralateral artery contributes to BHS, then angioplasty and stenting of the vessel may relieve the symptoms by improving the collateral blood supply. Finally, sacrifice of the affected artery is the least common treatment, but is occasionally required.
Surgical decompression of the VA through various approaches has been described in the literature.[1,8] Lu et al. reported a case of successful decompression of the VA between the skull base and C-1 via a minimally invasive 22-mm tubular retractor. Cornelius et al. reported a clinical series of five patients with BHS caused by mechanical occlusion of the VA that had surgical decompression of the VA via an antero-lateral approach in four of the five patients, with one patient requiring a posterior approach and simultaneous occipto-cervical fusion (C0-C2) due to preexisting instability. In their study, they hypothesize that the presence of antero-lateral fibrous bands, which are not identifiable on preoperative imaging, may have explained some of the surgical failures from using a posterior midline approach as reported by Matsuyama et al.[10] The risk of postoperative recurrence following decompressive surgery with reocclusion of the operated VA has also been reported. Matsuyama et al. reported that three out of nine patients showed postoperative recurrence after decompression surgery and no recurrence among eight patients after posterior fusion.[9]
Endovascular treatment options are an effective and potentially less invasive option in the treatment of BHS. VA stenting has been used in the setting of contralateral VA stenosis.[13] VA compression caused by head rotation is usually asymptomatic due to sufficient contralateral flow, however, vertbrobasilar insufficiency does occur in cases with contralateral severe stenosis or occlusion. Husni and Storer[6] reported 23 patients with vertebrobasilar insufficiency induced by rotational occlusion of one VA. The opposite VA was hypoplastic or absent in 22 patients and narrowed at its origin in 1 patient.
Sugiu et al. [13] reported a case of a patient with severe stenosis at the origin of the left VA found on angiography. In addition, dynamic angiography with head turning to the left detected a right VA occlusion at the C1-2 level by a bony structure. The patient underwent angioplasty and stent placement at the origin of the left VA, which resulted in vessel patency and no recurrence of symptoms postoperatively at 6 months follow-up. Resolution of the symptoms was a result of improving collateral blood flow from the left VA. In contrast, Horowitz et al. stated that their experience with stenting in this location has not been favorable.[7] The success rates for angioplasty and stenting of the proximal VA based on modern series reports by Hatano et al.[5] and Vaida et al.[14] demonstrate >90% success with delayed restenosis rates of 5-12%. The case we report is notable for unusual patholophysiology since the patient had a patent left VA but had a 4 mm mobile thrombus in the dissected right VA that was causing recurrent PCS.
After a thorough discussion of all treatment options with the patient and his family, a decision was made to sacrifice the right VA and trap the dissected segment and large thrombus, which was adherent to the flap. The least common treatment option was chosen in our patient because of the extremely tenuous nature of the clot. As seen during angiography, the thrombus was very mobile and tenuous within the lumen, and any device that could be introduced in the area for angioplasty or stenting could easily dislodge the clot leading to catastrophic results. Therefore the decision to sacrifice the right VA was made in order to ultimately trap the distal segment and prevent further emboli. As illustrated in this case, sacrificing the right VA stopped the thromboembolic events and avoided the future need for surgery to decompress the anomalous occipital condyle spur.
CONCLUSION
We report a rare case of BHS due to dynamic right VA occlusion from a right occipital condyle spur. The intermittent compression led to a right VA dissection and thrombus formation, therefore causing multiple posterior circulation thromboembolic strokes. Endovascular treatment options including vessel sacrifice should be considered in cases that have failed conservative management, especially when there is a risk of PCS from recurrent thromboembolic events. Our case demonstrates the importance of maintaining a high clinical suspicion for the diagnosis of BHS in patients with vertebrobasilar ischemia.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/148/121647
Contributor Information
Tony I. Anene-Maidoh, Email: tanenemaidoh@mcvh.vcu.edu.
Rafael A. Vega, Email: ravega@mcvh.vcu.edu.
Gregory L. Fautheree, Email: geauxlsu77@cox.net.
John F. Reavey-Cantwell, Email: jreavey-cantwell@mcvh-vcu.edu.
REFERENCES
- 1.Cornelius JF, George B, N’dri Oka D, Spiriev T, Steiger HJ, Hanggi D. Bow-hunter's syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction-a management algorithm based on a systemic review and a clinical series. Neurosurg Rev. 2012;35:127–35. doi: 10.1007/s10143-011-0343-4. [DOI] [PubMed] [Google Scholar]
- 2.Ganesan V, Chong WK, Cox TC, Chawda SJ, Prengler M, Kirkham FJ. Posterior circulation stroke in childhood: Risk factors and recurrence. Neurology. 2002;59:1552–6. doi: 10.1212/01.wnl.0000033092.87560.1a. [DOI] [PubMed] [Google Scholar]
- 3.Golomb MR, Fullerton HJ, Nowak-Gottl U, Deveber G. Male predominance in childhood ischemic stroke: Findings from the international pediatric stroke study. Stroke. 2009;40:52–7. doi: 10.1161/STROKEAHA.108.521203. [DOI] [PubMed] [Google Scholar]
- 4.Greiner HM, Abruzzo TA, Kabbouche M, Leach JL, Zuccarello M. Rotational vertebral artery occlusion in a child with multiple strokes: A case-based update. Childs Nerv Syst. 2010;26:1669–74. doi: 10.1007/s00381-010-1299-3. [DOI] [PubMed] [Google Scholar]
- 5.Hatano T, Tsukahara T, Miyakoshi A, Arai D, Yamaguchi S, Murakami M. Stent placement for atherosclerotic stenosis of the vertebral artery ostium: Angiographic and clinical outcomes in 117 consecutive patients. Neurosurgery. 2011;68:108–16. doi: 10.1227/NEU.0b013e3181fc62aa. [DOI] [PubMed] [Google Scholar]
- 6.Husni EA, Storer J. The syndrome of mechanical occlusion of the vertebral artery; further observations. Angiology. 1967;18:106–16. doi: 10.1177/000331976701800205. [DOI] [PubMed] [Google Scholar]
- 7.Horowitz M, Jovin T, Balzar J, Welch W, Kassam A. Bow hunter's syndrome in the setting of contralateral vertebral artery stenosis: Evaluation and treatment options. Spine. 2002;27:E495–8. doi: 10.1097/00007632-200212010-00015. [DOI] [PubMed] [Google Scholar]
- 8.Lu DC, Gupta N, Mummaneni PV. Minimally invasive decompression of a suboccipital osseous prominence causing rotational vertebral artery occlusion. J Neurosurg Pediatr. 2009;4:191–5. doi: 10.3171/2009.3.PEDS08270. [DOI] [PubMed] [Google Scholar]
- 9.Matsuyama T, Morimoto T, Sakaki T. Bow Hunter's stroke caused by a nondominant vertebral artery occlusion: Case report. Neurosurgery. 1997;41:1393–5. doi: 10.1097/00006123-199712000-00030. [DOI] [PubMed] [Google Scholar]
- 10.Matsuyama T, Morimoto T, Sakaki T. Comparison of C1-2 posterior fusion and decompression of the vertebral artery in the treatment of bow hunter's stroke. J Neurosurg. 1997;86:619–23. doi: 10.3171/jns.1997.86.4.0619. [DOI] [PubMed] [Google Scholar]
- 11.Miele VJ, France JC, Rosen CL. Subaxial positional vertebral artery occlusion corrected by decompression and fusion. Spine. 2008;33:E366–70. doi: 10.1097/BRS.0b013e31817192a1. [DOI] [PubMed] [Google Scholar]
- 12.Sorensen BF. Bow hunter's stroke. Neurosurgery. 1978;2:259–61. doi: 10.1227/00006123-197805000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Sugiu K, Agari T, Tokunaga K, Nishida A, Date I. Endovascular Treatment for Bow Hunter's Syndrome: Case Report. Minim Invas Neurosurg. 2009;52:193–5. doi: 10.1055/s-0029-1239501. [DOI] [PubMed] [Google Scholar]
- 14.Vajda Z, Miloslavski E, Güthe T, Fischer S, Albes G, Heuschmid A, et al. Treatment of stenoses of vertebral artery origin using short drug-eluting coronary stents: Improved follow-up results. AJNR Am J Neuroradiol. 2009;30:1653–6. doi: 10.3174/ajnr.A1715. [DOI] [PMC free article] [PubMed] [Google Scholar]


