Abstract
Background:
In 2011, Epstein and Hood documented that 17.2% of 274 patients with cervical/lumbar complaints seen in first or second opinion over one year were told they needed “unnecessary” spine surgery (e.g., defined as for pain alone, without neurological deficits, or significant radiographic abnormalities). Subsequently, in 2012 Gamache found that 69 (44.5%) of the 155 second opinion patients seen over a 14-month period were told by outside spine surgeons that they needed surgery; the second opinion surgeon (Gamache) found those operations to be unnecessary. Increasingly, patients, spine surgeons, hospitals, and insurance carriers should not only be questioning whether spinal operations are “unnecessary”, but also whether they are “wrong” (e.g., overly extensive, anterior vs. posterior operations), or “right” (appropriate).
Methods:
Prospectively, 437 patients with cervical or lumbar complaints were seen in spinal consultation over a 20-month period. Of the 254 (58.1%) patients coming in for first opinions those with surgical vs. non-surgical lesions were identified. Of the 183 (41.9%) patients coming in for second opinions, who were previously told by outside surgeons that they needed spine operations, the second opinion surgeon documented the number of “unnecessary”, “wrong”, or “right” operations previously recommended.
Results:
Surgical pathology was identified in 138 (54.3%) patients presenting for first opinions. For patients seen in second opinion, 111 (60.7%) were told by outside surgeons that they required “unnecessary”, 61 (33.3%) the “wrong”, or 11 (6%) the “right” operations.
Conclusions:
Of 183 second opinions seen over 20 months, the second opinion surgeon documented that previous spine surgeons recommended “unnecessary” (60.7%), the “wrong” (33.3%), or the “right” (6%) operations.
Keywords: First opinions, right, spine surgery, second opinions, unnecessary, wrong
INTRODUCTION
Increasingly, patients, spine surgeons, hospitals, and insurance carriers are not only questioning whether spinal operations are “unnecessary,” but also whether the “wrong” (e.g., overly extensive cervical or lumbar multilevel fusions, anterior vs. posterior surgery, etc.) or “right” (appropriate) operations are being recommended to patients. In a prior study in 2011, out of 274 patients seen as first and second opinions over a 14-month period, Epstein and Hood documented a 17.2% incidence of “unnecessary” spine surgery being previously offered by outside spine surgeons.[4] The term “unnecessary” was defined as operations being recommended for pain alone, without any neurological deficit or significant radiographic finding.[4] Although that preliminary series did not distinguish between first and second opinions, it was, nevertheless, anticipated that the real frequency of “unnecessary” spinal surgery was substantially higher (e.g., at least 30%). In 2012, over a 14-month period, Gamache determined that 69 (44.5%) of 155 patients presenting for second opinions, were told that they needed surgery by other spine surgeons, but he did not recommend those operations.[5] In this follow-up prospective study, 437 patients presenting for both first and second spinal consultations were carefully assessed. Those coming in for first opinions were told whether or not they required surgery. Patients who were previously told by outside spine surgeons that they needed surgery, were put into three categories based on the second opinion surgeon's (author's) assessment; “unnecessary,” the “wrong” surgery (e.g., overly extensive, anterior vs. posterior operations), or the “right” (appropriate) surgery.
MATERIALS AND METHODS
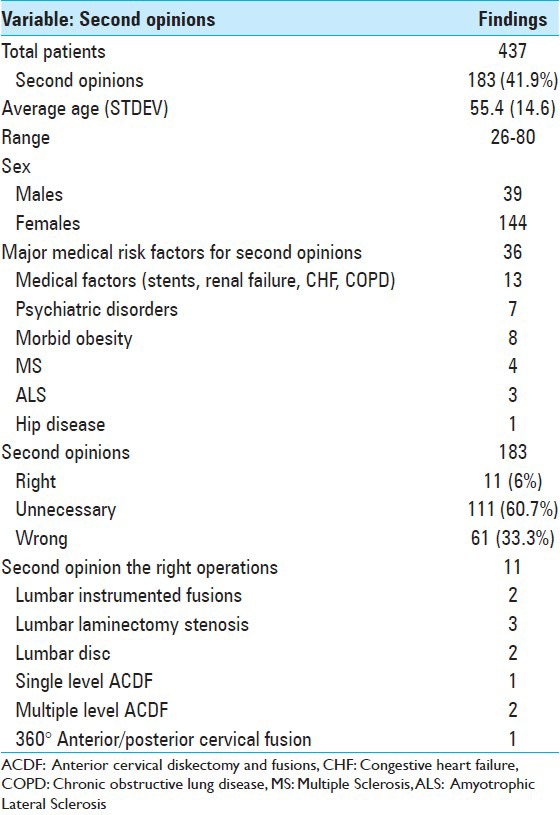
Prospectively, over a 20-month period, 437 patients with cervical or lumbar complaints were seen in first (254 = 58.1%) or second (183 = 41.9%) neurosurgical spinal opinion [Tables 1–3]. The author determined how many of the first opinion patients, averaging 57.5 years of age would benefit from surgery [Table 1]. Of the 183 patients seen in second opinion, who were previously told by outside surgeons that they needed spinal surgery (averaging 55.4 years of age), the second opinion surgeon (author) determined whether the recommended operations were deemed “unnecessary,” “wrong,” or “right” [Tables 2 and 3]. “Unnecessary” operations were defined as those recommended for pain alone, without focal neurological deficits, or significant radiographic abnormalities. The “wrong” operations were defined as those that were considered overly extensive (e.g., too many levels anterior, posterior, or circumferential) or performed from the wrong access route (e.g., anterior vs. posterior vs. circumferential). The “right” operation was considered the “appropriate,” meaning the prior and second opinion surgeon (author) agreed on the necessity, extent, and approach for surgical intervention.
Table 1.
Summary of clinical data for first opinions
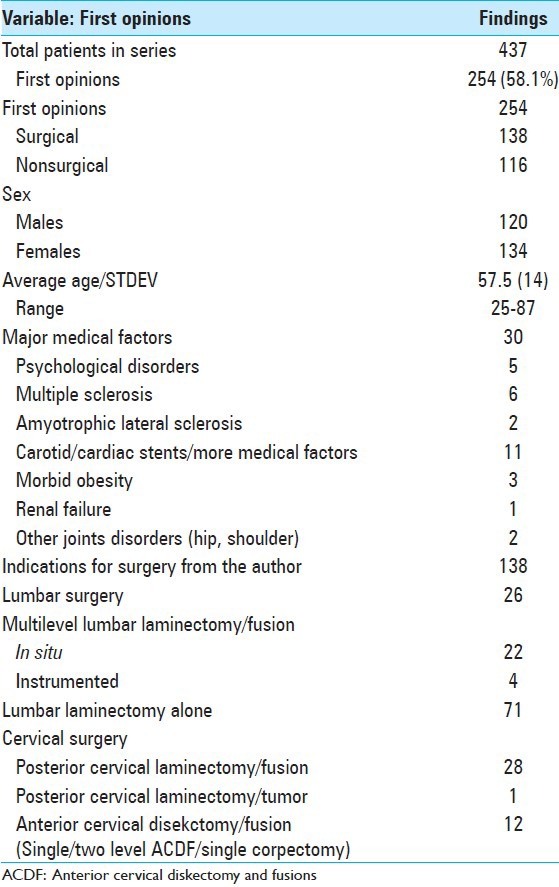
Table 3.
Second spinal surgical opinions: “Unnecessary” or “Wrong”
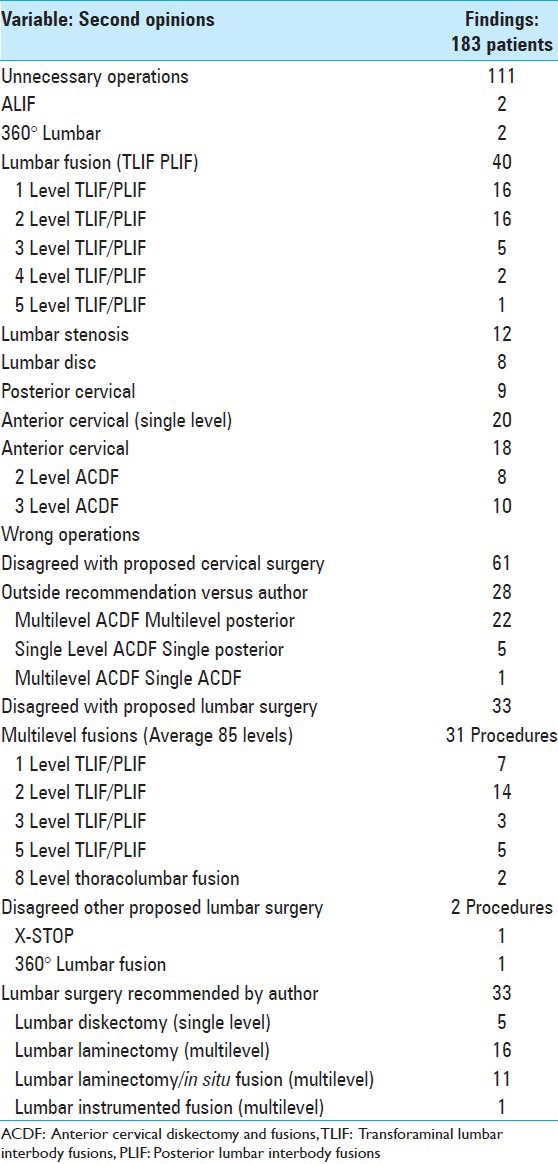
Table 2.
Clinical data for second opinions and “Right” operations
RESULTS
First opinion
Of the 254 patients seen in first opinion, 138 (54.3%) presented with surgical disease, while 116 (45.7%) had no surgical pathology [Table 1]. The recommended surgeries included 26 lumbar laminectomies with fusions (noninstrumented 22, instrumented 4), 71 lumbar laminectomies (multilevel stenosis and/or disc), 28 cervical laminectomies/fusions, 1 tumor resection, and 12 anterior cervical procedures [Table 1].
Major medical comorbid factors for 254 first opinion patients
Thirty major medical comorbidites were identified in the 254 patients; 11 had coronary/carotid stents, 5 had major psychological problems, and 3 were morbidly obese, 1 had renal failure and 2 had other joint disorders. Additional neurological diseases included Multiple Sclerosis (MS) in six patients and Amyotrophic Lateral Sclerosis (ALS) in two patients (one particular referring neurologist specialized in these diseases accounting for this unusual number).
Second opinions
There were 183 patients seen in second opinion who were previously told by outside surgeons that they needed spinal operations. The second opinion surgeon (author) determined that these operations were “unnecessary” in 111 patients (60.7%), the “wrong” operation in 61 patients (33.3%), or the “right” operation in 11 patients (6%) [Tables 2 and 3].
“Unnecessary” surgery recommended in 111 patients
For 111 (60.7%) of the 183 second opinion patients, the second opinion surgeon found these operations were both “unnecessary” and often too extensive [Table 3]. They ranged from 8 lumbar diskectomies and 12 multilevel laminectomies to 40 often multilevel (1-5 level) transforaminal lumbar interbody fusions (TLIF) or posterior lumbar interbody fusions (PLIF) [Table 3]. “Unnecessary” cervical procedures included 20 single level anterior cervical diskectomy and fusions (ACDFs), 18 multilevel ACDFs (typically 2-3 level procedures), and 9 multilevel posterior cervical decompressions/fusions [Table 3].
“Wrong” cervical and lumbar spinal operations recommended by prior spinal surgeons
In 61 of the 183 second opinion cases, the second opinion surgeon determined that the outside surgeon had recommended the “wrong” and typically too extensive operations [Table 3]. Twenty-two of the 28 “wrong” and too extensive cervical operations included multilevel anterior cervical procedures over 2-5 levels; these should/could have been multilevel posterior procedures. One example was a 70-year-old obese male (Body Mass Index [BMI] of 36.9) who presented with a severe progressive myelopathy (Nurick Grade IV/V). A neurosurgeon, not a spine surgeon, recommended, based on magnetic resonance imaging (MRI) alone, a C3-4 and C4-5 ACDF. However, when the second opinion spine surgeon performed a Computed Tomography (CT) scan suspecting the presence of OPLL, indeed it demonstrated marked continuous OPLL extending behind the C3 and C4 vertebrae, involving/crossing the C3/C4 and C4/C5 disc spaces (e.g., there were no soft cervical discs). Furthermore, the “double layer sign” on CT indicated that OPLL had likely extended through the dura, and an anterior approach would have significantly risked a cerebrospinal fluid (CSF) fistula. Since the patient had a massive chin, very short neck, an excellent cervical lordotic curvature, and OPLL on CT with a “double layer sign” of OPLL likely extending through the dura (increasing the risk of a CSF fistula), a cervical laminectomy of C3 and C4 with posterior C2-C5/C6 fusion was recommended and performed. The surgery resulted in full resolution of the patient's preoperative myelopathic deficit, and the postoperative MRI demonstrated adequate dorsal cord migration/decompression with resolution of the previously noted high T2 weighted intrinsic cord signal at the C3/C4 level.
Additionally, outside surgeons recommended single level ACDF for 5 of the 28 cervical cases; these should/could have been posterior diskectomies (single-level unilateral laminotomies, as all pathology was very lateral/foraminal). An example of this was a 55-year-old female (BMI of 32) with a unilateral C8 radiculopathy and MRI scan showing a foraminal C7-T1 disc herniation. She had been offered a C7-T1 ACDF. This was the wrong operation for several reasons; first, the original MRI and corroborative CT confirmed that the pathology was purely foraminal, (e.g., no anterior/anterolateral cord/root compression). Second, an anterior approach with the patient's large body habitus would have been challenging (e.g., likely requiring removal of the manubrium). Third, an ACDF at C7-T1 may have missed the focal and very foraminal pathology altogether.
One final patient of the 28 offered cervical surgery was told to undergo a multilevel ACDF; this should/could have been a single-level ACDF.
In the lumbar spine, outside surgeons’ overwhelmingly recommended 33 “wrong” procedures that were also typically too extensive. Twenty-nine patients were told to undergo 1-5 level TLIF and PLIF. Another two patients were offered eight-level thoracolumbar fusions. Of the remaining two patients, one was advised to undergo an X-STOP, while another was told to undergo a 360° lumbar fusion [Table 3]. Alternatively, the second opinion surgeon (author) recommended; 1 instrumented lumbar fusion, 5 lumbar diskectomies, 16 multilevel lumbar laminectomies, and 11 multilevel laminectomies with in situ fusions [Table 3].
Agreement with 11 second surgical opinions
Eleven of the 183 second opinion patients, who were told they needed surgery by outside spine surgeons, needed, according to the second opinion surgeon (author) precisely the operations recommended. In the lumbar spine these operations included: Two laminectomies/instrumented fusions, three posterior decompressions (stenosis), and two lumbar diskectomies. In the cervical spine these included: One single level ACDF, two multilevel ACDF, and one 360° circumferential cervical procedure.
Medical comorbid factors in patients presenting for second opinions
In the 183 patients seen for second opinion, major comorbidities were identified in 36 (19.7%) patients. The most prominent factors included: 13 instances of major medical risk factors (e.g., cardiac/carotid stents, congestive heart failure (CHF), chronic obstructive lung disease (COPD), and renal failure), 7 psychological disorders, 8 patients with morbid obesity, 4 with MS, and 3 with ALS (again note that the high incidence of MS and ALS was largely attributed to the referral pattern from neurologists specializing in these diseases).
DISCUSSION
Increased frequency of cervical and lumbar surgery in the US
Utilizing the annual National Hospital Discharge Survey of hospitalizations in the US from 1979 to 1990, Davis found that the frequency of hospitalizations for cervical spine surgery increased by over 45% (cervical fusions by > 70%), and for lumbar spine surgery increased by over 33% (exploration/decompression > 65%, lumbar fusions > 60%).[3]
From 1978 to 1985, McGuire et al. also observed that the hospitalization rates for lower back surgery increased by over 20% in the US.[6] In Iowa, the likelihood that patients insured by Blue Cross/Blue Shield (BCBS) would undergo spinal surgery positively correlated with the following variables; female gender, age over 44 years, hospitals with occupancy rates under 62%, hospitals with < 774 staff members, hospitals with < 267 beds, and without residency training programs.
When Nilasena et al. utilized Utah's Medicare (1984-1990) database to look at the frequency of spinal surgery for mechanical low back pain, Utah's laminectomy and discectomy rates were at least 20% over the US average, and increased over the 6-year study period by 55% (mostly due to surgery for spinal stenosis).[7] Interestingly, the frequency of spinal operations differed by as much as 50% among different areas within the state of Utah itself, but there was “no significant correlation between the number of surgeons performing back surgery and the rate of surgery.”
Second opinion surgeon in 2011: 17.2% rate of “unnecessary” spine surgery
In 2011, Epstein and Hood prospectively evaluated 274 patients with cervical or lumbar complaints who were seen as first or second opinions over a one year period; at least 17.2% of patients were told by prior spine surgeons that they needed spinal operations that the second opinion surgeon (author) determined were “unnecessary” and often very extensive.[4] For cervical complaints, 21 (23.1%) of 91 were told they needed 1-4 level anterior diskectomy/fusion (18 patients), laminectomies/fusions (2 patients), and a posterior cervical diskectomy (1 patient). For lumbar complaints, 26 (14.2%) of 183 were told they needed; single/multilevel PLIFs: 1-level (13 patients), 2-levels (7 patients), 3-levels (3 patients), 4-levels (2 patients), and 5-levels (1 patient).
In 2012 spine surgeon sees no need for surgery in 44.5% of second opinions
Subsequently in 2012, over a 14-month period, Gamache prospectively evaluated 240 consecutive patients seeking first (85 or 35%) or secondary (155 or 65%) opinions regarding the need for spine surgery.[5] Of 85 first opinion patients, referred by primary care doctors or neurologists due to MRI or CT reports indicating the presence of surgical lesions, he recommended no surgery in 37 (43%) patients. More critically, of the 155 patients coming in for second to fourth surgical opinions, where one or more previous surgeons recommended operations, he advised no surgery in 69 (44.5%) patients.
New study documents high incidence of “unnecessary” and “wrong” surgery
In this new study of 437 patients seen over a 20-month period, the numbers seen in first and second opinion for cervical or lumbar complaints were carefully quantitated [Tables 1–3]. Of the patients seen in first opinion in this series, 116 (45.7%) had no surgical pathology. Interestingly, this figure was quite similar to Gamache's observation that 37/85 (43%) first opinion patients also did not warrant surgery [Table 1].[5] More critically in this study, for patients told by outside surgeons that they needed operations, the second opinion surgeon (author) found that 111 (60.7%) of 183 patinents were told they needed “unnecessary” surgery. In Gamache's study, he found a somewhat lower 69/155 (44.5%) incidence of second opinion patients (e.g., who were previously told by outside surgeons they needed operations) who did not in his opinion, require surgery.[5]
What was new in this study was the further exploration of how often outside surgeons recommended the “wrong” (e.g., overly extensive or anatomic approach) operations for truly surgical lesions; indeed, 61 (33.3%) patients in this series, according to the second opinion surgeon (author) were told that they needed the “wrong” operations. The overly extensive procedures included the 29 TLIF/PLIF, 2 eight-level thoracolumbar fusions, one X-STOP, and one 360° fusion, while the “wrong approach” procedures predominated in the cervical spine [Table 3]. Of interest, only 11 (6%) of the 183 second opinion patients were told to have the “right” operations; these included single to multilevel ACDF, a circumferential cervical procedure, lumbar diskectomies/laminectomies (disc/stenosis), 2 instrumented lumbar fusions [Table 2].
One study documented “unnecessary” repeated spine fusions for failed backs
Arts et al. showed that of 82 patients undergoing additional spinal fusions for failed back surgery (e.g., persistent chronic low-back pain and/or leg pain lasting more than 1 year, despite one or more surgical procedures), 65% had unsuccessful outcomes or had “unnecessary” spinal operations.[1] Utilizing multiple outcome scores over an average of 15 postoperative months, they found mostly poor results from repeated fusions, and, therefore, recommended more careful patient selection to prevent future “unnecessary” spinal fusions, and promote the use of more nonsurgical measures.
Three studies showed “unnecessary” testing related to spinal surgery
Three studies found “unnecessary” testing for patients having spinal surgery.[2,8,9] First, Bohl et al. determined that when adequate intraoperative films were obtained following ACDF (plates/screws), it was “unnecessary” to acquire second X-rays in the postanesthesia care unit (PACU); the latter led to often inferior studies, no additional diagnosis of surgical problems, wasted time/cost, and “unnecessary” patient exposure to radiation.[2] Second, when Srinivas et al. initiated the National Physicians Alliance for “Promoting Good Stewardship in Clinical Practice,” they recommended no imaging for spine patients with 6 weeks or less of clinical complaints “unless red flags were present.”[9] Potential “harms” of early testing included; “labeling” patients (e.g., with spinal disease where most likely no real pathology was present), subjecting patients to more “unnecessary” testing or “unnecessary” surgery, and increased cost.[9] Third, O’Grady et al. confirmed that there was no value in performing routine preoperative blood tests for healthy patients undergoing spinal surgery; 95% of the total cost of these studies resulted in normal findings, and even the most abnormal results were nearly normal, and did not impact patient care.[8]
Limitations
The major limitation of this study was the “subjective” determination by one spine surgeon, a neurosurgeon, that prior spine surgeons’ recommendations for surgery were “unnecessary,” “wrong,” or “right.” Although some spine surgeons will argue operating for pain alone without corresponding neurological deficits or significant radiographic abnormalities is appropriate, many more will agree that these procedures are indeed “unnecessary.” Similarly, some may argue that operations should not be labeled “wrong” or “right,” but are just “differences in opinion.” However, judgment, experience, and training should play a significant role in better defining what is optimally accepted as the norm. Despite these limitations, the aim of this study was to focus spine surgeons’ attention on what is happening in spine surgery, specifically the “unnecessary” and “wrong” operations that are often recommended without sufficient clinical support.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/6/353/120774
Disclaimer: The authors of this article has no conflict of interest to disclose, and have adhered to SNI's policies regarding human/animal rights, and informed consent. Advertisers in SNI did not ask for, nor did they receive access to this article prior to publication.
REFERENCES
- 1.Arts MP, Kols NI, Onderwater SM, Peul WC. Clinical outcome of instrumented fusion for the treatment of failed back surgery syndrome: A case series of 100 patients. Acta Neurochir (Wien) 2012;154:1213–7. doi: 10.1007/s00701-012-1380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohl DD, Telles CJ, Hustedt JW, Blizzard DJ, Carlson EJ, Grauer JN. Postanesthesia care unit imaging is unnecessary when intraoperative imaging is used during anterior cervical decompression and fusion procedures. J Spinal Disord Tech. 2012;25:E174–7. doi: 10.1097/BSD.0b013e31825d99f6. [DOI] [PubMed] [Google Scholar]
- 3.Davis H. Increasing rates of cervical and lumbar spine surgery in the United States, 1979-1990. Spine. 1994;19:1117–23. doi: 10.1097/00007632-199405001-00003. [DOI] [PubMed] [Google Scholar]
- 4.Epstein NE, Hood DC. “Unnecessary” spinal surgery: A prospective 1-year study of one surgeon's experience. Surg Neurol Int. 2011;2:83. doi: 10.4103/2152-7806.82249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gamache FW. The value of “another” opinion for spinal surgery: A prospective 14-month study of one surgeon's experience. Surg Neurol Int. 2012;3(Suppl 5):S350–4. doi: 10.4103/2152-7806.103867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGuire SM, Phillips KT, Weinstein JN. Factors that affect surgical rates in Iowa. Spine. 1994;19:2038–40. doi: 10.1097/00007632-199409150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Nilasena DS, Vaughn RJ, Mori M, Lyon JL. Surgical trends in the treatment of disease of the lumbar spine in Utah's Medicare population, 1984-1990. Med Care. 1995;33:585–97. doi: 10.1097/00005650-199506000-00002. [DOI] [PubMed] [Google Scholar]
- 8.O’Grady I, McCarthy C, Kaliaperumal C, Marks JC, Kaar G, O’Sullivan M. Are we justified in doing blood tests ‘routinely’ for all neurosurgical patients? Ir Med J. 2013;106:18–20. [PubMed] [Google Scholar]
- 9.Srinivas SV, Deyo RA, Berger ZD. Application of “less is more” to low back pain. Arch Intern Med. 2012;172:1016–20. doi: 10.1001/archinternmed.2012.1838. [DOI] [PubMed] [Google Scholar]


