Abstract
Diabetes mellitus (DM) has assumed epidemic proportions and as a consequence, diabetic retinopathy is expected to be a major societal problem across the world. Diabetic retinopathy (DR) affects the vision by way of proliferative disease that results in vitreous hemorrhage and traction retinal detachment or by way of diabetic maculopathy (DME). The present-day management of diabetic retinopathy revolves around screening the diabetics for evidence of retinopathy and treating the retinopathy with laser photocoagulation. DME is treated with laser photocoagulation and/or intra- vitreal injection of anti-vascular endothelial growth factor (VEGF) agents or steroids. Laser remains the mainstay of treatment and is potentially destructive. Systemic management aims at preventing or delaying the onset of retinopathy; reversing the early retinopathy; or delaying the progression of established retinopathy. Evidence from multiple studies has confirmed the protective role of rigid control of blood glucose and blood pressure. The evidence for lipid control versus maculopathy was less definitive. However, the use of fenofibrates (originally used for lowering serum lipids) has shown a benefit on both proliferative disease and maculopathy outside their lipid-lowering effect. Other drugs being tried are the Protein Kinase C (PKC) inhibitors, other peroxisome proliferator-activated receptors (PPAR) agonists, Forsoklin (which binds GLUT 1 receptor), minocycline (for its anti inflammatory effect), and Celecoxib (Cox-2 inhibitor).
Keywords: Diabetic Retinopathy, Diabetic Maculopathy, Dyslipidemia, Fenofibrates, Hypertension, Systemic Management
INTRODUCTION
The World Health Organization estimates the prevalence of diabetes worldwide across all age groups at 4.4% in year 2030 - an increase by about 1.6% from the year 2000.[1] This should amount to an increase from 171 million to about 366 millions in actual numbers.
Diabetic retinopathy (DR) affects 1 in 3 persons with diabetes and is the leading cause of vision loss in adult persons of working age. Patients with DR have been reported to have poorer quality of life reduced physical, emotional and social wellbeing, and to utilize more healthcare resources.[2]
In the US, among the adults 40 years or older with diabetes mellitus, the prevalence of DR has been estimated at 40.3% and that of vision-threatening retinopathy, which includes diabetic macular edema (DME), is estimated at 8.2%.[3] Globally, it has been estimated that up to 100 million people have DR and more than 20 million will have vision-threatening retinopathy.[4]
The present-day management of DR revolves around laser photocoagulation for proliferative disease; laser photocoagulation, intra-vitreal anti-vascular endothelial growth factor (VEGF) agents and steroids for DME. Vitreo retinal surgery is reserved for the more serious complications such as vitreous hemorrhage, traction and combined retinal detachment, premacular vitreoretinal traction.[5]
While most agree that microvascular changes including DR are duration dependent to a great degree, there are obviously other factors that influence the onset and progression of the retinopathy. In this regard, many ocular treatments are indicated only when retinopathy has set in, and is akin to “fire fighting”. Laser photocoagulation, for example, remains the first and often repeated modality of treatment in most countries; unfortunately this modality is destructive in nature and leads to variable loss of peripheral field in an attempt to preserve some central vision.
Thus, systemic therapy could be preventive and hence potentially could have more impact on the overall public health outcome for the society at large.[6] Systemic approaches to treatment are aimed at preventing retinopathy, delaying the onset of retinopathy, reversing retinopathy (in some cases), or delaying the progression of early to advanced stages of retinopathy.
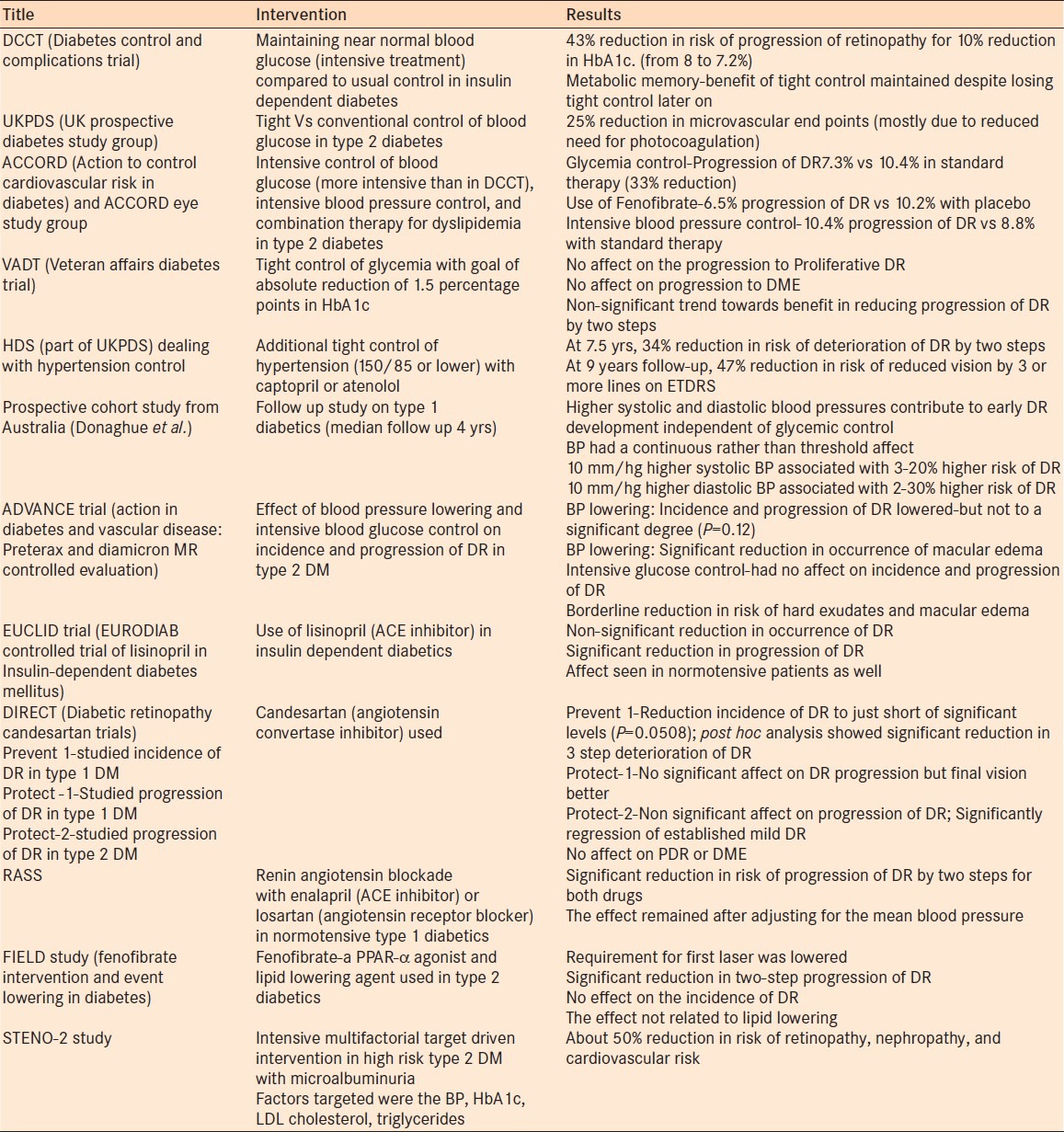
In this article we discuss some of the current concepts related to systemic therapy in diabetic retinopathy using the evidence from various clinical trials [Table 1].
Table 1.
Indications for PPV in diabetic macular edema
Glycemic control
Considering the fact that diabetes is primarily defined by raised blood glucose levels, it makes logical sense that good glycemic control should have beneficial effect on secondary effects of diabetes including microvascular complications and retinopathy.
The evidence
Two major trials- the Diabetes control and complications trial (DCCT)[7] involving insulin-dependent diabetics and the United Kingdom prospective diabetes study group (UKPDS)[8] involving non-insulin-dependent diabetics have answered the question in the affirmative. The DCCT has shown that a 10% reduction in HbA1c (e.g., 8-7.2%) is associated with a 43% reduction in progression of retinopathy in the intensive treatment group and 45% reduction in progression of retinopathy in the conventional treatment group- indicating that it is ultimately the control of blood glucose that is important. The study also showed that both the levels of HbA1c at start of the trial as well as the level achieved during the trial influenced the rate of progression of retinopathy. However, significantly the intensive treatment group had more incidence of hypoglycemic episodes. Follow-up studies on this group of patients have shown that the benefit of tight control on the progression of retinopathy was maintained, despite reducing difference in the values of HbA1c between the groups over time- a concept of “metabolic memory”.[9]
The UKPDS[8] studied similar tight control versus conventional control for type 2 diabetes. After 6 years of follow-up, the intensive treatment group had significantly smaller rate of the two-step progression of diabetic retinopathy (even if need for photocoagulation was excluded).
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial was designed primarily to study the affect of even more intensive glycemic control (than DCCT) on cardiovascular and microvascular events in patients with type 2 diabetes. The ACCORD eye study group has found a 33% reduction in the progression of DR in the intensive control group after a short period of 4 years.[10]
In contrast, the Veterans affairs diabetes study did not show any significant difference in the progression of microvascular changes after tight control of glycemia. Specifically, the study noted that the incidence of new ocular procedures; conversion to proliferative disease; and occurrence of macular edema were similar in both the groups while a non-significant beneficial trend was noted in terms of two-step progression of the retinopathy.[11]
Most reports mention halted or delayed progress of retinopathy but not reversal of established retinopathy. Very early retinal changes (such as increased fluorescein leak on vitreous fluorometry) has been shown to get reversed with intense glycemic control.[12]
An important issue to note is that tight control of blood glucose has been reported to cause early worsening of diabetic retinopathy and this has been attributed to up regulation of insulin-like growth factor-1 (IGF-1).[13,14,15] There are also case reports of rapid progression to florid retinopathy in insulin-dependent young diabetics, when put on intensive control of glycemia with continuous subcutaneous insulin infusion.[16] However, these patients also had significant other co-existing problems such as severe nephropathy. The ACCORD trial has shown increased risk of hypoglycemic episodes requiring medical assistance in the group with intensive treatment (aiming at >6% HbA1c). There was also increased rate of death from any cause in the group with intensive treatment -5% versus 4% in the conventional treatment.[10]
The inference
From a clinical practice perspective, it is perhaps impossible to replicate on a daily basis, the rigorous regimen of blood glucose control practiced in DCCT, ACCORD, and other trials. The message, however, is clear: better glucose control is associated with less risk of progression of DR. Good glycemic control right from diagnosis is beneficial in preventing the onset of diabetic retinopathy as well as in delaying the progression of the retinopathy. A ‘good’ control of glycemia is aimed at but not necessarily below normalcy. The long-term benefits of good control of glycemia outweigh the small risk of early worsening of retinopathy.
Control of hypertension
Hypertension is very often coexistent with diabetes. In a review publication by Mohan et al., the incidence of hypertension among type 2 diabetics was quoted at 20.6% in India, 78.4% in Thailand, 9.7% in Nigeria and 70.4% in Morocco.[17] Other studies have reported a three times greater incidence of hypertension among type 2 diabetics compared to age and sex-matched population without diabetes. Considering the known vascular damage that occurs with hypertension, there is expected to be additive affect of hypertension on the severity of diabetic retinopathy.
The evidence
The UKPDS studied the role of tight control of blood pressure on various end points - one of which is the retinopathy and visual loss.[18] There was a 35% reduction in the progression of retinopathy by 2 or more steps in the group with tight control of blood pressure. At 9 years follow-up, the group with tight control of blood pressure had a 47% reduction in risk of loss of 3 or more lines of vision (on ETDRS chart). Control of hypertension was also shown to have beneficiary affect on other end points such as myocardial infarction, stroke, renal failure, etc., In a prospective cohort study, Gallego et al. have identified systolic and diastolic pressure as predictors for onset of diabetic retinopathy in type 1 diabetes.[19] The association was found to be linear- an increase by 10 mm/hg in systolic blood pressure was associated with 3-20% increased risk of retinopathy and an increase by 10 mm/hg in diastolic blood pressure increased the risk by 2-30%.
In contrast to glucose control, follow-up studies on this group of patients have shown that the benefit of tight blood pressure control on the progression of retinopathy was not maintained over time; thus, blood pressure control has to be sustained throughout life.[20]
The Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation trial (ADVANCE) used perindopril-indapamide combination versus placebo for control of blood pressure in addition to glycemic control. The study, however, has shown only marginal benefit on the onset or progression of retinopathy with the pressure-lowering drugs.[21] The reduction in occurrence of macular edema was more significant.
The role of the renin-angiotensin system in the pathogenesis of DR has been of increasing interest. A local renin-angiotensin system has been identified to be functional in the eye and has been found to be upregulated during DR resulting in increased VEGF and other growth factors. Hence blockade of this system appears to be a logical approach to control the progression of retinopathy. Lisinopril, an angiotensin convertase enzyme (ACE) inhibitor, has been used in the EURODIAB trial (EUCLID Controlled trial of Lisinopril in Insulin-Dependent Diabetes Mellitus) and has been shown to have non-significant reduction in the occurrence of retinopathy (although not a primary end point) and significant reduction in progression of retinopathy.[22] This benefit on progression of retinopathy was noted even in normotensive patients with type 1 diabetes. This raises the possibility of direct effect of this drug on the retinopathy, outside of its blood pressure-lowering affects.
The DIRECT study is a large trial conducted to test the efficacy of Candesartan (an angiotensin receptor blocker) on diabetic retinopathy. The study had three components. The prevent-1 that studied the role of this drug in preventing diabetic retinopathy in type 1 diabetics and Protect-1 and Protect-2 that studied the effect of the drug in halting the progression of diabetic retinopathy in type 1 and type 2 diabetes, respectively.[23,24] Treatment with Candesartan was able to reduce the incidence of retinopathy by 18% (a marginally significant achievement P = 0.0508). Progression of retinopathy could not be influenced to a significant degree in both type 1 and type 2 diabetes. However, regression (reduction by 2 steps) of early stage retinopathy was achieved to a significant degree in type 2 diabetes. In general, it is believed that the treatment has reduced the retinopathy to a less severe variety more often than in the placebo group.
Yet another study- the Renin Angiotensin System Study (RASS) was designed to primarily study the occurrence of diabetic nephropathy, with retinopathy as additional end point. The study compared ACE inhibitor Enalapril or Angiotensin II receptor blocker Losartan with a placebo. Progression of retinopathy was significantly less with the both medications compared to placebo even when adjusted for blood pressure-lowering affect of the drugs.[25] The study has also demonstrated that the night ambulatory diastolic blood pressure is associated with increasing severity of diabetic retinopathy and this was attributed to the dysfunctional autonomic system in diabetics. The authors believe that the protective effect of ACE inhibitors and Angiotensin II receptor blockers could be due to the affect on the night time blood pressure rather than a direct affect on the rennin-angiotensin system in the eye.[26]
The inference
Control of blood pressure, along with good glycemic control, reduces the risk of progression of retinopathy. Furthermore, inhibition of the rennin-angiotensin pathway by an ACE inhibitor or angiotensin II receptor blocker seem to have effects beyond the impact of blood pressure control.
Control of dyslipidemia
The association between lipids and DR has been less well demonstrated compared to the role of hyperglycemia and hypertension.[27]
The evidence
The Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) has not shown any association of cholesterol levels with the severity of DR but showed significant association with severity and occurrence of hard exudates in young diabetics.[28] The ETDRS study found a two-fold increase in risk of retinal hard exudates with increased levels of cholesterol.[29] High serum triglycerides have also been shown to be associated with increased risk of development and progression of retinopathy by Hadjadj et al.[30] The DCCT has shown significant association between occurrence of clinically significant macular edema and levels of LDL as well as total cholesterol- HDL ratio.[31] Low levels of HDL cholesterol have been known to be a risk factor for cardiovascular disease but the ADVANCE study did not show similar relationship between low levels of HDL cholesterol and retinopathy although there was a relationship with nephropathy.[32]
The statins and the fibrates have been in use clinically to reduce the lipid levels. Statins primarily reduce the LDL cholesterol. Gupta et al. had a good success with use of atorvastatin in the reduction of diabetic macular edema.[33] Reduction in hard exudates was noted in as high as 66.6% cases with statins versus only 13.3% in control group. In a study by Gordon et al. of six patients, reduction in hard exudates was achieved with pravastatin along with reduction in total cholesterol and low-density lipoproteins.[34]
Peroxisome proliferator-activated receptors agonists
Peroxisome proliferator-activated receptors (PPAR) belong to a large super family of nuclear receptors.[35] These are ligand inducible transcription factors and serve as receptors for thyroid hormones, steroids, etc., They regulate the genes involved in carbohydrate and lipid metabolism and hence affect the insulin sensitivity and lipid homeostasis.[36] PPAR-α and γ are specifically of importance for this discussion. Drugs such as rosiglitazone, pioglitazone belonging to the group of thiazolidendiones are agonists of PPAR-γ and have serum glucose-lowering ability.[37] The fibrates are agonists of PPAR-α and have predominantly lipid-lowering function. Drugs such as Muralglitazar have dual (α/γ receptor agonists) affect and are expected to be even better since they have affect on lipid control as well as improving insulin sensitivity.[38]
PPAR-γ agonists are also suggested to have anti-inflammatory role since they have been shown to reduce the inflammatory markers such as serum C-reactive protein, IL-6, plasminogen activator-1, etc.[39]
Fenofibrates and diabetic retinopathy
Fibrates are PPAR- α agonists and have been extensively tested for diabetes and retinopathy.[40,41] The FIELD study (Fenofibrate Intervention and Event Lowering in Diabetes) is essentially a cardiovascular trial. However, the effect on reduction of myocardial infarction and coronary death was not found to be significant. There was beneficial effect on overall cardiovascular events. Study of diabetic retinopathy was actually a tertiary end-point, but showed a significant result. The need for first as well as repeat laser treatment for proliferative retinopathy and macular edema was significantly reduced with use of fenofibrate compared to placebo. A sub-study of 1012 patients who had baseline and follow-up fundus photographs was also carried out. This analysis revealed a markedly significant reduction in the need for laser photocoagulation, and also showed a significant reduction in 2-step progression of retinopathy. Incidence of macular edema showed non-significant trend toward reduction.
The mechanism by which fibrates achieved this beneficial effect on the retinopathy is, however, unclear. While lipid lowering is the identified primary action of fibrates, the actual levels of lipid lowering achieved in the study was not significant over time (although at 4 months there was significant reduction). The benefit on diabetic retinopathy progression was achieved against the backdrop of use of ACE inhibitors in both groups, as well as more use of statins in the placebo group over time.[42]
The ACCORD study also showed beneficial effect of fenofibrates. When added to statins, they significantly slowed the progression of diabetic retinopathy in type 2 diabetes mellitus.[10] Some of the mechanisms by which fenofibrates probably act are listed below.
Inhibitory affect on the VEGF pathway.[43]
Regulation of retinal endothelial cell survival and prevention of apoptotic death[44]
Anti-inflammatory effect: There is enough evidence that inflammation plays a role in the pathogenesis of DR.[45] The vitreous of PDR patients has been demonstrated to have elevated levels of proinflammatory cytokines, such as Interleukins- IL-1β, IL-6 and IL-8; TNF-α and vascular cell adhesion molecule-1.[46,47,48] Increased VEGF and IL-6 levels were also detected in the aqueous humor of diabetic patients with macular edema.[49] Reduced concentrations of TNF-α, Interleukin-6, and interleukin-1β have been seen with fenofibrates.[40,50,51]
Antioxidant property: Fenofibrates were shown to reduce the concentrations of melondialdehyde- a lipidperoxide formed due to reactive oxygen species.[52]
Considering the evidence of benefit of fenofibrates in DR, Treacy et al. suggest the exploration of intraocular delivery of the same along with anti-VEGF drugs in the management of DR. Currently available fenofibrate (oral) is converted to the active form by esterases. Hence bioavailability becomes an issue if administered intravitreally. A choline salt (ABT-335) has been identified that does not need activation by esterases.[53] Hopefully the future should see the conversion of this possibility into reality.
The inference
Control of dyslipidemia, possibly with fenofibrate, reduces the risk of progression of retinopathy.[54]
Multifactoral intervention
Most previous trials targeted only a single risk factor for DR. The effect of a multifactorial approach was investigated in the Steno-2 study in patients with type 2 diabetes and microalbuminuria.[55,56] The Steno-2 study encompassed treatment goals similar to those recommended in the American Diabetes Association guidelines. After 7.8 years of intensive treatment, the study group achieved lower systolic and diastolic blood pressures, lower HbA (1c), lower fasting serum total and low-density lipoprotein cholesterol, lower fasting serum triglycerides, and lower 24- hour urine albumin excretion. As a percentage of total energy, fat intake was less and carbohydrate intake was more. This resulted in significant reduction in microvascular events including diabetic retinopathy by about 50%.[55]
The inference
A multifactorial approach, targeting control of hyperglycemia, blood pressure, and dyslipidemia will reduces the risk of onset and progression of DR.
Other approaches to systemic medication
Anti-platelet agents
These have been the first to be tried for DR with no proven efficacy. Aspirin, ticlopidine, and dipyridamole have been tried.[57,58]
PKC inhibitors
Activation of Protein kinase C has been shown to have a role to play in development and progression of diabetic retinopathy. Ruboxistaurin - a selective PKC inhibitor has been tried for DR as well as DME.[59,60,61] Although the study revealed some beneficial affect in moderate and severe diabetic retinopathy, the drug has not been approved by the USA-FDA pending further trials.
Suppression of GLUT1
GLUT1 transports glucose between blood and the retina. Inhibiting the same by intra-ocular injection of siRNAs that inhibit the mRNA (that codes for GLUT) has been shown to reduce the retinal glucose levels.[62] Forskolin (which binds to GLUT1) when administered systemically has been shown to reduce retinal glucose levels in mice. Hence, GLUT1 can be a potential target for medical treatment- both locally and systemically.
Minocycline
A novel connection between bone marrow neuropathy, inflammation, and DR has been proposed.[63] Bone marrow neuropathy is supposed to increase the synthesis of inflammatory cells. This induces a sort of systemic inflammation that affects hypothalamus among other organs, and adversely affects the microvascular and macrovascular events. Minocycline (100 mgs twice a day)- a well-tolerated anti-inflammatory agent has been shown to have some benefit in improving visual acuity in type 2 diabetics with morbid obesity. In a pilot study of five patients with DME, Cukras et al. have found significant reduction in central macular thickness and improvement in vision.[64]
Rosiglitazone
As alluded to above, PPAR- γ agonist Rosiglitazone is primarily used for better control of diabetes. 65 Shen et al. have shown a 59% reduction in progression to proliferative DR from severe non-proliferative DR (47.4% vs 19.2%) with use of this drug over a 3-year period. 66 However, DME has been reported as a complication of use of this drug as well as with Pioglitazone.[67,68,69] However, Tatti et al. did not find any increased incidence of DME in patients being treated with Rosiglitazone.[70]
Celecoxib
Celecoxib is a Cyclo-oxygenase-2 (COX-2) inhibitor. Since COX-2 has been shown to upregulated in DR, inhibiting the same was thought to have benefit in DR. However, a placebo-controlled trial of Oral Celecoxib (200 mgs twice a day) has failed show any beneficial effect on the DME. Some decrease in fluorescein leakage was noticed.[71]
Adenosine receptor agonists or adenosine reuptake inhibitors
Adenosine has been shown to have anti-inflammatory affect. However, systemic administration of adenosine has severe side effects of hypotension, bradycardia, and sedation. Hence, agents that can inhibit its uptake or which mimic its action could be potential drugs for treatment of DR. This approach is at a concept level.[72]
Other agents that are under trial are canakinumab, a human anti-interleukin β monoclonal antibody (administered subcutaneously), Darapladib - a selective lipoprotein-associated phospholipase A2 inhibitor (administered orally) and Darbepoetin alpha (recombinant erythropoietin).
CONCLUSIONS
The present day treatment of established diabetic retinopathy mainly involves laser photocoagulation, which is basically a destructive treatment. Preventing the onset of DR or delaying the progression of DR can go a long way in preserving good vision and avoiding the laser photocoagulation. Normalizing the blood glucose levels, rigid control of blood pressure, reduction in LDL cholesterol by use of statins, use of fenofibrates and blockade of renin angiotensin system have all shown some benefit in the occurrence or progression of DR. The concept of multifactorial approach to simultaneously target each of the important issues that face a diabetic seem to be important since the cumulative benefit is very significant. The challenge is in implementing the study regimens in the general population so as to extract maximum mileage from the studies, in terms of reduction in societal burden of visual impairment caused by diabetes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes- Estimates for the year 2000 and projections for 2030. Diabetes care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36. doi: 10.1016/S0140-6736(09)62124-3. [DOI] [PubMed] [Google Scholar]
- 3.Kempen JH, O’Colmain BJ, Leske MC, Haffner SM, Klein R, Moss SE, et al. The prevalence of diabetic retinopathy among adults in United States. Arch ophthalmol. 2004;122:552–63. doi: 10.1001/archopht.122.4.552. [DOI] [PubMed] [Google Scholar]
- 4.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy- A systematic review. JAMA. 2007;298:902–16. doi: 10.1001/jama.298.8.902. [DOI] [PubMed] [Google Scholar]
- 6.Liew G, Mitchell P, Wong TY. Systemic mangament of diabetic retinopathy- New evidence from trials has implications for clinical practice. BMJ. 2009;338:612–3. [Google Scholar]
- 7.The relationship of glycemic exposure (HbA1C) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes. 1995;44:968–83. [PubMed] [Google Scholar]
- 8.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 9.Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. N Engl J Med. 2000;342:381–9. doi: 10.1056/NEJM200002103420603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The ACCORD Study Group; ACCORD Eye Study Group. Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, et al. Effects of Medical Therapies on Retinopathy Progression in Type 2 Diabetes. N Engl J Med. 2010;363:233–44. doi: 10.1056/NEJMoa1001288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in Veterans with type 2 Diabetes. N Engl J Med. 2009;360:130–9. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 12.White NH, Waltman SR, Krupin T, Santiago JV. Reversal of abnormalities in ocular fluorophotometry in insulin-dependent diabetes after 5-9 months of improved metabolic control. Diabetes. 1982;31:80–5. doi: 10.2337/diab.31.1.80. [DOI] [PubMed] [Google Scholar]
- 13.Chantelau E. Evidence that upregulation of serum IGF-1 concentration can trigger acceleration of diabetic retinopathy. Br J Opthalmol. 1998;82:725–30. doi: 10.1136/bjo.82.7.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chantelau E, Meyer-Schwickerath T. Reversion of ‘early worsening’ of diabetic retinopathy by deliberate restoration of poor metabolic control. Ophthalmologica. 2003;217:373–7. doi: 10.1159/000071355. [DOI] [PubMed] [Google Scholar]
- 15.Early worsening of diabetic retinopathy in the diabetes control and complications trial. Arch Ophthalmol. 1998;116:874–86. doi: 10.1001/archopht.116.7.874. [DOI] [PubMed] [Google Scholar]
- 16.Ballegooie VE, Hooymans JM, Timmerman Z, Reitsma WD, Sluiter WJ, Schweitzer NM, et al. Rapid deterioration of diabetic retinopathy during treatment with continuous subcutaneous insulin infusion. Diabetes Care. 1984;7:236–42. doi: 10.2337/diacare.7.3.236. [DOI] [PubMed] [Google Scholar]
- 17.Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in south ease asian and african regions: Need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013 doi: 10.1155/2013/409083. On line publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UK prospective diabetes study group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 19.Gallego PH, Craig ME, Hing S, Donaghue KC. Role of blood pressure in development of early retinopathy in adolescents with type 1 diabetes: Prospective cohort study. BMJ. 2008;337:a918. doi: 10.1136/bmj.a918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Longa term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359:1565–76. doi: 10.1056/NEJMoa0806359. [DOI] [PubMed] [Google Scholar]
- 21.Beulens JW, Patel A, Vingerling JR, Cruickshank JK, Hughes AD, Stanton A, et al. Effecs of blood pressure lowering and intensive glucose control on the incidence and progression of retinopathy in patients with type 2 diabetes mellitus: A randomized controlled trial. Diabetologia. 2009;52:2027–36. doi: 10.1007/s00125-009-1457-x. [DOI] [PubMed] [Google Scholar]
- 22.Chaturvedi N, Sjolie AK, Stephenson JM, Abrahamian H, Keipes M, Castellarin A, et al. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. The EUCLID Study Group. Lancet. 1998;351:28–31. doi: 10.1016/s0140-6736(97)06209-0. [DOI] [PubMed] [Google Scholar]
- 23.Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: Randomised, placebo-controlled trials. Lancet. 2008;372:1394–402. doi: 10.1016/S0140-6736(08)61412-9. [DOI] [PubMed] [Google Scholar]
- 24.Sjølie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): A randomised placebo-controlled trial. Lancet. 2008;372:1385–93. doi: 10.1016/S0140-6736(08)61411-7. [DOI] [PubMed] [Google Scholar]
- 25.Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A, Strand T, et al. Renal and Retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med. 2009;361:40–51. doi: 10.1056/NEJMoa0808400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klein R, Moss SE, Sinaiko AR, Zinman B, Gardiner R, Suissa S, et al. The relation of ambulatory blood pressure and pulse rate to retinopathy in type 1 diabetes mellitus. The Renin Angiotensin system study. Ophthalmology. 2006;113:2231–6. doi: 10.1016/j.ophtha.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Lim LS, Wong TY. Lipids and diabetic retinopathy. Expert Opin Biol Ther. 2012;12:93–105. doi: 10.1517/14712598.2012.641531. [DOI] [PubMed] [Google Scholar]
- 28.Klein BE, Moss SE, Klein R, Surawicz TS. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XIII. Relationship of serum cholesterol to retinopathy and hard exudate. Ophthalmology. 1991;98:1261–5. doi: 10.1016/s0161-6420(91)32145-6. [DOI] [PubMed] [Google Scholar]
- 29.Chew EY, Klein ML, Ferris FL, 3rd, Remaley NA, Murphy RP, Chantry K, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996;114:1079–84. doi: 10.1001/archopht.1996.01100140281004. [DOI] [PubMed] [Google Scholar]
- 30.Hadjadj S, Duly-Bouhanick B, Bekherraz A, Bridoux F, Gallois Y, Mauco G, et al. Serum triglycerides are predictive factor for the development and the progression of complications in patients with type 1 diabetes. Diabetes Metab. 2004;30:43–51. doi: 10.1016/s1262-3636(07)70088-5. [DOI] [PubMed] [Google Scholar]
- 31.Miljanovic B, Glynn RJ, Nathan DM, Manson JE, Schaumberg DA. A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes. Diabetes. 2004;53:2883–92. doi: 10.2337/diabetes.53.11.2883. [DOI] [PubMed] [Google Scholar]
- 32.Morton J, Zoungas S, Li Q, Patel AA, Chalmers J, Woodward M, et al. Low HDL cholesterol and the risk of diabetic nephropathy and retinopathy: Results of the ADVANCE study. Diabetes Care. 2012;35:2201–6. doi: 10.2337/dc12-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta A, Gupta V, Thapar S, Bhansali A. Lipid-lowering drug atorvastatin as an adjunct in the management of diabetic macular edema. Am J Ophthalmol. 2004;137:675–82. doi: 10.1016/j.ajo.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 34.Gordon B, Chang S, Kavanagh M, Berrocal M, Yannuzzi L, Robertson C, et al. The effects of lipid lowering on diabetic retinopathy. Am J Ophthalmol. 1991;112:385–91. doi: 10.1016/s0002-9394(14)76244-0. [DOI] [PubMed] [Google Scholar]
- 35.Desvergne B, Wahli W. Peroxisome proliferator- activated receptors: Nuclear control of metabolism. Endocr Rev. 1999;20:649–88. doi: 10.1210/edrv.20.5.0380. [DOI] [PubMed] [Google Scholar]
- 36.Escher P, Wahli W. Peroxisome proliferator-activated receptors: Insight into multiple cellular functions. Mutat Res. 2000;448:121–38. doi: 10.1016/s0027-5107(99)00231-6. [DOI] [PubMed] [Google Scholar]
- 37.Yki-Järvinen H. Thiazolidinediones. New Engl J Med. 2004;351:1106–18. doi: 10.1056/NEJMra041001. [DOI] [PubMed] [Google Scholar]
- 38.Kendall DM, Rubin CJ, Mohideen P, Ledeine JM, Belder R, Gross J, et al. Improvement of glycemic control, triglycerides, and HDL cholesterol levels with muraglitazar, a dual (alpha/gamma) peroxisome proliferator-activated receptor activator, in patients with type 2 diabetes inadequately controlled with metformin monotherapy: A double-blind, randomized, pioglitazone-comparative study. Diabetes Care. 2006;29:1016–23. doi: 10.2337/diacare.2951016. [DOI] [PubMed] [Google Scholar]
- 39.Mohanty P, Aljada A, Ghanim H, Hofmeyer D, Tripathy D, Syed T, et al. Evidence for a potent antiinflammatory effect of rosiglitazone. J Clin Endocrinol Metab. 2004;89:2728–35. doi: 10.1210/jc.2003-032103. [DOI] [PubMed] [Google Scholar]
- 40.Simó R, Hernández C. Prevention and Treatment of Diabetic Retinopathy: Evidence from Large, Randomized Trials. The Emerging Role of Fenofibrate. Rev Recent Clin Trials. 2012;7:71–80. doi: 10.2174/157488712799363299. [DOI] [PubMed] [Google Scholar]
- 41.Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TM, Moffitt MS, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): A randomised controlled trial. Lancet. 2007;370:1687–97. doi: 10.1016/S0140-6736(07)61607-9. [DOI] [PubMed] [Google Scholar]
- 42.Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): Randomised controlled trial. Lancet. 2005;366:1849–61. doi: 10.1016/S0140-6736(05)67667-2. [DOI] [PubMed] [Google Scholar]
- 43.Ferrara N. Role of vascular endothelial growth factor in regulationof physiological angiogenesis. Am J Physiol Cell Physiol. 2001;280:C1358–66. doi: 10.1152/ajpcell.2001.280.6.C1358. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Ahn JH, Kim JH, Yu YS, Kim HS, Ha J, et al. Fenofi brate regulates retinal endothelial cell survival through the AMPK signal transduction pathway. Exp Eye Res. 2007;84:886–93. doi: 10.1016/j.exer.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 45.Joussen AM, Poulaki V, Le ML, Koizumi K, Esser C, Janicki H, et al. A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J. 2004;18:1450–2. doi: 10.1096/fj.03-1476fje. [DOI] [PubMed] [Google Scholar]
- 46.Abu el Asrar AM, Maimone D, Morse PH, Gregory S, Reder AT. Cytokines in the vitreous of patients with proliferative diabetic retinopathy. Am J Ophthalmol. 1992;114:731–6. doi: 10.1016/s0002-9394(14)74052-8. [DOI] [PubMed] [Google Scholar]
- 47.Limb GA, Hickman-Casey J, Hollifield RD, Chignell AH. Vascular adhesion molecules in vitreous from eyes with proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 1999;40:2453–7. [PubMed] [Google Scholar]
- 48.Yuuki T, Kanda T, Kimura Y, Kotajima N, Tamura J, Kobayashi I, et al. Inflammatory cytokines in vitreous fluid and serum of patients with diabetic vitreoretinopathy. J Diabetes Complications. 2001;15:257–9. doi: 10.1016/s1056-8727(01)00155-6. [DOI] [PubMed] [Google Scholar]
- 49.Funatsu H, Yamashita H, Noma H, Mimura T, Yamashita T, Hori S. Increased levels of vascular endothelial growth factor and interleukin-6 in the aqueous humor of diabetics with macular edema. Am J Ophthalmol. 2002;133:70–7. doi: 10.1016/s0002-9394(01)01269-7. [DOI] [PubMed] [Google Scholar]
- 50.Villarroel M, Garcia-Ramírez M, Corraliza L, Hernández C, Simó R. Fenofibric acid prevents retinal pigment epithelium disruption induced by interleukin-1β by suppressing AMP-activated protein kinase (AMPK) activation activation. Diabetologia. 2011;54:1543–53. doi: 10.1007/s00125-011-2089-5. [DOI] [PubMed] [Google Scholar]
- 51.Bordet R, Ouk T, Petrault O, Gelé P, Gautier S, Laprais M, et al. PPAR: A new pharmacological target for neuroprotection in stroke and neurodegenerative diseases. Biochem Soc Trans. 2006;34:1341–6. doi: 10.1042/BST0341341. [DOI] [PubMed] [Google Scholar]
- 52.Cheung N, Wong TY. Fenofibrate and diabetic retinopathy. Lancet. 2008;371:721–2. doi: 10.1016/S0140-6736(08)60333-5. [DOI] [PubMed] [Google Scholar]
- 53.Treacy MP, Hurst TP. The case for intraocular delivery of PPAR agonists in the treatment of diabetic retinopathy. BMC ophthalmol. 2012;12:46. doi: 10.1186/1471-2415-12-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wong TY, Simó R, Mitchell P. Fenofibrate- A potential systemic treatment for diabetic retinopathy? Am J Ophthalmol. 2012;154:6–12. doi: 10.1016/j.ajo.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 55.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;30:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 56.Pedersen O, Gaede P. Intensified multifactorial intervention and cardiovascular outcome in type 2 diabetes: The steno-2 study. Metabolism. 2003;52:19–23. doi: 10.1016/s0026-0495(03)00213-0. [DOI] [PubMed] [Google Scholar]
- 57.Effect of aspirin alone and aspirin plus dipyridamole in early diabetic retinopathy. A multicenter randomized controlled clinical trial. Diabetes. 1989;38:491–8. [PubMed] [Google Scholar]
- 58.Ticlopidine treatment reduces the progression of nonproliferative diabetic retinopathy. Arch Ophthalmol. 1990;108:1577–83. doi: 10.1001/archopht.1990.01070130079035. [DOI] [PubMed] [Google Scholar]
- 59.The PKC-DRS Study Group. The effect of ruboxistaurin on visual loss in patients with moderately severe to very severe nonproliferative diabetic retinopathy: Initial results of the protein kinase C β inhibitor diabetic retinopathy study (PKC-DRS) multicenter randomized clinical trial. Diabetes. 2005;54:2188–97. doi: 10.2337/diabetes.54.7.2188. [DOI] [PubMed] [Google Scholar]
- 60.PKC-DRS2 Group. Aiello LP, Davis MD, Girach A, Kles KA, Milton RC, et al. Effect of ruboxistaurin on visual loss in patients with diabetic retinopathy. Ophthalmology. 2006;113:2221–30. doi: 10.1016/j.ophtha.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 61.The PKC-DMES Study Group. Effect of ruboxistaurin in patients with diabetic macular edema: Thirty-month results of the randomized PKC-DMES clinical trial. Arch Ophthalmol. 2007;125:318–24. doi: 10.1001/archopht.125.3.318. [DOI] [PubMed] [Google Scholar]
- 62.Lu L, Seidel CP, Iwase T, Stevens RK, Gong YY, Wang X, et al. Suppression of GLUT1; A new strategy to prevent diabetic complications. J Cell Physiol. 2013;228:251–7. doi: 10.1002/jcp.24133. [DOI] [PubMed] [Google Scholar]
- 63.Yellowlees Douglas J, Bhatwadekar AD, Li Calzi S, Shaw LC, Carnegie D, Caballero S, et al. Bone marrow-CNS connections: Implications in the pathogenesis of diabetic retinopathy. Prog Retin Eye Res. 2012;31:481–94. doi: 10.1016/j.preteyeres.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cukras CA, Petrou P, Chew EY, Meyerle CB, Wong WT. Oral minocycline for the treatment of diabetic macular edema (DME): Results of a phaseI/II clinical study. Invest ophthalmol Vis Sci. 2012;53:3865–74. doi: 10.1167/iovs.11-9413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nolan JJ, Jones NP, Patwardhan R, Deacon LF. Rosiglitazone taken once daily provides effective glycaemic control in patients with Type 2 diabetes mellitus. Diabet Med. 2000;17:287–94. doi: 10.1046/j.1464-5491.2000.00269.x. [DOI] [PubMed] [Google Scholar]
- 66.Shen LQ, Child A, Weber GM, Folkman J, Aiello LP. Rosiglitazone and delayed onset of proliferative diabetic retinopathy. Arch Ophthalmol. 2008;126:793–9. doi: 10.1001/archopht.126.6.793. [DOI] [PubMed] [Google Scholar]
- 67.Nyssen V, Hautenauven F, Lekeu Hinostroza JP, Guagnini AP. Diabetic edematous maculopathy associated with rosiglitazone treatment: Report of a case. Bull Soc Belge Ophtalmol. 2009;313:39–44. [PubMed] [Google Scholar]
- 68.Liazos E, Broadbent DM, Beare N, Kumar N. Spontaneous resolution of diabetic macular oedema after discontinuation of thiazolidenediones. Diabet Med. 2008;25:860–2. doi: 10.1111/j.1464-5491.2008.02491.x. [DOI] [PubMed] [Google Scholar]
- 69.Oshitari T, Asaumi N, Watanabe M, Kumagai K, Mitamura Y. Severe macular edema induced by pioglitazone in a patient with diabetic retinopathy: A case study. Vasc Health Risk Manag. 2008;4:1137–40. doi: 10.2147/vhrm.s3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tatti P, Arrigoni F, Longobardi A, Costanza F, Di Blasi P, Merante D. Retrospective analysis of rosiglitazone and macular oedema in patients with type 2 diabetes mellitus. Clin Drug Investig. 2008;28:327–32. doi: 10.2165/00044011-200828050-00006. [DOI] [PubMed] [Google Scholar]
- 71.Chew EY, Kim J, Coleman HR, Aiello LP, Fish G, Michael LP, et al. Preliminary assessment of Celecoxib and microdiode pulse laser treatment of diabetic macular edema. Retina. 2010;30:459–67. doi: 10.1097/IAE.0b013e3181bcf1a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liou GI, Ahmad S, Naime M, Fatteh N, Ibrahim AS. Role of adenosine in diabetic retinopathy. J Ocul Biol Dis Infor. 2011;4:19–24. doi: 10.1007/s12177-011-9067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


