Abstract
Thymoquinone (TQ) is the bioactive phytochemical constituent of the seeds oil of Nigella sativa. In vitro and in vivo research has thoroughly investigated the anticancer effects of TQ against several cancer cell lines and animal models. As a result, a considerable amount of information has been generated from research thus providing a better understanding of the anti-proliferating activity of this compound. Therefore, it is appropriate that TQ should move from testing on the bench to clinical experiments. The purpose of this review is to highlight the potential of TQ as an anticancer agent and the chances of this compound in the clinical treatment of cancer, with special attention on breast cancer treatment.
Keywords: Breast cancer, drug delivery, pharmacokinetics, thymoquinone
INTRODUCTION
Cancer is one of the most dreaded diseases of the 20th century and is spreading further with continuance and increasing incidence in 21st century. Breast cancer is the most prevalent cancer in women. Every year, the world celebrates “pink ribbon day” to spread awareness about this disease. It is one of the main life-threatening diseases that a woman may have to face during her lifetime, with 150 per 100,000 women being diagnosed with this illness each year.[1,2] It comprises 16% of all female cancers and is thought to cause half a million deaths annually.[2] Breast cancer is much less common among men, but it still strikes about 2,000 US males and kills nearly 400 annually.[3]
Several factors that contribute to life-style such as weight gain, obesity, and level of physical activity are associated with breast cancer risk. It was reported that a high intake of meat, dairy products, fat and alcohol may increase the risk and a high intake of fiber, fruits, vegetables, anti-oxidants, and phytoestrogens may reduce the risk of breast cancer.[4] The increasing incidence of breast cancer reported over the last few decades has led to the development of new anticancer drugs, drug combinations and chemotherapy strategies by the scientific exploration of an enormous pool of synthetic, biological, and natural products.[1,5] Experimental investigations demonstrated that many naturally occurring agents and plant extracts have shown anticancer potential in a variety of bioassay systems and animal models.[6,7,8] Nigella sativa, an oriental spice, which is also known as black seeds, has long been used as a natural medicine for treatment of many disease conditions.[9,10] Furthermore, the major bioactive constituent of the volatile oil of black seeds thymoquinone (TQ) [Figure 1] has shown promising pharmacological and therapeutic effects against in vitro and in vivo disease models.[11] There is an increasing research interest in TQ to evaluate its anticancer activity against breast cancer.[11,12,13] This coincides with interesting research findings suggesting new mechanisms of anticancer activity of TQ against breast cancer in vitro and in vivo models.[14,15] The availability of a review is needed to summarize these findings along with the latest progress in drug toxicity, pharmacokinetics and drug delivery studies of TQ, which could in principle, help in moving into the next level of clinical evaluation of TQ in breast cancer patients.
Figure 1.
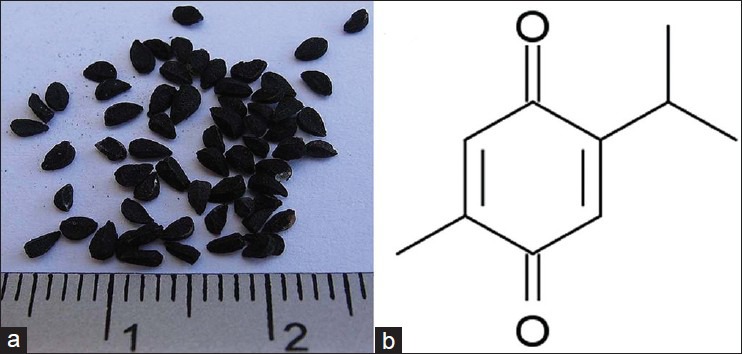
(a) Nigella sativa seeds (black seeds). (b) The chemical structure of thymoquinone; 2-isopropyl-5-methyl-1,4-benzoquinone (C10H12O2); Mwt 164.2
REVIEW AND DISCUSSION
TQ (2-isopropyl-5-methyl-benzoquinone) is one of the major components of the seeds oil of N. sativa. Specific chemical analyses using the high performance liquid chromatography of the seeds oil of N. sativa revealed that TQ may attain up to 27.8% of the volatile oil (w/w) composition.[16] TQ has been shown to possess beneficial therapeutic potential on human health as it is evident from many research findings.[11] There is a wide consensus in cancer research that TQ has promising anticancer activity in vitro and in vivo models.[7,15] It proved to be effective against several types of cancer cell lines in which the classical hallmark of apoptosis such as chromatin condensation, translocation of phosphatidyl serine across the plasma membrane, and DNA fragmentation have been documented in TQ-treated cells.[12] In addition to its apoptotic effect, recent published research revealed interesting inhibitory mechanisms imposed by TQ in breast cancer cell lines MCF-7, MDA-MB-231 and BT-474. Woo et al.[17] suggested a new molecular target for TQ anticancer activity against breast cancer cell lines, which is the peroxisome proliferator-activated receptors (PPARs). Three types of PPARs (α, β, γ) have been identified and PPAR-γ is found to play an important role in cell proliferation, differentiation and apoptosis.[18] It was shown to induce G1/S cell cycle arrest by up-regulating p21WAF1/Cip1[19] or p27Kip1[20] and down-regulating cyclin D1[21] and was reported to control invasion and metastasis of cancer. The authors presented molecular docking studies showing that TQ could make contact with amino-acids within the ligand binding pocket of PPAR-γ that are crucial for its activation. The activation of PPAR-γ was found to play a pivotal role in TQ-induced apoptosis through the activation of caspases and down-regulate PPAR-γ related genes, including Bcl-2, Bcl-xL and survivin at both mRNA and protein expression levels in MCF-7 cells. In addition, TQ was able to reduce the migration and invasion of MDA-MB-231 cells.
The development of multi-drug resistant human tumor cells including doxorubicin-resistant breast cancer cells, provoked further research with TQ to evaluate its effectiveness against this type of cells.[22,23] Arafa et al.[23] examined the anticancer effects of TQ in doxorubicin-resistant human breast cancer cells (MCF-7/DOX cells). The authors investigated the potential mechanism by which TQ may regulate cell proliferation and apoptosis in MCF-7/DOX cells. The suggested mechanism is that TQ induces apoptosis in doxorubicin-resistant breast cancer cells through the up-regulation of phosphatase and tensin homolog (PTEN) at the transcription level. The up-regulated PTEN, in turn, inhibits the phosphatidylinositol-3 kinase/Akt pathway and induces p53 and p21 protein expression, thereby causing G2/M cell cycle arrest and apoptosis.
Another potential molecular target for TQ was reported by Connelly et al.,[24] which is the nuclear factor kappa B (NF-κB). In vivo treatment of TQ on polyoma middle-T oncogene transgenic mouse model resulted in a reduction in tumor volume and weight as compared to the control. Inhibition of NF-κB by TQ increases apoptosis in hyperplastic stages of tumor development and decreases proliferation at least in part by reducing CyclinD1 expression, which inhibits mammary tumor progression.
There is no doubt that cancer research has demonstrated the therapeutic potential of TQ against breast cancer cell lines and animal models with the emphasis on the mechanism of action. In spite of this, there is however a lack of clinical studies testing TQ in human patients with breast cancer. In general, in the process of drug discovery a potential lead compound has to undergo preclinical evaluation prior to clinical trials. This includes understanding of the drug mechanism of action, drug toxicity and determination of its absorption, distribution, metabolism and excretion (ADME) of the drug. Once the ADME is defined, the compound enters the phase of drug development, production/formulation prior to clinical trials.[25] Accordingly, current research has addressed these issues and the use of TQ in clinical settings should therefore be encouraged. With the various mechanisms of action discussed earlier, issues such as: (1) Toxicity of TQ (2) pharmacokinetics of TQ (inclusive of ADME) and (3) TQ delivery will be further discussed herein.
Toxicity of TQ
Many studies were carried out to assess the toxicological properties of TQ in vitro and in vivo.[26,27,28] The oral and intraperitoneal median lethal dose (LD50) for TQ in rats as well as in mice were successfully assigned by several research groups.[29,30] The lack of preclinical studies with TQ reporting the maximum tolerated dose (MTD), which is defined as the highest dose that is safe to administer to animal models in the absence of intolerable adverse effects, for TQ toxicity is regarded as a limitation in using TQ in clinical settings to treat cancer. However, preliminary data regarding MTD for TQ in rats suggest lower MTD values in female than in male rats.[31] The possible risk of gender sensitivity to TQ toxicity with female breast cancer patients can be eliminated by adopting combinatorial drug therapy of TQ with doxorubicin, which is commonly used in chemotherapy to treat breast cancer.[32,33] It is worth mentioning that a couple of studies reported that TQ has an antioxidant protective effect against the doxorubicin-induced cardiotoxicity[34] and it does not interfere with the anticancer activity of doxorubicin[35] in animal models. In addition, using TQ in combination with ionizing radiation such as γ-radiation was found to exert a synergistic cytotoxic effect against breast cancer cells in vitro.[36]
Pharmacokinetics of TQ
The lack of bioavailability and pharmacokinetic parameters for TQ delayed the use of TQ in clinical settings. Study the interaction of TQ with blood components reflects the influence on its bioavailability, distribution in the body, metabolism and excretion. Hence, Lupidi et al.[37,38] reported the binding interaction of TQ with human serum albumin and Alpha-1 acid glycoprotein (AGP). This was confirmed by using the molecular modeling as well as Fluorescence quenching studies. El-Najjar et al.[39,40] studied the effect of TQ binding with bovine serum albumin (BSA) and AGP on its anticancer activity. The results suggested that covalent binding of TQ to BSA lead in losing the TQ anticancer activity against tested cancer cell lines, on the other hand, the TQ anticancer activity was not affected when TQ is bound to AGP. Further investigation is needed for better understanding of TQ pharmacokinetics and for future clinical development.
TQ delivery
The lipophilic nature of TQ introduces a solubility challenge, which could affect its bioavailability and cause limitation in drug formulation. TQ showed to be safe when it is administered orally in several disease animal models. A large number of studies used oral subacute and subchronic TQ in the range of 10-100 mg/kg body weight without any reported toxicity or deaths.[31] However, oral administration of TQ could lead to biotransformation due to induction of phase 2 enzymes in the liver such as DT-diaphorase, a quinine reductase, which catalyzes two electron reduction of TQ into a hydroquinone.[41] Serum protein binding and biotransformation are major factors in affecting TQ anticancer activity in vivo. Ravindran et al.[42] tested a novel delivery approach for TQ-loaded poly (lactide-co-glycolide) nanoparticles against several cancer cell lines including breast cancer line (MCF-7). The results showed a greater anticancer activity of the encapsulated TQ in nanoparticles than free TQ due to enhanced bioavailability and cellular uptake. Furthermore, Ganea et al.[43] tested the anticancer activity of TQ-loaded poly (lactide-co-glycolide) nanoparticles against other breast cancer cell line (MDA-MB-231) and showed to be more effective than free TQ. A recent research done by Odeh et al.[44] tested TQ-loaded liposomes particles against MCF-7 breast cancer cell line and proved to be effective in inhibiting the proliferation in this cell line. These results confirm the protective effect of the delivery vehicle against serum protein binding and biotransformation of TQ allowing better anticancer activity.
CONCLUSION AND FUTURE RECOMMENDATION
As per the discussion above, preclinical research results encourage the use of TQ in clinical settings. Considerable amount of information about TQ regarding its molecular anticancer activity, drug toxicity, bioavailability and pharmacokinetics and novel drug delivery approaches are now available for researchers. Al-Amri and Bamosa[45] investigated the effectiveness of oral TQ as an anticancer drug in advanced cancer patients including breast cancer patients. Patients with breast cancer were under treatment for 2 weeks with 400 mg/day. The authors reported neither toxicity nor therapeutic response. This study can be optimized and taken further with either the use of combination therapy of TQ with, for example, doxorubicin or the use of TQ-loaded nanoparticles to treat cancer patients. Moreover, TQ analogs such as caryophyllyl and germacryl conjugates as well as fatty acid conjugates showed a potent anticancer activity against sensitive and resistant MCF-7 breast cancer cell lines.[46,47] Therefore, these analogs can also be tested clinically to evaluate their anticancer activity in breast cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Banning M. Advanced breast cancer: Aetiology, treatment and psychosocial features. Br J Nurs. 2007;16:86–90. doi: 10.12968/bjon.2007.16.2.22765. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. Breast cancer: Prevention and control. 2009. [Last accessed on 2012 Dec]. Available from: http://www.who.int/cancer/detection/breastcancer/en/index.html .
- 3.CDC, US Cancer Statistics Working Group. Top 10 causes of death for women in the United States (2003) Atlanta CDC Statistics. 2007 [Google Scholar]
- 4.Farah IO, Begum RA. Effect of Nigella sativa (N. sativa L.) and oxidative stress on the survival pattern of MCF-7 breast cancer cells. Biomed Sci Instrum. 2003;39:359–64. [PubMed] [Google Scholar]
- 5.Foster TS, Miller JD, Boye ME, Blieden MB, Gidwani R, Russell MW. The economic burden of metastatic breast cancer: A systematic review of literature from developed countries. Cancer Treat Rev. 2011;37:405–15. doi: 10.1016/j.ctrv.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Mann J. Natural products in cancer chemotherapy: Past, present and future. Nat Rev Cancer. 2002;2:143–8. doi: 10.1038/nrc723. [DOI] [PubMed] [Google Scholar]
- 7.Gullett NP, Ruhul Amin AR, Bayraktar S, Pezzuto JM, Shin DM, Khuri FR, et al. Cancer prevention with natural compounds. Semin Oncol. 2010;37:258–81. doi: 10.1053/j.seminoncol.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Balachandran P, Govindarajan R. Cancer: An ayurvedic perspective. Pharmacol Res. 2005;51:19–30. doi: 10.1016/j.phrs.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Butt MS, Sultan MT. Nigella sativa: Reduces the risk of various maladies. Crit Rev Food Sci Nutr. 2010;50:654–65. doi: 10.1080/10408390902768797. [DOI] [PubMed] [Google Scholar]
- 10.Ilaiyaraja N, Khanum F. Nigella sativa L.: A review of therapeutic application. J Herb Med Toxicol. 2010;4:1–8. [Google Scholar]
- 11.Woo CC, Kumar AP, Sethi G, Tan KH. Thymoquinone: Potential cure for inflammatory disorders and cancer. Biochem Pharmacol. 2012;83:443–51. doi: 10.1016/j.bcp.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee S, Padhye S, Azmi A, Wang Z, Philip PA, Kucuk O, et al. Review on molecular and therapeutic potential of thymoquinone in cancer. Nutr Cancer. 2010;62:938–46. doi: 10.1080/01635581.2010.509832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Padhye S, Banerjee S, Ahmad A, Mohammad R, Sarkar FH. From here to eternity-the secret of Pharaohs: Therapeutic potential of black cumin seeds and beyond. Cancer Ther. 2008;6:495–510. [PMC free article] [PubMed] [Google Scholar]
- 14.Banerjee S, Parasramka M, Sarkar F, Mohammad R. Molecular insights and preclinical perspective of thymoquinone as chemotherapeutic agent and therapeutic adjuct in cancer. In: Shankar S, Srivastava R, editors. Nutrition, Deit and Cancer. Heidelberg: Springer Science; 2012. pp. 83–103. [Google Scholar]
- 15.Attoub S, Sperandio O, Raza H, Arafat K, Al-Salam S, Al Sultan MA, et al. Thymoquinone as an anticancer agent: Evidence from inhibition of cancer cells viability and invasion in vitro and tumor growth in vivo. Fundam Clin Pharmacol. 2012 doi: 10.1111/j.1472-8206.2012.01056.x. [DOI] [PubMed] [Google Scholar]
- 16.Ghosheh OA, Houdi AA, Crooks PA. High performance liquid chromatographic analysis of the pharmacologically active quinones and related compounds in the oil of the black seed (Nigella sativa L.) J Pharm Biomed Anal. 1999;19:757–62. doi: 10.1016/s0731-7085(98)00300-8. [DOI] [PubMed] [Google Scholar]
- 17.Woo CC, Loo SY, Gee V, Yap CW, Sethi G, Kumar AP, et al. Anticancer activity of thymoquinone in breast cancer cells: Possible involvement of PPAR-γ pathway. Biochem Pharmacol. 2011;82:464–75. doi: 10.1016/j.bcp.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 18.Kumar AP, Quake AL, Chang MK, Zhou T, Lim KS, Singh R, et al. Repression of NHE1 expression by PPARgamma activation is a potential new approach for specific inhibition of the growth of tumor cells in vitro and in vivo. Cancer Res. 2009;69:8636–44. doi: 10.1158/0008-5472.CAN-09-0219. [DOI] [PubMed] [Google Scholar]
- 19.Chang TH, Szabo E. Induction of differentiation and apoptosis by ligands of peroxisome proliferator-activated receptor gamma in non-small cell lung cancer. Cancer Res. 2000;60:1129–38. [PubMed] [Google Scholar]
- 20.Motomura W, Okumura T, Takahashi N, Obara T, Kohgo Y. Activation of peroxisome proliferator-activated receptor gamma by troglitazone inhibits cell growth through the increase of p27KiP1 in human. Pancreatic carcinoma cells. Cancer Res. 2000;60:5558–64. [PubMed] [Google Scholar]
- 21.Yin F, Wakino S, Liu Z, Kim S, Hsueh WA, Collins AR, et al. Troglitazone inhibits growth of MCF-7 breast carcinoma cells by targeting G1 cell cycle regulators. Biochem Biophys Res Commun. 2001;286:916–22. doi: 10.1006/bbrc.2001.5491. [DOI] [PubMed] [Google Scholar]
- 22.Worthen DR, Ghosheh OA, Crooks PA. The in vitro anti-tumor activity of some crude and purified components of blackseed, Nigella sativa L. Anticancer Res. 1998;18:1527–32. [PubMed] [Google Scholar]
- 23.Arafa el-SA, Zhu Q, Shah ZI, Wani G, Barakat BM, Racoma I, et al. Thymoquinone up-regulates PTEN expression and induces apoptosis in doxorubicin-resistant human breast cancer cells. Mutat Res. 2011;706:28–35. doi: 10.1016/j.mrfmmm.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Connelly L, Barham W, Onishko HM, Sherrill T, Chodosh LA, Blackwell TS, et al. Inhibition of NF-kappa B activity in mammary epithelium increases tumor latency and decreases tumor burden. Oncogene. 2011;30:1402–12. doi: 10.1038/onc.2010.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee KH. Discovery and development of natural product-derived chemotherapeutic agents based on a medicinal chemistry approach. J Nat Prod. 2010;73:500–16. doi: 10.1021/np900821e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qadri SM, Mahmud H, Föller M, Lang F. Thymoquinone-induced suicidal erythrocyte death. Food Chem Toxicol. 2009;47:1545–9. doi: 10.1016/j.fct.2009.03.037. [DOI] [PubMed] [Google Scholar]
- 27.Badary O, Al-Shabanah OA, Nagi MN, Al-Bekairi AM, Almazar MM. Acute and subchronic toxicity of thymoquinone in mice. Drug Develop Res. 1998;44:56–61. [Google Scholar]
- 28.Khader M, Bresgen N, Eckl PM. In vitro toxicological properties of thymoquinone. Food Chem Toxicol. 2009;47:129–33. doi: 10.1016/j.fct.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 29.Al-Ali A, Alkhawajah AA, Randhawa MA, Shaikh NA. Oral and intraperitoneal LD50 of thymoquinone, an active principle of Nigella sativa, in mice and rats. J Ayub Med Coll Abbottabad. 2008;20:25–7. [PubMed] [Google Scholar]
- 30.Mansour MA, Ginawi OT, El-Hadiyah T, El-Khatib AS, Al-Shabanah OA, Al-Sawaf HA. Effects of volatile oil constituents of Nigella sativa on carbon tetrachloride-induced hepatotoxicity in mice: Evidence for antioxidant effects of thymoquinone. Res Commun Mol Pathol Pharmacol. 2001;110:239–51. [PubMed] [Google Scholar]
- 31.AbuKhader MM. The effect of route of administration in thymoquinone toxicity in male and female rats. Indian J Pharm Sci. 2012;74:195–200. doi: 10.4103/0250-474X.106060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Effenberger-Neidnicht K, Schobert R. Combinatorial effects of thymoquinone on the anti-cancer activity of doxorubicin. Cancer Chemother Pharmacol. 2011;67:867–74. doi: 10.1007/s00280-010-1386-x. [DOI] [PubMed] [Google Scholar]
- 33.Ranson MR, Cheeseman S, White S, Margison J. Caelyx (stealth liposomal doxorubicin) in the treatment of advanced breast cancer. Crit Rev Oncol Hematol. 2001;37:115–20. doi: 10.1016/s1040-8428(00)00107-4. [DOI] [PubMed] [Google Scholar]
- 34.Nagi MN, Mansour MA. Protective effect of thymoquinone against doxorubicin-induced cardiotoxicity in rats: A possible mechanism of protection. Pharmacol Res. 2000;41:283–9. doi: 10.1006/phrs.1999.0585. [DOI] [PubMed] [Google Scholar]
- 35.al-Shabanah OA, Badary OA, Nagi MN, al-Gharably NM, al-Rikabi AC, al-Bekairi AM. Thymoquinone protects against doxorubicin-induced cardiotoxicity without compromising its antitumor activity. J Exp Clin Cancer Res. 1998;17:193–8. [PubMed] [Google Scholar]
- 36.Velho-Pereira R, Kumar A, Pandey BN, Jagtap AG, Mishra KP. Radiosensitization in human breast carcinoma cells by thymoquinone: Role of cell cycle and apoptosis. Cell Biol Int. 2011;35:1025–9. doi: 10.1042/CBI20100701. [DOI] [PubMed] [Google Scholar]
- 37.Lupidi G, Camaioni E, Khalifé H, Avenali L, Damiani E, Tanfani F, et al. Characterization of thymoquinone binding to human α1 -acid glycoprotein. J Pharm Sci. 2012;101:2564–73. doi: 10.1002/jps.23138. [DOI] [PubMed] [Google Scholar]
- 38.Lupidi G, Scire A, Camaioni E, Khalife KH, De Sanctis G, Tanfani F, et al. Thymoquinone, a potential therapeutic agent of Nigella sativa, binds to site I of human serum albumin. Phytomedicine. 2010;17:714–20. doi: 10.1016/j.phymed.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 39.El-Najjar N, Ketola RA, Nissilä T, Mauriala T, Antopolsky M, Jänis J, et al. Impact of protein binding on the analytical detectability and anticancer activity of thymoquinone. J Chem Biol. 2011;4:97–107. doi: 10.1007/s12154-010-0052-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El-Najjar N, Ketola R, Urtti A, Gali-Muhtaseb H, Vuorela H. Impact of protein binding on thymoquinone's analytical detection. Planta Med. 2010;76:351. [Google Scholar]
- 41.Nagi MN, Almakki HA. Thymoquinone supplementation induces quinone reductase and glutathione transferase in mice liver: Possible role in protection against chemical carcinogenesis and toxicity. Phytother Res. 2009;23:1295–8. doi: 10.1002/ptr.2766. [DOI] [PubMed] [Google Scholar]
- 42.Ravindran J, Nair HB, Sung B, Prasad S, Tekmal RR, Aggarwal BB. Thymoquinone poly (lactide-co-glycolide) nanoparticles exhibit enhanced anti-proliferative, anti-inflammatory, and chemosensitization potential. Biochem Pharmacol. 2010;79:1640–7. doi: 10.1016/j.bcp.2010.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Ganea GM, Fakayode SO, Losso JN, van Nostrum CF, Sabliov CM, Warner IM. Delivery of phytochemical thymoquinone using molecular micelle modified poly (D, L lactide-co-glycolide) (PLGA) nanoparticles. Nanotechnology. 2010;21 doi: 10.1088/0957-4484/21/28/285104. 285104. [DOI] [PubMed] [Google Scholar]
- 44.Odeh F, Ismail SI, Abu-Dahab R, Mahmoud IS, Al Bawab A. Thymoquinone in liposomes: A study of loading efficiency and biological activity towards breast cancer. Drug Deliv. 2012;19:371–7. doi: 10.3109/10717544.2012.727500. [DOI] [PubMed] [Google Scholar]
- 45.Al-Amri A, Bamosa A. Phase I safety and clinical activity study of thymoquinone in patients with advanced refractory malignant disease. Shiraz E-Med J. 2009;10:107–11. [Google Scholar]
- 46.Effenberger K, Breyer S, Schobert R. Terpene conjugates of the Nigella sativa seed-oil constituent thymoquinone with enhanced efficacy in cancer cells. Chem Biodivers. 2010;7:129–39. doi: 10.1002/cbdv.200900328. [DOI] [PubMed] [Google Scholar]
- 47.Breyer S, Effenberger K, Schobert R. Effects of thymoquinone-fatty acid conjugates on cancer cells. ChemMedChem. 2009;4:761–8. doi: 10.1002/cmdc.200800430. [DOI] [PubMed] [Google Scholar]


