Abstract
For pregnant women, exercise offers numerous benefits with little risk. The American College of Obstetricians and Gynecologists (ACOG) endorses aerobic exercise for all pregnant women without medical or obstetric complications. Nonetheless, only a small percentage of pregnant women meet exercise guidelines. We investigated the extent to which obstetricians (Obs) in private or small group practice in the USA actively recommend exercise to their pregnant patients. Surveys were sent to 300 Obs in 33 American cities, of which 83 were returned. 52% of respondents reported discussing exercise with 81-100% of their patients. Using a 7- point Likert scale (1 = never, 7 = always), Obs reported recommending aerobic exercise more often than resistance exercise (5.6 ± 1.5 versus 3.8 ± 1.6, p < 0.001). Obs do not routinely advise sedentary women to initiate exercise during pregnancy (mean 4.4 ± 1.8). Of the 67% of Obs who specify a target exercise duration, 95% recommend ≥ 16 min, consistent with ACOG guidelines. However, 62% of Obs reported that they regularly specify a maximum heart rate, even though ACOG guidelines do not. Half of respondents indicated that they advise a reduction in exercise load during the third trimester, even for uncomplicated pregnancies. Respondents’ opinions were mixed regarding the extent to which exercise reduces gestational diabetes or preeclampsia risk and they believe more research on exercise during pregnancy is needed. Half of Obs do not routinely discuss exercise. The majority is hesitant to advise sedentary gravidae to start exercise and is conservative with respect to exercise intensity. Action may be needed to convince more Obs to routinely recommend exercise to all healthy patients.
Key Points.
52% of surveyed obstetricians discuss exercise with 81-100% of pregnant patients.
68% of surveyed obstetricians do not regularly advise sedentary pregnant women to initiate an exercise program.
62% of surveyed obstetricians recommend pregnant patients not exceed a maximum heart rate during exercise, even though ACOG guidelines do not specify a maximum heart rate.
Approximately half of surveyed obstetricians recommend a reduction in exercise load during the third trimester, even though ACOG guidelines do not.
Regular exercise was thought by surveyed obstetricians to have some potential for reducing the risk of gestational diabetes, but little effect on risk of preeclampsia.
Key words: Physical activity, prenatal activity, pregnant women, guidelines for exercise
Introduction
Modern popular culture has embraced the concept of a "fit pregnancy", as demonstrated by the plethora of publications available on this topic. Scientific literature supports the contention that regular exercise during pregnancy incurs little risk (Avery et al., 1999; Hall and Kaufmann, 1987; Kardel and Kase, 1998; Leiferman and Evenson, 2003; Lokey et al., 1991; Morris and Johnson, 2005) and is beneficial, in terms of both mental (Da Costa et al., 2003; Goodwin et al., 2000; Marquez-Sterling et al., 2000; Poudivigne and O’Connor, 2006) and physical (Clapp, 2000; Dempsey et al., 2005; Pivarnik et al., 2006) health. In accordance with research findings, current guidelines published by the American College of Obstetricians and Gynecologists (ACOG), as well as other national organizations such as the Society of Obstetricians and Gynaecologists of Canada (SOGC), endorse exercise for pregnant women.
Specifically, the ACOG Committee Opinion on exercise during pregnancy published in 2002 recommends that, barring medical or obstetric contraindications, pregnant women engage in 30 or more minutes of moderate exercise daily, or at least on "most" days of the week (ACOG, 2002). This recommendation is essentially the same as that made for the general population by the U. S. Centers for Disease Control and Prevention and the American College of Sports Medicine (Pate et al., 1995). The 2003 joint statement of the SOGC and the Canadian Society for Exercise Physiology (CSEP) regarding exercise during pregnancy went beyond the ACOG statement in recommending resistance exercise as well as aerobic exercise (Davies et al., 2003). Although a priori evaluation is recommended for previously sedentary women, this population is not excluded from the general exercise recommendation by the ACOG or the SOGC/CSEP; indeed the latter groups’ statement provides a plan for inactive women to gradually increase their activity level (Davies et al., 2003).
Despite the positive image and scholarly endorsement of exercise during pregnancy, data from the 1994, 1996, 1998 and 2000 Behavior Risk Factor Surveillance System indicate that pregnant women participate in less leisure-time physical activity than do non-pregnant women (Evenson et al., 2004; Petersen et al., 2005). In fact, one third (34.5%) of the pregnant women sampled in 2000 were completely sedentary (no leisure-time activity), and only 16% undertook the ACOG recommended exercise volume (Evenson et al., 2004). Obstetricians are in a favorable position to encourage physical activity (Krans et al., 2005), hence we sought to determine the extent to which obstetricians in private or small group practice in the United States recommend exercise to healthy patients, in accordance with current ACOG guidelines. Due to the fact that the ACOG's position on exercise during pregnancy was significantly more restrictive prior to 1994, it is possible that some obstetricians adhere to now obsolete recommendations that heart rate not exceed 140 bpm and the duration of "strenuous" exercise be limited to 15 min. Therefore, we tested the possibility that obstetricians who have been in practice for > 10 years are more likely than those in practice ≤ 10 years to suggest a maximum heart rate and an exercise duration of ≤ 15 min. We also asked obstetricians about the recommendations they make regarding resistance exercise and modification of exercise volume for the third trimester, as well as about their beliefs regarding exercise and the risk of gestational diabetes mellitus (GDM) and preeclampsia, and the extent to which more research on exercise and pregnancy outcomes is needed.
Methods
This study was approved by the Northern Arizona University Institutional Review Board. An anonymous, 18 item survey was mailed to 300 obstetricians located in 33 cities representing 17 randomly selected states (AZ, CA, CO, GA, IA, KS, ME, MN, MT, NH, NM, OK, OR, SC, UT, WA, WY). The populations of the cities ranged from 6,000 to 360,000. Obstetricians were identified via on-line yellow pages and all listed obstetricians were included in the mailing unless a complete address could not be obtained. The one exception to this policy was the case of the largest listing, from which roughly 75% of the obstetricians were randomly selected for inclusion. Return of the survey was construed as consent to participate in the study. No incentives were offered for survey return.
The survey is available in the Appendix. All 18 questions were close-ended and screened by an obstetrician for face validity. Three items were self-descriptive multiple choice (e.g., clinical title). Ten of the items asked participants for a rating on a 7-point Likert scale with verbal anchors. The remaining five items were multiple choice, designed to elicit a single response. Survey responses were analyzed with SPSS-generated descriptive statistics, t-tests and a correlation matrix. For both the t-tests and Pearson correlation coefficients, significance was accepted at p ≤ 0.05. Responses for 7-point Likert scale items are reported as mean ± the standard deviation.
Results
Of the 300 surveys mailed, 85 surveys were returned, although two respondents stated that they no longer practiced obstetrics and therefore declined to complete the survey. Twenty-two surveys were returned undelivered, thus the response rate, considering only those surveys that presumably reached the addressee, was 30%.
Subject Characteristics
81 of 83 (98%) respondents identified themselves as holding the title of MD, obstetrics and gynecology. Two respondents identified themselves as holding the title MD, family medicine or other field. For simplicity, the term "obstetricians" is used in this paper to group all survey respondents. In terms of years of practice in the field of obstetrics, 41% indicated 10 years, 31% indicated 11-20 years, and 28% indicated > 20 years of experience. When asked to self-evaluate their familiarity with the ACOG 2002 Committee Opinion on exercise during pregnancy, the mean response was 5.2 ± 1.5, where 1 was equated to "not familiar at all" and 7 was equated to "very familiar". For this item, 24% of participants chose 7 ("very familiar"), while only 13% rated their familiarity at less than the mid-point (i.e., as a 1, 2, or 3).
Recommendations for Exercise
When asked to estimate with what percent of pregnant patients they specifically discuss exercise, half (52%) of respondents indicated 81-100%, while 18% estimated 61-80%, 16% estimated 41-60% and 14% estimated 0-40%. Self-reported familiarity with the ACOG 2002 Committee Opinion on exercise and pregnancy was positively correlated with the percent of patients with whom exercise is discussed (r = 0.29, p = 0.005). Three-quarters (75%) of respondents said that they initiate the discussion about exercise, 18% reported that they discuss exercise only when prompted by a client inquiry, and 7% indicated that their staff handles discussions of exercise with pregnant patients.
The mean response regarding how often obstetricians recommend aerobic exercise to patients in their first trimester was 5.6 ± 1.5, where 1 was equated to "never" and 7 to "always". Nearly two thirds (63%) of respondents chose either a 6 or 7 (Table 1). A significantly lower (p < 0.001) mean response, 3.8 ± 1.6, was obtained when the same question was asked about resistance exercise (strength training) (Table 1). With respect to how often obstetricians advise sedentary patients to begin a "moderate" exercise program during the pregnancy, the mean response was 4.4 ± 1.8, or about mid-way between "never" and "always". Only one third (31%) of respondents answered this question with a 6 or 7 (Table 1). Frequency of recommending aerobic exercise was positively correlated with recommending resistance exercise (r = 0.36, p = 0.001) and recommending exercise to previously sedentary patients (r = 0.44, p < 0.001).
Table 1.
Distribution of responses to questions regarding the frequency of: Recommending aerobic exercise, recommending resistance exercise, recommending that sedentary individuals initiate exercise during pregnancy, and recommending a maximum heart rate during exercise.
| Item | N | Likert Scale Response Value | |||
|---|---|---|---|---|---|
| 1 or 2 | 3 to 5 | 6 or 7 | Mean (±SD) | ||
| Freq Aerobic | 82 | 6.0% | 30.4% | 63.4% | 5.6 (1.5) |
| Freq Resist | 81 | 23.4% | 60.5% | 16.0% | 3.8 (1.6) |
| Freq BeginEx | 83 | 15.6% | 53.1% | 31.4% | 4.4 (1.8) |
| Freq MaxHR | 81 | 18.5% | 19.7% | 61.7% | 5.3 (2.1) |
Freq = frequency of recommending, Aerobic = aerobic exercise, Resist = resistance exercise, BeginEx = a sedentary individual begin an exercise program during the pregnancy, MaxHR = that patients keep their heart rate under a maximum level during exercise. Responses were made on a 1-7 Likert scale where 1 = "never" and 7 = "always".
Recommendations for Third Trimester
Half (54%) of the participants reported that they recommend patients who exercised throughout the first and second trimesters reduce their aerobic exercise load (duration and/or intensity) during the third trimester, even in the absence of obstetric complications. Essentially the same percentage (49%) expressed the identical opinion for resistance exercise. On the other hand, fewer than 10% of respondents recommend that patients stop aerobic or resistance exercise in the third trimester. Almost a quarter (23%) of the respondents said they offer no specific recommendation regarding aerobic or resistance exercise in the third trimester.
Intensity and Duration of Exercise
Participants were asked to estimate how often they advise patients to keep their heart rate under a maximum level, such as 140 or 150 bpm. The mean response to this question was 5.3 ± 2.1 (Table 1), where 1 was equated to "never" and 7 was equated to "always". A majority (62%) of participants selected a 6 or 7 in response to this question (Table 1).
When asked what duration of aerobic exercise they suggest, 64% of respondents chose ≥ 16 min of continuous exercise. Only 3 participants, all of whom have been in practice for at least 16 years, reported that they recommend a target duration of ≤ 15 min. A third (32%) of respondents said they offer no specific recommendation regarding the duration of aerobic exercise.
Health Benefits of Exercise and Research Need
When asked to what extent regular aerobic exercise would reduce the risk of GDM, respondents provided a mean rating of 4.7 ± 1.4, where 1 was equated to "not at all" and 7 to "quite a lot". Half (51%) of those polled selected a response above the mid-point (Figure 1). When asked the same question about exercise and the risk of preeclampsia, the mean value was significantly lower ( 2.7 ± 1.6, p < 0.001). Only 15% of the responses to this question were above the mid-point (Figure 2). Nonetheless, responses regarding GDM and preeclampsia were correlated; those who rated the efficacy of exercise to reduce the risk of GDM higher also rated the efficacy of exercise to reduce the risk of preeclampsia higher (r = 0.50, p < 0.001). Ratings regarding exercise and GDM were also positively correlated with recommending exercise to sedentary individuals (r = 0.45, p < 0.001).
Figure 1.
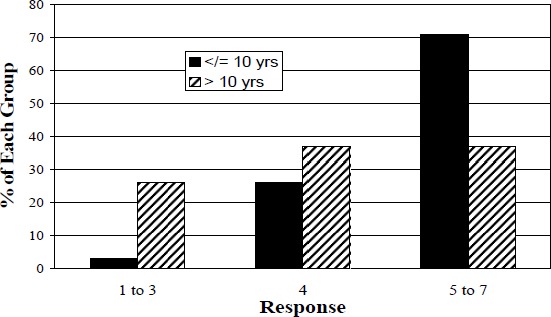
Comparison between obstetricians in practice for ≤ 10 years and those in practice for > 10 years on their ratings of the extent to which regular aerobic exercise can reduce the risk of gestational diabetes mellitus. Responses were made on a 7-point Likert scale where 1 was equated to "not at all" and 7 was equated to "quite a lot". The difference between the two groups was significant (p = 0.004).
Figure 2.
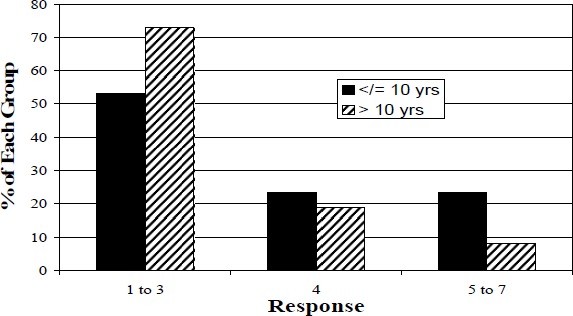
Comparison between obstetricians in practice for ≤ 10 years and those in practice for > 10 years on their ratings of the extent to which regular aerobic exercise can reduce the risk of preeclampsia. Responses were made on a 7- point Likert scale where 1 was equated to "not at all" and 7 was equated to "quite a lot". The difference between the two groups was significant (p = 0.052).
In general, obstetricians perceived a need for more research on the effects of exercise during pregnancy on pregnancy outcomes, as indicated by a mean response of 5.9 ± 1.2, and a modal response of 7, equated to "much need".
Comparison By Years in Practice
We hypothesized that obstetricians who have been practicing for ≤ 10 years adhere more closely to ACOG 2002 guidelines than those in practice longer. Contrary to expectation, we did not find any significant differences between the two groups in frequency of discussing or recommending exercise, or in their recommendations about duration and intensity of exercise, including recommendations for the third trimester. Where the two groups differed was in their beliefs about the health benefits of exercise. Respondents with ≤ 10 years in obstetrics practice (n = 34) rated exercise as significantly more effective in reducing the risk of GDM and preeclampsia than did subjects with >10 years in obstetrics practice (n = 49) (5.1 ± 1.0 versus 4.3 ± 1.6, p = 0.004 and 3.1 ± 1.7 versus 2.4 ± 1.5, p = 0.052, respectively) (Figures 1 and 2).
Discussion
Despite the position of the ACOG that healthy pregnant women carrying uncomplicated pregnancies should be encouraged to engage in regular exercise, we found that only about half of the obstetricians in our sample routinely discuss exercise with their pregnant patients. This finding is consistent with a recent study indicating that although 96% of pregnant women surveyed said they had received advice on exercise during their pregnancies, the primary sources of that advice were books, magazines, family, and friends (Clarke and Gross, ]2004). An even lower rate of exercise discussion by obstetricians was reported by Stafford and Blumenthal, 1998, who found that obstetrician/gynecologists provided counseling on exercise in only 13.8% of all adult patient visits, a frequency similar to that of several other medical specialties. It is possible that the lower frequency of exercise discussion found by Stafford and Blumenthal, 1998 compared to that estimated by our survey participants is due to increased frequency of exercise counseling by obstetricians over the last 5-10 years, overestimation of the true frequency by our survey respondents, or because obstetrician/gynecologists discuss exercise less frequently with non-pregnant compared to pregnant patients.
When obstetricians do discuss exercise with women in the first trimester of pregnancy, they frequently recommend aerobic exercise. Resistance exercise is recommended only by a minority of obstetricians (Table 1) who have apparently generalized their exercise endorsement beyond the ACOG statement. As a group, the respondents appeared hesitant to encourage sedentary women to initiate an exercise program during pregnancy (Table 1). Furthermore, contrary to our expectation, obstetricians in practice for ≤ 10 years were no more likely to recommend exercise to an inactive woman than those in practice for >10 years. Our findings contrast with a study of physicians in Michigan, of whom 87% believed that starting an exercise program is safe for pregnant women without contraindications (Bauer et al., 2004). The disparity between Bauer et al.’s (2004) finding and the present results suggests that there may be a disconnect between obstetricians’ beliefs and their behaviors (i.e., actively encouraging exercise). The reluctance of some obstetricians to advise sedentary women to begin an exercise program is at odds with scientific evidence supporting the safety and health benefits of initiating exercise during pregnancy (Marquez-Sterling et al., 2000; Lynch et al., 2003) and represents a missed opportunity to promote a positive, potentially long-term behavioral change (Artal and O’Toole, 2003; Paisley et al., 2003). Indeed, a study by Krans et al., 2005 found that the probability that a woman exercised during pregnancy was increased if her obstetrician encouraged her to exercise. One advantage of exercise promotion during obstetrical visits versus other primary care settings is that pregnant women generally make relatively frequent, repeated visits to their obstetrician, providing the opportunity for reinforcement of the exercise endorsement, a factor likely to improve compliance (Simons-Morton et al., 1998).
Nearly two thirds of obstetricians surveyed recommend a target duration for aerobic exercise of 16-30 minutes, or more, which is compatible with current ACOG guidelines. However, despite the fact that a heart rate maximum was eliminated from the ACOG guidelines in 1994 (ACOG, 1994), over 60% of respondents regularly advise pregnant patients to limit exercise intensity to the level eliciting a heart rate of 140 or 150 bpm (Table 1). Similarly, Bauer et al., 2004 found that 63% of physicians practicing in Michigan believe that pregnant individuals should not exceed a heart rate of 140 bpm during exercise and Krans et al., 2005 reported that the ACOG's more restrictive 1985 guidelines were invoked in 69% of discussions on exercise between obstetricians and their patients. Available studies do not support the necessity of a heart rate limitation (Kardel and Kase, 1998; Lokey et al., 1991; Zeanah and Schlosser, 1993; MacPhail et al., 2000), rather, a target range for rating of perceived exertion (e.g., Borg scale) has been proposed as an alternative means of selecting an appropriate exercise intensity (Artal and O’Toole, 2003; Stevenson, 1997).
When a pregnant woman chooses to be physically active during pregnancy, about half of obstetricians surveyed recommend that she reduce her exercise intensity and/or duration during the third trimester for both aerobic and resistance exercise. In contrast, the ACOG statement advises a second and third trimester reduction in exercise load only for women at elevated risk of preterm labor or fetal growth restriction (ACOG, 2002). A reduction in exercise load after mid-gestation has been found to increase maternal weight gain, fetal growth, and fetal fat mass (Clapp et al., 2002), thus a seemingly conservative recommendation to reduce exercise intensity and/or duration in the third trimester may have undesirable effects.
The ACOG 2002 opinion identifies the prevention and mitigation of GDM as potential benefits of regular exercise (ACOG, 2002). Nonetheless, opinions of the survey participants were mixed regarding the extent to which regular aerobic exercise can reduce the risk of GDM (Figure 1). Obstetricians in practice for ≤ 10 years rated exercise as more effective in reducing GDM risk than did those in practice > 10 years (p = 0.004), suggesting that the latter group are either less cognizant of current research or are more skeptical of the findings. Those who rated the potential of exercise to reduce GDM risk higher were also more likely to advise sedentary individuals to start exercising (r = 0.45, p < 0.001), which may indicate that obstetricians weigh potential benefits against perceived risk when choosing whether or not to advise the initiation of exercise.
Presently, the evidence to support a link between physical activity during pregnancy and the risk of preeclampsia, while promising, is limited to four observational studies (Irwin et al., 1994; Marcoux et al., 1989; Saftlas et al., 2004; Sorensen et al., 2003) and one experimental trial with 16 subjects (Yeo et al., 2000). Hence, it is not surprising that survey respondents were generally skeptical on this point, although obstetricians in practice for 10 years were more optimistic than those in practice for > 10 years (p = 0.052; Figure 2). Perceived potency of exercise to prevent GDM was positively correlated with perceived capacity of exercise to prevent preeclampsia (r = 0.50, p < 0.001), despite the relative lack of data on the latter complication, implying that some obstetricians view exercise as more broadly beneficial than do others.
Limitations
We were interested in the independent views and behaviors of "typical" practicing obstetricians rather than of those with highly specialized practices or significant teaching and/or research responsibilities. Consequently, we chose to survey obstetricians who were individually listed in the yellow pages and working in small to moderately large cities in the United States. This methodology likely biased our sample toward obstetricians in private or small group practice rather than those who work for large hospitals. Obstetricians working in larger facilities may have more opportunity to exchange ideas with other professionals and attend professional meetings, and thereby may be more quickly apprised of ideological shifts. It is also possible that systematic differences exist between obstetricians practicing in cities with populations > 360,000 and those practicing in cities in the size range we sampled (6,000 to 360,000), although it is not clear a priori which group would adhere more closely to ACOG guidelines
The response rate to this survey, 30%, is within the range reported for mailed surveys of obstetrician-gynecologists. Two factors may contribute to the response rate: First, no second requests or reminders were mailed and second, the survey did not originate from a Department of Obstetrics and Gynecology or the ACOG's own Department of Research, and therefore some recipients may have perceived it as unofficial or unimportant. On the assumption that physicians who view exercise more positively would be more likely to respond to a survey related to exercise, it is possible that the mean responses obtained overestimate the true means with respect to frequency of discussing and recommending exercise to pregnant patients. Thus, despite the potential limitations of our sample, we believe our results point to a disparity between ACOG guidelines on exercise during pregnancy and the actual practices of obstetricians in private or small group practice in the United States.
Conclusions
Active promotion of exercise by obstetricians may help to raise rates of physical activity among pregnant women (Krans et al., 2005; Simons-Morton et al., 1998). Our findings indicate that while some obstetricians do follow current ACOG guidelines and routinely recommend aerobic exercise to healthy, pregnant patients, a significant percentage do not do so. In particular, many obstetricians seldom advise sedentary women to initiate an exercise program during the pregnancy, despite the low risk and high probability of health benefits, possibly including a decreased risk of GDM (Dempsey et al., 2004) and preeclampsia (Marcoux et al., 1989; Saflas et al., 2004; Sorensen et al., 2003; Yeo et al., 2000). This reluctance to encourage healthy but sedentary women to begin an exercise regime is particularly unfortunate as pregnancy may be a period of particular receptivity to health-promoting suggestions (Paisley et al., 2003). Furthermore, evidence does support the contention that women are more likely to exercise during pregnancy if their obstetrician encourages them to do so (Krans et al., 2005).
Consistent with their reservations regarding exercise initiation, a majority of obstetricians are more conservative than ACOG guidelines in terms of exercise intensity and exercise load in the third trimester. A general skepticism toward the safety and efficacy of exercise is also reflected in a perceived need for more research and information on the effects of exercise during pregnancy on pregnancy outcomes. Taken together, the current findings suggest that practicing obstetricians are less confident in recommending exercise during pregnancy than the ACOG guidelines would suggest. Action may be needed to allay concerns and convince more obstetricians to routinely discuss exercise with all healthy patients. If that can be done, then it is likely that exercise will be recommended more often, and the health benefits of exercise enjoyed by more pregnant women.
Acknowledgements
The authors are grateful for the input and advice of Dr. Diana Herman, M.D., FACOG and Dr. Elliot Entin, Ph.D.
This experiment was conducted in compliance with all laws of the United States of America.
Biographies
Pauline L. ENTIN
Employment
Associate professor of exercise science in the Department of Biological Sciences at Northern Arizona University.
Degree
PhD.
Research interests
Limits to gas exchange during exercise
E-mail: Pauline.entin@nau.edu
Kelly M. MUNHALL
Employment
Southern College of Optometry in Memphis, Tennessee, USA.
Degree
BS.
APPENDIX : (Survey Questions)
-
What is your clinical title?
M.D., obstetrics and gynecology
M.D., family medicine or other field
D.O., obstetrics and gynecology
D.O., family medicine or other field
Other (please specify): ______________________________
-
For how many years has your own clinical practice included monitoring of pregnancies?
5 years or less
6-10 years
11-15 years
16-20 years
More than 20 years
-
How familiar are you with the American College of Obstetrics and Gynecology (ACOG) Committee Opinion (January, 2002) on exercise during pregnancy?
-
With what percentage of your pregnant patients do you specifically discuss exercise during pregnancy?
0-20%
21-40%
41-60%
61-80%
81-100%
-
In general, do you initiate a discussion about exercise with your pregnant patients, or do you discuss exercise only if your patient asks for your input?
I initiate the discussion about exercise
I discuss exercise with pregnant patients only if the patient asks for my input
My staff discusses exercise with my patients
-
When you discuss exercise with your patients in their first trimester, how often do you recommend aerobic exercise such as swimming, stationary biking, stairmaster etc?
-
When you discuss exercise with your patients in their first trimester, how often do you recommend resistance exercise (strength training) such as weight machines?
-
Do you recommend that patients without obstetric complications who exercise during the first and second trimesters decrease their aerobic exercise load (duration and/or intensity) during the third trimester?
I recommend that patients reduce their aerobic exercise load in the third trimester
I recommend that patients stop aerobic exercise during the third trimester
I recommend no reduction in aerobic exercise load during the third trimester
I make no specific recommendation regarding aerobic exercise in the third trimester
-
Do you recommend that patients without obstetric complications who exercise during the first and second trimesters decrease their resistance exercise load (duration and/or intensity) during the third trimester?
I recommend that patients reduce their resistance exercise load in the third trimester
I recommend that patients stop resistance exercise during the third trimester
I recommend no reduction in resistance exercise load during the third trimester
I make no specific recommendation regarding resistance exercise in the third trimester
-
When you discuss exercise with your pregnant patients, how often do you recommend that patients keep their exercise heart rate under a maximum level, such as 140 or 150 bpm?
-
When you discuss exercise with your pregnant patients, what duration do you usually suggest as a target or goal for aerobic exercise?
No exercise
15 min or less of continuous exercise
16-30 min of continuous exercise
More than 30 min of continuous exercise
I do not make any specific recommendation regarding duration
-
When counseling pregnant patients who are not physically active but are otherwise healthy, how often do you advise the patient to begin a moderate exercise program at some point during the pregnancy?
-
To what extent do you think that the performance of regular aerobic exercise by a pregnant woman will reduce the probability that she will develop gestational diabetes?
-
To what extent do you think that the performance of regular aerobic exercise by a pregnant woman will reduce the probability that she will develop preeclampsia?
-
* To what extent do you think there is a need for more research and information on the effects of exercise during pregnancy on pregnancy outcomes?
Footnotes
Note: There were three additional items that are not pertinent to the present report.
References
- American College of Obstetricians and Gynecologists (2002) ACOG Committee Opinion #267: Exercise during pregnancy and the postpartum period. Obstetrics and Gynecology 99, 171-173 [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists (1994) ACOG Technical Bulletin #189: Exercise during pregnancy and the post-partum period. International Journal of Gynecology and Obstetrics 45, 65-70 [PubMed] [Google Scholar]
- Artal R., O’Toole O. (2003) Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. British Journal of Sports Medicine 37, 6-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery N.D., Stocking K.D., Tranmer J.E., Davies G.A., Wolfe L.A. (1999) Fetal responses to maternal strength and conditioning exercises in late gestation. Canadian Journal of Applied Physiology 24, 362-376 [DOI] [PubMed] [Google Scholar]
- Bauer P.W., Broman C.L., Pivarnik J.M. (2004) Exercise and pregnancy survey for health care providers. Medicine and Science in Sports and Exercise 36(5), Abstract S113 [Google Scholar]
- Clapp J.F. (2000) Exercise during pregnancy. A clinical update. Clinical Sports Medicine 19, 273-286 [DOI] [PubMed] [Google Scholar]
- Clapp J.F., Kim H., Burcio B., Schmidt S., Petry K., Lopez B. (2002) Continuing regular exercise during pregnancy: effect of exercise volume on fetoplacental growth. American Journal of Obstetrics and Gynecology 186, 142-147 [DOI] [PubMed] [Google Scholar]
- Clarke P.E., Gross H. (2004) Women’s behavior, beliefs and information sources about physical exercise in pregnancy. Midwifery 20, 133-141 [DOI] [PubMed] [Google Scholar]
- Da Costa D., Rippen N., Dritsa M., Ring A. (2003) Self-reported leisure-time physical activity during pregnancy and relationship to psychological well-being. Journal of Psychosomatic Obstetrics and Gynaecology 24, 111-119 [DOI] [PubMed] [Google Scholar]
- Davies G.A., Wolfe L.A., Mottola M.F., MacKinnon C. (2003) Joint SOGC/CSEP clinical practice guideline: exercise in pregnancy and the postpartum period. Journal of Obstetrics and Gynaecology Canada 25, 516-529 [DOI] [PubMed] [Google Scholar]
- Dempsey J.C., Sorensen T.K., Williams M.A., Lee I.M., Miller R.S., Dashow E.E., Luthy D.A. (2004) Prospective study of gestational diabetes mellitus risk in relation to maternal recreational physical activity before and during pregnancy. American Journal of Epidemiology 159, 663-670 [DOI] [PubMed] [Google Scholar]
- Dempsey J.C., Butler C.L., Williams M.A. (2005) No need for a pregnant pause: physical activity may reduce the occurrence of gestational diabetes mellitus and preeclampsia. Exercise and Sport Sciences Reviews 33(3), 141-149 [DOI] [PubMed] [Google Scholar]
- Evenson K.R., Savitz D.A., Huston S.L. (2004) Leisure-time physical activity among pregnant women in the US. Paediatric and Perinatal Epidemiology 18, 400-4007 [DOI] [PubMed] [Google Scholar]
- Goodwin A., Astbury J., McMeeken J. (2000) Body image and psychological well-being in pregnancy. A comparison of exercisers and non-exercisers. Australian and New Zealand Journal of Obstetrics and Gynaecology 40, 422-447 [DOI] [PubMed] [Google Scholar]
- Hall D.C., Kaufmann D.A. (1987) Effects of aerobic and strength conditioning on pregnancy outcomes. American Journal of Obstetrics and Gynecology 157, 1199-1203 [DOI] [PubMed] [Google Scholar]
- Irwin D.E., Savitz D.A., Andre K.A., Hertz-Picciotto I. (1994) Study of occupational risk factors for pregnancy-induced hypertension among active duty enlisted Navy personnel. American Journal of Industrial Medicine 25, 349-359 [DOI] [PubMed] [Google Scholar]
- Kardel K.R., Kase T. (1998) Training in pregnant women: effects on fetal development and birth. American Journal of Obstetrics and Gynecology 178, 280-286 [DOI] [PubMed] [Google Scholar]
- Krans E.E., Gearhart J.G., Dubbert P.M., Klar P.M., Miller A.L., Replogle W.H. (2005) Pregnant women’s beliefs and influences regarding exercise during pregnancy. Journal of the Mississippi State Medical Association 46(3), 67-73 [PubMed] [Google Scholar]
- Leiferman J.A., Evenson K.R. (2003) The effect of regular leisure physical activity on birth outcomes. Maternal and Child Health Journal 7, 59-64 [DOI] [PubMed] [Google Scholar]
- Lokey E.A., Tran Z.V., Wells C.L., Myers B.C., Tran A.C. (1991) Effects of physical exercise on pregnancy outcomes: a meta-analytic review. Medicine and Science in Sports and Exercise 23, 1234-1239 [PubMed] [Google Scholar]
- Lynch A.M., McDonald S., Magann E.F., Evans S.F., Choy P.L., Dawson B., Blanksby B.A., Newnham J.P. (2003) Effectiveness and safety of a structured swimming program in previously sedentary women during pregnancy. Journal of Maternal-Fetal and Neonatal Medicine 14(3), 163-169 [DOI] [PubMed] [Google Scholar]
- MacPhail A., Davies G.A., Victory R., Wolfe L.A. (2000) Maximal exercise testing in late gestation: fetal responses. Obstetrics and Gynecology 96, 565-570 [DOI] [PubMed] [Google Scholar]
- Marcoux S., Brisson J., Fabia J. (1989) The effect of leisure time physical activity on the risk of pre-eclampsia and gestational hypertension. Journal of Epidemiology and Community Health 43, 147-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez-Sterling S., Perry A.C., Kaplan T.A., Halberstein R.A., Signorile J.F. (2000) Physical and psychological changes with vigorous exercise in sedentary primigravidae. Medicine and Science in Sports and Exercise 32, 58-62 [DOI] [PubMed] [Google Scholar]
- Morris S.N., Johnson N.R. (2005) Exercise during pregnancy: a critical appraisal of the literature. Journal of Reproductive Medicine 50(3), 181-188 [PubMed] [Google Scholar]
- Paisley T.S., Joy E.A., Price R.J. (2003) Exercise during pregnancy: a practical approach. Current Sports Medicine Reports 2, 325-330 [DOI] [PubMed] [Google Scholar]
- Pate R.R., Pratt M., Blair S.N., Haskell W.L., Macera C.A., Bouchard C., Buchner D., Ettinger W., Health G.W., King A.C., Kriska A., Leon A.S., Marcus B.H., Morris J., Paffenbarger R.S., Patrick K., Pollock M.L., Rippe J.M., Sallis J., Wilmore J.H. (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Journal of the American Medical Association 273, 402-407 [DOI] [PubMed] [Google Scholar]
- Petersen A.M., Leet T.L., Brownson R.C. (2005) Correlates of physical activity among pregnant women in the United States. Medicine & Science in Sports & Exercise 37, 1748-1753 [DOI] [PubMed] [Google Scholar]
- Pivarnik J.M., Chambliss H.O., Clapp J.F., Dugan S.A., Hatch M.C., Lovelady C.A., Mottola M.F., Williams M.A. (2006) Impact of physical activity during pregnancy and postpartum on chronic disease risk. Medicine & Science in Sports & Exercise 38, 989-1006 [DOI] [PubMed] [Google Scholar]
- Poudevigne M.S., O’Connor P.J. (2006) A review of physical activity patterns in pregnant women and their relationship to psychological health. Sports Medicine 36, 19-38 [DOI] [PubMed] [Google Scholar]
- Saftlas A.F., Logsden-Sackett N., Wang W., Woolson R., Bracken M.B. (2004) Work, leisure-time physical activity, and risk of preeclampsia and gestational hypertension. American Journal of Epidemiology 160, 758-765 [DOI] [PubMed] [Google Scholar]
- Simons-Morton D.G., Calfas K.J., Oldenburg B., Burton N.W. (1998) Effects of interventions in health care settings on physical activity or cardiorespiratory fitness. American Journal of Preventive Medicine 15, 413-430 [DOI] [PubMed] [Google Scholar]
- Sorensen T.K., Williams M.A., Lee I.M., Dashow E.E., Thompson M.L., Luthy D.A. (2003) Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension 41, 1273-1280 [DOI] [PubMed] [Google Scholar]
- Stafford R.S., Blumenthal D. (1998) Specialty differences in cardiovascular disease prevention practices. Journal of the American College of Cardiology 32, 1238-1243 [DOI] [PubMed] [Google Scholar]
- Stevenson L. (1997) Exercise in pregnancy. Part 2: Recommendations for individuals. Canadian Family Physician 43, 107-111 [PMC free article] [PubMed] [Google Scholar]
- Yeo S., Steele N.M., Chang M.C., Leclaire S.M., Ronis D.L., Hayashi R. (2000) Effect of exercise on blood pressure in pregnant women with a high risk of gestational hypertensive disorders. Journal of Reproductive Medicine 45(4), 293-298 [PubMed] [Google Scholar]
- Zeanah M., Schlosser S.P. (1993) Adherence to ACOG guidelines on exercise during pregnancy: effect on pregnancy outcome. Journal of Obstetric, Gynecologic, and Neonatal Nursing 22, 329-335 [DOI] [PubMed] [Google Scholar]


