Abstract
Objective
Several studies have provided prevalence estimates of posttraumatic stress disorder (PTSD) related to the September 11, 2001 (9/11) attacks in broadly affected populations, although without sufficiently addressing qualifying exposures required for assessing PTSD and estimating its prevalence. A premise that people throughout the New York City area were exposed to the attacks on the World Trade Center (WTC) towers and are thus at risk for developing PTSD has important implications for both prevalence estimates and service provision. This premise has not, however, been tested with respect to DSM-IV-TR criteria for PTSD. This study examined associations between geographic distance from the 9/11 attacks on the WTC and reported 9/11 trauma exposures, and the role of specific trauma exposures in the development of PTSD.
Methods
Approximately 3 years after the attacks, 379 surviving employees (102 with direct exposures, including 65 in the towers, and 277 with varied exposures) recruited from 8 affected organizations were interviewed using the Diagnostic Interview Schedule/Disaster Supplement and reassessed at 6 years. The estimated closest geographic distance from the WTC towers during the attacks and specific disaster exposures were compared with the development of 9/11–related PTSD as defined by the Diagnostic and Statistical Manual, Fourth Edition, Text Revision.
Results
The direct exposure zone was largely concentrated within a radius of 0.1 mi and completely contained within 0.75 mi of the towers. PTSD symptom criteria at any time after the disaster were met by 35% of people directly exposed to danger, 20% of those exposed only through witnessed experiences, and 35% of those exposed only through a close associate’s direct exposure. Outside these exposure groups, few possible sources of exposure were evident among the few who were symptomatic, most of whom had preexisting psychiatric illness.
Conclusions
Exposures deserve careful consideration among widely affected populations after large terrorist attacks when conducting clinical assessments, estimating the magnitude of population PTSD burdens, and projecting needs for specific mental health interventions.
Keywords: September 11 attacks, posttraumatic stress disorder, trauma exposure, disaster, disaster mental health services
Effective disaster mental health planning and response depend on accurate information about the numbers of people who will need distinct types of services. In large-scale disasters (eg, the September 11, 2001 [9/11] terrorist attacks) affecting large populations, estimated proportions may translate into tens and hundreds of thousands of people needing services. Based in part on the shocking nature of the 9/11 attacks on civilians, the mental health consequences were expected to be profound and far reaching, affecting people throughout the New York City (NYC) area and across the United States, who were the terrorists’ psychological target.1
Remarkably, the first 9/11 mental health research studies of affected populations were conducted within several days to weeks after the attacks through the use of telephone random digit dial2–5 and predisaster panel sampling methods.6,7 Measured at 2 to 3 years or longer after the disaster, current 9/11–related posttraumatic stress disorder (PTSD) prevalence was estimated to be 15% to 20% among highly exposed samples such as evacuees from the World Trade Center (WTC) towers and other damaged buildings and other people in close proximity during the attacks.8–11 Information also is needed on all of the expected cases, not only chronic cases 2 to 3 years later, for public health planning and provision of treatment for PTSD in such highly exposed populations. In more broadly affected populations, estimates of current PTSD in the first postdisaster months were considerably lower, 8% to 11% among residents of NYC2–4,7 and 4% among national US samples.7 A “probable PTSD” prevalence estimate in the NYC borough of Manhattan decreased from 7.5% 1 month after the attacks to 0.6% 6 months after the attacks.4 This 92% remission rate in 5 months is uncharacteristic of the course of PTSD in other studies of major disasters and in other populations,12–19 suggesting that these estimates may have captured substantial numbers of individuals with symptoms that are not consistent with PTSD assessed using full diagnostic criteria.
A premise of the NYC population studies was that people throughout the area were exposed to the attacks and thus are at risk for developing PTSD.20 This premise has important implications for both prevalence estimates and service provision; it has not, however, been tested with respect to the Diagnostic and Statistical Manual, Fourth Edition, Text Revision (DSM-IVTR) criteria for PTSD. Indeed, on the day of the event, widespread anxiety was evident throughout the metropolitan region, as clouds of dust spread across a wide part of NYC. Communication among families and friends was limited by a breakdown of telephone and other systems, and information was available mainly by radio or television and not always reliable. Although the 9/11 terrorist attacks constituted an undeniable traumatic event, this is not sufficient for the diagnosis of PTSD; a qualifying exposure to the traumatic event is also necessary for consideration of this diagnosis. Even when a mass trauma is profound enough to merit national significance, exposure cannot be assumed; it must be determined on a case-by-case basis.
The present study examines the disaster trauma exposure and its relation to PTSD in a sample of 379 employees of 8 NYC organizations with a range of exposures, including evacuees from the WTC towers and others in the adjacent vicinity. This study uniquely combined assessment of PTSD according to full DSM-IV-TR criteria with detailed data about geographical proximity and specific experiences of the 9/11 WTC attacks for determination of qualifying trauma exposure. Specific research questions were how does distance from the towers relate to disaster exposures? And how do exposures relate to the development of PTSD? This is the largest WTC study to date that has used full diagnostic assessment methods, and one of the few disaster studies of this size ever conducted using a full diagnostic instrument.
METHODS
Approximately 3 years (median 35 months, range 27–52 months) after the 9/11 terrorist attacks, study participants provided informed consent and completed structured interviews assessing detailed disaster exposure information and incidence of PTSD during the interim since the attacks. A follow-up assessment was conducted at approximately 6 years (median 72 months, range 65–93 months) postdisaster (median interinterview interval 36 months, range 18–63 months). Participants were offered a $75 payment or a donation to a fund to assist disaster victims. Human studies approval for the study was obtained from the cooperating academic institutions.
Sample
As detailed in Table 1, participants were recruited from 8 organizations substantially affected by the attacks, including 176 from companies located in the WTC towers and 203 from organizations not located in the towers. Participating organizations distributed information about the study to their employees. Potential respondents contacted the research staff to inquire about or enroll in the study or both. Summary demographics for all of the employees on September 11, 2001, were obtained for the 2 large WTC companies only and were compared with sample demographics of participants from those 2 companies to estimate demographic representativeness of these 2 groups with high exposure levels. The 166 participants from these 2 companies represented 17% of these companies’ combined 994 employees; participants had more female representation compared with all of the employees (58% vs 45%; χ2=10.54, df 1, P<.001) but did not differ in age, ethnicity, education, or marital status.
TABLE 1.
Sample Characteristics
| % (n/N) | Mean (SD) | Median | Range | Description | |
|---|---|---|---|---|---|
| (Organization) No. participants | |||||
| (1) 187 | Large WTC company located above strike zone, nearly 200 employees loss | ||||
| (2) 79 | Large WTC company located in mid-level floors, 1 employee loss | ||||
| (3) 10 | Smaller WTC company located in lower floors with 0 employee losses | ||||
| (4) 39 | Organization within 2 blocks, with damage from planes hitting towers | ||||
| (5) 52 | Airline company, with losses of employees, passengers, and equipment | ||||
| (6) 25 | Utility company (Ground Zero response) | ||||
| (7) 27 | Disaster response agency | ||||
| (8) 60 | Disaster response agency | ||||
| Male sex | 47 (179/379) | ||||
| Ethnic/racial group | |||||
| White | 71 (266/374) | ||||
| Black | 15 (58/374) | ||||
| Hispanic | 8 (29/374) | ||||
| Asian/Pacific Islander | 5 (18/374) | ||||
| Other | 1 (3/374) | ||||
| Marital status | |||||
| Married | 51 (195/379) | ||||
| Divorced | 13 (51/379) | ||||
| Separated | 3 (10/379) | ||||
| Widowed | 2 (6/379) | ||||
| Never married | 31 (117/379) | ||||
| Age, y | 45.2 (11.1) | 44 | 21–80+ | ||
| Level of education | |||||
| College degree | 67 (250/375) | ||||
| Graduate degree | 39 (147/375) | ||||
| Years of education | 16.6 (3.1) | 16 | 10–29 |
SD=standard deviation; WTC=World Trade Center.
At follow-up, 228 (60%) of the participants were reinterviewed, including 49 (75%) of the WTC tower evacuees. Follow-up success was not associated with sex, marital status, predisaster psychopathology, PTSD symptom criteria met, or any postdisaster diagnosis (P>.05 for all comparisons), but it was significantly associated with nonminority ethnic status (65% vs 50%; χ2=6.99, df 1, P=.008), college education (64% vs 52%; χ2=5.00, df 1, P=.025), and having a DSM-IV-TR–qualifying 9/11 trauma exposure (68% vs 54%; χ2=7.92, df 1, P=.005).
Assessment
The Diagnostic Interview Schedule (DIS) for DSM-IV21 modules for PTSD, major depression, panic disorder, generalized anxiety disorder, and alcohol and drug use disorders were administered by mental health professionals who were formally trained on this interview. The DIS has been demonstrated to possess acceptable diagnostic reliability and validity22–26 and has been extensively used in studies of disasters.27–32 Diagnosis of PTSD using the DSM-IV-TR criteria33 requires determination of exposure to a traumatic event (PTSD criterion A) and PTSD symptoms related to qualifying exposures to the event in 3 categories (PTSD criterion B for intrusive reexperiencing, C for avoidance and numbing, and D for hyperarousal) that were new after the event, lasted for more than 1 month (criterion E), and were associated with clinically significant distress or impaired functioning (criterion F). Criterion A defines traumatic events, which involve a physical threat to life or limb through qualifying exposures, which may occur in 3 ways: physical endangerment involving “direct personal experience of an event that involves actual or threatened death or serious injury,” “witnessing an event that involves death, injury, or a threat to the physical integrity of another person,” or “learning about unexpected or violent death, serious harm, or threat of death or injury experienced by a [close] family member or other close associate” (page 463). For this study, therefore, “witnessing” the 9/11 attacks was counted only if it was an in-person, eyewitness exposure (not including viewing media images such as television coverage as forms of witnessing), and “close associate” was limited to only nuclear family members, “close” family members, or associates who were considered a “best friend” or a “close friend.” The DIS was modified to key the occurrence of disorders to the time of the attacks, allowing assessment of predisaster, postdisaster, and current prevalence of psychiatric disorders.
The DIS Disaster Supplement34 assessed DSM-IV-TR– qualifying 9/11 trauma exposures: physical endangerment (by planes striking the towers and collapse of the towers, while fleeing the falling towers and debris, or documented by physical injury in the attacks); witnessing injury to others either during the attacks or during the aftermath at the Ground Zero site during the recovery operation (eg, people falling from the towers, people with severe injuries, dead bodies and body parts); and through exposures of close associates (ie, immediate family members/close friends). Participants provided their geographic locations (eg, nearest estimated street and cross street) at 4 specific time points: during the times the planes struck the towers (8:46 am and 9:03 am) and when the towers collapsed (9:59 am and 10:28 am). These 4 time points reported by participants provide objective anchors in their memories, similar to the salient memories of where people were on learning that President John F. Kennedy had been assassinated.35
Geographical proximity to the attacks was represented by calculation of the nearest reported location to the WTC towers during the attacks. For a few participants who were unaware of the unfolding disaster even at times that they were close to the disaster, such as those below ground in subways, the closest location they reported when they were aware of the attacks was counted as their nearest location. Specific exposure types were tabulated and hierarchically ordered by hypothesized severity, following the order of DSM-IV-TR–qualifying PTSD criterion A exposure types (direct exposure to danger first, directly witnessing danger second, and exposure through close associates third).
Statistical Analysis
For the statistical analysis we used SAS 9.2 (SAS Institute, Cary, NC) and for the geographic computation of distances we used ArcGIS version 9.3 (Esri, Redlands, CA). Categorical variables were compared using 2-sided χ2 analyses, substituting Fisher exact tests when expected cell sizes were <5 observations. The non-parametric Mann-Whitney test was used for comparison of dichotomous and numerical variables for non-normally distributed data.
To explore the first research question, reported disaster exposures were examined in relation to distance from the WTC towers during the attacks. The median distance within which most of the physical or directly witnessed exposures to danger were reported was selected as a perimeter within which all were considered likely to have DSM-IV-TR–qualifying direct exposures to 9/11 trauma. It was hypothesized that reported exposures within this zone differed from experiences reported outside it, and that exposures differed between those inside and outside the towers within a 0.1-mi radius. The second research question was addressed by comparing symptom criteria for PTSD among exposure groups and examining features of cases without DSM-IV-TR–qualifying exposures that met full PTSD symptom criteria B through F related to the 9/11 attacks.
RESULTS
Sample Characteristics
Table 1 provides demographics of the sample, which was approximately equal in gender representation, predominantly white, and well educated; approximately half were married, and the average age was the mid-40s. The median distance from the towers among those outside the towers was 5.2 mi (9 were > 1000 mi away; maximum distance was 3470 mi).
Specific Disaster Exposures and Geographic Proximity the WTC Towers During the 9/11 Attacks
Direct physical exposure to danger was identified among 65 participants in the towers and another 17 outside the towers but within 0.1 mi (approximately 1 block), where they were endangered by the planes striking the towers and the towers collapsing (n=82). Outside the 0.1-mi perimeter, another 20 (all within 0.75 mi of the towers) reported endangerment by planes striking the towers or the towers collapsing, fleeing the falling towers and debris, or sustaining physical injuries in the attacks. These 102 individuals were classified as physically exposed to danger in the attacks (Table 2).
TABLE 2.
Proportions Meeting PTSD Symptom Criteria by Disaster Exposure Group Hierarchy
| Disaster Exposure Group | Met PTSD Symptom Criteria, % (n/N) |
|---|---|
| Direct physical exposure to danger | 35.3 (36/102) |
| Witnessed exposure only (not physically endangered) | 19.5 (8/41)* |
| Eyewitness to disaster only (not physically endangered) | 21.1 (4/19) |
| Witnessed disaster aftermath only (not physically endangered, not eyewitness to the attacks) | 18.2 (4/22) |
| Exposure through close associate (not physically endangered, not exposed via witnessing attacks or aftermath) | 34.6 (9/26)† |
| Any of these exposures (meeting PTSD criterion A) | 31.4 (53/169) |
| None of these exposures (not meeting PTSD criterion A) | 12.0 (25/209) |
PTSD=posttraumatic stress disorder.
Compared with those physically endangered, χ2=3.42, df 1, P=.064.
Compared with those physically endangered, χ2=.56, df 1, P=.454.
Personally witnessing people falling from the towers or seeing seriously injured people or dead bodies during the attacks (n=85) and witnessing the gruesome aftermath of the Ground Zero disaster site, where dead bodies and body parts were encountered (n=24 response/recovery workers), were classified as directly witnessed trauma exposures. The groups with these witnessed exposures overlapped with each other and with those physically exposed to danger during the attacks. Of those not physically exposed to danger in the attacks, 19 reported eyewitness exposures to the attacks and another 22 without eyewitness exposures to the attacks witnessed the aftermath.
Exposure through a close associate’s direct exposure to the attacks was reported by 57 participants, including 54 whose close associates died and another 3 whose close associates survived. Among those not physically exposed to danger or directly witnessing the attacks or the aftermath, 26 were exposed only through a close associate’s exposure.
In summary, 169 (45% of the sample) had a DSM-IV-TR–qualifying exposure. Of these, 102 were physically exposed to danger in the attacks, another 41 not physically endangered were exposed through directly witnessing the attacks or the Ground Zero aftermath, and another 26 were exposed only through the exposure of a close associate.
The maximum nearest distance to the towers among those reporting endangerment by planes striking the towers or the towers collapsing, fleeing the falling towers and debris, or sustaining physical injuries ranged from 0.60 to 0.77 mi; the median nearest distance for these exposures, however, was inside the towers (0.0 mi). The maximum distance reported for seeing people falling from the towers was 1.5 mi, but the median distance was 0.09 mi. The maximum distance reported for seeing seriously injured people/dead bodies was 11.6 mi, but the median distance was inside the towers (0.0 mi). Thus, the typical distance for reporting direct exposures to danger or directly witnessing trauma was ≤.1 mi.
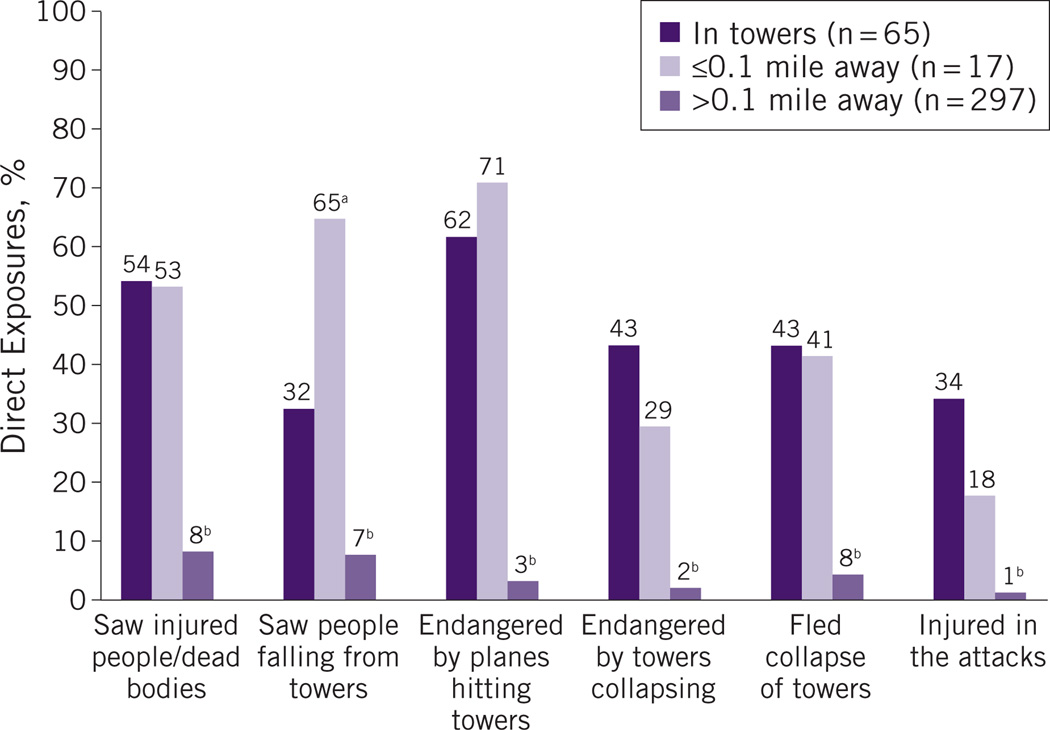
Figure 1 shows the proportions of the sample who reported specific exposures to the attacks among those inside the towers, those within 0.1 mi of the towers, and those at distances beyond 0.1 mi. Injuries in the attacks were sustained by 34% of those inside the towers and 18% of those outside the towers but within 0.1 mile. More than half of those within 0.1 mile (including those inside the towers) reported being endangered when the planes struck the towers and also seeing dead or injured people. Compared to people inside the towers, more of those outside the towers but within 0.1 mile reported seeing people falling from the towers (because those outside had a less-obstructed view). People beyond 0.1 mi from the towers had significantly lower proportions on every reported exposure in Figure 1 compared to those within the 0.1-mi radius.
Figure 1.
Exposures to the attacks by geographic location relative to World Trade Center towers.
aCompared with those in towers, P ≤.05.bCompared with all of those within 0.1 mi (both inside and not inside towers), P ≤.001.
PTSD Symptom Criteria in Relation to Exposures
Meeting PTSD symptom criteria was not associated with sex, number of months since the 9/11 attacks, or interview date at baseline or follow-up (P> .05 for all of these comparisons);PTSD analyses were not controlled for these variables. Among those individuals not located within 0.1 mile of the towers, meeting PTSD symptom criteria was not associated with distance from the towers (Mann-Whitney z=−1.55, P=.123). Thus, geographical distance did not predict PTSD symptom criteria beyond a short distance from the towers.
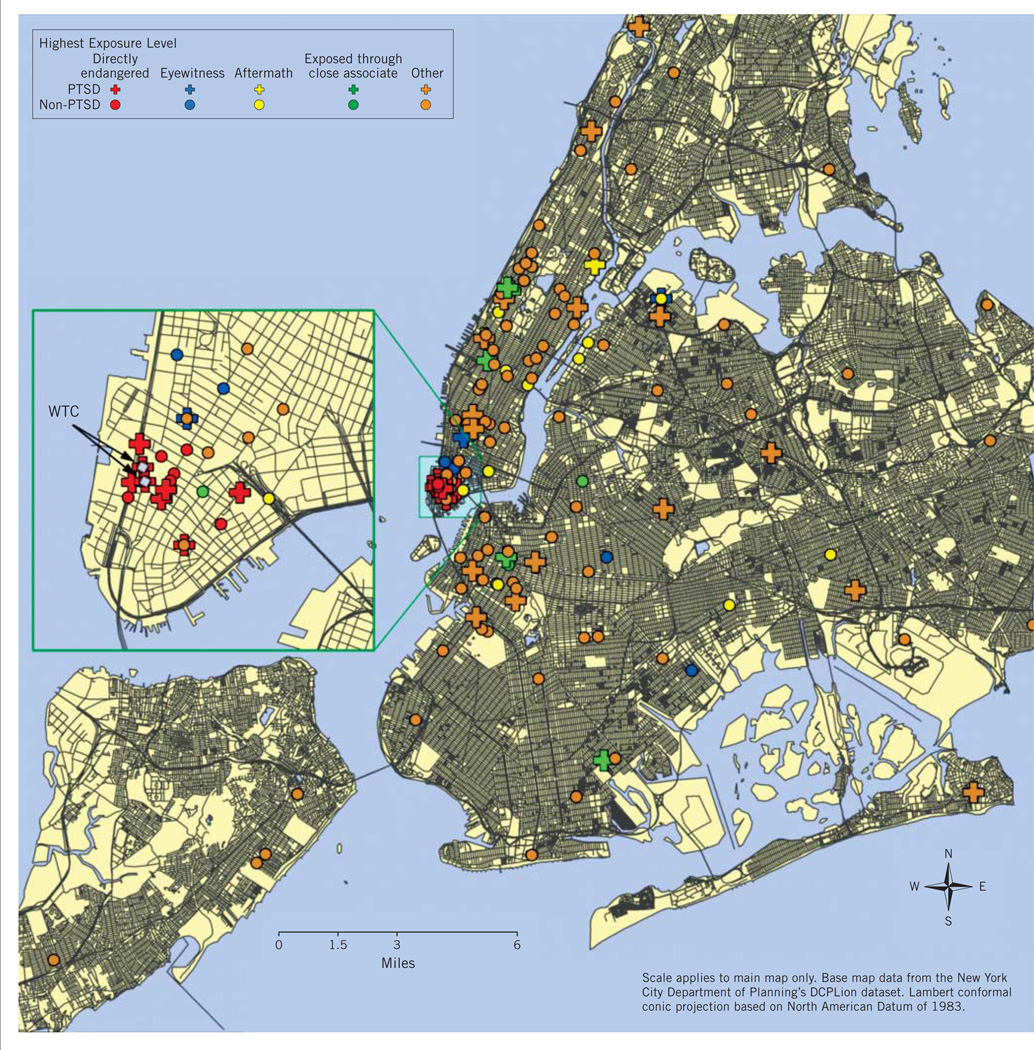
Table 2 shows the proportions of those who met PTSD symptom criteria according to hierarchical exposure level. PTSD symptom criteria were met by 35% of those physically exposed to danger through location either in the towers or in the near vicinity during the attacks (23/65 of those in the towers and 13/37 of those exposed to danger outside the towers). Among others without these direct physical exposures to danger, PTSD symptom criteria were met by 20% of those exposed through directly witnessing danger. Of those without any of the above exposures, PTSD symptom criteria were met by 35% of those exposed through direct exposure of a close associate, representing 4% of participants without exposures through direct endangerment or witnessing danger. Figure 2 depicts the nearest geographical locations of participants who met vs participants who did not meet PTSD symptom criteria, color coded by highest exposure level.
Figure 2.
Nearest geographic locations to World Trade Center (WTC) towers during the attacks among those who met and who did not meet posttraumatic stress disorder (PTSD) symptom criteria, by exposure group hierarchy.
The proportion of the sample that met PTSD criteria was non-significantly higher among those directly exposed to physical danger during the attacks than among others with witnessed exposures but not endangerment, and was equivalent to the proportion among those exposed only through a close associate’s exposure (Table 2). Among the group directly exposed to danger during the attacks, report of additional eyewitnessed experiences during the attacks was associated with higher rates of PTSD symptom criteria (47%, 31/66 vs 14%, 5/36 of others without eyewitnessed exposures; χ2=11.16, df 1, P<.001). Additional exposure through a close associate’s direct exposure, however, did not increase the likelihood of meeting PTSD criteria among those physically endangered (χ2=0.16, df 1, P=.692). Conventional statistical significance testing demonstrated that the 3 main exposure types did not differ in the proportions that met PTSD symptom criteria, but among those directly exposed to danger, additional eyewitness exposures (of people falling from the towers or dead/injured people) significantly added to the likelihood of meeting PTSD symptom criteria.
Of those with PTSD, 40% (21/52) had achieved remission at baseline (approximately 3 post-9/11 years), yielding 19% with current PTSD. At follow-up (approximately 6 post-9/11 years), 59% (24/41) had achieved remission, yielding 15%with current PTSD.
Among those without clear DSM-IV-TR–qualifying 9/11 trauma exposures, 40 people reported that they saw the planes hitting the towers, the towers burning, or the towers collapsing at distances between 0.15 and 13 (median 3.0) mi; 4 of these individuals met PTSD symptom criteria. An additional 21 people without known qualifying exposures or who did not see the planes or the towers being attacked met PTSD symptom criteria, at distances between 2.3 and 48 (median 7.0) mi. Of these 25 individuals meeting symptom criteria without qualifying exposures, 20 (80%) had a predisaster psychiatric disorder (compared with 25 of 48 [53%] of those with direct exposure to danger; χ2=4.74, df 1, P=.029). Of the remaining 5, 3 knew someone who was killed, 1 was 1.9 mi away, and 1 was 3.4 mi away but worked with families of 9/11 victims.
COMMENT
PTSD, Trauma Exposures, and Geographic Distance
To our knowledge, the present study is the only one to have examined specific DSM-IV-TR–defined exposures to the 9/11 attacks and emergence of the PTSD symptom complex in relation to these exposures. This was made possible by combining full diagnostic assessment with a range of trauma exposures in the sample, including substantial representation of the most intensely exposed subgroup—those in the towers and nearby.
The postdisaster prevalence rate of PTSD in the first 3 years after the terrorist attacks was 35% of those in the towers or nearby who were directly exposed to physical danger in the attacks, a finding that is remarkably consistent with the 34% PTSD incidence identified among directly exposed survivors of the 1995 Oklahoma City bomb blast in the first 6 months13 using the same assessment tool. It is also consistent with the weighted 34% PTSD estimate at 1 to 2 months postdisaster by Galea et al4 among 10 individuals in the towers during the attacks. These findings collectively suggest that among highly exposed survivors of severe terrorist incidents, one-third may be expected to develop PTSD.
The zone of direct physical exposure to the WTC attacks clearly includes the area where people were injured and could see other people being injured and killed—a radius of about 0.1 mi (approximately 1 block)—with complete containment of exposure within 0.75 mi. Beyond the 0.1-mi perimeter, distance was not associated with meeting PTSD symptom criteria. Rather than functioning as a continuous variable with exposure level gradually fading with increasing distance from the towers, distance effectively functioned as a dichotomous indicator of direct exposures, with the dividing point being close to the towers. An important yet somewhat intuitive finding of the present study was that a qualifying exposure for PTSD through physical endangerment or direct witnessing of injury/death requires close geographical proximity to the incident. It is therefore unlikely that widespread PTSD-qualifying trauma exposure through direct or witnessed endangerment occurred in populations geographically distant from the 9/11 attack sites. Regardless, it is likely that some people geographically distant may have had PTSD-qualifying exposures through close associates who were victims of the disaster.
The PTSD symptom complex was largely confined to a circumscribed group of individuals with DSM-IV-TR–qualifying trauma exposures: those directly exposed to danger or witnessing endangerment to others in close geographic proximity to the site of the attacks and those exposed through endangerment of close associates. Outside these exposure groups, few possible sources of exposure were evident among the few individuals who were symptomatic, most of whom had preexisting psychiatric illness. These findings support and provide operationalization for the Galea group’s argument that “PTSD, which nosologically requires linkage to exposure, may not be plausibly present in distant populations (eg, general US samples) after a disaster in New York City but may well be plausible in areas closer to the disaster site” (page 130),20 which the present study identified as areas mostly within about 1 block of Ground Zero.
Previous 9/11-related studies have included loss of possessions, job loss, and death of friends or relatives resulting from the attacks as disaster exposures,20 but these represent largely nonqualifying trauma exposures for a DSM-IV-TR PTSD diagnosis. In the present study, 80% of those who said they knew someone who had been killed in the attacks did not have a close associate killed, as DSM-IV-TR criteria require for indirect exposure. Although one-third of people across most of Manhattan reported that they “directly witnessed” the attacks,2 data from the present study suggest that beyond a short distance, seeing the planes or towers during the attacks—which were visible from many miles away—was not a realistic source of PTSD among previously mentally healthy people.
Measurement and Sampling Issues
A strength of the present study was the use of structured diagnostic interviews and full DSM-IV-TR criteria to assess PTSD, which other studies of the 9/11 attacks on the WTC have not provided. The present study also provided prevalence of both current and remitted PTSD and predisaster psychiatric disorders. Prior prevalence studies conducted 2 to 6 years postdisaster have reported only current prevalence and not all of the PTSD cases that occurred after the disaster.8–11 PTSD cases that may have already resolved during that time were thus not addressed and not detected, which in the present study represented 40% of cases at 3 years and nearly 60% at 6 years. Estimates made years after a disaster that are limited to current prevalence may underrepresent the amount of all postdisaster PTSD. The present study’s estimate of all PTSD among 9/11-exposed groups, although likely to represent an underestimate based on the retrospective assessment, provides a starting point for projecting treatment needs for all of the PTSD that may be expected after future terrorist attacks.
Current PTSD prevalence at 2 to 3 years in previous 9/11 studies was estimated at 15% of WTC evacuees,11 21% of occupants of buildings damaged by the 9/11 attacks or on the street nearby (about 0.3 mi),9 and 17% of office workers and 19% of people in transit south of Chambers Street (increasing to 19% and 23%, respectively, at 5–6 years).8 These rates are similar to the 19% current PTSD prevalence at 3 years and 15% current PTSD prevalence at 6 years in the present study.
Most published 9/11 studies estimating PTSD prevalence have relied on PTSD symptom scales that do not link symptoms to specific diagnosis-qualifying exposures.8–10 By definition, posttraumatic symptoms must be anchored to a qualifying trauma exposure to be considered contributory to PTSD.36 Symptom scales applied without assessment of trauma exposure may count symptoms unrelated to trauma exposure and cannot accurately estimate PTSD incidence. This problem is magnified in populations with low exposure levels and thus low PTSD risk,37 such as geographically broad 9/11-affected populations, yielding gross overestimates of PTSD prevalence. McDonald and Calhoun37 cautioned that inappropriate use of symptom checklists as diagnostic tools “can lead to inaccurate diagnosis, unnecessary intervention or missed opportunities to treat, a spoiling of the PTSD data base, and misaligned clinical resource management”(page 985).Symptom checklists may thus function especially poorly in the assessment ofDSM-IV-TRcriteria in populations with low exposure.
The present study demonstrated that in low-exposure populations, measurement of symptoms without assessing whether individual exposures qualify may identify a number of symptomatic individuals who cannot by definition meet PTSD criteria. In large populations, even small proportions of cases like these could translate into substantial numbers (tens to hundreds of thousands) of cases incorrectly estimated to have PTSD, easily producing 10-fold overestimates of numbers of people with mental health services needs.37 People without sufficient exposure to warrant a diagnosis of PTSD or without sufficient symptoms to qualify for this diagnosis may have another psychiatric disorder or other stressors accounting for their symptoms. It is also possible that symptoms among those without a psychiatric disorder may represent nonpathologic subdiagnostic distress,13 which is far more common than PTSD.
This study’s sample recruitment from highly affected organizations may have overrepresented high levels of exposures compared to the average NYC area population. The volunteer nature of the sample and low participation rate may have overrepresented those with severe symptoms that motivated them to participate. The sample also may have underrepresented both those too avoidant or upset to discuss their 9/11 experience among high-exposure groups and those feeling unaffected and consequently not motivated to participate. Obtaining a representative sample was also a problem for the WTC registry,38 representing about 14% (3271/24 015) of all of those estimated to have been in the towers during the attacks, from which major 9/11 mental health studies have obtained research samples.8–10 The barriers to rapid, systematic access to the mostly highly exposed survivor groups, inherent in 9/11 research, are widely recognized.39 Study attrition also introduced potential bias in our follow-up data. The temporal variability in timing of data collection may have reduced the precision of PTSD remission data in particular, although rates of PTSD and PTSD remission were not associated with timing of interviews.
Because the present study’s sample cannot be assumed to be representative of either NYC or 9/11-affected populations, it cannot provide a definitive estimate of 9/11-related PTSD prevalence. The major value of these data are, rather, in the opportunity to study the occurrence of PTSD in relation to objective 9/11 trauma exposures.
Implications for Planning and Delivery of Services
Although this study identified a substantial burden of PTSD among adults highly exposed to a terrorist incident such as the 9/11 attacks, the mental health sequelae among groups outside a narrow geographic exposure zone without exposures through close associates are not as clear. Psychiatric symptoms in these populations may represent problems other than PTSD such as other psychiatric difficulties (eg, major depression, substance abuse, psychiatric symptoms) and substantial emotional distress that has been demonstrated to have considerable prevalence in broadly affected 9/11-affected populations.2,3,5–7 Differentiating distress from PTSD and other psychiatric disorders could help to prevent inappropriate pathologizing of normal responses. These distinctions may have important implications for effective and efficient planning and implementation of appropriate disaster mental health interventions for different conditions: psychiatric treatment tailored for specific psychiatric disorders and other interventions such as psychological first aid and crisis counseling services for distress.40
CONCLUSIONS
Reflecting on a decade of mental health research on the 9/11 attacks, it is clear that the complexities of exposure in the estimation of PTSD present a substantial challenge to researchers to provide accurate information to guide disaster mental health planning. A substantial proportion of people in the present study who were directly exposed to physical danger or exposed through close associates developed PTSD. This PTSD was relatively persistent. Among those outside a small geographic distance from the towers without physical endangerment or witnessed exposures—who by definition cannot be diagnosed as having PTSD unless exposed through directly exposed associates—a small proportion, representing potentially large numbers of people in extended populations, may develop similar symptoms. This raises the question of what such symptoms presenting in the absence of known qualifying exposures for PTSD represent. Further research is needed to provide answers to this question.
This study has clarified the value of fully considering exposures to terrorist attacks when estimating PTSD prevalence, and it has demonstrated these considerations to be especially pertinent in populations outside close geographic proximity to the incident. The importance of examining trauma exposures with precision is relevant for populations with other types of trauma, such as military combat veterans who deserve similar careful consideration of trauma exposures in relation to PTSD.41
Acknowledgments
This research was partially supported by National Institute of Mental Health (NIMH) Grant MH68853 to Dr North and a grant from the National Memorial Institute for the Prevention of Terrorism (MIPT) and the Office of State and Local Government Coordination and Preparedness, US Department of Homeland Security MIPT106-113-2000-020 to Dr Pfefferbaum.
Dr North has received research support from NIAAA, NIDDK, the Department of Veterans Affairs, the American Psychiatric Association, and the Orthopaedic Trauma Association, and consultant fees from the University of Oklahoma Health Sciences Center and from the Tarrant County, TX, Department of Health. Dr Pfefferbaum has received research funding from NIMH and MIPT.
Footnotes
Disclaimer:Points of view in this article are those of the authors and do not necessarily represent the official position of the Department of Veterans Affairs or the US government.
Author Disclosures: The other authors report no conflicts of interest.
REFERENCES
- 1.Silver RC, Holman A, McIntosh DN, et al. Coping with a national trauma: a nationwide longitudinal study of responses to the terrorist attacks of September 11. In: Neria Y, Gross R, Marshall RD, et al., editors. 9/11: Mental Health in the Wake of Terrorist Attacks. New York: Cambridge University Press; 2006. pp. 45–70. [Google Scholar]
- 2.Galea S, Ahern J, Resnick H, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- 3.Galea S, Resnick H, Ahern J, et al. Posttraumatic stress disorder in Manhattan, New York City, after the September 11th terrorist attacks. J Urban Health. 2002;79(3):340–353. doi: 10.1093/jurban/79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea S, Vlahov D, Resnick H, et al. Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. Am J Epidemiol. 2003;158(6):514–524. doi: 10.1093/aje/kwg187. [DOI] [PubMed] [Google Scholar]
- 5.Schuster MA, Stein BD, Jaycox L, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345(20):1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 6.Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nation-wide longitudinal study of psychological responses to September 11. JAMA. 2002;288(10):1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- 7.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 8.Brackbill RM, Hadler JL, DiGrande L, et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302(5):502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- 9.Farfel M, DiGrande L, Brackbill R, et al. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health. 2008;85(6):880–909. doi: 10.1007/s11524-008-9317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiGrande L, Perrin MA, Thorpe LE, et al. Posttraumatic stress symptoms, PTSD, and risk factors among lower Manhattan residents 2–3 years after the September 11, 2001 terrorist attacks. J Trauma Stress. 2008;21(3):264–273. doi: 10.1002/jts.20345. [DOI] [PubMed] [Google Scholar]
- 11.DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. Am J Epidemiol. 2011;173(3):271–281. doi: 10.1093/aje/kwq372. [DOI] [PubMed] [Google Scholar]
- 12.North CS, McCutcheon V, Spitznagel EL, Smith EM. Three-year follow-up of survivors of a mass shooting episode. J Urban Health. 2002;79(3):383–391. doi: 10.1093/jurban/79.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- 14.Grace MC, Green BL, Lindy JL, et al. The Buffalo Creek disaster: a 14-year follow-up. In: Wilson JP, Raphael B, editors. International Handbook of Traumatic Stress Syndromes. New York: Plenum; 1993. pp. 441–449. [Google Scholar]
- 15.McFarlane AC. Posttraumatic stress disorder: a model of the longitudinal course and the role of risk factors. J Clin Psychiatry. 2000;61(Suppl 5):15–20. discussion 21–23. [PubMed] [Google Scholar]
- 16.North CS, Smith EM, Spitznagel EL. Posttraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry. 1994;151(1):82–88. doi: 10.1176/ajp.151.1.82. [DOI] [PubMed] [Google Scholar]
- 17.Breslau N. Outcomes of posttraumatic stress disorder. J Clin Psychiatry. 2001;62(Suppl 17):55–59. [PubMed] [Google Scholar]
- 18.Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. J Abnorm Psychol. 1998;107(3):508–519. doi: 10.1037//0021-843x.107.3.508. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 20.Galea S, Ahern J, Resnick H, et al. Post-traumatic stress symptoms in the general population after a disaster: implications for public health. In: Neria Y, Gross R, Marshall RD, et al., editors. 9/11:Mental Health in the Wake of Terrorist Attacks. New York: Cambridge University Press; 2006. pp. 19–44. [Google Scholar]
- 21.Robins LN, Cottler LB, Compton WM, Bucholz K, North CS, Rourke KM. Diagnostic Interview Schedule for the DSM-IV. DIS-IV. St Louis, Mo: Washington University School of Medicine; 2000. [Google Scholar]
- 22.Ross HE, Swinson R, Doumani S, Larkin EJ. Diagnosing comorbidity in substance abusers: a comparison of the test-retest reliability of two interviews. Am J Drug Alcohol Abuse. 1995;21(2):167–185. doi: 10.3109/00952999509002686. [DOI] [PubMed] [Google Scholar]
- 23.Erdman HP, Klein MH, Greist JH, Bass SM, Bires JK, Machtinger PE. A comparison of the Diagnostic Interview Schedule and clinical diagnosis. Am J Psychiatry. 1987;144(11):1477–1480. doi: 10.1176/ajp.144.11.1477. [DOI] [PubMed] [Google Scholar]
- 24.Goethe JW, Ahmadi KS. Comparison of Diagnostic Interview Schedule to psychiatrist diagnoses of alcohol use disorder in psychiatric inpatients. Am J Drug Alcohol Abuse. 1991;17(1):61–69. doi: 10.3109/00952999108992810. [DOI] [PubMed] [Google Scholar]
- 25.Wittchen HU, Semler G, von Zerssen D. A comparison of two diagnostic methods. Clinical ICD diagnoses vs DSM-III and Research Diagnostic Criteria using the Diagnostic Interview Schedule (version 2) Arch Gen Psychiatry. 1985;42(7):677–684. doi: 10.1001/archpsyc.1985.01790300045005. [DOI] [PubMed] [Google Scholar]
- 26.Helzer JE, Spitznagel EL, McEvoy L. The predictive validity of lay Diagnostic Interview Schedule diagnoses in the general population. A comparison with physician examiners. Arch Gen Psychiatry. 1987;44(12):1069–1077. doi: 10.1001/archpsyc.1987.01800240045007. [DOI] [PubMed] [Google Scholar]
- 27.North CS, Pfefferbaum B, Narayanan P, et al. Comparison of postdisaster psychiatric disorders after terrorist bombings in Nairobi and Oklahoma City. Br J Psychiatry. 2005;186:487–493. doi: 10.1192/bjp.186.6.487. [DOI] [PubMed] [Google Scholar]
- 28.North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry. 2011;68(2):173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- 29.Canino G, Bravo M, Rubio-Stipec M, et al. The impact of disaster on mental health: prospective and retrospective analyses. Int J Ment Health. 1990;19:51–69. [Google Scholar]
- 30.Robins LN, Fishbach RL, Smith EM, et al. Impact of disaster on previously assessed mental health. In: Shore JH, editor. Disaster Stress Studies: New Methods and Findings. Washington, DC: American Psychiatric Association; 1986. pp. 22–48. [Google Scholar]
- 31.North CS, Pfefferbaum B, Vythilingam M, et al. Exposure to bioterrorism and mental health response among staff on Capitol Hill. Biosecur Bioterror. 2009;7(4):379–388. doi: 10.1089/bsp.2009.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 34.North CS, Pfefferbaum B, Robins LN, Smith EM. St Louis, Mo: Washington University School of Medicine; 2001. The Diagnostic Interview Schedule/Disaster Supplement (DIS-IV/DS) [Google Scholar]
- 35.North CS. Approaching disaster mental health research after the 9/11 World Trade Center terrorist attacks. Psychiatr Clin North Am. 2004;27(3):589–602. doi: 10.1016/j.psc.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 36.North CS, Surís AM, Davis M, et al. Toward validation of the diagnosis of posttraumatic stress disorder. Am J Psychiatry. 2009;166:1–8. doi: 10.1176/appi.ajp.2008.08050644. [DOI] [PubMed] [Google Scholar]
- 37.McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD checklist: a critical review. Clin Psychol Rev. 2010;30(8):976–987. doi: 10.1016/j.cpr.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 38.Dolan M, Murphy J, Thalji L, Pulliam P. World Trade Center Health Registry: sample building and denominator estimation. [Accessed April 10, 2011]; http://www.nyc.gov/html/doh/downloads/pdf/wtc/wtc-building-denominator.pdf Published January 2006.
- 39.North CS, Pfefferbaum B, Hong B. Historical perspective and future directions in research on psychiatric consequences of terrorism and other disasters. In: Yuval N, Gross R, Marshall R, et al., editors. September 11, 2001: Treatment, Research and Public Mental Health in the Wake of a Terrorist Attack. New York: Cambridge University Press; 2006. pp. 95–113. [Google Scholar]
- 40.North CS, Hong BA, Pfefferbaum B. P-FLASH: Development of an empirically-based post-9/11 disaster mental health training program. Mo Med. 2008;105(1):62–66. [PubMed] [Google Scholar]
- 41.Dohrenwend BP, Turner JB, Turse NA, et al. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]