Abstract
Participant accrual to research studies is a challenge, and oftentimes advertisements are used to supplement cases ascertained through clinic caseloads and cancer registries. It is unknown however, if cases ascertained through these two sources differ. In this study, we compare self-referred (n=209) versus cancer registry-ascertained participants (n=334) enrolled in FRESH START, a randomized controlled trial promoting a healthy diet and increased exercise among breast and prostate cancer survivors. The two groups were compared on baseline characteristics, adherence, attrition, and outcomes by study arm. Compared to participants enrolled from registries, self-referrals were significantly younger (54.1±10.4 vs. 58.7±10.7 years), more likely to have later-staged disease and to have received chemotherapy (40% vs. 19%), and more likely to report “fighting spirit” coping styles (50% vs. 30%), lower quality-of-life (88.2+15.1 vs. 92.0+12.9), fewer co-morbid conditions (1.87±1.60 vs. 2.24±1.78), and lower consumption of 5 or more daily servings of fruits and vegetables (35% vs. 45%)(p-values <.05). While no differences in behavior change were observed between self-referred and registry-ascertained cases assigned to the tailored intervention arm, this was not the case within the attention control arm. Among those who received the attention control intervention of standardized materials in the public domain, self-referred versus registry-ascertained participants demonstrated significantly greater increases in exercise at 1-year follow-up, and significantly greater increases in fruit and vegetable consumption at both 1- and 2-year follow-up (p-values <.05). Several differences exist between self-referred versus registry-ascertained participants, including motivation to respond to standardized educational materials which appears significantly greater in self-referred populations.
Keywords: patient selection, registries, neoplasms, advertising
Introduction
Recruitment to research trials is challenging (1,2). Fewer than 5% of cancer patients participate in clinical trials (3). Institutional constraints and privacy issues contribute to the costly and labor intensive process of subject recruitment (2). Furthermore, cancer registry policies regarding patient education and physician involvement deter researchers’ ability to notify patients about research opportunities (1,4). These barriers affect recruitment strategies, design, and cost (2).
Researchers may diversify recruitment strategies to expand the subject pool for clinical trials (5). Although recruitment through advertisement has been commonly used for clinical trials targeting diseases, such as diabetes and hypertension, which affect 20-30% of American adults (6,7), to date such means have not been frequently pursued in oncology trials, primarily due to low cancer prevalence (3-4%) (8). However, the Internet now makes it possible to reach cancer survivors (newly-diagnosed and long-term) for clinical trials. The differences between survivors responding to these solicitations, as compared to those recruited from cancer registries, however, are not known. No studies have reported differences in characteristics or outcomes in behavioral interventions among self-referred versus registry-ascertained cancer study subjects, though such differences have been documented in other health conditions (5,9,10). For example, differences in motivation have been observed among people who self-referred to a weight management program versus those ascertained from clinics (11). Furthermore, self-referred problem drinkers were more likely to reduce alcohol consumption with bibliotherapy (self-help) than those identified through at-risk screening (12). Advertisement may yield cost savings by reducing recruitment duration (5), however, such strategies might yield biased samples whose characteristics and study performance are not generalizable to populations of interest (9,10).
We compared cancer survivors accrued from two sources, self-referral and cancer registry, enrolled in a two-arm randomized behavioral lifestyle intervention trial entitled FRESH START, testing the efficacy and durability of sequentially-tailored versus standardized print materials in improving diet and exercise behaviors of breast and prostate cancer survivors (13,14). We hypothesized that compared to participants ascertained from cancer registries, those who self-referred might differ with regard to cancer coping style (i.e., manifest higher proportions of “fighting spirits” vs. “fatalists”), and also have higher levels of interest, readiness and self-efficacy to pursue lifestyle change at baseline. In addition, we speculated that self-referred participants would demonstrate greater levels of adherence once enrolled in the intervention.
Materials and Methods
Subjects
The methods and main outcomes for this trial have been reported elsewhere (13,14). Briefly, potential study participants who were within 9-months of diagnosis with early-stage female breast or prostate cancer (in situ, localized or regional) were identified using two accrual sources: 1) cases rapidly-ascertained through cancer registries with subsequent approval from their oncology care physicians; and 2) self-referrals responding to study flyers, magazine articles, Internet sites, targeted list-serves (e.g. NexCura©, Inc., Seattle, WA), support groups, national meetings, and word-of-mouth. Institutional review boards at all participating institutions approved the study, which complied with the Health Insurance Portability and Accountability Act (HIPAA) guidelines.
From July 2002 through August 2004, a total of 762 survivors responded with interest (42% response rate), provided written consent, and were screened to exclude individuals with medical or physical conditions precluding unsupervised exercise or a high F&V diet.(13,14) Individuals also were excluded if they practiced at least two of the following behaviors: 1) consumption of five or more daily servings of F&Vs; 2) adherence to a diet <30% of energy from fat; and/or 3) participation in over 150 minutes of exercise weekly. After screening, 543 participants were enrolled.
Measures
Participants completed two computer-assisted telephone interviews of 45-55 minutes each at baseline, and at one-and two-year follow-up. Minutes per week of moderate, hard, and very hard exercise of at least five metabolic equivalents (MET – kcal/kg/hr) were captured using the 7-Day Physical Activity Recall (PAR) (15). Servings per day of F&V, and % energy from fat (total and saturated) were derived using the Diet History Questionnaire (DHQ) (16). Additionally, at baseline, the following additional measures were collected: socio-demographic characteristics (treatment, education, and income); cancer coping style (modified Mini-Mental Adjustment to Cancer subscale); barriers to exercise and eating a low-fat, high F&V diet; quality-of-life ([Functional Assessment of Cancer Therapy (FACT-G)]; risk for depression [Center for Epidemiologic Studies of Depression (CESD)]; social support [Duke Social Support Index (DSSI)]; co-morbidity; perceived health; self-efficacy and stage-of-readiness for exercising 150+ minutes/week, eating five or more servings of F&V/day and consuming a low-fat diet; smoking; and weight status (12).
Interventions
The interventions are described in detail elsewhere (13,17,18). Briefly, participants in both groups received a personalized workbook and additional information to improve diet and exercise behaviors. The intervention arm received sequentially-tailored mailed materials over a 10-month period sent as a series of seven newsletters every six weeks for each behavior being addressed. The attention control arm received standardized print materials in the public domain on diet and exercise (13). Both groups also received a brief survey between each mailing.
Statistical Analyses
Self-referred participants were compared to registry participants on variables measured at baseline, 1-year, and 2-year. The 1- and 2-year outcomes included lifestyle practices, adherence, and attrition rates. Differences between self-referred and registry participants on baseline measures, adherence, and attrition rates were tested using t-tests or the chi-square tests, as appropriate. Comparison of the tailored intervention and attention control study arms by self-referral versus registry patients on 1- and 2-year outcome data were tested in separate regression models, one model for each outcome variable and each time point. Logistic regression was used to test for accrual group differences in attainment of each of the three goal behaviors (yes/no); ordinal logistic regression was used to test for a group difference in number of goal behaviors achieved; and the general linear model was used to test for group differences on each of the continuous outcome variables. The following baseline variables were controlled for in all models: study arm, the outcome under study, percent energy from dietary fat, number of servings of F&V, exercise minutes, the number of behaviors already practicing at baseline (0 or 1), gender, race, and social support. All analyses were performed using SAS (version 9.1, 2003, SAS Institute, Cary, NC).
Results
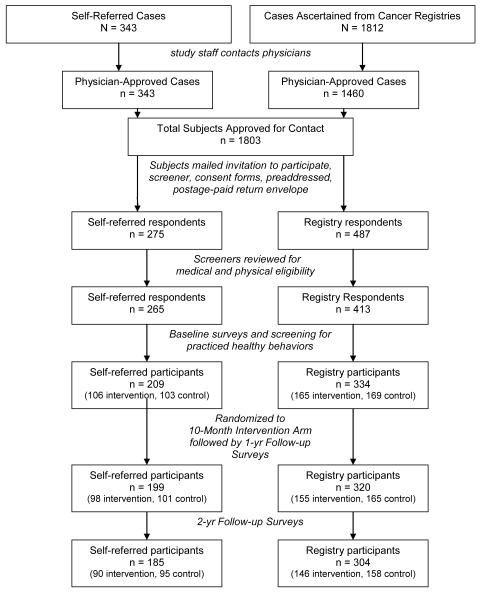
A total of 543 individuals were accrued including 209 self-referred and 334 registry-ascertained. Self-referred subjects were more likely than registry subjects to respond with interest (80% versus 33%, respectively) (p=0.001) (Figure 1). When compared to registry participants, self-referred participants were significantly younger, more likely to have received chemotherapy (owing to more aggressive disease among women with breast cancer), more likely to identify with the “fighting spirit” cancer coping style, more likely to report greater self-efficacy for fat restriction, a greater stage of readiness to exercise and restrict fat, lower quality-of-life, fewer co-morbid conditions, and lesser frequency of eating five or more daily F&Vs (Table 1).
Figure 1.
Cancer survivor participation in FRESH START by accrual source
Table 1.
Characteristics of self-referred vs. registry-solicited participants in the FRESH START trial
| Characteristic | Self-referred (n=209) |
Registry (n=334) |
p-value |
|---|---|---|---|
| Age | |||
| - mean (sd) - range |
54.1 (10.4) 30-75 |
58.7 (10.7) 22-85 |
<.0001 |
| Gender - % (n) | |||
| - male | 39% (81) | 47% (156) | .07 |
| Race - % (n) | |||
| - White - Black - Other |
83% (173) 12% (26) 5% (10) |
83% (279) 14% (46) 3% (9) |
.81* |
| Type/Clinical Cancer Stage % (n) | |||
| - Breast | |||
| -Stage 0 -Stage I -Stage II -Stage IIIA |
8% (10) 44% (56) 41%. (53) 7% (9) |
17% (31) 57% (101) 21% (37) 5% (9) |
<.0001 |
| - Prostate | |||
| -Stage I -Stage II -Unknown |
49% (39) 44% (36) 7% (6) |
35% (55) 57% (88) 8% (13) |
.06† |
| Marital Status- % (n) | |||
| - Single - Married or Stable Union - Divorced or Widowed |
6% (12) 78% (164) 16% (33) |
5% (16) 77% (258) 18% (60) |
.74‡ |
| Education - % (n) | |||
| - ≤ High School Grad - Some College or Associate - College Grad/Post Grad |
9% (19) 29% (61) 62% (129) |
13% (45) 31% (103) 56% (186) |
.09 |
| Income - % (n) | |||
| - <$20K - $20K to <$40K - $40K to $60K - >$60K |
5% (10) 15% (32) 21% (43) 59% (122) |
9% (28) 16% (53) 21% (66) 54% (174) |
.12 |
| Cancer Coping Style (%) | |||
| - Fighting spirit - Fatalistic - Other (cognitive avoider, anxious preoccupier, helpless-hopeless) |
50% (105) 43% (89) 7% (15) |
30% (99) 62% (208) 8% (27) |
.001 |
| Treatment - % (n) | |||
| - Surgery - Radiation Therapy (including brachytherapy) - Chemotherapy - Hormonal Therapy - Other |
84% (175) 46% (97) 40% (83) 39% (82) 5% (11) |
85% (285) 43% (143) 19% (62) 38% (128) 4% (14) |
.62 .41 <.0001 .83 .56 |
| Number of Co-Morbid Factors - mean (sd) | 1.87 (1.60) | 2.24 (1.78) | .01 |
| Risk for Depression (CES-D) – Mean (sd) | 2.84 (4.05) | 2.24 (3.46) | .07 |
| Social Support (DSSI) – Mean (sd) | 27.7 (2.6) | 28.0 (3.7) | .22 |
| Perceived Health - % (n) | |||
| - Good/Excellent - Fair/Poor |
81% (168) 19% (39) |
86% (287) 14% (47) |
.14 |
| Quality of Life (FACT-G) – Mean (sd) | 88.2 (15.1) | 92.0 (12.9) | .002 |
| Self-efficacy for Exercise – Mean (sd) | 3.95 (1.08) | 3.80 (1.12) | .12 |
|
| |||
| Stage of Readiness for Exercise % (n) | |||
| - Precontemplator - Contemplator - Prepared |
12 (5.7) 21 (10.1) 176 (84.2) |
37 (11.1) 34 (10.2) 263 (78.7) |
.05§ |
|
| |||
| Self-efficacy for Fat Restriction – Mean (sd) | 4.05 (0.93) | 3.84 (0.99) | .02 |
|
| |||
| Stage of Readiness for Fat Restriction % (n) | |||
| - Precontemplator - Contemplator - Prepared |
14 (6.7) 7 (3.4) 188 (89.9) |
46 (13.8) 8 (2.4) 280 (83.8) |
.02 |
|
| |||
| Self-efficacy for Eating 5+ fruits & vegetables – Mean (sd) | 4.01 (0.92) | 3.85 (1.06) | .05 |
|
| |||
| Stage of Readiness for Eating 5+ fruits & vegetables % (n) | |||
| - Precontemplator - Contemplator - Prepared |
12 (5.7) 2 (1.0) 195 (93.3) |
32 (9.6) 5 (1.5) 297 (88.9) |
.09 |
|
| |||
| Current Practice of Goal Lifestyle Behaviors | |||
| - 5+ servings of fruits & vegetables/day - <30% calories from fat (<10% from saturated fat) - 150+ minutes of exercise/week - Non-smoker - BMI <25.0 |
35% (74) 8% (16) 12% (25) 96% (200) 37% (77) |
44% (149) 5% (16) 10% (33) 93% (309) 36% (121) |
.03 .17 .45 .15 .88 |
White vs others.
Stage I vs Stage II.
Married vs others.
P-value < .05.
There were no significant associations between accrual source and study arm, adherence, adverse health events, or attrition (drop-outs) at either follow-up time-point. Means (sd) for adherence for self-referred versus registry participants were 5.6 (2.3) and 5.5 (2.3), respectively. Approximately 52% of self-referred participants compared to 55% of registry participants reported at least one health event. Ninety-five percent of participants (regardless of accrual source) completed 1-year of the study, while by 2-years, the rate declined to 89% and 91% for self-referred and registry participants, respectively.
Table 2 presents change scores for frequencies and means (se) from baseline to1-year follow-up by study arm and accrual source for the 519 subjects who completed the 1-year assessment.. Comparing self-referred and registry participants in the intervention arm, there were no significant differences in weekly exercise minutes, percent energy from fat, F&V daily servings, or number of behaviors practiced at goal levels (data not shown) at 1-year follow-up. Within the control arm, self-referred participants demonstrated significantly greater increases in exercise, and F&V consumption after 1-year follow-up (p-values <.05) and also experienced significantly more durable effects with regard to F&V consumption after 2-year follow-up when compared to registry participants (+1.25 vs. +0.38 daily servings, respectively) (p-value = .007) Self-referred participants in the control arm also significantly increased the numbers of behaviors practiced at goal levels at 1-year follow-up compared to registry participants (0 goal-achievement = −15.9% vs. −3.6%; 1 goal-achievement = −10.8% vs.−9.1%; 2 goal-achievement = 20.8% vs. 12.1%; and 3 goal-achievement = 5.9% vs. 0.6%, respectively) (p = .01).
Table 2.
Comparison of intervention and attention control study arms by self-referred versus cancer registry solicited participants from baseline to 1-year follow-up and change in behavioral outcomes.
| Change from Baseline to Year 1 | |||
|---|---|---|---|
|
| |||
| Self-Referral | Registry | p-value* | |
|
| |||
| Achieved Exercise Goal: 150+ min/week-% (n) | |||
| Intervention† | +23% (22) | +18% (28) | .11 |
| Attention Control‡ | +25% (25) | +7% (12) | .002 |
|
| |||
| Exercise (min/week)-mean (se) | |||
| Intervention | +64 (16) | 57 (11) | .26 |
|
|
|||
| Attention Control | +60 (15) | +26 (9) | .004 |
|
| |||
| Achieved Fat Goal: <30% of Energy from fat-% (n) | |||
| Intervention | +17% (17) | +19% (29) | .76 |
|
|
|||
| Attention Control | +2% (2) | +4% (7) | .71 |
|
| |||
| % Energy Fat - mean (se) | |||
| Intervention | −4% (0.6) | −5% (0.5) | .59 |
|
|
|||
| Attention Control | −2% (0.5) | −2% (0.4) | .30 |
|
| |||
| Achieved F&V§ Goal:5+ servings/day- % (n) | |||
| Intervention | +27% (26) | +17% (26) | .23 |
|
|
|||
| Attention Control | +22% (22) | +6% (9) | .04 |
|
| |||
| Daily Servings of F&V-mean (se) | |||
| Intervention | +1.5 (0.3) | +0.8 (0.2) | .18 |
|
|
|||
| Attention Control | +1.1 (0.2) | +0.4 (0.2) | .02 |
P-values reflect the difference between recruitment sources within each treatment arm.
Intervention arm, self-referred (n=98), registry (n =155).
Attention control arm, self-referred (n=101), registry (n = 165).
F&V=fruit and vegetable.
Discussion
To our knowledge, this is the first trial comparing the characteristics and performance of self-referred versus registry-ascertained cancer survivors in a lifestyle intervention trial. Our findings have implications for the utility of diverse recruitment strategies in expanding the available population for cancer research studies.
Self-referral sources may be particularly useful to bolster both response rate and accrual for home-based behavioral intervention studies and may offer a cost-effective approach to recruitment. By adding self-referral sources to the standard registry-ascertained cases, we reduced the time required for sample accrual and also achieved some measure of cost-savings. However, self-referral sources also introduced bias, since these participants were younger, reported lower quality-of-life and fewer co-morbid conditions. Despite these differences, we were surprised to find no observed differences between accrual groups with regard to income, education, and minority-status. This was a similar finding to Henrikson and colleagues (2007), who reported that participants who self-referred to a genetics registry were comparable in terms of demographic characteristics (except education) to an actively recruited population-based sample, whereas, psychosocial differences existed between the groups (10). FRESH START, however, like many diet and exercise interventions that target cancer survivors, accrued a mostly white (83%) and upper-socio-economic sample (19). Our ability to observe a differential in socioeconomic diversity may have been limited.
Our findings also are similar to those of Scholle and colleagues (2000) who enrolled bipolar disorder registry members via diverse recruitment sources that included health professionals, the Internet, support groups, and general marketing (5). Their data suggest that the cost per participant accrued was substantially lower for registrants accrued via support groups and Internet sources than those ascertained via health professionals and general marketing. Unlike our study, these investigators found that both strategies yielded a more highly educated sample; however, like our study, participants accrued via the Internet were significantly younger than registrants from all other groups. Further, in a study of irritable bowel syndrome subjects, Lee and colleagues (1999) found that the type of recruitment method used (advertisement versus clinic referral) affected patient characteristics, including demographics, physical and psychological symptoms, as well as quality-of-life (9).
Perhaps the most important finding of this secondary analysis was that while self-referred and registry participants performed similarly in the tailored intervention arm, self-referred participants performed significantly better than registry participants in the attention control arm (receiving standardized materials) in terms of exercise and F&V consumption. One could intuit that individuals who actively seek enrollment into a behavioral intervention trial might be more motivated than those who are solicited from a cancer registry. Binks and O’Neil (2002) also found greater levels of motivation for weight loss among individuals who self-referred compared to individuals who were physician-referred to a weight loss program (11). However, these findings differ from FRESH START in that they found no differences in weight loss by accrual source. Indeed, our study may be similar to a meta-analysis by Apodaca and Miller (2003) who found that self-help bibliotherapy was less effective among drinkers who were identified through at risk screening than those who were self-referred (12). While self-referred populations may benefit from standardized health promotion materials that are low in cost, populations that do not actively seek health promotion opportunities, i.e., cases solicited from registries and clinics, may require tailored interventions to achieve behavior change.
In conclusion, researchers must continue to devise efficient, low-cost, high-yield recruitment strategies in order to achieve targeted accrual. At the same time, researchers must work toward broader dissemination of lifestyle interventions to the growing population of cancer survivors. Efforts must be made to recruit representative populations and craft interventions that enable behavior modification. Although it was less costly and more efficient to enroll participants who self-referred to FRESH START, researchers should consider potential differences in characteristics and outcomes at the time of recruitment planning and study implementation.
Acknowledgments
Supported by the National Institutes of Health (CA81191, CA74000, CA63782, and M01-RR-30), the American Institute of Cancer Research and the Susan G. Komen Foundation
Footnotes
Results presented in a poster presentation at the 2006 Cancer Survivorship Conference, Bethesda, MD
References
- 1.Beskow LM, Sandler RS, Weinberger M. Research recruitment through US central cancer registries: balancing privacy and scientific issues. Am J Public Health. 2006;96:1920–6. doi: 10.2105/AJPH.2004.061556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fost NF, Levine RJ. The dysregulation of human subjects research. JAMA. 2007;298(18):2196–8. doi: 10.1001/jama.298.18.2196. [DOI] [PubMed] [Google Scholar]
- 3.Elting LS, Cooksley C, Bekele BN, et al. Generalizability of cancer clinical trial results: prognostic differences between participants and nonparticipants. Cancer. 2006;106:2452–8. doi: 10.1002/cncr.21907. [DOI] [PubMed] [Google Scholar]
- 4.Beskow LM, Millikan RC, Sandler RS, Godley PA, Weiner BJ, Weinberger M. The effect of physician permission versus notification on research recruitment through cancer registries (United States) Cancer Causes Contr. 2006;17:315–23. doi: 10.1007/s10552-005-0521-1. [DOI] [PubMed] [Google Scholar]
- 5.Scholle SH, Peele PB, Kelleher KJ, Frank E, Jansen-McWilliams L, Kupfer D. Effect of different recruitment sources on the composition of a bipolar disorder case registry. Soc Psychiatry Psychiatr Epidemiol. 2000;35:220–7. doi: 10.1007/s001270050231. [DOI] [PubMed] [Google Scholar]
- 6.Newlin K, Melkus GD, Jefferson V, Langerman S, Womack J, Chyun D. Recruitment of black women with type 2 diabetes into a self-management intervention trial. Ethn Dis. 2006;16(14):956–62. [PubMed] [Google Scholar]
- 7.Appel LJ, Vollmer WM, Obarzanek E, et al. Recruitment and baseline characteristics of participants in the dietary approaches to stop hypertension trial. J Am Diet Assoc. 1999;99:S69–S75. doi: 10.1016/s0002-8223(99)00419-8. [DOI] [PubMed] [Google Scholar]
- 8.Ries LA, Harkins D, Krapcho M, et al. SEER cancer statistics review, 1975-2003. National Cancer Institute; Bethesda(MD): 2006. [Google Scholar]
- 9.Lee OY, Fitzgerald LZ, Naliboff B, et al. Impact of advertisement and clinic populations in symptoms and perception of irritable bowel syndrome. Aliment Pharmacol Ther. 1999;13:1631–8. doi: 10.1046/j.1365-2036.1999.00657.x. [DOI] [PubMed] [Google Scholar]
- 10.Henrikson NB, Harris JN, Bowen DJ. Predictors of self-referral into a cancer genetics registry. Cancer Epidemiol Biomarkers Prev. 2007;16:1387–92. doi: 10.1158/1055-9965.EPI-06-0009. [DOI] [PubMed] [Google Scholar]
- 11.Binks M, O’Neil PM. Referral sources to a weight management program. J Gen Intern Med. 2002;17:596–603. doi: 10.1046/j.1525-1497.2002.11028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apodaca TR, Miller WR. A Meta-analysis of the effectiveness of bibliotherapy for alcohol problems. J Clin Psychol. 2003;59:289–304. doi: 10.1002/jclp.10130. [DOI] [PubMed] [Google Scholar]
- 13.Demark-Wahnefried W, Clipp EC, McBride C, et al. Design of FRESH START: a randomized trial of exercise and diet among cancer survivors. Med Sci Sports Exerc. 2003;35:415–24. doi: 10.1249/01.MSS.0000053704.28156.0F. [DOI] [PubMed] [Google Scholar]
- 14.Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: a sequentially-tailored, diet and exercise, mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25:2709–19. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- 15.Blair S, Haskell W, Ho P, et al. Assessment of habitual physical activity by seven-day recall in a community and controlled experiments. Am J Epidemiol. 1985;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 16.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires. Am J Epidemiol. 2001;154:1089–99. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 17.Macri JM, Downs SM, Algoti S, Demark-Wahnefried W, Snyder DC, Lobach D. F A simplified approach to generating tailored questionnaires, health education messages and guideline recommendations. CIN-Comput Inform Nurs. 2005;23:316–21. doi: 10.1097/00024665-200511000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demark-Wahnefried W. Tailoring print material interventions that make a difference: approaches used in the FRESH START trial to improve cancer survivors’ dietary and exercise practices. Nutr Today. 2007;42:131–8. doi: 10.1097/01.NT.0000277790.03666.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stull VB, Snyder DC, Demark-Wahnefried W. Lifestyle interventions in cancer survivors: designing programs that meet the needs of this vulnerable and growing population. J Nutr. 2007:243S–8S. doi: 10.1093/jn/137.1.243S. [DOI] [PubMed] [Google Scholar]