Abstract
Aims
Radiological inappropriateness in medical imaging leads to loss of resources and accumulation of avoidable population cancer risk. Aim of the study was to audit the appropriateness rate of different cardiac radiological examinations.
Methods and Principal Findings
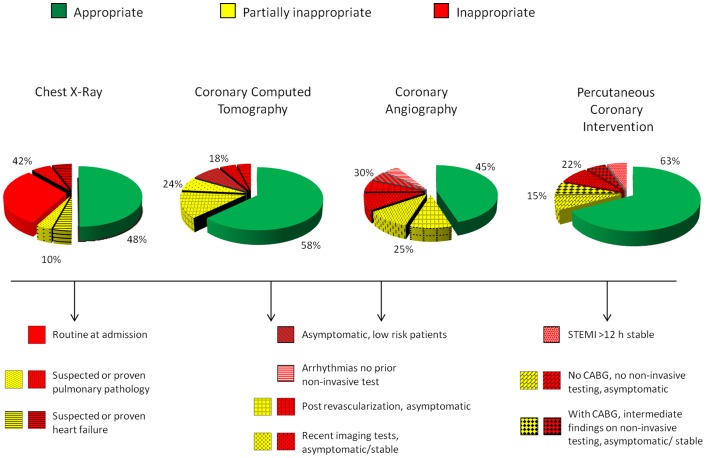
With a retrospective, observational study we reviewed clinical records of 818 consecutive patients (67±12 years, 75% males) admitted from January 1-May 31, 2010 to the National Research Council – Tuscany Region Gabriele Monasterio Foundation cardiology division. A total of 940 procedures were audited: 250 chest x-rays (CXR); 240 coronary computed tomographies (CCT); 250 coronary angiographies (CA); 200 percutaneous coronary interventions (PCI). For each test, indications were rated on the basis of guidelines class of recommendation and level of evidence: definitely appropriate (A, including class I, appropriate, and class IIa, probably appropriate), uncertain (U, class IIb, probably inappropriate), or inappropriate (I, class III, definitely inappropriate). Appropriateness was suboptimal for all tests: CXR (A = 48%, U = 10%, I = 42%); CCT (A = 58%, U = 24%, I = 18%); CA (A = 45%, U = 25%, I = 30%); PCI (A = 63%, U = 15%, I = 22%). Top reasons for inappropriateness were: routine on hospital admission (70% of inappropriate CXR); first line application in asymptomatic low-risk patients (42% of CCT) or in patients with unchanged clinical status post-revascularization (20% of CA); PCI in patients either asymptomatic or with miscellaneous symptoms and without inducible ischemia on non-invasive testing (36% of inappropriate PCI).
Conclusion and Significance
Public healthcare system – with universal access paid for with public money – is haemorrhaging significant resources and accumulating avoidable long-term cancer risk with inappropriate cardiovascular imaging prevention.
Introduction
How the USA (and Europe) will pay for healthcare is a subject on the mind of virtually every American (and European) today. Are there areas where expenses can be cut without undermining the quality of care provided? One of these areas is certainly the inappropriate misuse and overuse of medical imaging [1]. The proliferation of cardiac imaging may represent added value when appropriate, and added cost when inappropriate [2]. The rate of inappropriateness was around 30% for stress echocardiography in our own lab [3], and similar values were found in laboratories of undisputed reputation in Australia, USA and South America for stress echo [3], [4], MPI [5], cardiac CT [6], CA [7] and even for PCI [8]. Appropriateness in healthcare is a moving target and not easy to define. Appropriateness criteria change rapidly as new evidence appears [9]; also, the cultural and economic climate has recently changed abruptly, with efforts by scientific societies to promote the culture of appropriateness [10]–[13] and of political governance to monitor inappropriateness in order to slow the fiscal bleeding [14], [15]. Inappropriateness in medical imaging is not only exorbitantly costly [2], but is also an avoidable risk for the patient when performed with ionizing radiation (in radiology and nuclear medicine), in spite of recent efforts by scientific societies [12], [13] and government [14], [15] to promote radiological responsibility and imaging appropriateness. Still, many medical acts (imaging, therapies, interventions) contribute to wasted money and decreased levels of safety in contemporary medicine [16], [17].
The aim of this study was to audit the level of appropriateness of four index cardiac radiology procedures, in a high-volume, tertiary care cardiovascular referral center in Tuscany, Italy. The monitored examinations reflected a wide spectrum of complexity, cost and radiation dose: chest x-ray (CXR), coronary computed tomography (CCT), diagnostic invasive coronary angiography (CA), coronary percutaneous interventions (PCI).
Methods
Ethics Statement
Written consent was given by the patients before an imaging procedure. The study was approved by the Pisa Ethical Committee as a part (work package 1) of the SUIT-Heart (Stop Useless Ionizing Testing in Heart Disease) study on October 1, 2010 (Study Protocol n.3005/2010).
Study population
The CNR Institute of Clinical Physiology maintains an electronic database with data on all patients undergoing imaging procedures. With a retrospective, observational study design, we reviewed 940 consecutive medical imaging examinations performed during the period January 1-May 31, 2010 in Pisa, IFC CNR-RT FGM, in 818 patients: 250 CXR's (in 233 patients); 240 CCT's (in 240 patients); 250 CA's (in 245 patients); 200 PCI's (in 200 patients). For each examination, an independent expert clinical cardiologist (Head of the Cardiovascular Division, but not directly involved in the care of the audited patients) reviewed all available clinical records and scored the individual exam as: appropriate (class I definitely appropriate and class IIa, probably appropriate); uncertain (class IIb, probably inappropriate); definitely inappropriate (class III). Reference guidelines were those adopted in our Institute following the recommendations of the European Society of Cardiology [18] and American College of Cardiology/American Heart Association [19], [20]. Pre-test likelihood of coronary artery disease (CAD) by age, gender and symptoms for symptomatic patients and Framingham risk criteria to determine the risk of CAD for asymptomatic patients were calculated according to the European and ACC/AHA Guidelines for Chronic Stable Angina [18], [21]. Grading of angina pectoris by the Canadian Cardiovascular Society Classification System was also obtained [22].
Definition of Appropriateness
(An appropriate test is one that is expected to provide more benefit than risk for a patient with a given indication or set of indications).
For all individual examinations, a senior clinical cardiologist independently reviewed clinical and imaging information relating to the request for testing, including review of the patient chart. The first step involved defining the frequency of inappropriate testing. There are currently no specific guidelines or protocols but just some indications regarding when to order a CXR [23]. These last indications were divided into four categories: screening in asymptomatic patients/routine admission, suspected or proven lung pathology, before major surgery, suspected or proven cardiac pathology. Regarding the initial diagnostic assessment of angina the use of CXR is recommended (Class I) in patients with suspected heart failure and in patients with clinical evidence of significant pulmonary disease (ESC guidelines) [24]. The clinical presentation was used to define whether the clinical setting corresponded to an appropriate indication based on the latest specialty guidelines of the American College of Cardiology (ACC)/American Heart Association (AHA) for appropriate use as follows: A = definitely appropriate, score 7–9, the procedure should be performed (Class I of Recommendations, Class IIa = probably appropriate, it is reasonable to perform the test; benefit > risk), U = uncertain, score 4–6, the procedure may be considered (Class IIb = probably inappropriate, benefit ≥ risk), or I = definitely inappropriate, score 1–3, the procedure should not be performed (Class III = definitely inappropriate, risk > benefit). Indications for CCT were divided into seven categories: symptomatic, asymptomatic, risk assessment without prior test results, risk assessment with prior test results, risk assessment: preoperative evaluation for non-cardiac surgery, post-revascularization (PCI or CABG) according to the latest appropriateness guidelines [25]. Indications for CA were divided into six categories: acute coronary syndrome, without non-invasive stress imaging, with prior non-invasive test results, post-revascularization or myocardial infarction, post-arrhythmias and before major surgery based on the latest (2012) guidelines of the ACCF/AHA for the appropriate use of diagnostic catheterization [26]. Indications for PCI were divided into three categories: acute coronary syndrome, without prior bypass surgery, with prior bypass surgery based on the latest (2012) guidelines of the ACCF/AHA for the appropriate use of coronary revascularization [27]. For each procedure the clinical presentation was allocated within the principal category, and it was graded according to the subcategories/scenarios as being used by the scientific societies and according to patient CAD risk.
The second step involved categorizing the causes of inappropriateness (in classes IIb and III), using groupings according to European Union Medical Imaging guidelines (2001) [28], into one of six possible broad categories:
Repeating tests that have already been done (e.g., at another hospital).
Investigation when results are unlikely to affect patient management (e.g., because the anticipated positive finding is usually irrelevant or because a positive finding is so unlikely).
Investigating too often (e.g., before the disease could have progressed or resolved, or before the results could influence treatment).
Do the wrong test.
Failing to provide appropriate clinical information and questions that the imaging investigation should answer.
Excessive investigation. Some clinicians tend to rely on tests more than others, and some patients have inappropriate expectations of the optimal type of examination.
Statistical Analysis
Continuous data are expressed as mean ± SD, and dichotomous variables as percentages. We compared continuous data with unpaired-sampled Student's t-test and proportions by X2 statistics. We considered statistically significant a p-value <.05.
Results
Patients
The clinical presentation of the 818 patients is reported in Table 1, and broken down into the type of examination performed. Fifty-five percent of patients underwent two radiation imaging examinations, 24% underwent three. Patients undergoing CCT were younger with a lower risk factor profile (Table 1).
Table 1. Patient characteristics.
| CXR | CCT | CA | PCI | |
| Number of patients | 233 | 240 | 245 | 200 |
| Age (yrs) | 67±14 | 63±11 | 67±10 | 67±10 |
| Gender (M/F) | 120/117 | 161/79 | 185/60 | 160/40 |
| Diabetes (%) | 17 | 19 | 18 | 25 |
| Hypertension (%) | 60 | 27 | 50 | 65 |
| Hyperlipidemia (%) | 65 | 34 | 65 | 78 |
| Smoking history (%) | 65 | 16 | 70 | 51 |
| Prior MI (%) | 30 | 12 | 37 | 34 |
| Prior PCI or CABG (%) | 15 | 25 | 29 | 37 |
| Chest pain history (%) | 51 | 27 | 62 | 60 |
| Dyspnea (%) | 24 | 20 | 25 | 20 |
| Rest ECG normal (%) | 48 | 72 | 11 | 12 |
M = male; F = female; MI = myocardial infarction; PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft; CXR = chest x-ray; CCT = coronary computed tomography; CA = diagnostic invasive coronary angiography.
Appropriateness
The top reasons for inappropriateness are listed in Table 2. Screening in asymptomatic patients and/or as routine admission was the top indication for CXR. There were significant differences in the rate of the indications between CCT and CA except for follow-up testing post-revascularization (Table 2). The appropriateness score for each imaging test is shown in Fig. 1. The inappropriateness rate ranged from 18% of CCT to 42% of CXR. If partially appropriate examinations were also included, the inappropriateness rate ranged from 37% of PCI to 55% of CA.
Table 2. Top reasons for inappropriate testing for the four procedures.
| CXR | CCT | CA | PCI | |
| Screening in asymptomatic patients/routine at admission% | 70 | |||
| Suspected or proven pulmonary pathology% | 13 | |||
| Suspected heart failure | 13 | |||
| Detection of CAD, asymptomatic, low risk patients% | 42 | 17 | ||
| Recent imaging tests, asymptomatic/stable symptoms% | 23 | 27 | ||
| Post revascularization, asymptomatic% | 20 | 20 | ||
| Arrhythmias no prior non-invasive test% | 13 | |||
| No CABG, one or two vessel CAD without prox LAD, no non-invasive testing, asymptomatic% | 36 | |||
| With prior CABG, all bypass graft patent, intermediate findings on non-invasive testing, asymptomatic/stable% | 23 | |||
| STEMI >12 h from symptom onset, asymptomatic, stable% | 23 |
CAD = coronary artery disease; CABG = coronary artery bypass graft; LAD = left anterior descending; STEMI = ST Elevation Myocardial Infarction; CXR = chest x-ray; CCT = coronary computed tomography; CA = diagnostic invasive coronary angiography. PCI = percutaneous coronary intervention.
Figure 1. Rate of appropriateness for the four procedures.
Pie graph show the rate of appropriate (green slices), partially appropriate (yellow slices) and inappropriate (red slices) examinations for 4 different tests: chest x-ray, coronary computed tomography, diagnostic invasive coronary angiography and coronary percutaneous interventions. The top reasons for inappropriate and partially inappropriate testing are indicated for the four procedures as reported in Table 2. CCT: coronary computed tomography; CA: coronary angiography; PCI: percutaneous coronary intervention.
The top three reasons for inappropriateness (classes IIb and III) were 1) inconclusive, unlikely to alter management, in 50% of all inappropriate tests, 2) tests performed as first-line test (35%) and 3) tests performed as a part of a regular follow-up program (after an acute event or mechanical revascularization) at regular intervals (from the revascularization or previous stress test) in the absence of any change in clinical status (15% of all inappropriate tests).
Discussion
This study shows a high rate of inappropriateness in medical imaging testing performed in a high-volume tertiary care referral cardiovascular center in Tuscany, Italy.
Comparison with Previous Studies
The problem of waste and inappropriateness in medical testing is neither new nor restricted to cardiovascular imaging. A recent Thomson Reuters White paper on healthcare waste estimates unwarranted use as a source of 250–325 billion US dollars annual waste in the USA [1]. Examples of this unwarranted use of services include brand name drugs prescribed when generic alternatives are available or a surgical (or interventional) procedure with a patient-preferred medical treatment alternative. Imaging testing is a major source of waste due to unwarranted use, for several reasons. For instance, diagnostic imaging tests are performed to protect against malpractice exposure, or a high-cost diagnostic procedure is used for patients at low risk for the condition, or a diagnostic test is applied in spite of no expected impact on the course of the treatment or for lack of communication and imperfect exchange of information among physicians. As a result, more than 95 million high-tech scans are done each year in the USA, and medical imaging, including CT, MRI and PET scans, has ballooned into a $100 billion a year industry in the United States, with Medicare paying for $14 billion of that [1]. As many as 20% to 50% should never have been performed because their results did not help diagnose ailments or treat patients [1], [28].The reported inappropriateness is relatively high for all imaging techniques around the world [3], [4], [5], [6], [7], [8]. Therefore, we cannot consider surprising the results of the appropriateness audit performed in our Institution “out of the blue”. Nevertheless, some data are worth noting. First, in our public health system there is no direct professional economic benefit for the practitioner, although there is institutional economic benefit, since hospitals are reimbursed by the Regional Government on a “pay-per-volume” basis, without weighing for appropriateness rate. Second, the clinical theatre was the largest cardiovascular center in Tuscany, a region credited with one of the most advanced models of healthcare in Italy, which in turn is ranked very high in the WHO ranking for quality and equity of healthcare [29]. The Region of Tuscany is the co-owner of the Hospital, and the Regional health plan listed “appropriateness” as one of the four key words in the strategic plan 2008–2010 [30]. Finally, the appropriateness issue and radiation responsibility was first raised in our Institute as a key problem of the sustainability of the healthcare system [31], [32]. Unfortunately, moral suasion in absence of audit and action is not an effective way to change time-honoured prescription habits. It is also interesting that the inappropriateness rate was homogeneously distributed in our sample across all imaging testing procedures, regardless of the cost, radiation dose, and invasiveness. The radiation dose of a Multidetector-row CT is around 750 chest x-rays. A PCI dose ranges from 350 to 2,500 CXRs [33]. They are prescribed with an inappropriateness rate similar to that of a simple CXR.
Study Limitations
We accepted published guidelines as the only possible gold standard against which to assess appropriateness. The approach to defining appropriateness from guidelines is simple, but it is limited since this process does not allow the evaluation of nuances according to the situation of the patient. In addition, most of the guidelines and society recommendations are based on level of evidence C, that is the consensus of the monitoring committee in the absence of a firm evidence base [34].
The setting of the study is a single tertiary care referral center. All of the ordering physicians and imaging lab physicians were salaried staff physicians who had no direct financial incentive for the performance of additional tests and no financial interest in the imaging equipment. The inappropriateness rate would conceivably be higher if a direct financial incentive were present.
This is a retrospective study and, as such, reflects the real world situation as it is. [35].
Clinical Implications and conclusions
Our data emphasize the need for urgent action to abate the waste and risks inherent in the application of inappropriate testing. The use of noninvasive imaging in appropriately selected patients translates into life and cost savings. On the other hand useless examinations pose an economic burden to society, restrict access to patients in need, carry acute risks without offering commensurate benefit, and do not increase (and possibly reduce) the quality of health care. As recently emphasized by the February, 2010 FDA initiative [14] to reduce unnecessary medical radiation exposure from medical imaging, and by the International Atomic Energy Agency's 2010 [15] 3A's strategy (Awareness, Appropriateness, Audit), every effort should be made by scientific and political authorities to achieve the currently elusive goal of having each patient get the right imaging exam with the right dose at the right time. This will help slow fiscal bleeding due to healthcare waste, prevent avoidable long-term cancer risk due to radiation exposure, and improve the quality of healthcare [35].
Funding Statement
The study was funded by the SUIT-Heart (Stop Useless Ionizing Testing in Heart Disease) grant of the Istituto Tumori of the Tuscany Region (ITT), Italy. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.White Paper (2009) Where can $700 Billion in Waste be Cut Annually from the U.S. Healthcare System? Thomson Reuters, Oct. 2009.
- 2. Bonow RO (2008) Is appropriateness appropriate? J Am Coll Cardiol 51: 1290–1291. [DOI] [PubMed] [Google Scholar]
- 3. Picano E, Pasanisi E, Brown J, Marwick TH (2007) A gatekeeper for the gatekeeper: inappropriate referrals to stress echocardiography. Am Heart J 154: 285–290. [DOI] [PubMed] [Google Scholar]
- 4. Mansour IN, Lang RM, Aburuwaida WM, Bhave NM, Ward RP (2010) Evaluation of the clinical application of the ACCF/ASE appropriateness criteria for stress echocardiography. J Am Soc Echocardiogr 23: 1199–1204. [DOI] [PubMed] [Google Scholar]
- 5. Gibbons RJ, Miller TD, Hodge D, Urban L, Araoz PA, et al. (2008) Application of appropriateness criteria to stress single-photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol 51: 1283–1289. [DOI] [PubMed] [Google Scholar]
- 6. Ayyad AE, Cole J, Syed A, Desai MY, Halliburton S, et al. (2009) Temporal trends in utilization of cardiac computed tomography. J Cardiovasc Comput Tomogr 3: 16–21. [DOI] [PubMed] [Google Scholar]
- 7. Gontijo RV, Proietti FA, Amaral CF, de Rezende NA (2005) Appropriateness use of coronary angiography in patients with suspected ischemic heart disease in Brazil. Int J Cardiol 104: 348–349. [DOI] [PubMed] [Google Scholar]
- 8. Chan PS, Patel MR, Klein LW, Krone RJ, Dehmer GJ, et al. (2011) Appropriateness of Percutaneous Coronary Intervention. JAMA 306: 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Patel MR, Spertus JA, Brindis RG, Hendel RC, Douglas PS, et al. (2005) ACCF proposed method for evaluating the appropriateness of cardiovascular imaging. J Am Coll Cardiol 46: 1606–1613. [DOI] [PubMed] [Google Scholar]
- 10. Gibbons RJ, Eckel RH, Jacobs AK (2006) The utilization of cardiac imaging. Circulation 113: 1715–1716. [DOI] [PubMed] [Google Scholar]
- 11. Redberg RF (2007) The appropriateness imperative. Am Heart J 154: 201–202. [DOI] [PubMed] [Google Scholar]
- 12. Gerber TC, Carr JJ, Arai AE, Dixon RL, Ferrari VA, et al. (2009) Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation 119: 1056–1065. [DOI] [PubMed] [Google Scholar]
- 13. Brindis R, Douglas PS (2010) President's page: The ACC encourages multi-pronged approach to radiation safety. J Am Coll Cardiol 56: 522–524. [DOI] [PubMed] [Google Scholar]
- 14.Food and Drug Administration. Initiative to reduce unnecessary radiation exposure. Available: http://www.fda.gov/RadiationEmittingProducts/RadiationSafety/RadiationDoseReduction/ucm199904.htm. Accessed 2013 Oct 20.
- 15.IAEA (2010) Enhances Patient Radiation Safety in Medical Diagnosis and Treatment. Available: http://www.iaea.org/NewsCenter/News/2010/radsafety.html. Accessed 2013 Oct 20.
- 16.President's Cancer Panel: Environmentally caused cancers are “grossly underestimated” and “needlessly devastate American lives”. Available: http://www.environmentalhealthnews. org/ehs/news/presidents-cancer-panel. Accessed 2013 Oct 20.
- 17. Lauer MS (2009) Elements of danger--the case of medical imaging. N Engl J Med 361: 841–843. [DOI] [PubMed] [Google Scholar]
- 18. Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, et al. (2006) Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology; ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J 27: 1341–1381. [DOI] [PubMed] [Google Scholar]
- 19. Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer JG, et al. (1999) ACC/AHA Guidelines for Coronary Angiography: Executive Summary and Recommendations: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) Developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation 99: 2345–2357. [DOI] [PubMed] [Google Scholar]
- 20. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, et al. (2011) ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions Writing Committee Members. Circulation 124: e574–e651. [DOI] [PubMed] [Google Scholar]
- 21. Fraker TD Jr, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, et al. (2007) Chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol 50: 2264–2274. [DOI] [PubMed] [Google Scholar]
- 22. Campeau L (1976) Grading of angina pectoris [letter]. Circulation 54: 522–523. [PubMed] [Google Scholar]
- 23.The Royal College of Radiologists London. Making the best use of clinical radiology services. Referral Guidelines. Six Edition. 2007. [DOI] [PubMed]
- 24. Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, et al. (2003) ACC/AHA 2002 Guideline Update for the Management of Patients With Chronic Stable Angina A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 41: 159–168. [DOI] [PubMed] [Google Scholar]
- 25. Hendel RC, Patel MR, Kramer CM, Poon M, Carr JC, et al. (2006) ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Appropriateness Criteria for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging*.A Report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 48: 1475–1497. [DOI] [PubMed] [Google Scholar]
- 26. Patel MR, Bailey SR, Bonow RO, Chambers CE, Chan PS, et al. (2012) ACCF/SCAI/AATS/AHA/ASE/ASNC/HFSA/HRS/SCCM/SCCT/SCMR/STS 2012 Appropriate Use Criteria for Diagnostic Catheterization. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons Diagnostic Catheterization Writing Group. J Am Coll Cardiol 59: 1995–2027. [DOI] [PubMed] [Google Scholar]
- 27. Patel MR, Dehme GJ, Hirshfeld JW, Smith PK, Spertus JA (2012) ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 Appropriate Use Criteria for Coronary Revascularization Focused Update. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol 59: 857–881. [DOI] [PubMed] [Google Scholar]
- 28.EU Guidelines for Healthcare Professionals who prescribe Imaging Investigations involving Ionising Radiation. Available: http://ec.europa.eu/energy/nuclear/radioprotection/publication/doc/118_update_en.pdf.Accessed 2013 Oct 20.
- 29.World Health Organization, The World Health Report 1995. Bridging the gap. Geneva, WHO 1995.
- 30.A more appropriateness in medical imaging. Interview with Italian Health Minister. La repubblica, December 31,2012. Available:Larepubblica.it/repubblica/archivio/repubblica/2012/12/31/la-salute.html?ref = search. Accessed Oct 20.
- 31. Picano E (2004) Sustainability of medical imaging. BMJ 328: 578–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Picano E (2004) Informed consent and communication of risk from radiological and nuclear medicine examinations: how to escape from a communication inferno. BMJ 329: 849–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248: 254–263. [DOI] [PubMed] [Google Scholar]
- 34. Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC Jr (2009) Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA 301: 831–841. [DOI] [PubMed] [Google Scholar]
- 35.Picano E, Vano E, Rehani MM, Cuocolo A, Mont L, et al.. (2013)The appropriate and justified use of medical radiation in cardiovascular imaging: a position document of the ESC Associations of Cardiovascular Imaging, Percutaneous Cardiovascular Interventions and Electrophysiology. Eur Heart J; 2013.doi:10.1093. [DOI] [PubMed]