Abstract
Penile amputations are uncommon injuries, therefore, the management and outcome of these patients have been compiled from solitary case studies or short reviews. Accidental trauma during circumcision, injury inflicted by a partner following marital discord, and genital self-mutilation observed in patients with deep psychosis, account for a majority of the presentations. Initially, patients with total penile amputations were managed by resuturing the penile structures without repairing the vessels. A high incidence of skin and glans necrosis, urethral strictures, and a failure of sensory recovery were observed, though the penile shaft sometimes survived. Presently, microsurgical replantation has markedly improved the results, though issues of skin loss and urethral stricture still persist. A series of three patients with penile amputation is presented (complete = 2, partial = 1); the technical considerations and outcomes are discussed.
Keywords: penile replantation, genital, self-mutilation
Penile amputations are uncommon injuries, which result in severe functional and psychological disturbances.
The rarity of incidence of penile amputation is supported by the fact that most published reports are solitary case studies or small reviews. The incidence of penile amputation is unclear and possibly underreported.1 About 100 patients of penile replantations have been reported of which ∼ 30 are microsurgical replantations.2 3 Published series have included both partially and totally amputated penises,4 with both nonmicrovascular, and microvascular repair having shown good results.5 6 7 8 Penile amputation may be a result of self-mutilation1 5 9 10 11 12 13 accidental trauma during circumcision,14 15 entrapment in machinery,16 or trauma inflicted by partner following marital discord.17 Genital self-mutilation is the result of a deep psychological aberration, the understanding of which is not clear.
Prior to 1977 penile replantation involved repair of the urethra and corpora without repair of the neurovascular components. In 1977 Tamai and Cohen separately described microsurgical repair of the penis with good results,18 19 which has now become the mainstay of management in penile amputations.
Management
Patients presenting to the emergency room with the unusual injury of genital mutilation, may have severe bleeding, may be psychotic, or drowsy due to the influence of drugs or alcohol. This could confuse or influence the course of management. Penile replantation differs from other replants as a majority of these patients may have a psychiatric back ground, with self-mutilation being the cause of the amputation. They do not take timely medical help, resulting in severe blood loss and shock. Management should focus on resuscitation, retrieval of the amputated part, and replantation.
Early attention is focused on the patient. The patients may be violent, requiring restraint and intravenous sedation. Resuscitation holds priority.8 20 Adequate fluid replacement and often blood transfusion may be necessary.1 8 9 21 Placing a catheter through the injured stump is difficult. A suprapubic catheter needs to be placed, which helps in monitoring, as well as acting as a urinary diversion. If a proximal stump is available, bleeding may be controlled using a Penrose drain tied around it—acting as a tourniquet. In the absence of a stump, when amputation is flush with the pubis, a pressure dressing such as a spica bandage may be used.
The amputated part itself may not have been retrieved from the scene of the accident. Simultaneously with the resuscitation, the amputated part needs to be retrieved, cleaned, and preserved. The amputated part has been retrieved from the toilet8 23 or even from mud.7 It may be washed either with saline or flowing water, wrapped in saline gauze, and placed in a plastic bag. This bag is then placed in a second bag containing a slush of ice.
Other injuries should be looked for. Multiple attempts at self-amputation may injure the genitalia at different places (Fig. 1A and 1B). After resuscitation, psychiatric assessment may be required; this may be difficult considering prior use of sedatives. Due to the unique nature of the injury presenting to the physician, the question that often arises is whether replantations are warranted in such patients. The literature does support the benefits of such replantation, leading to a successful outcome.7 13 22
Fig. 1.

(A,B) Genital self-mutilation in a psychiatric patient. (C) Following microsurgical replantation. (D) Follow-up 2 1/2 years following replantation. Note the incomplete erection and prominent preputial vein.
Penile replantation is an emergency surgical procedure requiring the expertise of a microsurgeon. After resuscitation, the patient should be transferred to a center where such expertise exists.
Treatment is often delayed, the patient may be psychotic or has other injuries. The question arises as to the time limit of a replantation attempt. No clear details regarding ischemia is available in the literature. Successful replantation has taken place 18 hours following injury.15 Injuries up to 24 hours can be replanted if the part has been carefully preserved. The part's record of warm, cold, and rewarm time will possibly give a clearer insight to the extent of tolerable ischemic insult.7
Technique
General anesthesia is preferred, as the patients may be uncooperative because of psychosis or sedatives. A thorough examination of the part, especially to look for multiple injuries is done. Meticulous cleaning and conservative debridement is performed. A silicone urethral catheter is placed through the amputated penis and then through the stump; this acts as a stent, stabilizing it during the repair. Using the operating microscope the vessels and nerves are inspected, dissected and tagged. The urethra is repaired first, using #5/0 polydioxanone sutures taking care to spatulate the opening. Repair is done in two layers. Identification and dissection of the deep (profunda) arteries is then performed attempting to free a small length. Excessive dissection should be avoided as this may interfere with cavernosal blood flow. Applying clamps to these small vessels with inadequate stumps may not be possible. Anastomosis of these vessels may need to be done without the use of approximator clamps. The tunica albuginea is repaired using #4/0 polydioxanone sutures, followed by repair of the cavernosa. The cavernosa may be repaired using a continuous suture to provide a watertight closure. Establishing corporal flow revascularizes the penile shaft. The superficial and deep dorsal veins, dorsal artery, and dorsal nerves are then repaired using #10/0 nylon under the operating microscope. The fascia and skin are loosely approximated. Excessive skin debridement leads to tension, which should be avoided. Postoperative edema is common and this may aggravate skin tension.24 25 Chou et al advocated multiple skin incisions to reduce edema.26 Loose dressing is applied with the scrotum and penis being well supported. Two illustrative cases are presented to illustrate the technique.
Patient 1
A 23-year-old man, on irregular psychiatric treatment, was brought to the emergency department with self-inflicted amputation of his genitalia 6 hours following the episode.
The patient had been diagnosed as a paranoid schizophrenic, and was on irregular treatment for 3 years. He had discontinued the medication for 4 months prior to the incident, and was being counseled by “faith-healers.” Prior to the event, he complained of voices “commanding” him to do various acts. On the night of the injury, he heard similar voices, after which he amputated his genitals using a kitchen knife. He presented with amputation of his genitalia, which were in three separate parts: penis and both testes (Fig. 1A and B).
Replantation of the amputated penis and one testis was done, banking the other testis subcutaneously in the thigh. The right deep artery of the penis, which was larger, was repaired. The corpora cavernosa was repaired using #4/0 polyglactin and urethra using #4/0 catgut. The dorsal artery, superficial, and deep dorsal veins and dorsal nerve were repaired using #10/0 nylon. A silicone catheter was kept as a urethral stent for 3 weeks, urinary diversion being performed using a suprapubic catheter (Fig. 1C).
The left testis was revascularized anastomosing the testicular artery and vein close to the upper pole of the testes. Epididymal continuity could not be restored for technical reasons. Postoperatively the patient was under continuous observation on antipsychotic drugs. The patient had an uneventful recovery and was discharged after 2 weeks and attached to the psychiatric outpatient unit.
He had been on regular psychiatric supervision until his last follow-up 21/2 years following the replantation. He had a good return of sensation of the glans, and developed erection, but it was not sustainable for long (Fig. 1D).
Patient 2
The patient sustained complete penile amputation when his loose underclothes were entrapped in a grass-cutting machine. He presented 4 hours following injury. After resuscitation, microsurgical replantation with repair of his dorsal and deep arteries of the penis, dorsal veins, and nerves were done. Postoperatively he developed partial skin necrosis, which was managed with dressings (Fig. 2A).
Fig. 2.

(A) Early postoperative view showing partial skin necrosis following replantation of a traumatically amputated penis. (B) After secondary healing. (C) Urethral stricture noted in late postoperative period managed by regular dilatation.
His last follow-up was 6 months after his injury. He had gained sensations to his glans, but no erectile function could be elicited. He developed a mild stricture of his urethra that was treated by dilatations (Fig. 2B and 2C).
Discussion
Patients with penile amputations are rare and only a few microsurgeons have or will experience managing such a patient during their career; therefore, the course of management has to be carefully outlined given the case's rarity.
Prior to the independent reports of Tamai and Cohen in 197718 19 of successful microsurgical replantations of the penis, repair involved suturing of the major structures— corpora cavernosa, urethra, and skin without repair of the nerves and vessels. This was often complicated with partial or total skin and glans necrosis, urethral fistula, stricture formation, incomplete erection, and failure of sensory recovery.10 15 17 20 A series of 18 patients reported by Bhagananda et al17 where nonmicrosurgical repair was done showed a high complication of skin loss. Twelve of these patients developed skin loss, of which eight had complete loss. Partial loss of glans was seen in 6 of the 14 patients.17 A technique described was to completely debride the penile skin and bury it into a scrotal pocket to avoid this complication.23 All patients in this study reported loss of penile sensations, but retained erectile function. The other frequent complication reported following nonmicrosurgical repair was urethral stricture, occurring in four out of seven complete amputations.17
Even though microsurgical repair has markedly reduced the complications witnessed earlier,10 24 27 the scope of no microsurgical repair may be an option for distal penile amputations,6 17 28 29 or where microsurgical expertise is not available.
Skin loss has been problematic even following microsurgical repair. Data analyzed from the compilation of 28 patients reviewed by Landstorm et al showed 15 patients with skin loss of which 2 were complete loss.25 30
The blood supply to the penis is from the internal pudendal arteries, which continue as the common penile artery, dividing into two: one entering the corpora cavernosa as the deep (profunda) artery responsible for erection and supply to the penile shaft, and the second continuing as the dorsal artery of the penis supplying the penile skin. The two systems connect with each other. The venous drainage is from the superficial and deep dorsal veins (Fig. 3). The blood supply to the penis is responsible for its survival as well as perfusing it during erectile function. This dual system of supply may be responsible for the survival of the penile shaft, through the corpora only. Establishing corporeal sinusoidal blood flow has been credited in perfusing the distal segment. This circulation, however, is insufficient to perfuse the skin and glans completely. Anatomically, this explains the need to repair the dorsal arteries to reduce skin complications.
Fig. 3.
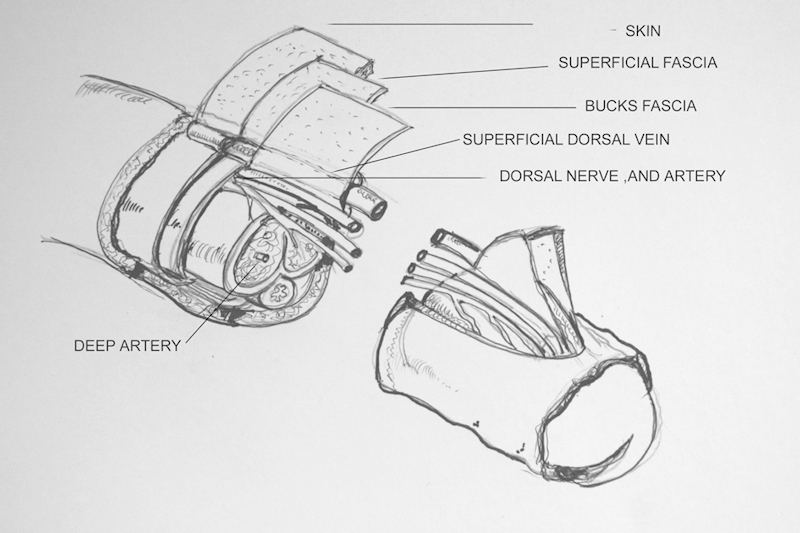
Diagram illustrating the skin, fascial layers, cross section, and vessels of the penis.
Correlating the relationship of the number of arteries or veins repaired with skin loss did not give a clear conclusion. Skin loss was observed in patients in whom both dorsal arteries and deep arteries were repaired.7 20 Anastomosis of the deep arteries only was insufficient to prevent skin complications. A report documented complete skin necrosis after repairing both profunda arteries only.30 Wei et al suggested that at least one dorsal artery needed to be repaired.11 It was proposed that the commonly observed preputial edema may be an aggravating factor in skin necrosis. Ishida et al suggested increasing the venous outflow, repairing both superficial and deep dorsal veins.24 Even after both superficial and deep venous anastomosis, skin necrosis was observed,24 31 32 33 suggesting that this may not be the only reason. Edema of the loose preputial skin, prolonged ischemia, use of heparin postoperatively have all been implicated in contributing to skin necrosis.24 26 32 Debridement of skin and placing it in a skin pocket prophylactically has been suggested by some authors to avoid these complications.7 25 Hyperbaric oxygen was used by Landstorm and Chou after skin problems arose.7 34 Multiple drainage incisions, loose skin suturing, avoiding the use of heparin, elevation of the replanted penis, have all been suggested in preventing this complication.7 24
Both microsurgical and nonmicrosurgical techniques have shown a return of erectile function as a result of repair of the corpora. Of the 28 patients of microsurgical replantation analyzed by Landstorm, 22 patients achieved erection, of which 4 were partial. The need to repair the deep artery to achieve better erectile function is controversial.7 Proximal amputations expose a deep artery of a sizable dimension for approximation. Distally the size of the deep artery narrows, and it may be difficult to approximate it. From the available data, it was observed that in six patients in whom one or both deep arteries had been repaired only three had normal erections. It was hypothesized by Landstrom et al that the poor erectile results could be due to excessive dissection of the deep arteries, compromising further the cavernosal blood flow.7 Compiled data also show that erection was achieved in 15 of the 22 patients in whom the deep (profunda) artery was not repaired. Lidman et al reported good erectile function with repair of only the dorsal arteries.13 He suggested that because communication between the two systems exists, it is not necessary to repair the deep artery. Repair of the deep artery whenever possible is preferred without excessive dissection. It is also interesting to note that 5 of the patients in the group of 28 microsurgical replants where the dorsal nerves were not repaired, erection could be achieved.
Erectile function is difficult to assess as it involves a complex neuro–circulatory reflex, involving various factors, which may be influenced by medication, psychiatric background, and general shyness. Erectile function tests, such as the nocturnal penile test and prostaglandin tests have been documented to demonstrate erectile function in one study, as early as 3 weeks following repair.21
Urethral stricture and fistulas are other complications. Stricture can be avoided by spatulating the urethral margins prior to repair. Total failure of replantation has been reported: one as a consequence of self-manipulation after repair,34 and a second following thrombosis.23
Genital self-mutilations are a unique group of patients that account for 87% of all reported penile amputations. Self-inflicted injuries have been reported in patients under psychiatric care and also in those without previous psychiatric history. Aboserf et al22 reported a series of 14 patients, 65% of whom had psychiatric illness and 35% who had no such illness. Sanger et al10 reported four patients with genital self-mutilation, three being schizophrenic and the fourth having a personality disorder. This group of psychiatric patients with genital self-mutilation was categorized into schizophrenic, transvestites, and patients with religious or cultural conflicts.31
Acute schizophrenia attacks associated with visual delusions are commonly reported in this group.7 35 Injuries in this group of patients involve multiple attempts at self-mutilation complicating the management (Fig. 1A). It has been reported in a study that one in five patients in the series had a previous history of self-mutilation.36 Various accounts of microsurgical replants of the penis have been reported in these patients.11 12 13 31 33 These reports have noted the need for prolonged follow-up not only to assess the results of replantation, but also to identify those patients who are prone to reinflict such injuries again.
Most patients are under treatment by psychiatrists and are reluctant to return for assessment to the reconstructive clinic. Late follow-up of these patients is scanty.13 37 Behavioral changes may be observed in these patients because of the trauma, psychiatric background, testicular amputation, medications, or because of low testosterone levels.37
However, penile replantation is not a contraindication in psychiatric patients. Replantation is superior to any presently available method of reconstruction.
References
- 1.Evins S C, Whittle T, Rous S N. Self-emasculation: review of the literature, report of a case and outline of the objectives of management. J Urol. 1977;118(5):775–776. doi: 10.1016/s0022-5347(17)58190-2. [DOI] [PubMed] [Google Scholar]
- 2.Romilly C S, Isaac M T. Male genital self-mutilation. Br J Hosp Med. 1996;55(7):427–431. [PubMed] [Google Scholar]
- 3.Bhatt Y C, Vyas K A, Srivastava R K, Panse N S. Microneurovascular reimplantation in a case of total penile amputation. Indian J Plast Surg. 2008;41(2):206–210. doi: 10.4103/0970-0358.44945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thatte R L, Wagh M S, Kulkarni N D. Identical unusual subtotal penile amputation in children: a report of four cases. Br J Plast Surg. 1993;46(6):535–537. doi: 10.1016/0007-1226(93)90232-z. [DOI] [PubMed] [Google Scholar]
- 5.Stewart D E, Lowrey M R. Replantations surgery following self-inflicted amputation. Can J Psychiatry. 1980;25(2):143–150. doi: 10.1177/070674378002500208. [DOI] [PubMed] [Google Scholar]
- 6.Ehrich W S. Two unusual penile injuries. J Urol. 1929;21:239–243. [Google Scholar]
- 7.Landström J T, Schuyler R W, Macris G P. Microsurgical penile replantation facilitated by postoperative HBO treatment. Microsurgery. 2004;24(1):49–55. doi: 10.1002/micr.10192. [DOI] [PubMed] [Google Scholar]
- 8.Jezior J R, Brady J D, Schlossberg S M. Management of penile amputation injuries. World J Surg. 2001;25(12):1602–1609. doi: 10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]
- 9.Mora W, Drach G W. Self-emasculation and self-castration: immediate surgical management and ultimate psychological adjustment. J Urol. 1980;124(2):208–209. doi: 10.1016/s0022-5347(17)55375-6. [DOI] [PubMed] [Google Scholar]
- 10.Sanger J R, Matloub H S, Yousif N J, Begun F P. Penile replantation after self-inflicted amputation. Ann Plast Surg. 1992;29(6):579–584. doi: 10.1097/00000637-199212000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Wei F C, McKee N H, Huerta F J, Robinette M A. Microsurgical replantation of a completely amputated penis. Ann Plast Surg. 1983;10(4):317–321. doi: 10.1097/00000637-198304000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Zenn M R, Carson C C III, Patel M P. Replantation of the penis: a patient report. Ann Plast Surg. 2000;44(2):214–220. doi: 10.1097/00000637-200044020-00015. [DOI] [PubMed] [Google Scholar]
- 13.Lidman D, Danielsson P, Abdiu A, Fåhraeus B. The functional result two years after a microsurgical penile replantation. Case report. Scand J Plast Reconstr Surg Hand Surg. 1999;33(3):325–328. doi: 10.1080/02844319950159325. [DOI] [PubMed] [Google Scholar]
- 14.Aydin A, Aslan A, Tuncer S. Penile amputation due to circumcision and replantation. Plast Reconstr Surg. 2002;110(2):707–708. doi: 10.1097/00006534-200208000-00066. [DOI] [PubMed] [Google Scholar]
- 15.Hashem F K, Ahmed S, al-Malaq A A, AbuDaia J M. Successful replantation of penile amputation (post circumcision), complicated by prolonged ischemia. Br J Plast Surg. 1999;52(4):308–310. doi: 10.1054/bjps.1999.3097. [DOI] [PubMed] [Google Scholar]
- 16.Matloub H S, Yousif N J, Sanger J R. Temporary ectopic implantation of an amputated penis. Plast Reconstr Surg. 1994;93(2):408–412. doi: 10.1097/00006534-199402000-00031. [DOI] [PubMed] [Google Scholar]
- 17.Bhanganada K, Chayavatana T, Pongnumkul C. et al. Surgical management of an epidemic of penile amputations in Siam. Am J Surg. 1983;146(3):376–382. doi: 10.1016/0002-9610(83)90420-8. [DOI] [PubMed] [Google Scholar]
- 18.Tamai S, Nakamura Y, Motomiya Y. Microsurgical replantation of a completely amputated penis and scrotum: case report. Plast Reconstr Surg. 1977;60(2):287–291. doi: 10.1097/00006534-197708000-00028. [DOI] [PubMed] [Google Scholar]
- 19.Cohen B E, May J W Jr, Daly J S, Young H H. Successful clinical replantation of an amputated penis by microneurovascular repair. Case report. Plast Reconstr Surg. 1977;59(2):276–280. [PubMed] [Google Scholar]
- 20.Darewicz B, Galek L, Darewicz J, Kudelski J, Malczyk E. Successful microsurgical replantation of an amputated penis. Int Urol Nephrol. 2001;33(2):385–386. doi: 10.1023/a:1015226115774. [DOI] [PubMed] [Google Scholar]
- 21.Carroll P R, Lue T F, Schmidt R A, Trengrove-Jones G, McAninch J W. Penile replantation: current concepts. J Urol. 1985;133(2):281–285. doi: 10.1016/s0022-5347(17)48918-x. [DOI] [PubMed] [Google Scholar]
- 22.Aboseif S, Gomez R, McAninch J W. Genital self-mutilation. J Urol. 1993;150(4):1143–1146. doi: 10.1016/s0022-5347(17)35709-9. [DOI] [PubMed] [Google Scholar]
- 23.Yeniyol C O, Yener H, Keçeci Y, Ayder A R. Microvascular replantation of a self amputated penis. Int Urol Nephrol. 2002;33(1):117–119. doi: 10.1023/a:1014437927083. [DOI] [PubMed] [Google Scholar]
- 24.Ishida O, Ikuta Y, Shirane T, Nakahara M. Penile replantation after self-inflicted complete amputation: case report. J Reconstr Microsurg. 1996;12(1):23–26. doi: 10.1055/s-2007-1006448. [DOI] [PubMed] [Google Scholar]
- 25.Heymann A D, Bell-Thompson J, Rathod D M, Heller L E. Successful reimplantation of the penis using microvascular techniques. J Urol. 1977;118(5):879–880. doi: 10.1016/s0022-5347(17)58233-6. [DOI] [PubMed] [Google Scholar]
- 26.Chou E K, Tai Y T, Wu C I, Lin M S, Chen H H, Chang S C. Penile replantation, complication management, and technique refinement. Microsurgery. 2008;28(3):153–156. doi: 10.1002/micr.20470. [DOI] [PubMed] [Google Scholar]
- 27.Jordan G H, Gilbert D A. Management of amputation injuries of the male genitalia. Urol Clin North Am. 1989;16(2):359–367. [PubMed] [Google Scholar]
- 28.Sherman J, Borer J G, Horowitz M, Glassberg K I. Circumcision: successful glanular reconstruction and survival following traumatic amputation. J Urol. 1996;156(2 Pt 2):842–844. [PubMed] [Google Scholar]
- 29.Gluckman G R, Stoller M L, Jacobs M M, Kagan B A. New born penile glans amputation during circumcision and successful attachment. J Urol. 1995;153:778–779. [PubMed] [Google Scholar]
- 30.Jiménez-Cruz J F, Garcia-Reboll L, Alonso M, Broseta E, Sanz S. Microsurgical penis replantation after self-mutilation. Eur Urol. 1995;27(3):246–248. doi: 10.1159/000475170. [DOI] [PubMed] [Google Scholar]
- 31.Blacker K H, Wong N. Four cases of autocastration. Arch Gen Psychiatry. 1963;8:169–176. doi: 10.1001/archpsyc.1963.01720080059009. [DOI] [PubMed] [Google Scholar]
- 32.Mosahebi A, Butterworth M, Knight R, Berger L, Kaisary A, Butler P E. Delayed penile replantation after prolonged warm ischemia. Microsurgery. 2001;21(2):52–54. doi: 10.1002/micr.1008. [DOI] [PubMed] [Google Scholar]
- 33.Yamano Y, Tanaka H. Replantation of a completely amputated penis by the microsurgical technique: a case report. Microsurgery. 1984;5(1):40–43. doi: 10.1002/micr.1920050109. [DOI] [PubMed] [Google Scholar]
- 34.Pederson W C. Replantation. Plast Reconstr Surg. 2001;107(3):823–841. doi: 10.1097/00006534-200103000-00027. [DOI] [PubMed] [Google Scholar]
- 35.Stunell H, Power R E, Floyd M Jr, Quinlan D M. Genital self-mutilation. Int J Urol. 2006;13(10):1358–1360. doi: 10.1111/j.1442-2042.2006.01548.x. [DOI] [PubMed] [Google Scholar]
- 36.Greilsheimer H, Groves J E. Male genital self-mutilation. Arch Gen Psychiatry. 1979;36(4):441–446. doi: 10.1001/archpsyc.1979.01780040083009. [DOI] [PubMed] [Google Scholar]
- 37.Griffiths M, Britto J, Frame J. 5-year follow-up of replantation of penis and testis in a child. Lancet. 2003;361(9353):263. doi: 10.1016/S0140-6736(03)12302-1. [DOI] [PubMed] [Google Scholar]


