Abstract
Objectives
The role of genetic polymorphisms of tumor necrosis factor-alpha (TNF-α) for lung cancer development was evaluated.
Methods
Genotypes of the TNF-α polymorphisms, -1210C>T, -487A>G, -417A>G, IVS1+123G>A, and IVS3+51A>G, were determined in 616 lung cancer cases and 616 lung cancer-free controls.
Results
After adjusting for body mass index and smoking, each TNF-α genotype or haplotype composed of five TNF-α single nucleotide polymorphisms did not show an association with lung cancer risk (p>0.05). The statistical power was found to be 88.4%, 89.3%, 93.3%, 69.7%, and 93.9% for 1210C>T, -487A>G, -417A>G, IVS1+123G>A, and IVS3+51A>G, respectively. Furthermore, the effects of each SNP or haplotype on lung cancer risk were not found to be different according to the cell type of lung cancer (p>0.05). In the repeated analysis with only subjects without other diseases related to inflammation, there was also no association between polymorphisms or haplotypes of the TNF-α gene and lung cancer risk (p>0.05).
Conclusions
This study found no association between common variants of the TNF-α gene and lung cancer risk.
Keywords: Lung cancer risk, Polymorphism, Tumor necrosis factor-alpha
Introduction
Inflammation is the dynamic response of vascularized tissue to injury, and is an important part of the body's defense mechanisms [1]. However, although inflammation is required for homeostasis, excessive inflammation itself may cause disease [2]. In particular, chronic inflammation is accepted as an important underlying condition for tumor development, and is thought to account for the development of approximately 20% of human cancers [3]. Furthermore, many epidemiologic studies have demonstrated a correlation between genetic polymorphisms of inflammation-related genes and an elevated cancer incidence [4,5]. Tumor necrosis factor-alpha (TNF-α) is an important inducer of the inflammatory response and is regarded as an endogenous tumor promoter [6]. In addition, TNF-α variations at the genetic level have been reported to affect the risk of a variety of diseases including cancer [7,8]. Therefore, changes in TNF-α function, as a result of genetic variation, may affect lung carcinogenesis. However, additional studies also showed no association of TNF-α polymorphisms with inflammatory diseases [9-11]. Several studies reported the relationship between TNF-α polymorphisms and lung cancer risk and their results were found to be controversial, possibly due to the small sample size or no consideration of polymorphisms in other sites of the TNF-α gene [12,13]. Therefore, in the present study, we explored TNF-α genetic polymorphisms in 616 lung cancer patients and 616 lung cancer-free controls. For five selected polymorphisms, the frequency was determined and the association between TNF-α gene polymorphisms and lung cancer susceptibility was examined.
Materials and Methods
Study Population
A total of 616 newly diagnosed lung cancer patients were recruited without age, histologic, or stage restrictions at Chungbuk National University Hospital, Dankook University Hospital, and Inha University Hospital between 2001 and 2003 [14]. The control subjects consisted of 248 non-lung cancer patients admitted to the same hospitals (Table 1) and 368 participants in the health checkup program of each hospital. They were individually matched to the cases by sex and age (±2 years). Detailed information on weight, height, smoking history, family history of cancer, history of diseases including lung cancer, and other socio-economic characteristics, etc., were collected by trained interviewers using a structured questionnaire. The institutional review board (IRB) at the Seoul National University Hospital approved our study protocol (IRB no., C-0602-083-169), and all study participants provided written informed consent. Venous blood samples from all subjects were collected and stored at -70℃ until used for DNA extraction.
Table 1.
Baseline characteristics of lung cancer cases and control subjects
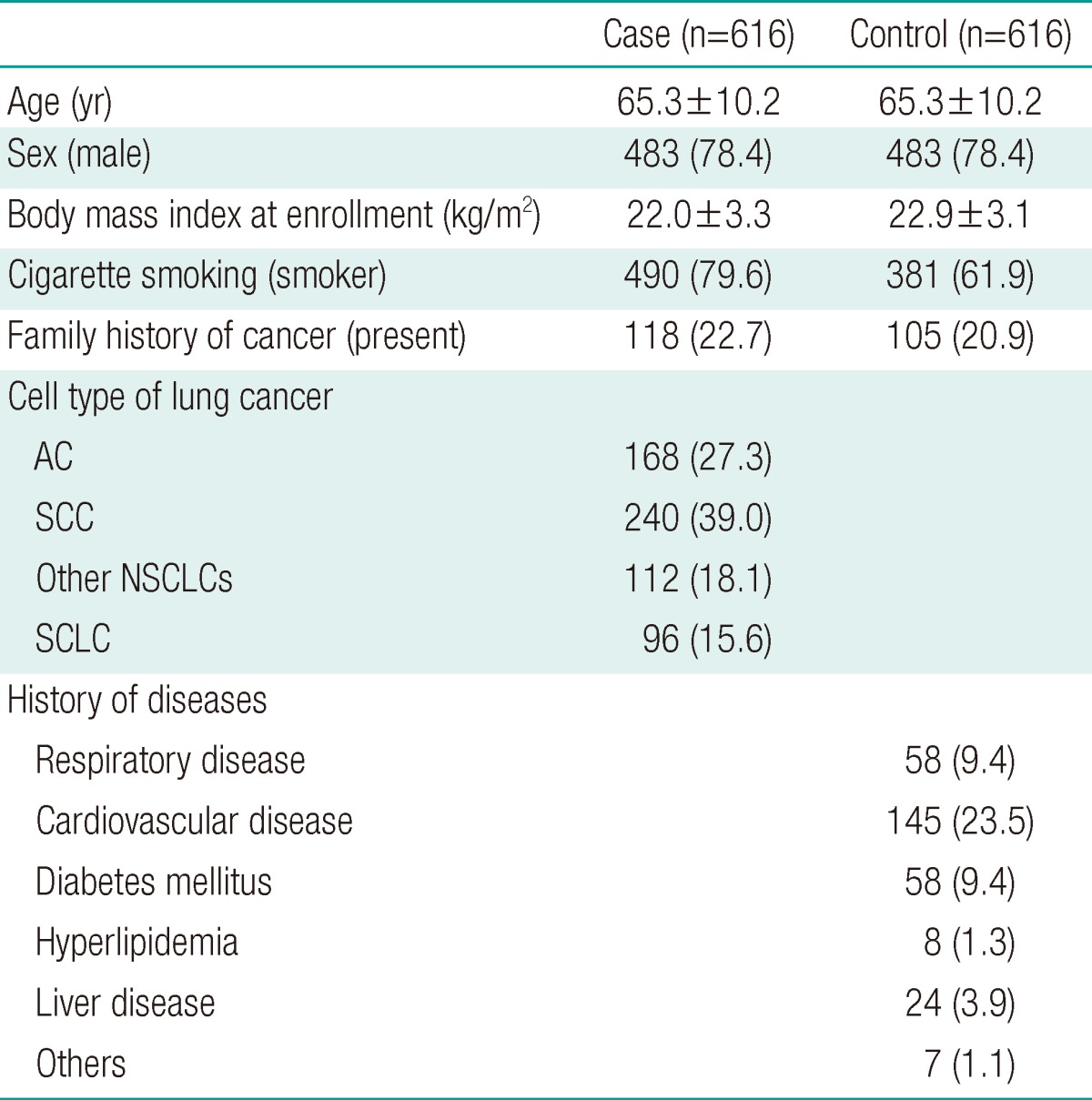
Values are presented as mean±SD or number (%).
SD, standard deviation; AC, adenocarcinoma; SCC, squamous cell carcinoma; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer.
Genotyping
In a study with a limited number of subjects, low minor allele frequency of single nucleotide polymorphisms (SNPs) may lead to a null result even though the SNPs are meaningful for the risk of the target disease. Therefore, we first selected nine TNF-α SNPs (rs1799964, rs1800630, rs1799724, rs1800629, rs361525, rs3093661, rs1800610, rs3093664, and rs3093668) that have more than 5% minor allele frequencies based on the SNP500Cancer database (http://snp500cancer.nci.nih.gov/home.cfm) and then the Dan Stram's haplotype-tagging SNP program (tagSNPsv2.exe) was used to determine the best set of haplotype-tagging SNPs. From this program, five SNPs (-1210C>T, rs1799964; -487A>G, rs1800629; -417A>G, rs361525; IVS1+123G>A, rs1800610; and IVS3+51A>G, rs3093664, r2=0.9432) out of the nine were selected and then successfully genotyped.
DNA was extracted from subjects' blood samples using the QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA). SNP genotyping was performed by SNP-IT™ assays (for rs1799964, rs1800629, and rs3093664) using the SNPstream 25K® System (Orchid Biosciences, Princeton, NJ, USA) and single base primer extension assay (for rs361525 and rs1800610) using the SNaPShot assay kit (Applied Biosystems Inc., Foster City, CA, USA) according to previously reported procedures [14]. The designed primers and probes are listed in Table 2. All genotyping was performed with blinding to the case-control status, and repeated for 5% of the total subjects with a 100% concordance rate.
Table 2.
Primers and probes used for the polymerase chain reaction
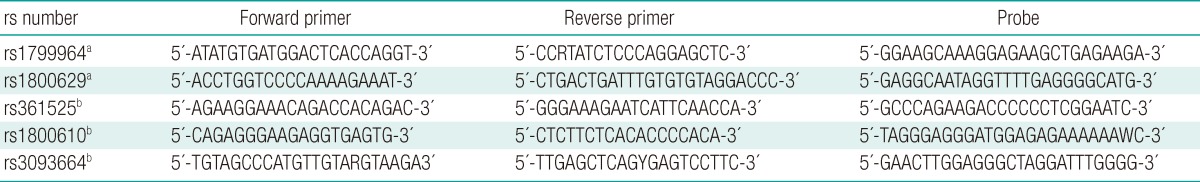
aSNP-IT™; bSNaPshot.
Statistical Analysis
To identify whether each SNP site was on the Hardy-Weinberg equilibrium (HWE), the observed genotype frequency distributions were compared with expected ones using the χ2-test. Data missing for at least one of the five SNPs were excluded and then individual haplotypes were estimated from genotype data using the PHASE version 2.0.2 [15]. Pairwise linkage disequilibrium among the five polymorphic sites was estimated as relative disequilibrium (D') [16]. To estimate the odds ratio (OR) with 95% confidence interval (CI) according to TNF-α gene polymorphisms or haplotypes, unconditional logistic regression was used after adjusted for body mass index (BMI) and smoking. For the statistical power calculation, a web-based power calculation program (SISA, http://home.clara.net/sisa/powhlp.htm) was used. SAS version 8.1 (SAS Inc., Cary, NC, USA), was used for all statistical analysis.
Results
Participants were mostly males (78%) and the mean age was 65.3 years (standard deviation [SD]=10.2 years). The minor allele frequencies of four loci in this Korean population (-1210C, 0.19; -487A, 0.08; -417A, 0.04; and IVS3+51G, 0.04) were shown to be similar to those of the SNP500Cancer database (0.25, 0.08, 0.09, and 0.12, respectively), but the allele frequency of the site IVS1+123G was different between them (Korean, 0.80 and database, 0.10). All genotype distributions were on the HWE (p>0.05), and the relative D' between pairs of the five sites showed that all five of the selected sites were strongly linked (D'≥0.95, p<0.01), although the D' between -1210C>T and IVS1+123G>A showed no linkage (D'=0.11, p<0.01).
Family history of cancer was not significantly different between the cases and controls (OR, 1.11; 95% CI, 0.82 to1.49). However, BMI at enrollment and smoking were found to affect the lung cancer risk (BMI: OR, 1.10; 95% CI, 1.06 to1.14; and smoking: OR, 2.40; 95% CI, 1.86 to 3.09). After adjusted for BMI and smoking, the effects of selected TNF-α genotypes on lung cancer risk were evaluated separately. As shown in Table 3, TNF-α genotypes were not associated with lung cancer risk. When haplotypes were composed of the five TNF-α SNP sites, the effects of each haplotype on lung cancer risk were not found to be significant (p>0.05) (Table 4). Because lung cancer is composed of heterogeneous cell types and baseline characteristics are different according to the cell type, we tried to estimate whether the effects of SNPs or haplotypes on lung cancer risk were different according to cell type of lung cancer (non-small cell lung cancer, n=520; and small cell lung cancer, n=96). However, the effects of each SNP or haplotype on lung cancer risk were not found to be different according to cell type of lung cancer (p>0.05).
Table 3.
The distributions of tumor necrosis factor-alpha genotypes and lung cancer risk
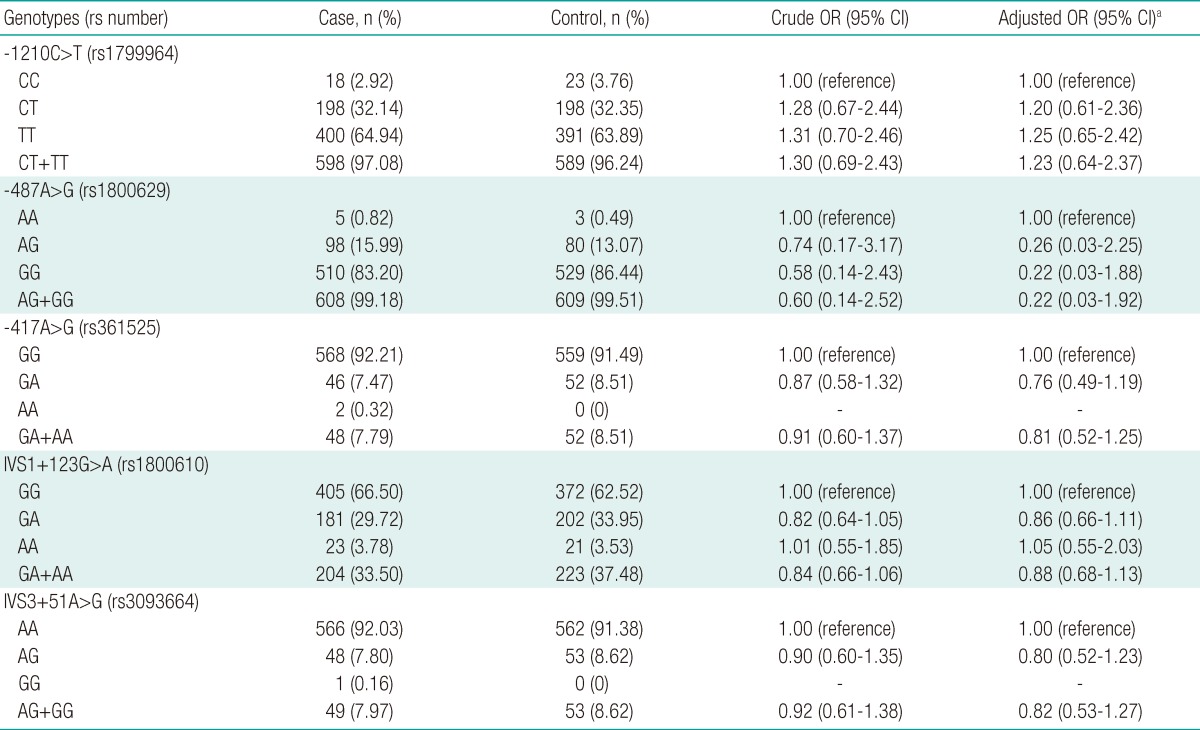
OR, odds ratio; CI, confidence interval.
aAdjusted for body mass index and smoking status.
Table 4.
Tumor necrosis factor-alpha haplotypes and lung cancer risk
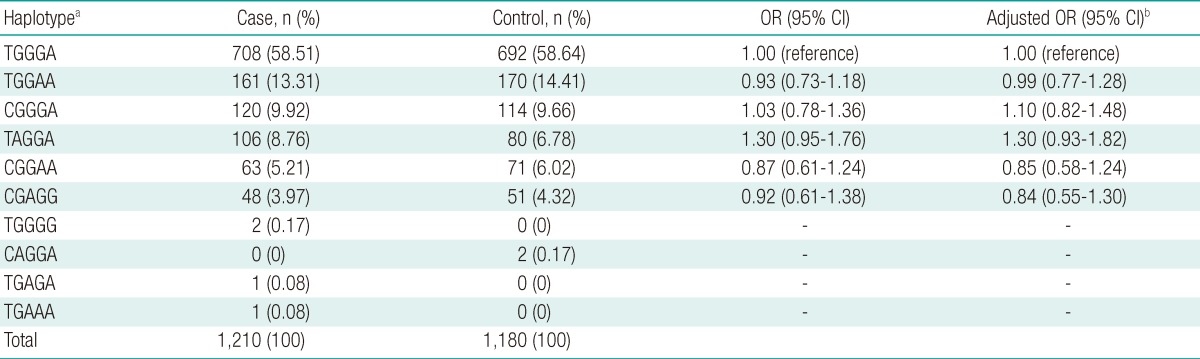
OR, odds ratio; CI, confidence interval.
aComposed of five polymorphic sites: -1210C>T, -487A>G, -417A>G, IVS1+123G>A, and IVS3+51A>G; bOR adjusted for body mass index and smoking status.
In the present study, we repeated the analysis with lung cancer patients and controls without other diseases related to inflammation (lung cancer patients, n=312; and control, n=368), because other diseases related to inflammation may affect the effect of TNF-α gene polymorphisms on lung cancer risk. In the repeated analysis with only subjects without other diseases related to inflammation, we also found no association between polymorphisms or haplotypes of the TNF-α gene and lung cancer risk (p>0.05).
To calculate the statistical power of our study results, we used a web-based power calculation program. Using this program, we obtained the statistical power values 88.4%, 89.3%, 93.3%, 69.7%, and 93.9%, for -1210C>T, -487A>G, -417A>G, IVS1+123G>A, and IVS3+51A>G, respectively.
Discussion
The present study showed no association between TNF-α gene polymorphisms and lung cancer risk. Our result that polymorphisms of the TNF-α gene did not affect lung cancer risk is inconsistent with findings from studies that have examined the relationship between several polymorphisms of the TNF-α gene and cancers [12,17,18]. However, a previous study reported no association of TNF-α polymorphisms with lung cancer risk [13]. Moreover, previous studies that reported a positive association between TNF-α gene polymorphisms and cancer risk had low statistical power because they had a very small sample size of lymphoma, myeloma, or lung cancer (power, 58.1%, 61.0%, 9.4%, and 1.7%, respectively, for the site of -1210C>T in lymphoma, for the site of -487A>G in myeloma, and for the site of -487A>G or -417A>G in lung cancer). In the present study, the corresponding power values were 88.4%, 89.3%, and 93.3%, respectively, for the sites of -1210C>T, -487A>G, and -417A>G, showing the higher reliability of our data to estimate the effect of TNF-α polymorphisms on lung cancer risk. Furthermore, most of the previous studies did not consider the TNF-α SNPs as a haplotype block in spite of strong linkage among them [12,17]. To overcome the limitation of previous studies, we used a haplotype-based approach and also found no association between TNF-α haplotypes and lung cancer risk. In addition, we conducted repeated analysis in subjects without other diseases related to inflammation except lung cancer, because other inflammation-related diseases may affect the effect of TNF-α gene polymorphisms on lung cancer risk. Regardless of the existence or absence of other inflammation-related diseases, we also found no association between polymorphisms or haplotypes of the TNF-α gene and lung cancer risk, indicating that our results are very robust. The strengths of our study include a relatively large sample size of a single ethnic group and higher power values compared with previous studies. Moreover, this report is the first one to try to estimate the relationship between TNF-α haplotypes and lung cancer risk. However, further study is needed to evaluate the effects of TNF-α polymorphisms on lung cancer susceptibility because the present study showed the same direction in the effects of two TNF-α SNPs, -487A>G and -417A>G, on cancer risk as a previous report [12], although our study showed a statistically insignificant association between TNF-α gene polymorphisms and lung cancer risk with higher power compared with a previous study [12]. In conclusion, we report no association between common variants of the TNF-α gene and lung cancer risk.
Acknowledgements
We thank Kang-Hyeon Choe, Kye Young Lee, and Jeong-Seon Ryu for donating DNA of study participants and Kwan-Hee Lee for performing data cleaning of the collected data. This study was supported by the Eco-technopia 21 Project of the Ministry of Environment, Republic of Korea.
Footnotes
This article is available from: http://e-eht.org/
The authors have no conflicts of interest with material presented in this paper.
References
- 1.Kaysen GA. Inflammation: cause of vascular disease and malnutrition in dialysis patients. Semin Nephrol. 2004;24(5):431–436. doi: 10.1016/j.semnephrol.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Busse WW, Lemanske RF., Jr Asthma. N Engl J Med. 2001;344(5):350–362. doi: 10.1056/NEJM200102013440507. [DOI] [PubMed] [Google Scholar]
- 3.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morgan GJ, Adamson PJ, Mensah FK, Spink CF, Law GR, Keen LJ, et al. Haplotypes in the tumour necrosis factor region and myeloma. Br J Haematol. 2005;129(3):358–365. doi: 10.1111/j.1365-2141.2005.05467.x. [DOI] [PubMed] [Google Scholar]
- 5.Xu J, Lowey J, Wiklund F, Sun J, Lindmark F, Hsu FC, et al. The interaction of four genes in the inflammation pathway significantly predicts prostate cancer risk. Cancer Epidemiol Biomarkers Prev. 2005;14(11 Pt 1):2563–2568. doi: 10.1158/1055-9965.EPI-05-0356. [DOI] [PubMed] [Google Scholar]
- 6.Szlosarek PW, Balkwill FR. Tumour necrosis factor alpha: a potential target for the therapy of solid tumours. Lancet Oncol. 2003;4(9):565–573. doi: 10.1016/s1470-2045(03)01196-3. [DOI] [PubMed] [Google Scholar]
- 7.Pérez C, González FE, Pavez V, Araya AV, Aguirre A, Cruzat A, et al. The -308 polymorphism in the promoter region of the tumor necrosis factor-alpha (TNF-alpha) gene and ex vivo lipopolysaccharide-induced TNF-alpha expression in patients with aggressive periodontitis and/or type 1 diabetes mellitus. Eur Cytokine Netw. 2004;15(4):364–370. [PubMed] [Google Scholar]
- 8.Hsieh YY, Chang CC, Tsai FJ, Lin CC, Yeh LS, Tsai CH. Tumor necrosis factor-alpha-308 promoter and p53 codon 72 gene polymorphisms in women with leiomyomas. Fertil Steril. 2004;82(Suppl 3):1177–1181. doi: 10.1016/j.fertnstert.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 9.Seifart C, Dempfle A, Plagens A, Seifart U, Clostermann U, Müller B, et al. TNF-alpha-, TNF-beta-, IL-6-, and IL-10-promoter polymorphisms in patients with chronic obstructive pulmonary disease. Tissue Antigens. 2005;65(1):93–100. doi: 10.1111/j.1399-0039.2005.00343.x. [DOI] [PubMed] [Google Scholar]
- 10.Higham MA, Pride NB, Alikhan A, Morrell NW. Tumour necrosis factor-alpha gene promoter polymorphism in chronic obstructive pulmonary disease. Eur Respir J. 2000;15(2):281–284. doi: 10.1034/j.1399-3003.2000.15b10.x. [DOI] [PubMed] [Google Scholar]
- 11.Ferrarotti I, Zorzetto M, Beccaria M, Gilè LS, Porta R, Ambrosino N, et al. Tumour necrosis factor family genes in a phenotype of COPD associated with emphysema. Eur Respir J. 2003;21(3):444–449. doi: 10.1183/09031936.03.00051303. [DOI] [PubMed] [Google Scholar]
- 12.Shih CM, Lee YL, Chiou HL, Chen W, Chang GC, Chou MC, et al. Association of TNF-alpha polymorphism with susceptibility to and severity of non-small cell lung cancer. Lung Cancer. 2006;52(1):15–20. doi: 10.1016/j.lungcan.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Seifart C, Plagens A, Dempfle A, Clostermann U, Vogelmeier C, von Wichert P, et al. TNF-alpha, TNF-beta, IL-6, and IL-10 polymorphisms in patients with lung cancer. Dis Markers. 2005;21(3):157–165. doi: 10.1155/2005/707131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim JH, Kim H, Lee KY, Choe KH, Ryu JS, Yoon HI, et al. Genetic polymorphisms of ataxia telangiectasia mutated affect lung cancer risk. Hum Mol Genet. 2006;15(7):1181–1186. doi: 10.1093/hmg/ddl033. [DOI] [PubMed] [Google Scholar]
- 15.Stephens M, Smith NJ, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001;68(4):978–989. doi: 10.1086/319501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee KM, Choi JY, Park SK, Chung HW, Ahn B, Yoo KY, et al. Genetic polymorphisms of ataxia telangiectasia mutated and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005;14(4):821–825. doi: 10.1158/1055-9965.EPI-04-0330. [DOI] [PubMed] [Google Scholar]
- 17.Tsukasaki K, Miller CW, Kubota T, Takeuchi S, Fujimoto T, Ikeda S, et al. Tumor necrosis factor alpha polymorphism associated with increased susceptibility to development of adult T-cell leukemia/lymphoma in human T-lymphotropic virus type 1 carriers. Cancer Res. 2001;61(9):3770–3774. [PubMed] [Google Scholar]
- 18.Morgan GJ, Adamson PJ, Mensah FK, Spink CF, Law GR, Keen LJ, et al. Haplotypes in the tumour necrosis factor region and myeloma. Br J Haematol. 2005;129(3):358–365. doi: 10.1111/j.1365-2141.2005.05467.x. [DOI] [PubMed] [Google Scholar]


