Abstract
Injury to anterior teeth is a common event. It requires a treatment approach that assures the complete biologic healing and functional restoration of the tooth or teeth involved. A cystic lesion, which is unable to heal nonsurgically, heals well with surgical intervention and use of mineral trioxide aggregate (MTA) as retrograde filling has been reported in literature. Another material with largely improved handling properties; Biodentine™ (Septodont, St. Maurdes Fossés, France) was introduced in 2011. It is a calcium silicate based material and manufacturers claim that it can be used for crown and root dentin repair treatment, repair of perforations or resorptions, apexification, and root end fillings. This article presents a case report of surgical management of a large cystic lesion using Biodentine™ as retrograde filling material which has not been reported in literature so far. Eighteen months radiographic follow-up exhibited completely healed cystic lesion.
Keywords: Apical surgery, apiceoctomy, Biodentine™, periapical lesion
INTRODUCTION
Traumatic injuries to the anterior teeth are one of the common unanticipated events that cause pain, disfigurement, and psychological problems. Cyst-like apical periodontitis could be the fate of untreated traumatically injured teeth. Treatment options like periapical surgery have been proposed to manage such cases.[1]
Surgical endodontics is a reliable method for the treatment of teeth with periapical lesions that do not respond to conventional root canal treatment. Successful outcomes have been reported in over 80% of cases. This high success rate may be due to modern surgical techniques, magnifying devices, microsurgery instruments, ultrasonic retrotips, and improved root end filling materials.[2]
The cause of apical periodontitis emerges from a pulpal inflammation that exceeds to a necrotic pulp which gives opportunity for bacteria from the oral environment to enter the pulp chamber and the root canal. This colonization inside the tooth results in a leakage of bacterial products, toxins, and/or bacteria's through the apical foramen causing an inflammatory reaction in the periapical tissue.[3,4,5]
The reaction due to the microbial attacks and host response events, results in an apical granulation tissue, that is, periradicular bone resorption and degradation of the apical periodontal ligament. Some of the apical granulomas turn into cysts. The reported incidence of periapical cyst formation varies from 6 to 54%.[6]
Review of literature supports that mineral trioxide aggregate (MTA) due to its higher biocompatibility and sealing ability promotes better healing of the tissues when placed in contact with the dental pulp or periradicular tissues over the available root end filling materials. A novel material Biodentine™ was announced in September of 2010, and made available in January of 2011. Biodentine™ is similar to MTA in basic composition and can serve as its substitute.
This case report demonstrates successful surgical management of a large periapical lesion using Biodentine™ as a retrograde filling material with 18 months evident follow-up.
CASE REPORT
A healthy 24-year-old male patient was reported to the Department of Conservative Dentistry and Endodontics with a chief complaint of broken, discolored tooth and swelling in the previously traumatized maxillary anterior region. The patient gave a history of fall and broken tooth 2 years ago. Medical history was noncontributory and clinical examination revealed a soft, fluctuant, and nontender swelling in the anterior region with fractured and discolored maxillary right central incisor [Figure 1a]. Radiographic examination revealed well-defined radiolucency involving the coronally fractured and discolored maxillary right central incisor and lateral incisor.
Figure 1.
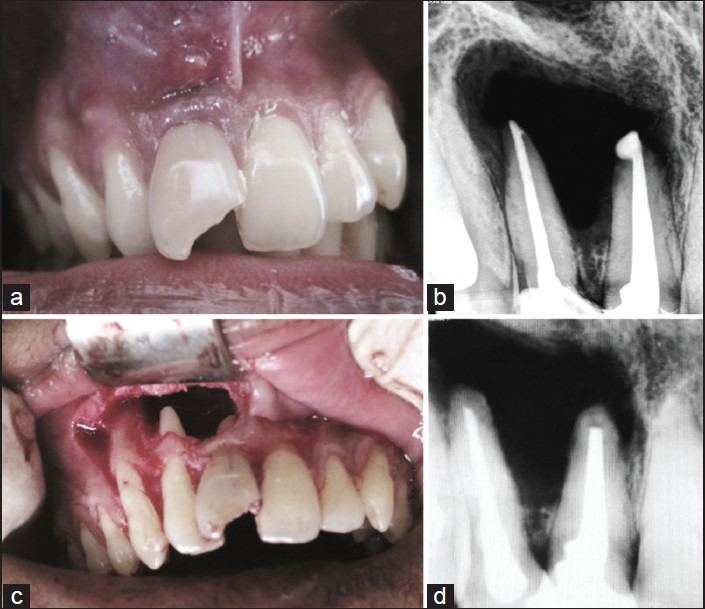
(a) Preoperative photograph showing swelling and fractured central incisor. (b) Post-obturation X-Ray of tooth number 11 and 12. (c) Enucleation of the periapical pathosis. (d) Apical resection and placement of Biodentine™ as retrograde filling X-Ray
Both the teeth presented a negative response to pulp testing and endodontic treatment for both the incisors were scheduled. The endodontic treatment procedures were conducted under magnification (loops × 2.5, Carl Zeiss, Germany). After teeth isolation the access cavities were prepared followed by shaping and cleaning and placement of intracanal medicament of calcium hydroxide (RC Cal, Prime Dental Products, India), which was renewed every 15 days for 3 months. Radiographic examination at 3 months proved no traits of healing and hence a periapical surgery was scheduled.
The teeth were then obturated using cold lateral condensation [Figure 1b]. Raising a double vertical trapezoidal flap, a periapical surgery was performed and periapical pathosis was enucleated [Figure 1c]. Maxillary right central and lateral incisors were apically resected 3 mm from the apex and retrograde cavity was prepared using ultrasonic tip. Biodentine™ was placed as retrograde restorative material of 3 mm thickness. The placement of the retrograde filling material was confirmed using a radiograph [Figure 1d] and the sutures were placed. Biopsy of enucleated lesion was sent for histopathologytests.
The patient was recalled after a week for suture removal. The patient was kept under symptomatic and radiographic observation for the purpose of postoperative evaluation of healing of the periapical intervention in intervals of 1, 3, 6, 12, and 18 months. Biopsy report confirmed the periapical pathology to be a periapical cyst. Periodic radiographic evaluation of the area of intervention showed progressive healing and 18 months follow-up X-ray showed complete bone formation and tooth was asymptomatic [Figures 2a-d]. The patient refused for an orthodontic treatment for correcting his misaligned teeth so the tooth was restored by an esthetic composite class IV restoration [Figure 2e].
Figure 2.
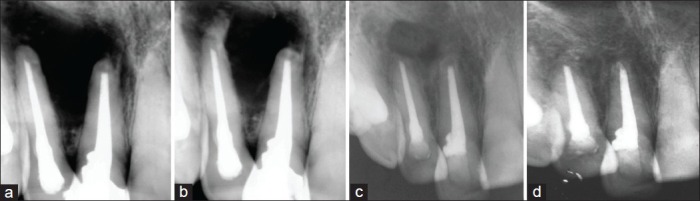
(a-d) Follow up X-rays at the interval of 1, 6, 12, and 18 months showing progressive healing
DISCUSSION
The goal of a periradicular surgery is to gain access to the affected area, evaluate the root circumference and root canal anatomy, and place a biocompatible seal in the form of root end filling that stimulates the regeneration of periapical tissues. The principal modality available to manage failure of conventional orthograde endodontic treatment for a large nonhealing periapical lesion is apical surgery with the success rate being 86-92%.[7] Large cyst-like periapical lesions can drastically change the treatment to more complex procedures with nonsurgical approach being one of the options for managing such cases. However, it requires multiple visits for intracanal medicament placement before permanent filling of the root canal space.[8] This may not be suitable for time constrained patients.
Various cements have been used as root end filling materials. The choice of a root end filling material could be governed by handling properties, biocompatibility, apical seal, and long-term clinical success. MTA has been investigated and used as a root end filling material since its introduction. Despite its good physical and biological properties and it being hydrophilic in nature; its use has always remained a challenge because of its technique sensitivity, prolonged setting time, and high cost. The search for an alternative material was with the aim to reduce cost and increase the feasibility for both professionals and patients.
Biodentine™ is similar to MTA in its basic composition. The powder mainly contains tricalcium silicate, calcium carbonate, and dicalcium silicate; the principal components of MTA. Zirconium oxide serves as the radiopacifier. The liquid consists of calcium chloride in aqueous solution with an admixture of polycarboxylate. The addition of setting accelerators, which is calcium chloride, not only results in fast setting but also improves the handling properties and strength. Calcium silicate cements have setting times in the range of several hours. Decreasing the setting time was achieved by a combination of different effects. First particle size greatly influences the setting time, since the higher the specific surface, the shorter the setting. Also, adding calcium chloride to the liquid component accelerates the system. Finally, the decrease of the liquid content in the system decreases the setting time to harden within 9-12 min.[9]
Kokate and Pawar conducted a study that compared the microleakage of glass ionomer cement, MTA, and Biodentine™ when used as a retrograde filling material and concluded that Biodentine™ exhibited the least microleakage when compared to other materials used.[10]
Research suggests that the high pH and released calcium ions are required for a material to stimulate mineralization in the process of hard tissue healing. Sulthan carried out a study to evaluate the pH and calcium ion release of MTA and Biodentine™ when used as root end fillings. He concluded that Biodentine™ presented alkaline pH and ability to release calcium ions similar to that of MTA.[11] In another study by Han and Okiji that compared the uptake of calcium and silicon released from MTA and Biodentine™ used as endodontic materials into root canal dentine concluded that the elemental uptake into dentine was more prominent for Biodentine™ than for MTA.[12]
Since the introduction of Biodentine™ to be a material of choice as a retrograde filling material, so far there is very less literature other than manufacturers scientific file on its clinical use as a retrograde filling material, so it was proposed in this case to use Biodentine™ as a retrograde filling material and clinically observe for at least a period of 18 months to authentically exhibit the results those can be relied upon.
CONCLUSION
This case report has shown that routine endodontic therapy followed by surgical intervention with a placement of biocompatible retrograde filling material like Biodentine™ for management of endodontic periapical lesions of chronicity would positively affect the treatment outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ahmed HM, Al Rayes MI, Saini D. Management and prognosis of teeth with traumatic induced crown fractures and large periapical cyst like lesions following apical surgery with and without retrograde filling. J Conserv Dent. 2012;15:77–9. doi: 10.4103/0972-0707.92612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maddalone M, Gagliani M. Periapical endodontic surgery: A 3-year follow-up study. Int Endod J. 2003;36:193–8. doi: 10.1046/j.1365-2591.2003.00642.x. [DOI] [PubMed] [Google Scholar]
- 3.Nair PN, Sjogren U, Krey G, Kahnberg KE, Sundqvist G. Intraradicular bacteria and fungi in rootfilled, asymptomatic human teeth with therapy-resistant periapical lesions: A long-term light and electron microscopic follow-up study. J Endod. 1990;16:580–8. doi: 10.1016/S0099-2399(07)80201-9. [DOI] [PubMed] [Google Scholar]
- 4.Tronstad L, Barnett F, Cervone F. Periapical bacterial plaque in teeth refractory to endodontic treatment. Endod Dent Traumatol. 1990;6:73–7. doi: 10.1111/j.1600-9657.1990.tb00394.x. [DOI] [PubMed] [Google Scholar]
- 5.Sen BH, Piskin B, Demirci T. Observation of bacteria and fungi in infected root canals and dentinal tubules by SEM. Endod Dent Traumatol. 1995;11:6–9. doi: 10.1111/j.1600-9657.1995.tb00671.x. [DOI] [PubMed] [Google Scholar]
- 6.Mortensen H, Winther JE, Birn H. Periapical granulomas and cysts. An investigation of 1,600 cases. Scand J Dent Res. 1970;78:241–50. [PubMed] [Google Scholar]
- 7.Girish CS, Ponnappa K, Girish T, Ponappa M. Sealing ability of mineral trioxide aggregate, calcium phosphate and polymethylacrylate bone cements on root ends prepared using Erbium: Yttriumaluminium garnet laser and ultrasonics evaluated by confocal laser scanning microscopy. J Conserv Dent. 2013;16:304–8. doi: 10.4103/0972-0707.114355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandes M, de Ataide I. Nonsurgical management of periapical lesions. J Conserv Dent. 2010;13:240–5. doi: 10.4103/0972-0707.73384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SeptodontBiodentine™ Active BiosilicateTechnology™ scientific file. 2010 [Google Scholar]
- 10.Kokate SR, Pawar AM. An in vitro comparative stereomicroscopic evaluation of marginal seal between MTA, Glass Inomer Cement&Biodentine as root end filling materials using 1% methylene blue as tracer. Endod. 2012;2:36–42. [Google Scholar]
- 11.Sulthan IR, Ramchandran A, Deepalakshmi A, Kumarapan SK. Evaluation of pH and calcium ion release of mineral trioxide aggregateand a new root-end filling material. e-Journal of Dentistry. 2012;2:166–9. [Google Scholar]
- 12.Han L, Okiji T. Uptake of calcium and silicon released from calcium silicate — based endodontic materials into root canal dentine. Int Endod J. 2011;44:1081–7. doi: 10.1111/j.1365-2591.2011.01924.x. [DOI] [PubMed] [Google Scholar]


