Abstract
Reported herein is a case of recurrent major depression with impulse control difficulty in a 33-year-old man with Dandy-Walker variant. He was diagnosed as having major depressive disorder a year before he presented himself to the authors' hospital, and had a history of three-time admission to a psychiatric unit in the previous 12 months. He was readmitted and treated with sodium valporate 1,500 mg/day, mirtazapine 45 mg/day, and quetiapine 800 mg/day during the three months that he was confined in the authors' hospital, and the symptoms were reduced within three months but remained thereafter. This is the only case so far reporting recurrent depression with impulse control difficulty associated with Dandy-Walker variant. This case implies that any cerebellar lesion may cause the appearance of recurrent depression with impulse control difficulty in major depressive disorder.
Keywords: Dandy-Walker variant, Cerebellum, Depression, Impulse control, Aggression
INTRODUCTION
The cerebellum is traditionally involved in the coordination and integration of the motor function. Its contribution to the modulation of higher-order functions is increasingly being recognized.1 Patients with cerebellar diseases such as cerebellar tumor, stroke, and cerebellar atrophy have difficulty controlling their behavior and often show impulsive behavior, have difficulty concentrating, and have compulsive personality disorders.2-4 Classic Dandy-Walker malformation represents cystic dilatation of the fourth ventricle and enlarged posterior fossa, complete or partial agenesis of the cerebellar vermis, elevated tentorium cerebelli, and hydrocephalus. Dandy-Walker variant has been introduced to describe variable hypoplasia of the cerebellar vermis with or without enlargement of the cisterna magna, communication between the fourth ventricle and the arachnoid space, and no hydrocephalus.5
Previous case studies reported that Dandy-Walker malformation was found to be associated with mental retardation, ADHD, schizophrenia, and bipolar disorder.6-11 No previous case study, however, has reported findings of the association of major depression and impulse control difficulty with Dandy-Walker malformation, as shown in this case study. Thus, reported herein is a case of recurrent depression with impulse control difficulty in a 33-year-old man with Dandy-Walker variant.
CASE
A 33-year-old man presented depression, aggressiveness, and impulsivity in his visit to the authors' hospital and was thus compulsorily admitted. He had a two-year depressive episode, was diagnosed as having major depressive disorder a year earlier, and has been on medication irregularly. He had a history of three-time admission to a psychiatric unit in the previous 12 months. His initial admission was a year earlier, after attempting suicide by ingesting pesticide. One day before admission, he presented verbal abuse and aggression. He had no family history of psychiatric disorder, including depression. The patient had two-year, withdrawn university education and he had had various jobs but never managed to keep any of them for more than two months. There was no evidence of substance use and head trauma in the history of the patient.
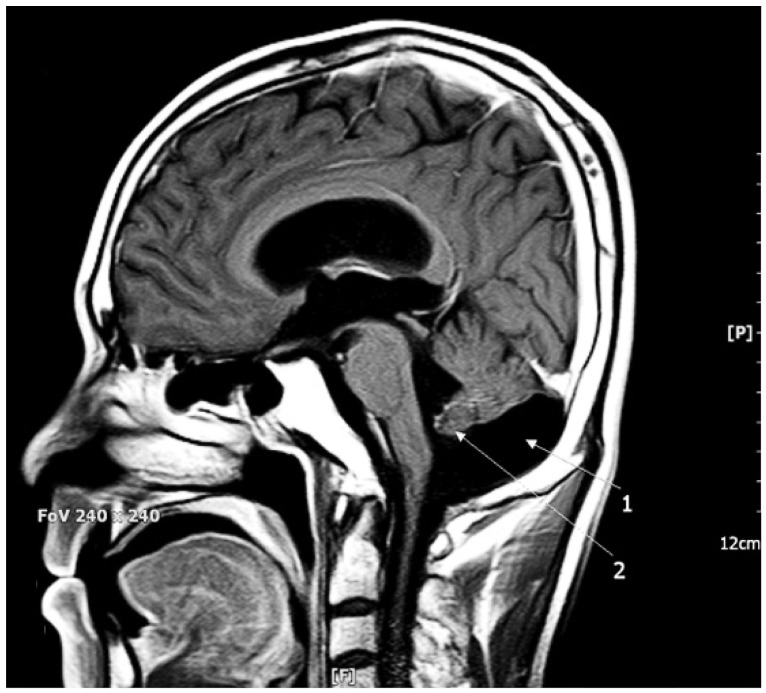
Brain MRI (Figure 1) disclosed an enlarged cisterna magna, hypoplasia of the cerebellar vermis, and dilated ventricles, indicating Dandy-Walker variant. Intelligence testing (K-WISC) confirmed a normal range of intelligence (IQ: 94; latent IQ: 105). The result of the psychological testing showed that the patient had aggressive perceptions of other people, and that he had poor impulse control ability. The patient was anticipated to be sensitive to trivial external stimuli, to easily become angry, and to be aggressive. Beck Depression Inventory (BDI) and Hamilton Depression Scale (HAM-D) tests were performed the day after his admission, and the patient obtained 23/63 and 28/50 scores, respectively.
Figure 1.
MRI coronal scan: Dandy-Walker variant manifesting an enlarged cisterna magna, a slightly hypotrophied cerebella vermis, and slightly dilated ventricles (1, 2).
Mirtazapine treatment was started at a dose of 7.5 mg/day and the dose was increased to 45 mg/day on the fifth day, for the patient's depression. Valproate treatment was started at a dose of 450 mg/day for the patient's aggressiveness and lack of impulse control, and the dose was increased to 1500 mg/day on the 12th day of the patient's confinement. About a week after the initiation of valproate treatment, the patient's aggressiveness and uncontrolled impulsive behavior were slightly alleviated. Quetiapine was added for further treatment of his aggression. Quetiapine was added at a dose of 100 mg/day on the 12th day of confinement, and the dose was increased to 800 mg/day on the 20th day. The BDI score decreased from 23 to 9, and the HAM-D score went down from 28 to 10 after three months of treatment. The patient still presented some uncontrolled impulse and aggression, although these had improved much in the three months.
DISCUSSION
Cerebellar lesions do not always cause ataxic motor syndrome. They also have manifestations as cerebellar cognitive affective syndrome (CCAS), including depression and various symptoms (e.g., aggression, psychotic disorder). The cognitive and psychiatric factors of CCAS have been conceptualized as "cognitive dysmetria concept".12 This holds that a universal cerebellar transform facilitates the autonomic modulation of behavior around the homeostatic baseline, and the behavior being modulated is determined by the specificity of the anatomic subcircuits, or loops, within the cerebrocerebellar system.13
The patient in this case study had major depressive disorder with impulsive behavior as a main problem, but his superficial relationships with other people, difficulty in building appropriate relationships, and frequent change of occupation despite his higher-than-average intelligence seemed to have been associated with his Dandy-Walker-variant-associated cerebellar lesion. The patient had had recurent depression and had shown impulsive behavior for a long time and was recently diagnosed with major depressive disorder. He had poorer effects compared to other patients with depression, which was a characteristic of the patient.
Leroi et al.14 found that more than half of their patients with cerebellar degeneration had psychopathology including depression, personality change, psychotic disorders, and impaired cognition. In another study, the cerebellar vermis was smaller in the patients who experienced multiple episodes of depression.15 This suggested that cerebellar vermal atrophy may be a late neurodegenerative event in those who have had multiple affective episodes. In this case study, the MRI result showed that the patient also had cerebellar vermal hypotrophy, which supports the aforementioned suggestion. This case study also showed the previous understanding of the role of the cerebellum and similar manifestations shown in case studies on Dandy-Walker malformation. In addition, the theoretical explanation that the cerebellum is associated with repeated depression and impulsive behavior has been confirmed via Dandy-Walker variant. The previously explained theories have been further developed via this case study, where superficial relationships with other people, repeated impulsive behavior, persistent exacerbation and repetition of depression, and resistance to treatment were unique features of the patient.
In conclusion, this case study showed that the cerebellum could be associated with depression with impulsive symptom, and expanded the understanding of Dandy-Walker-variant-associated cerebellar lesions.
Acknowledgments
This paper was supported by Konkuk University in 2012.
References
- 1.Schmahmann JD. An emerging concept. The cerebellar contribution to higher function. Arch Neurol. 1991;48:1178–1187. doi: 10.1001/archneur.1991.00530230086029. [DOI] [PubMed] [Google Scholar]
- 2.Parker J, Mitchell A, Kalpakidou A, Walshe M, Jung HY, Nosarti C, et al. Cerebellar growth and behavioural & neuropsychological outcome in preterm adolescents. Brain. 2008;131:1344–1351. doi: 10.1093/brain/awn062. [DOI] [PubMed] [Google Scholar]
- 3.Tiihonen J, Rossi R, Laakso MP, Hodgins S, Testa C, Perez J, et al. Brain anatomy of persistent violent offenders: more rather than less. Psychiatry Res. 2008;163:201–212. doi: 10.1016/j.pscychresns.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Chung SC, Choi MH, Lee SJ, Choi JS, Lee BY, Moon SW, et al. Correlation between psychological factors and the cerebellar volume of normal young adults. Int J Clin Health Psychol. 2010;10:75–88. [Google Scholar]
- 5.ten Donkelaar HJ, Lammens M, Wesseling P, Thijssen HO, Renier WO. Development and developmental disorders of the human cerebellum. J Neurol. 2003;250:1025–1036. doi: 10.1007/s00415-003-0199-9. [DOI] [PubMed] [Google Scholar]
- 6.Langarica M, Peralta V. Psychosis associated to megacisterna magna. An Sist Sanit Navar. 2005;28:119–121. doi: 10.4321/s1137-66272005000100012. [DOI] [PubMed] [Google Scholar]
- 7.Papazisis G, Mastrogianni A, Karastergiou A. Early-onset schizophrenia and obsessive-compulsive disorder in a young man with Dandy-Walker variant. Schizophr Res. 2007;93:403–405. doi: 10.1016/j.schres.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 8.Lingeswaran A, Barathi D, Sharma G. Dandy-Walker variant associated with bipolar affective disorder. J Pediatr Neurosci. 2009;4:131–132. doi: 10.4103/1817-1745.57341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner SJ, Poole R, Nicholson MR, Ghadiali EJ. Schizophrenia-like psychosis and Dandy--Walker variant. Schizophr Res. 2001;48:365–367. doi: 10.1016/s0920-9964(00)00048-7. [DOI] [PubMed] [Google Scholar]
- 10.Gan Z, Diao F, Han Z, Li K, Zheng L, Guan N, et al. Psychosis and Dandy-Walker complex: report of four cases. Gen Hosp Psychiatry. 2012;34:102.e7–102.e11. doi: 10.1016/j.genhosppsych.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Turan T, Besirli A, Asdemir A, Ozsoy S, Esel E. Manic episode associated with mega cisterna magna. Psychiatry Investig. 2010;7:305–307. doi: 10.4306/pi.2010.7.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreasen NC, O'Leary DS, Cizadlo T, Arndt S, Rezai K, Ponto LL, et al. Schizophrenia and cognitive dysmetria: a positron-emission tomography study of dysfunctional prefrontal-thalamic-cerebellar circuitry. Proc Natl Acad Sci U S A. 1996;93:9985–9990. doi: 10.1073/pnas.93.18.9985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16:367–378. doi: 10.1176/jnp.16.3.367. [DOI] [PubMed] [Google Scholar]
- 14.Leroi I, O'Hearn E, Marsh L, Lyketsos CG, Rosenblatt A, Ross CA, et al. Psychopathology in patients with degenerative cerebellar diseases: a comparison to Huntington's disease. Am J Psychiatry. 2002;159:1306–1314. doi: 10.1176/appi.ajp.159.8.1306. [DOI] [PubMed] [Google Scholar]
- 15.DelBello MP, Strakowski SM, Zimmerman ME, Hawkins JM, Sax KW. MRI analysis of the cerebellum in bipolar disorder: a pilot study. Neuropsychopharmacology. 1999;21:63–68. doi: 10.1016/S0893-133X(99)00026-3. [DOI] [PubMed] [Google Scholar]