Abstract
Purpose
Although traumatic osteochondral fractures of the knee represent a common pathology of the knee joint, there is no general agreement concerning specific treatment of this entity. This meta-analysis was initiated in order to evaluate scientific evidence on different treatment options for acute osteochondral fractures of the knee.
Methods
For this purpose an OVID-based systematic literature search was performed including the following databases: MEDLINE, MEDLINE preprints, Embase, CINAHL, Life Science Citations, British National Library of Health and Cochrane Central Register of Controlled Trials. The literature search period was from 1946 to January 2012, which led to the identification of 1,226 articles. After applying study-specific inclusion criteria a total of 19 studies with clinical follow-up of 638 patients were included. The methodology of these studies was systematically analysed by means of the Coleman Methodology Score. Outcome and success rates were evaluated depending on treatment applied.
Results
All studies (n = 19) identified represent case series (evidence-based medicine level IV) and included a total of 638 patients. The average post-operative follow-up was 46 ± 27 months (range 3.75–108). The mean number of study subjects per study was 33 ± 44 patients (range 4–169). The average Coleman Methodology Score was 29 ± 17 points (range 5–72). Six different scoring systems were used for clinical assessment. The overall clinical success rate was 83 % and varied between 45 and 100 %.
Conclusions
This meta-analysis reveals a significant lack of scientific evidence for treatment of osteochondral fractures of the knee. No valid conclusion can be drawn from this study concerning the recommendation of a specific treatment algorithm. Nevertheless, the overall failure rate of 17 % underlines that an acute osteochondral fracture of the knee represents an important pathology which is not a self-limiting injury and needs further investigation.
Keywords: Osteochondral fractures of the knee, Meta-analysis, No valid conclusions, High failure rate
Introduction
Traumatic osteochondral fractures of the knee joint are a common clinical problem in orthopaedic surgery and were first described by Milgram and co-workers in 1943 [1]. The incidence and aetiology of this pathology have been analysed and described in detail. Although both result in an osteochondral defect, the aetiology of fresh traumatic osteochondral fractures differs completely from other osteochondral pathologies of the knee joint such as Ahlbäck’s disease or osteochondritis dissecans (OD). Therefore acute traumatic osteochondral fractures related to trauma represent a different pathology and need to be evaluated and discussed separately.
While the knee joint is the joint most frequently affected by osteochondral fractures, most of these injuries are related to dislocation of the patella or ruptures of the anterior cruciate ligament (ACL). Some authors have described an incidence of osteochondral fractures as almost half of all traumatic patellar dislocations [2, 3], while the incidence of cartilage defects including osteochondral fractures in ACL ruptures is lower, but still remarkably high (16–46 %) [4]. With regard to this, osteochondral fractures seem to be a common pathology of the knee. Mechanisms of osteochondral injuries of the knee joint are similar to those following patellar dislocation and ACL rupture. More specifically, Kennedy et al. [5] described a detailed analysis of possible mechanisms as early as 1966. Those include a direct force to the patella (also described as a possible mechanism for traumatic patella dislocation) and indirect forces such as an external rotation of the tibia or the femur in hyperextension or slight flexion (also accepted as a typical mechanism for ACL rupture). Concerning age, the highest incidence can be found in patients aged around 20 years. Since calcification of the tidemark seems of relevance for stability of the interface between cartilage and subchondral bone, osteochondral fractures are rare in children before calcification of the tidemark has occurred. Nevertheless, osteochondral fractures can occur in every age group.
Concerning treatment options for osteochondral fractures, there are three potential strategies that can be applied. First is fixation of the dislocated fragment, second is removal of the osteochondral fragment and third is to perform any kind of regenerative procedure in order to achieve healing of the injury (such as bone marrow stimulation or any kind of transplantation technique aiming for regeneration of bone and cartilage). Although most authors agree that fixation seems the ideal treatment for acute displaced osteochondral fragments, there are many relevant questions:
Technical aspects of fixation of osteochondral fractures have not been analysed systematically. Many different techniques using conventional screws, bioresorbable implants and sutures have been described.
A critical size has not been determined that makes refixation necessary.
The time between surgery and injury seems of interest concerning healing of the displaced fragment.
Concerning regenerative procedures it remains unclear if adjuvant therapies provide better clinical results instead of resection of the fragment alone.
The existence of prognostic parameters such as age, location within the knee joint and concomitant pathologies could potentially influence treatment decisions.
These relevant questions certainly do not cover all important aspects during treatment of osteochondral fractures of the knee. Nevertheless, in order to better understand those issues, this meta-analysis was performed including all relevant studies, which deal with the issue of treatment of osteochondral fractures at the knee joint.
Methods
For this systematic review, an OVID-based literature search was performed to identify any published clinical studies on the treatment of osteochondral fractures of the knee including the following databases: MEDLINE, MEDLINE preprints, Embase, CINAHL, Life Science Citations, British National Library of Health, and Cochrane Central Register of Controlled Trials (CENTRAL).
The literature search period was from the beginning of 1946 to January 2012. The search was performed on 7 February 2012, using the following strategy: database Ovid MEDLINE® <1946 to January Week 4 2012 > 1 knee/ (9519); 2 exp knee joint/ (37983); 3 exp knee injuries/ (14060); 4 knee.mp. (89714); 5 1 or 2 or 3 or 4 (91120); 6 osteochondral.mp. (2979); 7 5 and 6 (1179). Data from Ovid MEDLINE® In-Process & Other Non-Indexed Citations < February 06, 2012 > were added with the search strategy: 1 knee.mp. (3940); 2 osteochondral.mp. (132); 3 1 and 2 (47). In OvidSP database, ‘exp.’ (explode subject heading) searches main headings and all narrower terms underneath or lower in MeSH (medical subject heading) hierarchy. The function ‘mp.’ searches in the title, abstract and in MeSH headings.
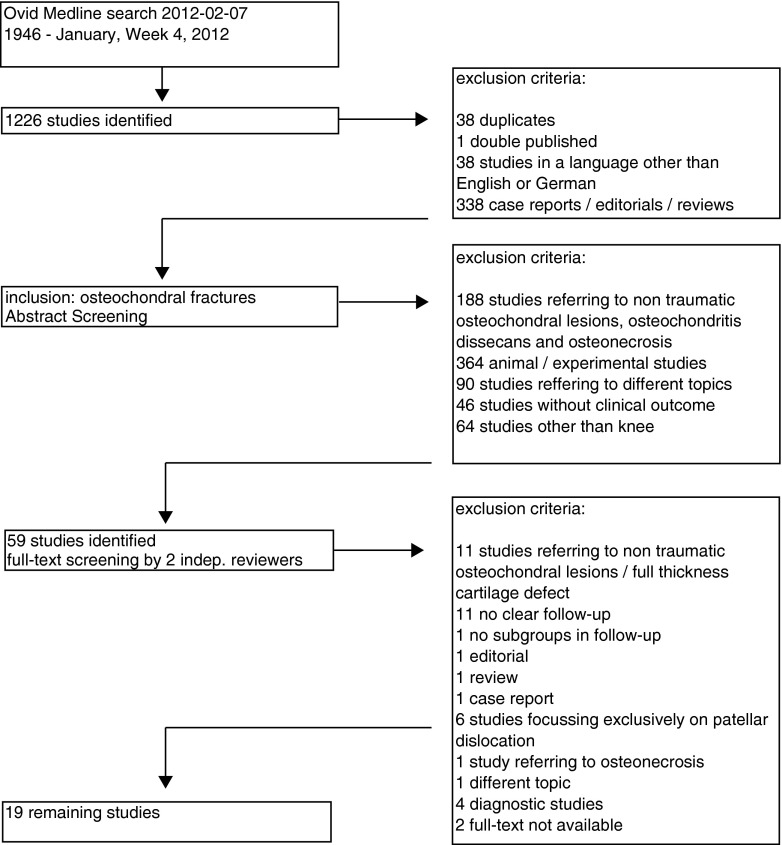
In accordance with the search strategy, a total of 1,226 articles related to osteochondral fractures of the knee were identified: 38 articles were excluded because they were duplicates, one article was double published, 338 articles were excluded since the articles represented review articles, editorials without original data and case reports with a number of patients of three or less and 38 articles were excluded since they had been published in a language other than English or German.
The 811 remaining abstracts were scanned for appropriateness for this meta-analysis. Of these 123 articles were excluded because they focused on treatment of osteochondral lesions that were not traumatic osteochondral fractures. For the same reason, 65 articles concerning OD and osteonecrosis were also excluded; 364 articles described experimental and animal studies and were therefore excluded, 46 articles showed no clinical outcome, 90 studies were related to different topics and 64 studies described chondral treatment in a region other than the knee joint.
Of all remaining 59 articles, full texts were obtained and screened by two independent reviewers. All studies reporting the clinical results for treatment of traumatic osteochondral fractures of the knee were included regardless of population size, methodology, follow-up time and rate and indication (n = 19, see Fig. 1).
Fig. 1.
Chart illustrates the number of identified studies using the search strategy given in the “Methods” section, reason for dropout and number of clinical trials involved
Data on study characteristics and design, level of evidence, demographic parameters, diagnosis, defect characteristics, surgical technique and rehabilitation protocol, associated surgical procedures, clinical follow-up and treatment outcomes were extracted from every article included in this systematic review. Specific focus was placed on extracting data describing clinical efficacy of treatment, including clinical function scores. In cases of additional reporting of radiographs, magnetic resonance imaging (MRI) or diagnostic arthroscopy data, these have been evaluated separately. Level of evidence was categorised according to the definition given by the Oxford Centre for Evidence-based Medicine and published by Hanzlik et al. [6].
To assess the methodological quality of the collected data, the modified Coleman Methodology Scores and subscales were determined for each study [7, 8]. The Coleman Methodology Score assesses the methodology of clinical studies by using subscores assigned ten specific quantitative and qualitative criteria (study size, mean duration of follow-up, number of surgical procedures, type of study, diagnostic certainty, description of surgical procedure, post-operative rehabilitation, outcome measures, outcome assessment and selection process). The studies were graded by assigning a score for each criterion, with a result between 0 and 100. A score of 100 indicates the highest study quality. The modified Coleman Methodology Score has been previously used for analysis of methodological quality of cartilage repair studies [8, 9] (Table 2).
Table 2.
Detailed characteristics of all studies included in this meta-analysis (n = 19)
| First author | Year | Journal | Patients | Cases of OCF | Follow-up (months) | Diagnosis | Localisation | Treatment | Pat./treatment | Implant |
|---|---|---|---|---|---|---|---|---|---|---|
| Rosenberg [22] | 1964 | JBJS Am | 15 | 15 | 30 | Patellar dislocation, OCF | Not exactly stated for every case | Removal of free fragments (if present) | 11/removal of free fragments, rest/plaster cast | None |
| Ahstrom [23] | 1965 | JBJS Am | 18 | 18 | 24.4 | OCF, patellar dislocation | LFC: 8 Pat.: 8 |
Debridement | 18/debridement | None |
| Lindholm [24] | 1977 | Clin Orthop | 20 | 2 | 60 | OCF | n.a. | Refixation with bone peg | 2/refixation | Bone peg |
| Myllynen [25] | 1986 | Ann Chir Gynaecol | 4 | 4 | 3.75 | OCF | LFC: 1 Pat.: 3 |
Refixation with bone peg | 4/refixation | Bone peg |
| ten Thije [26] | 1986 | Neth J Surg | 9 | 7 | 18.5 | OCF, patellar dislocation | LFC: 2 Pat.: 5 |
Refixation with fibrin adhesive | 4/fibrin adhesive, 2/screws, 1/debridement | Fibrin adhesive, screw |
| Kaplonyi [17] | 1988 | Injury | 28 | 12 | 18 | Distortion of the knee, patellar dislocation | LFC: 7 Pat.: 6 |
Refixation with fibrin adhesive | 12/refixation | Fibrin adhesive (Tissucol) |
| Mayer [21] | 1988 | Arch Orthop Trauma Surg | 50 | 16 | 66 | OCF | LFC: 6 Pat.: 10 |
Refixation with corticalis pin, screw, debridement | 9/refixation | 9 allogenic cortical bone pins, 1 screw |
| Meyers [11] | 1989 | JBJS Am | 58 | 3 | 42 | OCF | FC: 3 | Psteochondral allografts from fresh cadavers | 3/transplant | Osteochondral allografts from fresh cadavers |
| Savarese [20] | 1990 | Chir Organi Mov | 37 | 20 | 36 | Patellar dislocation, OCF | n.a. | Debridement, refixation | 8/debridement, 12/refixation | Suture |
| Paar [16] | 1991 | Chirurg | 169 | 118 | 30 | OCF | n.a. | Fibrin adhesive, fibrin adhesive + absorbable implant (pin), K-wire | 94/fibrin adhesive, 14/fibrin adhesive + absorbable implant (pin), 2/K-wire, 10/debridement | Fibrin adhesive, polylactide pin, K-wire |
| Korkala [27] | 1995 | Arch Orthop Trauma Surg | 16 | 5 | 52 | OCF | FC: 10 Pat.: 6 FC + pat.: 1 |
Debridement of loose fragments, osteoperiosteal graft | 5/osteoperiosteal grafts | Allogenic osteoperiosteal graft, fibrin glue |
| Matsusue [28] | 1996 | Clin Orthop | 5 | 2 | 49 | OCF | n.a. | Refixation of fragment with absorbable implant (polylactide), fixation of autogenous osteochondral graft | 1/refixation, 1/fixation of autogenous graft | Polylactide pin |
| Marcacci [29] | 1999 | Orthopedics | 13 | 6 | 61.5 | 6 OCF 2 OD, 5 osteonecrosis |
FC: all | OATS | 6/OATS | OATS (4 press-fit, 9 screws) |
| Fuchs [10] | 2003 | Chirurg | 15 | 11 | 14.3 | 4 distortion of the knee, 6 patellar dislocation | LFC: 2 Pat.: 7 LFC + pat.: 1 |
Refixation with absorbable implant (polylactide) | 11/refixation | Polylactide pin or screw |
| Walsh [12] | 2008 | JBJS Am | 8 | 8 | 108 | OCF, patellar dislocation | LFC: 8 | Refixation with multiple absorbable implants (polylactide) | 8/refixation with absorbable implant | Polylactide pin |
| Wachowski [13] | 2011 | Z Orthop Unfall | 12 | 10 | 78 | OCF | FC: 5 Pat.: 5 |
Refixation with absorbable implant (polylactide) | Refixation with absorbable implant | Polylactide pin or screw |
| Wouters [18] | 2011 | KSSTA | 5 | 3 | 60 | OCF | n.a. | Refixation with meniscal arrows | 3/refixation with meniscal arrows | Meniscal arrow |
| Chotel [30] | 2011 | Orthop Traumatol Surg Res | 14 | 14 | 30 | OCF, patellar dislocation | LFC: 9 Pat.: 5 |
Refixation with absorbable pins, screws and suture | 5/refixation with absorbable implant (pin), 5/refixation with screws, 4/refixation with pull-out suture | Polylactide pin, screw or suture |
| Ollat [19] | 2011 | Orthop Traumatol Surg Res | 142 | 79 | 96 | OCF | LFC: 17 % MFC: 75 % Pat.: 5 % Trochlea: 3 % |
OATS | 79 OATS | OATS |
OCF osteochondral fracture, LFC lateral femoral condyle, OD osteochondritis dissecansMFC medial femoral condyle, OATS osteochondral autograft transfer system
Since various outcome parameters have been used in the studies included in this systematic review, in each individual score, a “good” or “excellent” was identified according the recommendations given by the authors of the individual score. For the purpose of this analysis, the percentage of “good” and “excellent” results was considered “success rate”.
The data were independently checked against the original papers using a standard quality-control procedure. Any differences of opinion between the original reviewer and quality control reviewer were resolved by discussion and reference to the study paper. In these cases a consensus was achieved. The data were analysed using established statistical software (SPSS software Version 17.0). The analysed standard deviations were computed of the reported means per paper. Because according to the author’s opinion studies included were found to be too heterogeneous and study quality was too low, no additional statistical analysis has been performed.
Results
Characteristics of included patients
Of the 1,226 studies that were identified using the search algorithm given in Table 1, a total of 19 studies that reported on clinical outcome following treatment of traumatic osteochondral fractures in the knee joint were included, describing the clinical follow-up of 638 patients. The average post-operative follow-up was 46 ± 27 months (range 3.75–108). The mean number of study subjects per study was 33 ± 44 patients (range 4–169).
Table 1.
Reviewed demographics and all included studies
| Demographics | |
|---|---|
| Number of included studies | 19 |
| Number of patients | 638 |
| Number of patients with osteochondral fracture of the knee | 353 |
| Average follow-up | 46 ± 27 months (range 3.75–108) |
| Average number of patients per study | 34 ± 44 (range 4–169) |
| Overall success rate (percentage of excellent/good) | 83 (range 45–100) |
Treatment characteristics of included studies
In the majority of studies (13 studies), a refixation technique was used for the treatment of osteochondral defects. In three studies fragments were exclusively refixed with bioabsorbable implants, in two studies a bone peg was used and in one study meniscus arrows were used for refixation. In two studies fibrin adhesive was used exclusively and in four studies different techniques or a combination of methods were used (bioabsorbable implants, bone pegs, fibrin adhesive, screw debridement). In two studies the osteochondral fragments were debrided, and in three studies an autogenous osteochondral graft was transplanted. Characteristics of all included studies are given in Tables 1 and 2.
Outcome parameters and overall success rate
For post-operative assessment of clinical function, a total of eight different scores were used. In most studies, however, a rating as excellent, good, fair and poor was stated as the outcome criterion. The scores which were used in one study were the Tegner activity score, the McDermott score and the German Society of Autologous Cartilage and Bone Cell Transplantation (DGKKT) score [10]. In another study, a rating system according to Merle D’Aubigné and Postel was used [11], in a third study the International Knee Documentation Committee (IKDC) score and the Cincinnati score [12] and in a fourth study the Lysholm score, McDermott score, Knee Society Score and the Tegner score were used [13]. The overall clinical success rate was 83 % and varied between 45 and 100 % according to the individual scoring system used for the evaluation of clinical outcome (Table 3).
Table 3.
Outcome analysis of included studies (n = 19)
| First author | Outcome parameters | Success (healing) | Success rate (healing) | Success (function) | Success rate (function) | MRI |
|---|---|---|---|---|---|---|
| Rosenberg [22] | Rating as good and fair | n.a. | n.a. | 12 good, 1 fair, 2 not stated | 80 % | n.a. |
| Ahstrom [23] | Classification as good, fair and poor | n.a. | n.a. | 10 good, 2 good after secondary patellar stabilisation, 2 fair, 1 poor | 67 % | n.a. |
| Lindholm [24] | Excellent, good, fair, poor | n.a. | n.a. | n.a. | n.a. | n.a. |
| Mylynen [25] | Radiographs, clinical signs | 4 healed | 100 % | 4 normal function, 2 mild quadriceps atrophy | 100 % | n.a. |
| ten Thije [26] | Radiograph, ROM | 1 loose body | 86 % | 2 limited flexion, rest full ROM | 78 % | n.a. |
| Kaplonyi [17] | Arthroscopic follow-up (healing, joint surface, degenerations), radiological follow-up (union, non-union, arthrosis), joint function (excellent or good, fair, poor) | Radiological: mostly union, but not specified for knee joint | n.a. | Not specified for knee joint | n.a. | n.a. |
| Mayer [21] | ROM, pain, radiographs | All fragments healed | 100 % | All patients could fully bear weight, no further functional outcome in subgroups assessed | 100 % | n.a. |
| Meyers [11] | Knee rating system according to Merle d’Aubigné and Postel | “Success” | 100 % | 2 excellent, 1 fair | 67 % | n.a. |
| Savarese [20] | “Hall” criteria (excellent, good, fair, poor) | “No major complications related to surgery” | 100 % | 6 excellent, 9 good, 4 fair, 1 poor | 75 % | n.a. |
| Paar [16] | Pain, MRI, arthroscopy | 6 fragmented OCF did not heal, cartilage damage, all other fragments healed | 95 % | 9 patients had pain on weight-bearing and 2nd arthroscopy, all others good to fair results | n.a. | 10: no or minor cartilage damage, 9: severe cartilage damage |
| Korkala [27] | Larson score | 5 healed | 100 % | Larson: 1× E 100, 1× E 95, 1× F 76, 1× G 84, 1× E 95 | 80 % | n.a. |
| Matsusue [28] | ROM, redisplacement, bone marrow | 2 healed | 100 % | No pain, good ROM | 100 % | Not exactly stated |
| Marcacci [29] | Lysholm, IKDC, Cincinnati, Swedish rating system, radiograph, CT | 13 OATS healed | 100 % | 12 excellent and good, 1 fair (Lysholm/IKDC/Swedish) | 92 % | n.a. |
| Fuchs [10] | Tegner score, McDermott score, DGKKT score | 11 OCF knee healed | 100 % | Tegner level 4.6, McDermott 89 points, DGKKT 78.8 points | 45 % | 9: normal thickness of cartilage (8), small cartilage damage (1) |
| Walsh [12] | IKDC score, Cincinnati score, clinical evaluation, radiographs, MRI | 7 healed, 1 partly unstable | 88 % | 5 IKDC grade A, 2 B, 1C; 3 Cincinnati score excellent, 2 good, 3 fair | 88 % | No full thickness cartilage loss, 6 small abnormal cleft-like signal posterior, 2 without cartilage thinning, 4 small area of cartilage thinning, 1 moderate, 1 large |
| Wachowski [13] | Lysholm, Tegner, KSS, McDermott, VAS, MRT: mod. Henderson score | Modified Henderson score (MRT): 11.6 points (knee only) | 100 % | KSS 189.4, Lysholm 88.9, Tegner pre-op 6.1, Tegner FU 4.6, McDermott 94.1, VAS 0.8 | 100 % | Modified Henderson score (MRT): 11.6 points (knee only) |
| Wouters [18] | Arthroscopy, return to previous activities | 3 healed, 1 resection of heads of meniscal arrows | 100 % | 2 return to previous activities after 3 months, 1 after 6 months | 100 % | n.a. |
| Chotel [30] | IKDC score, radiographs, MRI (5 patients), clinical examination (ROM) | 14 healed (5 verified by MRT scan) | 100 % | A: 8, B: 5, C: 1, mean 88 ± points; flexion mean 140°, deficit mean 5° | 93 % | 5 patients; fragment healed |
| Ollat [19] | ICRS clinical, IKDC function and Hughston scores, CT scan, arthroscopy or MRI/MOCART (80 cases) | Mean score of 7 (4–10) on an 11-point modified MOCART scale | n.a. | 71.2 % IKDC | 71 % |
ROM range of motion, OCF osteochondral fracture, IKDC International Knee Documentation Committee, CT computed tomography, OATS osteochondral autograft transfer system, DGKKT German Society of Autologous Cartilage and Bone Cell Transplantation, KSS Knee Society Score, VAS visual analogue scale, MRT magnetic resonance tomography, FU follow-up, ICRS International Cartilage Repair Society, MOCART magnetic resonance observation of cartilage repair tissue
Available evidence
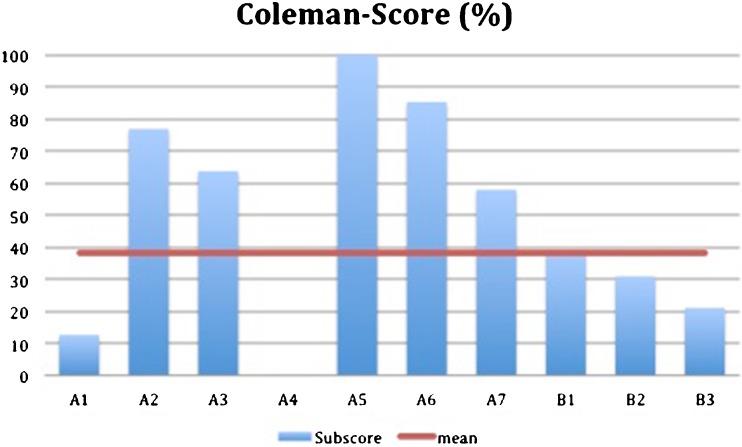
No controlled studies could be identified that reported on clinical outcome following traumatic osteochondral fractures of the knee joint. All studies that were identified were classified as case series. The majority of the studies included reported on retrospective studies. According to the recommendations given by Hanzlik et al. [6], all studies were therefore classified as evidence level IV. The average Coleman Methodology Score was 29 ± 17 points (range 5–72). Subscores are given in Fig. 2.
Fig. 2.
Subscores of the study quality assessed by means of the Coleman Methodology Score
Discussion
This study was set up in order to analyse the scientific evidence available on the treatment of acute osteochondral fractures of the knee joint related to trauma. In order to identify relevant studies, a systematic literature search of the most important scientific libraries was performed. Although osteochondral fracture is a very common problem in orthopaedic surgery, interestingly there is a significant lack not only of high-quality studies, but also of any kind of controlled studies and systematic case series for this pathology.
The initial literature search led to a high number of potentially relevant studies concerning treatment of osteochondral fractures. Nevertheless, the vast majority of the studies were considered not appropriate after scanning either abstract or full text. By application of the major inclusion criteria (traumatic osteochondral lesion, knee joint, report of clinical outcome, more than three cases reported), a total of only 19 studies were identified that met the criteria for evaluation in this meta-analysis. This overall amount of available literature on clinical outcome of traumatic osteochondral fractures of the knee is in contrast to the relevance of this issue in daily practice.
With regard to the available evidence grades, all studies identified were categorised as evidence-based medicine (EBM) level IV, most representing retrospective case series. Furthermore, the methodology of the studies was assessed by means of the Coleman Methodology Score. This score has recently been widely used especially in the field of knee surgery and cartilage repair [9, 14] and also allows one to systematically analyse weaknesses of studies with regard to the available subscales.
The average Coleman Methodology Score was 29 ± 17 points (range 5–72), which is low compared to related subjects, such as the treatment of cartilage defects of the knee [8, 15]. The weaknesses of the available studies are crucial and can be easily identified by the subscales of the Coleman Methodology Score. Interestingly, the major weaknesses of the available literature can be identified in the subparts A1 (case number) and A4 (study design), while the major strength—typical for surgical studies—is represented by a high diagnostic certainty and a detailed description of the type of treatment (A5).
Concerning case numbers, the studies included in this analysis report a mean of 32.6 patients, but only a mean of 17.2 patients suffering from traumatic osteochondral fractures. Some of the studies are characterised by mixing up different patient populations and including patients with osteochondral fractures of other joints such as the talus and the elbow. Additionally, chondral fractures without subchondral bone fragments are also included, which also represent a different pathology with regard to the lack of vascularisation of the detached fragment [16, 17]. Some other studies do not focus on a specific kind of treatment but report overall outcome of patients treated with different surgical techniques [16].
Furthermore, the studies available are characterised by heterogeneity concerning clinical follow-up. Only seven studies used standardised scoring systems for evaluation of patients at the time of follow-up allowing at least indirect comparison to the clinical results of other studies. The remaining studies report success rates without referring to established reporting systems. This could be explained by earlier publication dates. Overall, most studies included date back from the 1980s. Those studies, which have been published more recently, mostly focus on new types of fixation and new implants [10, 12, 18], such as meniscus arrows or bioresorbable pins. As far as treating cartilage injuries by debridement alone, only two studies were eligible; these studies did not provide data on clinical outcome. Conservative treatment has not been described, which might underline that most authors consider the evidence of an osteochondral fracture as an indication for surgical treatment.
In detail the largest study available was published by Paar et al. [16]. A total of 180 patients were included, and 118 of these patients were included with the diagnosis of an osteochondral fracture. The mean follow-up was 30 months—considerably low in order to identify complications on a long-term basis such as post-traumatic osteoarthritis. Nevertheless, a great variety of different surgical procedures including debridement alone, K-wire fixation, fibrin glue fixation and fixation using bioresorbable implants were included. A systematic evaluation of benefits, approach-specific complications or the specific indication for the different treatment options is missing, which might be caused by the fact that treatment has changed over time. Additionally, the study lacks a standardised scoring system for post-operative evaluation of function. The authors reported that a low proportion of patients had ongoing pain (n = 9) and a total of six fragments which had been fixed did not heal.
The second largest cohort of patients was reported and analysed by a French multicentre study of the efficiency of mosaicplasty [19]. Of 142 patients included in this study 79 patients suffered from an acute osteochondral fracture of the knee. This study evaluated patients by means of the International Cartilage Repair Society (ICRS) score at a mean follow-up of 96 months which also represents the second longest follow-up period. A mean IKDC score of only 71.2 points underlines the fact that restitutio ad integrum does not seem to have been achieved in the majority of the cases. Since the paper focuses more on the outcome of mosaicplasty as a surgical treatment option, subanalysis of patients with inferior or superior outcome depending on specific characteristics of the osteochondral fracture such as defect size or defect location was not performed.
Those two studies represent the largest cohort of patients reported in the scientific literature describing treatment of osteochondral fractures. Other authors mostly report cohorts between three and 20 patients, treated with a single surgical technique. With regard to this limited evidence available, this only allows one to describe the surgical technique and report preliminary results on outcome and complications. Information on long-term outcome or healing rate cannot be given as it seems impossible to identify a subgroup of patients with good or poor prognosis.
Summarising these studies, Savarese and Lunghi [20] report the outcome of 20 patients with osteochondral fracture following patella dislocation, treated with either debridement or suture refixation. At a mean of 36 months, the success rate in terms of “excellent” and “good” was 75 %. No specific complications were noted. Mayer and Seidlein [21] published the outcome of 16 patients with different refixation techniques including allogenic cortical pins. No treatment failure was observed in this group. A standardised scoring system was not used for clinical assessment. Fuchs et al. [10] reported the outcome of 11 patients treated with refixation using a bioresorbable implant. The McDermott score was on average 89 points at 14 months following refixation and the overall success rate was 45 % concerning clinical outcome, while the healing rate of fixed fragments was 100 %. A longer follow-up of the same group at 78 months was reported by Wachowski et al. [13] including ten patients. The success rate increased to 100 %, and the authors found a Lysholm score of 89 points representing good clinical outcomes. The Tegner score decreased slightly from 6.3 preoperatively to 4.6 at final follow-up. Clinical results following fibrin refixation were published by Kaplonyi and co-workers [17]. Nevertheless, this study was not specific for the knee joint, a score for post-operative evaluation was not used and a knee-specific success rate was not given. Debridement, which still is an option especially in small defects, has not been evaluated in recent studies. The studies dealing with clinical outcome following debridement date back to the 1960s when Rosenberg [22] and Ahstrom [23] each published a study on 15 and 18 patients treated with surgical debridement. They found “good” clinical outcome in the majority of the patients treated. Conclusions on the overall prognosis of an osteochondral fracture are limited. Most authors report satisfying clinical results independent of what kind of therapy was applied. Data on the incidence of post-traumatic osteoarthritis are lacking, the percentage of incomplete integration after refixation remains unclear due to the limited amount of patients available and even functional outcome following either refixation or debridement cannot be compared sufficiently, since no standardised score is used for patients’ evaluation. With regard to the potential superiority or inferiority of any specific technique for fragment refixation, no conclusions at all can be drawn. Several issues that are really important and of high relevance for clinical practice such as integration rate after refixation depending on the time between injury and treatment or on the defect size or location within the knee have not been addressed at all.
In conclusion, many questions remain in the scientific literature with regard to the characteristics of osteochondral fractures of the knee, concerning optimal treatment, outcome of the available treatment options and prognosis of this injury. This is even more remarkable, since osteochondral fractures represent a common entity in orthopaedic practice and occur frequently especially in patients suffering from patellar dislocation or rupture of the ACL. Those questions need to be addressed in larger studies following this meta-analysis. This seems of additional importance since for a relevant proportion of patients poor outcome that seemed to follow failed therapy is reported. With regard to this, multicentre studies with larger case numbers are encouraged in order to clarify some of the remaining scientific questions.
References
- 1.Milgram J. Tangential osteochondral fracture of the patella. J Bone Joint Surg Am. 1943;25:271–280. [Google Scholar]
- 2.Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513–515. doi: 10.1097/01241398-199407000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19:717–721. doi: 10.1016/S0749-8063(03)00401-8. [DOI] [PubMed] [Google Scholar]
- 4.Brophy RH, Zeltser D, Wright RW, et al. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy. 2010;26:112–120. doi: 10.1016/j.arthro.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy JC, Grainger RW, McGraw RW. Osteochondral fractures of the femoral condyles. J Bone Joint Surg Br. 1966;48:436–440. [PubMed] [Google Scholar]
- 6.Hanzlik S, Mahabir RC, Baynosa RC, et al. Levels of evidence in research published in The Journal of Bone and Joint Surgery (American Volume) over the last thirty years. J Bone Joint Surg Am. 2009;91:425–428. doi: 10.2106/JBJS.H.00108. [DOI] [PubMed] [Google Scholar]
- 7.Coleman BD, Khan KM, Maffulli N, et al. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 8.Jakobsen RB, Engebretsen L, Slauterbeck JR. An analysis of the quality of cartilage repair studies. J Bone Joint Surg Am. 2005;87:2232–2239. doi: 10.2106/JBJS.D.02904. [DOI] [PubMed] [Google Scholar]
- 9.Mithoefer K, McAdams T, Williams RJ, et al. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37:2053–2063. doi: 10.1177/0363546508328414. [DOI] [PubMed] [Google Scholar]
- 10.Fuchs M, Vosshenrich R, Dumont C, et al. Refixation of osteochondral fragments using absorbable implants. First results of a retrospective study. Chirurg. 2003;74:554–561. doi: 10.1007/s00104-003-0623-9. [DOI] [PubMed] [Google Scholar]
- 11.Meyers MH, Akeson W, Convery FR. Resurfacing of the knee with fresh osteochondral allograft. J Bone Joint Surg Am. 1989;71:704–713. [PubMed] [Google Scholar]
- 12.Walsh SJ, Boyle MJ, Morganti V. Large osteochondral fractures of the lateral femoral condyle in the adolescent: outcome of bioabsorbable pin fixation. J Bone Joint Surg Am. 2008;90:1473–1478. doi: 10.2106/JBJS.G.00595. [DOI] [PubMed] [Google Scholar]
- 13.Wachowski MM, Floerkemeier T, Balcarek P, et al. Mid-term clinical and MRI results after refixation of osteochondral fractures with resorbable implants. Z Orthop Unfall. 2011;149:61–67. doi: 10.1055/s-0030-1250591. [DOI] [PubMed] [Google Scholar]
- 14.Niemeyer P, Salzmann G, Schmal H, et al. Autologous chondrocyte implantation for the treatment of chondral and osteochondral defects of the talus: a meta-analysis of available evidence. Knee Surg Sports Traumatol Arthrosc. 2012;20:1696–1703. doi: 10.1007/s00167-011-1729-0. [DOI] [PubMed] [Google Scholar]
- 15.Harris JD, Siston RA, Pan X, et al. Autologous chondrocyte implantation: a systematic review. J Bone Joint Surg Am. 2010;92:2220–2233. doi: 10.2106/JBJS.J.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paar O, Boszotta H. Avulsion fractures of the knee and upper ankle joint. Classification and therapy. Chirurg. 1991;62:121–125. [PubMed] [Google Scholar]
- 17.Kaplonyi G, Zimmerman I, Frenyo AD, et al. The use of fibrin adhesive in the repair of chondral and osteochondral injuries. Injury. 1988;19:267–272. doi: 10.1016/0020-1383(88)90043-5. [DOI] [PubMed] [Google Scholar]
- 18.Wouters DB, Burgerhof JGM, de Hosson JTM, et al. Fixation of osteochondral fragments in the human knee using Meniscus Arrows. Knee Surg Sports Traumatol Arthrosc. 2011;19:183–188. doi: 10.1007/s00167-010-1158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ollat D, Lebel B, Thaunat M, et al. Mosaic osteochondral transplantations in the knee joint, midterm results of the SFA multicenter study. Orthop Traumatol Surg Res. 2011;97:S160–S166. doi: 10.1016/j.otsr.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Savarese A, Lunghi E. Traumatic dislocations of the patella: problems related to treatment. Chir Organi Mov. 1990;75:51–57. [PubMed] [Google Scholar]
- 21.Mayer G, Seidlein H. Chondral and osteochondral fractures of the knee joint–treatment and results. Arch Orthop Trauma Surg. 1988;107:154–157. doi: 10.1007/BF00451595. [DOI] [PubMed] [Google Scholar]
- 22.Rosenberg NJ. Osteochondral fractures of the lateral femoral condyle. J Bone Joint Surg Am. 1964;46:1013–1026. [PubMed] [Google Scholar]
- 23.Ahstrom JP., Jr Osteochondral fracture in the knee joint associated with hypermobility and dislocation of the patella. Report of eighteen cases. J Bone Joint Surg Am. 1965;47:1491–1502. [PubMed] [Google Scholar]
- 24.Lindholm S, Pylkkänen P, Osterman K (1977) Fixation of osteochondral fragments in the knee joint. A clinical survey. Clin Orthop 126:256–260 [PubMed]
- 25.Myllynen P, Alberty-Ryöppy A, Harilainen A. Cortical bone pegs in the treatment of osteochondral fracture of the knee. Ann Chir Gynaecol. 1986;75:160–163. [PubMed] [Google Scholar]
- 26.ten Thije JH, Frima AJ. Patellar dislocation and osteochondral fractures. Neth J Surg. 1986;38:150–154. [PubMed] [Google Scholar]
- 27.Korkala OL, Kuokkanen HO. Autoarthroplasty of knee cartilage defects by osteoperiosteal grafts. Arch Orthop Trauma Surg. 1995;114:253–256. doi: 10.1007/BF00452081. [DOI] [PubMed] [Google Scholar]
- 28.Matsusue Y, Nakamura T, Suzuki S, et al (1996) Biodegradable pin fixation of osteochondral fragments of the knee. Clin Orthop 322:166–173 [PubMed]
- 29.Marcacci M, Kon E, Zaffagnini S, et al. Use of autologous grafts for reconstruction of osteochondral defects of the knee. Orthopedics. 1999;22:595–600. doi: 10.3928/0147-7447-19990601-09. [DOI] [PubMed] [Google Scholar]
- 30.Chotel F, Knorr G, Simian E, et al. Knee osteochondral fractures in skeletally immature patients: French multicenter study. Orthop Traumatol Surg Res. 2011;97:S154–S159. doi: 10.1016/j.otsr.2011.09.003. [DOI] [PubMed] [Google Scholar]