Abstract
Purpose
The Reflection® second-generation uncemented acetabular component was designed to address increased rates of failure observed with the early acetabular designs. However, the reported survivorship of this acetabular component has been conflicting. The aim of this study was to describe the ten to 15-year survivorship and polyethylene wear rate for the uncemented Reflection® acetabular component performed as part of a primary total hip replacement.
Methods
One hundred and four consecutive Reflection® uncemented acetabular components in 97 patients were identified from a prospective arthroplasty database with a minimum of ten years of follow-up. No patient was lost to follow-up. Mean cohort age was 59.1 years.
Results
There were 24 revisions of the acetabular component. The all-cause survival rate at ten years was 77.2 % [95 % confidence interval (CI) 73.9–80.5]. Mean linear wear was 0.20 mm [standard deviation (SD) 0.08] per year and the volumetric wear was 106.2 mm3 per year. At final follow-up, more than half the patients had osteolysis identified around the femoral component. The mean Oxford Hip Score was 35.6 (SD 9.8) at a mean follow-up of 11.9 years, with six (11.1 %) excellent, 26 (48.1 %) good, 17 (31.5 %) fair and five (9.3 %) poor outcomes. Despite the fact that more than a third had a fair or poor outcome, only four (7.4 %) were not satisfied with their hip.
Conclusions
Due to the high rate of relatively asymptomatic polyethylene wear and osteolysis associated with this acetabular component, in our department, we now review all surviving patients both clinically and radiographically on an annual basis.
Keywords: Reflection, Total hip arthroplasty, Uncemented, Acetabular, Survival, Outcome, Wear, Failure
Introduction
The acetabular component of total hip replacement (THR) remains the weakest link in primary arthroplasty, with higher revision rates relative to the stem in national joint replacement registries [1–3]. Indications for early revision of the acetabular component include infection, periprosthetic fractures and component malposition, whereas the most frequent indication for THR revision after three years is due to polyethylene wear and osteolysis, which result in aseptic loosening. The first generation of uncemented acetabular cups produced mixed survivorships, with issues relating to fixation failure, accelerated polyethylene wear and osteolysis [4–6]. Subsequent generations of uncemented acetabular cups have been developed to address these complications and have achieved survival rates comparable with that of their cemented counterparts after ten or more years of follow-up [7].
The Reflection® (Smith & Nephew, Memphis, TN, USA) second-generation uncemented acetabular component was designed to address the issue of backside wear using a thicker and more conforming component–liner interface with a polished inner surface in combination with an improved locking mechanism [8]. These design changes are supported by good survivorship results from both single-centre and registry data [9–12]. Civinini et al. [9] followed up 118 uncemented Reflection acetabular components and demonstrated a 96 % all-cause survivorship rate at ten years. This figure was also supported by data from the Norwegian Arthroplasty Register, in which the Reflection component was found to be one of the best surviving metal-backed acetabular components, with an all-cause ten-year survival rate of 93 % [12]. Teo et al. [10] reported the largest series of patients with a 15 year follow-up, finding an overall survival rate of 90 % and a 99 % survival for the acetabular shell.
Despite this reported excellent survival rate, the senior authors of this paper observed significant rates of polyethylene wear with associated osteolysis at the mid- to long-term follow-up of the uncemented Reflection acetabular component implanted within our study centre. Similar observations were made by Crockarell [11], in a review of 38 THR performed with an uncemented Reflection acetabular component, who found an average linear wear rate of 0.15 mm per year, with more than half of the radiographs demonstrating acetabular osteolysis. In a larger group of 158 THR, he found a 12 % revision rate at a mean follow-up of five years.
The primary aim of this study was to describe the ten to 15-year survivorship and polyethylene wear rate for the uncemented Reflection acetabular component performed as part of a primary THR. Our secondary aim was to assess the functional outcome according to the Oxford Hip Score (OHS) and patient satisfaction.
Patients and methods
During a five-year period (1999–2002), 104 consecutive Reflection uncemented acetabular components were used as part of THR in 97 patients at our centre. These patients were retrospectively identified from a prospectively compiled arthroplasty patient database. The study centre serves a population of approximately 780,000 people [13]. The surgery was performed or supervised by one of four consultant surgeons. A posterior or Moore’s approach was used for 88 THR, and the remainder were performed through a lateral or Hardinge approach. A cemented Exeter stem (Stryker Howmedica Osteonics, Allendale, NJ, USA) was used for all except four THR hybrid combinations; these four patients all received an uncemented Synergy stem (Smith & Nephew, Memphis, TN, USA). A 26-mm femoral head was used for all cases in combination with a 26-mm internal diameter liner. A standardised rehabilitation protocol was used for all patients, with active mobilisation on the first postoperative day. Patients were then reviewed at six weeks and then one, five and ten years post index surgery.
Survival
Several end points were defined for revision: all cause, aseptic loosening and intention to treat (revision surgery performed or offered to patient but refused, or patient deemed too frail to undergo revision). Patient mortality data were obtained from hospital records and the Scottish Office (Communities Analytical Services, Scottish Executive Justice and Communities) in order to adjust survival analysis for patients who died during the study period.
Radiographic analysis
Patients had routine radiographs performed as part of their normal clinical follow-up during the study period. The inclination angle of the Reflection component was measured as the angle between a horizontal line drawn through the intertear drop line and a line bisecting the superior and inferior angles of the acetabular component on a anteroposterior radiograph centred on the hip joint [14]. Polyethylene wear was measured using digital radiographs (Kodak© Picture Archiving and Communication System on a liquid crystal display) according to the technique described by Martell and Berdia [15] and based on edge detection and vector wear. This technique is thought to one of the most accurate measures available to assess polyethylene wear, with an accuracy of ±0.08 mm compared with specimens retrieved at autopsy [16]. A wear rate of ≥0.2 mm a year was defined as excessive [17]. Volumetric wear was calculated using the identified linear wear measurement, which assumes the femoral head creates a cylindrical wear track in the polyethylene liner. The formula to calculate this is: v = πr2w, where v is volume change, r is the radius of the femoral head and w is linear wear measurement [16]. Radiograph magnification was adjusted according to the size of the femoral head to ensure all measurements were comparable. Radiographs were assessed by a single trained observer blinded to other parameters for lucent lines (<2 mm) and osteolysis, which were described according to the three zones defined by DeLee and Charnley [18] for the acetabulum and by Gruen, McNiece and Amstutz [19] for proximal femur zones.
Functional outcome and satisfaction
Patients alive at the last follow-up and without revision were asked to complete an OHS [20] and record their level of satisfaction with their THR. The OHS consists of 12 questions assessed on a Likert scale, with values from 0 to 4; a summative score is then calculated, in which 48 is the best possible score (least symptomatic) and 0 is the worst possible score (most symptomatic). The outcome of this score was then graded into excellent (42–48), good (34–41), fair (27–33) and poor (0–26) according to Kalairajah et al. [21]. Patient satisfaction was assessed by asking the question: “How satisfied are you with your operated hip?” The response was recorded using a 5-point Likert scale: very satisfied, satisfied, neutral, unsatisfied and very unsatisfied. Patients were then categorised into those satisfied (very satisfied and satisfied) and those not (neutral, unsatisfied, and very unsatisfied), which has been used previously to assess patient satisfaction after THR [22].
Statistical analysis
Statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Unpaired Student’s t test and analysis of variance (ANOVA) were used to compare linear variables between groups. Pearson’s correlation was used to assess the relationship between linear variables. Dichotomous variables were assessed using a chi-square test. Kaplan–Meier methodology [23] and a life table was used to investigate implant survival [24]. Cox regression analysis was used to identify independent predictors of implant survival. A p value of ≤0.05 determined statistical significance.
Ethical approval was obtained for this study from the regional ethics committee.
Results
No patient was lost to follow-up; however 18 patients died during the study period. Mean cohort age at time of surgery was 59.1 years [standard deviation (SD) 12.6, range 24–90 years]. There were 58 men and 39 women, with a mean age of 58.9 (SD 10.6) and 59.4 (SD 15.3) years, respectively (p = 0.86 t-test). Median follow-up for all patients, including those who had died or had been revised (taken as time of revision), was 10.8 years, with an interquartile range of 7.7–12.4 years.
Survival
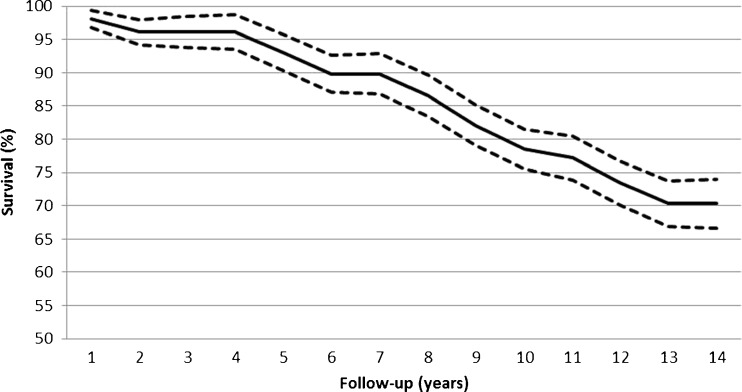
There were 24 revisions during the study period and a periprosthetic femoral fracture two years postoperatively, which was fixed without revision of the acetabular component. There were four early (under two years) revisions performed for recurrent dislocation in three patients, and one had a liner exchange because it had become disengaged ten months after surgery. The further 20 revisions were performed because of polyethylene wear with progressive secondary osteolysis or symptomatic loosening, with a fatigue fracture of the femoral stem in two patients. The all-cause survival rate for the acetabular component at ten years was 77.2 % [95 % confidence interval (CI) 73.9–80.5] (Table 1). The all-cause survival rate was generally static for the first five years after early revisions for dislocation and liner dissociation, but after this time point, survivorship steadily declined to 70 % at 13 years (Fig. 1). The survival rate for aseptic loosening (n = 17) of the acetabular component at ten years was 80.0 % (95 % CI 74.8–85.2). However, this decreased to 74.0 % (95 % CI 69.4–78.6) for intension to treat survival at ten years, as an additional five patients were offered revision due to progressive osteolysis and pain but declined to undergo revision surgery at that time. Neither age (p = 0.52), gender (p = 0.64), surgeon (p = 0.85) nor date of index procedure (p = 0.34) were significant predictors of aseptic revision of the acetabular component (Cox regression analysis).
Table 1.
Life table for survival of the uncemented Reflection acetabular component
| Years since operation | Number at start | Failure | Withdrawn | Number at risk | Annual failure rate (%) | Cumulative survival | 95 % confidence interval | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| 0–1 | 104 | 2 | 1 | 103.5 | 1.9 | 98.1 | 96.7 | 99.4 |
| 1–2 | 101 | 2 | 1 | 100.5 | 2.0 | 96.1 | 94.3 | 98.0 |
| 2–3 | 98 | 0 | 2 | 97 | 0.0 | 96.1 | 93.8 | 98.4 |
| 3–4 | 96 | 0 | 3 | 94.5 | 0.0 | 96.1 | 93.5 | 98.8 |
| 4–5 | 93 | 3 | 0 | 93 | 3.2 | 93.0 | 90.3 | 95.8 |
| 5–6 | 90 | 3 | 4 | 88 | 3.4 | 89.8 | 87.0 | 92.7 |
| 6–7 | 83 | 0 | 1 | 82.5 | 0.0 | 89.8 | 86.8 | 92.9 |
| 7–8 | 82 | 3 | 1 | 81.5 | 3.7 | 86.5 | 83.5 | 89.6 |
| 8–9 | 78 | 4 | 1 | 77.5 | 5.2 | 82.1 | 79.1 | 85.1 |
| 9–10 | 73 | 3 | 6 | 70 | 4.3 | 78.6 | 75.6 | 81.6 |
| 10–11 | 64 | 1 | 14 | 57 | 1.8 | 77.2 | 73.9 | 80.5 |
| 11–12 | 49 | 2 | 16 | 41 | 4.9 | 73.4 | 70.1 | 76.7 |
| 12–13 | 31 | 1 | 15 | 23.5 | 4.3 | 70.3 | 66.9 | 73.7 |
| 13–14 | 15 | 0 | 14 | 8 | 0.0 | 70.3 | 66.6 | 74.0 |
Fig. 1.
Kaplan–Meier curve, with 95 % confidence intervals (dashed lines), for all-cause survival of the uncemented Reflection acetabular component
Radiographic assessment
Radiographs were available for 83 (80 %) of the 104 THR performed. The reason for the loss of 12 patients’ radiographs was due to their death, and the policy at the study institute is to destroy radiographs four years after a patient’s death. The additional nine radiographs were unavailable due to revision surgery performed prior to digital archiving and were not available for assessment. The mean inclination angle of the acetabular component was 44.2° (SD 5.8°, range 31–55°). Only three patients had an inclination angle <35°; one had an inclination angle >55° [25]. There was no significant difference in inclination angle between the four surgeons performing the surgery (p = 0.54 ANOVA).
Mean linear wear was 0.20 mm (SD 0.08) per year; volumetric wear was 106.2 mm3 per year. The rate of linear and volumetric wear were directly proportional to age, with younger age being associated with an increased wear rate (r = 0.46, p < 0.001 Pearson’s test). In addition, male gender was associated with an increased rate of linear (0.21 mm vs 0.17 mm per year, p = 0.001 t test) and volumetric (111.5 mm3 vs 90.3 mm3 per year, p = 0.001 t test) wear compared with women. There was no significant association between cup inclination angle and polyethylene wear (p = 0.67, Pearson’s test), or rate of wear between the four surgeons performing the surgery (p = 0.78 ANOVA).
All 83 radiographs, including those prior to revision, were assessed for lucent lines and osteolysis. There was a high rate of both lucent lines and osteolysis (up to 99 %), with more than 20 % of patients having osteolysis in acetabular DeLee zones 2 and 3, and more than half of the patients had osteolysis in femoral Gruen zone 7 (Table 2). It is interesting to note that one in five patients had osteolysis in Gruen zones 1, 2, 6 and 7 (Fig. 2), which resulted in two stem failures because of cantilever bending (Fig. 3).
Table 2.
Rate of lucent lines and osteolysis for total hip replacement (THR) with an uncemented Reflection acetabular component according to zones defined by DeLee and Gruen (n = 83)
| Classification zones | Lucent line [n, (%)] | Osteolysis [n, (%)] | Total [n, (%)] | |
|---|---|---|---|---|
| Delee | 1 | 33 (39.8) | 9 (10.8) | 42 (50.6) |
| 2 | 44 (53.0) | 19 (22.9) | 63 (75.9) | |
| 3 | 30 (36.1) | 18 (21.9) | 48 (57.8) | |
| Gruen | 1 | 23 (27.7) | 35 (42.2) | 58 (69.9) |
| 2 | 19 (22.9) | 28 (33.7) | 47 (56.6) | |
| 3 | 11 (13.3) | 11 (13.3) | 22 (26.5) | |
| 4 | 4 (4.8) | 3 (3.6) | 7 (8.4) | |
| 5 | 11 (13.3) | 9 (10.8) | 20 (24.1) | |
| 6 | 20 (24.1) | 33 (39.8) | 53 (63.9) | |
| 7 | 33 (39.8) | 49 (59.0) | 82 (98.8) | |
Fig. 2.
Radiograph demonstrating marked osteolysis around both total hip replacements (THR): the left was 8 years and the right 9 years from time of surgery. This pattern of proximal femoral osteolysis in Gruen zones 1, 2, 6 and 7, in association with cortical thickening in zones 3–5 was a typical observation in patients with polyethylene wear. In addition, on the right side a small area of osteolysis in DeLee zone 2 can be seen, which typically continues to progress to involve zone 3 with continued polyethylene wear
Fig. 3.
Failure of the femoral stem due to proximal femoral lysis 8 years from surgery
Functional outcome and satisfaction
There were 80 patients not revised during the study period, but 17 of them had died and an additional nine were not willing to participate in the completion of their OHS. This left 54 patients, 37 men and 17 women, with a mean age of 68.3 years, who completed both the OHS and satisfaction assessments. Mean OHS was 35.6 (SD 9.8, range 20–46) at a mean follow-up of 11.9 years. According to the grading system of Kalairajah et al. [21], postoperative OHS showed six (11.1 %) excellent, 26 (48.1 %) good, 17 (31.5 %) fair and five (9.3 %) poor outcomes. Despite the fact that more than a third had a fair or poor outcome according to their OHS, only four (7.4 %) were not satisfied with their THR.
Discussion
This study demonstrates a high rate of polyethylene wear associated with the uncemented Reflection acetabular component used as a part of THR. Associated with this increased rate of polyethylene wear, approximately one in five patients had osteolysis in one or more zones around the acetabular component, and more than half had osteolysis in one or more zones around the femoral component. This was associated with an aseptic acetabular component survival rate of 80 % at ten years (74 % ten-year survival on an intention to revise basis). Forty percent of patients who retained their original THR had a fair or poor functional outcome; however 93 % remained satisfied with their hip.
The main limitation of our study is the number of patients assessed; 98 patients is a relatively small series compared with other authors reporting the outcome of the uncemented Reflection acetabulum [10–12]. However, we report a consecutive series of patients, with no loss to follow-up, at a single study centre that has a defined catchment population and is the sole public hospital offering orthopaedic services to that population, all of which support the accuracy of our findings. In addition, although it could be argued that survivorship may be affected by the fact there were four different consultant surgeons performing the surgery, there was no difference in the acetabular component inclination angle, wear rate or revision rate between these surgeons.
The reason the accelerated polyethylene wear rate and associated increased revision rate observed for our cohort is worse than that reported in the literature for the uncemented Reflection cup is not clear. Civinini et al. [9] reported a similar-sized cohort of 118 THR in 98 patients. They illustrated an all-cause survival rate of 96 % at ten years and 95 % if osteolysis was taken as the end point. This figure is supported by a more recent series of 363 THR by Teo et al. [10] demonstrating a 94 % ten-year and a 90 % 15-year all-cause survival rate. Those authors also found an impressive 99 % 15-year survival rate for the Reflection shell. However, in contrast, Crockarell [11] described an 88 % (n = 19/158) survival rate at five years, of which eight patients had complications due to liner wear and a further six were advised to have revision surgery for progressive osteolysis. Our longer-term results support the reduced five-year survival rates identified by him, with nearly identical results at that time point. He hypothesised that this early failure rate was due to ethylene oxide sterilisation, without radiation, of the polyethylene used for the Reflection cup. This has been shown to almost double the rate of wear compared with polyethylene sterilised with gamma irradiation in an inert gas [26]. Despite the differing survivorships reported by Teo et al. [10] and Crockarell [11], both reports note an identical linear wear rate of 0.15 mm per year, which is 0.05 mm less than our cohort. However, even this rate is more than that observed with a cemented acetabular polyethylene component [7, 27]. In addition, Teo et al. [10] observed a high rate of osteolysis in around 29 % of femoral components and 20 % of acetabular components. Crockarell [11] also found in his series of 38 THR that osteolysis was present in 53 % of hips, which is similar to the rate in our series. The reason we observed an increased wear rate may relate to our relatively younger patients (compared with Teo et al. [10]) and a greater rate in men (60 %) compared with the other two studies.
All comparative studies reporting wear rates between cemented and uncemented cups identify an equal or increased articular wear rate with uncemented fixation [7]. Similar findings were reported using radiostereometric methodology [28]. Wear rates and early osteolysis in uncemented designs can be rapid and extensive, with overall survival between 50 % and 70 % after 12–16 years of observation [29]. It was suggested that this may be because cement absorbs some of the stress and thus reduces forces on the polyethylene [30]. Also, backside polyethylene wear, which is a well-documented phenomenon with uncemented designs, may contribute to the increased wear rate [27]. Bjerkholt et al. [31] recently compared polyethylene wear between cemented and uncemented acetabular cups in a multivariate analyses. They demonstrated a significantly increased rate of wear in younger patients and with an increasing inclination angle but not with fixation type. This accelerated wear is thought to be related to the increased level of activity of younger patients, although irrespective of age, wear is thought to be a function of use, not time [32]. In addition, Bjerkholt et al. [31] illustrated a significant association between the degree of inclination and wear, with uncemented cups being inserted with a higher degree of inclination than cemented cups. These facts support the notion that uncemented cups do not wear more than cemented cups in the long term provided the correct orientation is obtained. The correct orientation is, however, more difficult to achieve with uncemented fixation, as emphasised by Chawda et al. [33] in a comparative trial using navigation.
The rate of polyethylene wear associated with the Reflection acetabular component may be a cause for concern, with an increased rate of radiographic osteolysis and revision surgery that seems to be relatively asymptomatic. As a result of this study, our departmental policy now allows annual review of the surviving patients in anticipation of continued polyethylene wear, with secondary osteolysis and implant failure a future possibility.
Acknowledgments
The authors thank Mr. Richard Nutton for allowing his patients to be included in the study cohort.
References
- 1.Makela KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 2.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 3.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988;70:337–346. [PubMed] [Google Scholar]
- 5.Dodge BM, Fitzrandolph R, Collins DN (1991) Noncemented porous-coated anatomic total hip arthroplasty. Clin Orthop Relat Res (269):16–24 [PubMed]
- 6.Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992;74:63–66. doi: 10.1302/0301-620X.74B1.1732268. [DOI] [PubMed] [Google Scholar]
- 7.Clement ND, Biant LC, Breusch SJ (2011) Total hip arthroplasty: to cement or not to cement the acetabular socket? A critical review of the literature. Arch Orthop Trauma Surg 132(3):411–427 [DOI] [PubMed]
- 8.Smith & Nephew (1996) Reflection I & V porous-coated acetabular component: surgical technique. Smith 7 Nephew, Memphis. http://www.bonerepmedical.com/main_site/surgical_techniques/Reflection.pdf
- 9.Civinini R, D’Arienzo M, Innocenti M. A ten-year follow-up of the Reflection cementless acetabular component. J Bone Joint Surg Br. 2008;90:570–573. doi: 10.1302/0301-620X.90B5.20116. [DOI] [PubMed] [Google Scholar]
- 10.Teo YS, Corten K, McCalden RW, MacDonald SJ, Bourne RB. The minimum 10-year results of a second-generation cementless acetabular shell with a polished inner surface. J Arthroplasty. 2012;27:1370–1375. doi: 10.1016/j.arth.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Crockarell JR., Jr Polyethylene sterilized without irradiation in a polished uncemented acetabular component-a clinical and radiographic analysis. J Arthroplasty. 2008;23:911–915. doi: 10.1016/j.arth.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 12.Hallan G, Dybvik E, Furnes O, Havelin LI. Metal-backed acetabular components with conventional polyethylene: a review of 9113 primary components with a follow-up of 20 years. J Bone Joint Surg Br. 2010;92:196–201. doi: 10.1302/0301-620X.92B2.22179. [DOI] [PubMed] [Google Scholar]
- 13.General Register Office for Scotland (2010) GROS Mid-2008 population estimates scotland: population estimates by sex, age and administrative area http://www.gro-scotland.gov.uk/files2/stats/gros-mid-2008-population-estimates-scotland-population-estimates-by-sex-age-and-administrative-area/j1075008.htm (date last accessed 16th April 2013)
- 14.Goosen JH, Verheyen CC, Tulp NJ. Mid-term wear characteristics of an uncemented acetabular component. J Bone Joint Surg Br. 2005;87:1475–1479. doi: 10.1302/0301-620X.87B11.16101. [DOI] [PubMed] [Google Scholar]
- 15.Martell JM, Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635–1641. doi: 10.2106/00004623-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Rahman L, Cobb J, Muirhead-Allwood S. Radiographic methods of wear analysis in total hip arthroplasty. J Am Acad Orthop Surg. 2012;20:735–743. doi: 10.5435/JAAOS-20-12-735. [DOI] [PubMed] [Google Scholar]
- 17.Puolakka TJ, Laine HJ, Moilanen TP, Koivisto AM, Pajamaki KJ. Alarming wear of the first-generation polyethylene liner of the cementless porous-coated Biomet Universal cup: 107 hips followed for mean 6 years. Acta Orthop Scand. 2001;72:1–7. doi: 10.1080/000164701753606608. [DOI] [PubMed] [Google Scholar]
- 18.DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res (121):20–32 [PubMed]
- 19.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res (141):17–27 [PubMed]
- 20.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 21.Kalairajah Y, Azurza K, Hulme C, Molloy S, Drabu KJ. Health outcome measures in the evaluation of total hip arthroplasties—a comparison between the Harris hip score and the Oxford hip score. J Arthroplasty. 2005;20:1037–1041. doi: 10.1016/j.arth.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 22.Clement ND, MacDonald D, Howie CR, Biant LC. The outcome of primary total hip and knee arthroplasty in patients aged 80 years or more. J Bone Joint Surg Br. 2011;93:1265–1270. doi: 10.1302/0301-620X.93B9.25962. [DOI] [PubMed] [Google Scholar]
- 23.Kaplan EL, Meier P. Nonparametric estimation from incomplete observation. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 24.Murray DW, Carr AJ, Bulstrode C. Survival analysis of joint replacements. J Bone Joint Surg Br. 1993;75:697–704. doi: 10.1302/0301-620X.75B5.8376423. [DOI] [PubMed] [Google Scholar]
- 25.Sarmiento A, Ebramzadeh E, Gogan WJ, McKellop HA. Cup containment and orientation in cemented total hip arthroplasties. J Bone Joint Surg Br. 1990;72:996–1002. doi: 10.1302/0301-620X.72B6.2246305. [DOI] [PubMed] [Google Scholar]
- 26.Digas G, Thanner J, Nivbrant B, Rohrl S, Strom H, Karrholm J. Increase in early polyethylene wear after sterilization with ethylene oxide: radiostereometric analyses of 201 total hips. Acta Orthop Scand. 2003;74:531–541. doi: 10.1080/00016470310017910. [DOI] [PubMed] [Google Scholar]
- 27.McCombe P, Williams SA. A comparison of polyethylene wear rates between cemented and cementless cups. A prospective, randomised trial. J Bone Joint Surg Br. 2004;86:344–349. doi: 10.1302/0301-620X.86B3.14567. [DOI] [PubMed] [Google Scholar]
- 28.Onsten I, Carlsson AS, Besjakov J. Wear in uncemented porous and cemented polyethylene sockets: a randomised, radiostereometric study. J Bone Joint Surg Br. 1998;80:345–350. doi: 10.1302/0301-620X.80B2.8032. [DOI] [PubMed] [Google Scholar]
- 29.Hallan G, Lie SA, Havelin LI. High wear rates and extensive osteolysis in 3 types of uncemented total hip arthroplasty: a review of the PCA, the Harris Galante and the Profile/Tri-Lock Plus arthroplasties with a minimum of 12 years median follow-up in 96 hips. Acta Orthop. 2006;77:575–584. doi: 10.1080/17453670610012638. [DOI] [PubMed] [Google Scholar]
- 30.Hernandez JR, Keating EM, Faris PM, Meding JB, Ritter MA. Polyethylene wear in uncemented acetabular components. J Bone Joint Surg Br. 1994;76:263–266. [PubMed] [Google Scholar]
- 31.Bjerkholt H, Hovik O, Reikeras O. Direct comparison of polyethylene wear in cemented and uncemented acetabular cups. J Orthop Traumatol. 2010;11:155–158. doi: 10.1007/s10195-010-0104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmalzried TP, Shepherd EF, Dorey FJ. Wear is a function of use not time. Clin Orthop Relat Res. 2000;381:36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Chawda M, Hucker P, Whitehouse SL, Crawford RW, English H, Donnelly WJ. Comparison of cemented vs uncemented acetabular component positioning using an imageless navigation system. J Arthroplasty. 2009;24:1170–1173. doi: 10.1016/j.arth.2008.09.018. [DOI] [PubMed] [Google Scholar]