Abstract
Purpose
The question arises as to whether it is possible to obtain rigid fixation of the ultra-short metaphyseal-fitting anatomic cementless stem without diaphyseal fixation in the elderly as well as younger patients. We investigated whether ultra-short, metaphyseal-fitting anatomic cementless femoral stem would provide similar functional improvements in the younger and elderly patients, radiographically secure implant fixation would be achieved in both groups, the bone content would be preserved in both groups, and complication rates would be similar in both groups.
Methods
A total of 100 patients (114 hips) in the younger patient group and 100 patients (112 hips) in the elderly patient group were included in the study. Their mean age was 43.9 ± 6.11 years (range, 31–65 years) in the younger patient group and 78.9 ± 12.1 years (range, 66–91 years) in the elderly patient group. The mean duration of follow-up was 7.5 years (range, six to nine years) in the younger patient group and 7.6 years (range, six to nine years) in the elderly patient group.
Results
The mean postoperative Harris hip scores (95 points versus 91 points), WOMAC scores (11 points versus 15 points), thigh pain (none in either group), UCLA activity scores (6.5 points versus 4.5 points), and radiographic results were not significantly different between the two groups. No hip in either group had an aseptic loosening. No hip in either group had clicking or squeaking sounds or ceramic fractures.
Conclusion
The cementless ultra-short, metaphyseal-fitting anatomic cementless femoral component provides stable fixation without any need of diaphyseal fixation in both younger and elderly patients. Despite the concern, the poor bone quality in elderly patients did not compromise the stability, and osseointegration of this ultra-short, anatomic cementless femoral stem was achieved in all elderly patients.
Keywords: Ultra-short stem, Ultra-short stemmed hip replacement, Metaphyseal fitting anatomic cementless femoral component, Osteoarthritis, Osteonecrosis, Hip replacement
Introduction
Although the results of modern cemented or cementless total hip arthroplasty (THA) are generally good [1–15], thigh pain, stress shielding and periprosthetic fracture are still potential problems [2, 6–9]. In an effort to reduce the periprosthetic fracture, thigh pain, and stress shielding, an ultra-short, anatomic metaphyseal-fitting cementless femoral component was developed.
Ultra-short stem requires less resection of the upper femur and/or less reaming of the femoral shaft. This serves a dual purpose of facilitating future revision while providing a postoperative state closely mimicking the originally functioning hip [16–18]. This ultra-short stem provided vertical stability by the wedge shape of the stem with the addition of a lateral flare and preservation of the femoral neck. Preservation of femoral neck provides greater torsional stability and reduces distal migration of the femoral stem [19]. The absence of the distal stem fixation is allowed because of the effective stability given by the lateral flare and preservation of the femoral neck. The absence of the diaphyseal anchorage attempts proximal load transfer to reduce stress shielding, thigh pain, and periprosthetic fracture. It also attempts preservation of the femoral canal and femoral elasticity, and ease of revision [6]. The question thus arises as to whether it is possible to obtain rigid fixation of this cementless ultra-short stem without diaphyseal fixation in the elderly as well as in younger patients.
We investigated whether (1) an ultra-short, anatomic metaphyseal-fitting cementless femoral stem would provide similar functional improvements in the young and elderly patients, (2) radiographically secure implant fixation would be achieved with this ultra-short stem in both young and elderly patients, (3) the bone content would be preserved at the baseline level or above at the final follow-up in both groups, and (4) complication rates including periprosthetic fracture, dislocation, and/or squeaking or clicking sounds would be similar in both groups.
Materials and methods
From May 2004 to January 2007, 114 primary THAs were performed in 100 unselected, consecutive patients less than 65 years old, and 122 primary THAs were performed in 110 unselected, consecutive patients more than 66 years old. In the younger patient group, no patient was lost to follow-up after the operation, and no patient died in the interim. Therefore, all patients were available for clinical evaluation. In the elderly patient group, five patients died from unrelated causes and five were lost to follow-up less than two years after the operation. A total of 15 patients who were unable to return for follow-up completed a telephone questionnaire, and responded to a request to send recent radiographs. Therefore, 100 patients (112 hips) were available for clinical evaluation in the elderly patient group. The study was approved by our institutional review board and all patients provided informed consent. Osteonecrosis (61 %) was the predominant diagnosis for THAs in the younger patient group and osteoarthritis (52 %) was the predominant diagnosis in the elderly patient group (Table 1).
Table 1.
Patient demographics
| Parameters | Younger group (< 65 years) | Elderly group (> 66 years) | P-value |
|---|---|---|---|
| Number of patients (hips) | 100 (114) | 100 (112) | |
| Male:female ratio | 56/44 | 45/55 | 0.134c |
| Agea (years) | 43.9 ± 6.11 (31–50) | 78.9 ± 12.11 (66–91) | 0.0001d |
| Weighta (kg) | 76.3 ± 9.23 (56–104.8) | 78.5 ± 10.5 (59–109) | 0.412d |
| Heighta (cm) | 165.1 ± 8.73 (148–185) | 161 ± 9.72 (145–184) | 0.613d |
| Body mass index (height/m2)a | 28.3 ± 4.4 (25.5–30.8) | 30.2 ± 4.2 (28.1–32) | 0.591 |
| Diagnosis | |||
| Osteonecrosis | 61 (61 %) | 36 (36 %) | 0.457c |
| Osteoarthritis | 19 (19 %) | 52 (52 %) | |
| Developmental dysplastic hip | 16 (16 %) | – | |
| Traumatic arthritis | 4 (4 %) | – | |
| Femoral neck fracture | – | 12 (12 %) | |
| Follow-upb (years) | 7.5 (6−9) | 7.6 (6−6) | 0.615d |
aThe values are given as the mean and the standard deviation, with the range in parentheses
bThe value is given as the mean, with the range in parentheses
cChi-square test
dStudent t-test
All of the operations were performed by the senior author (YHK) using a posterolateral approach. A fully porous-coated cementless pinnacle acetabular component (DePuy, Warsaw, Indiana) with a 36-mm (inner diameter) Biolox delta ceramic liner (Ceram Tec AG, Polchingen, Germany) was used in all of the hips in both groups. The acetabular components were press-fitted after the under-reaming by 1 mm, and in 15 hips (13 %) in the younger patient group and in 28 hips (25 %) in the elderly patient group one or two screws were used for additional fixation. The acetabular component sizes ranged from 52 mm to 58 mm. The acetabular component was fixed between 40° and 45° inclination and between 20° and 30° anteversion.
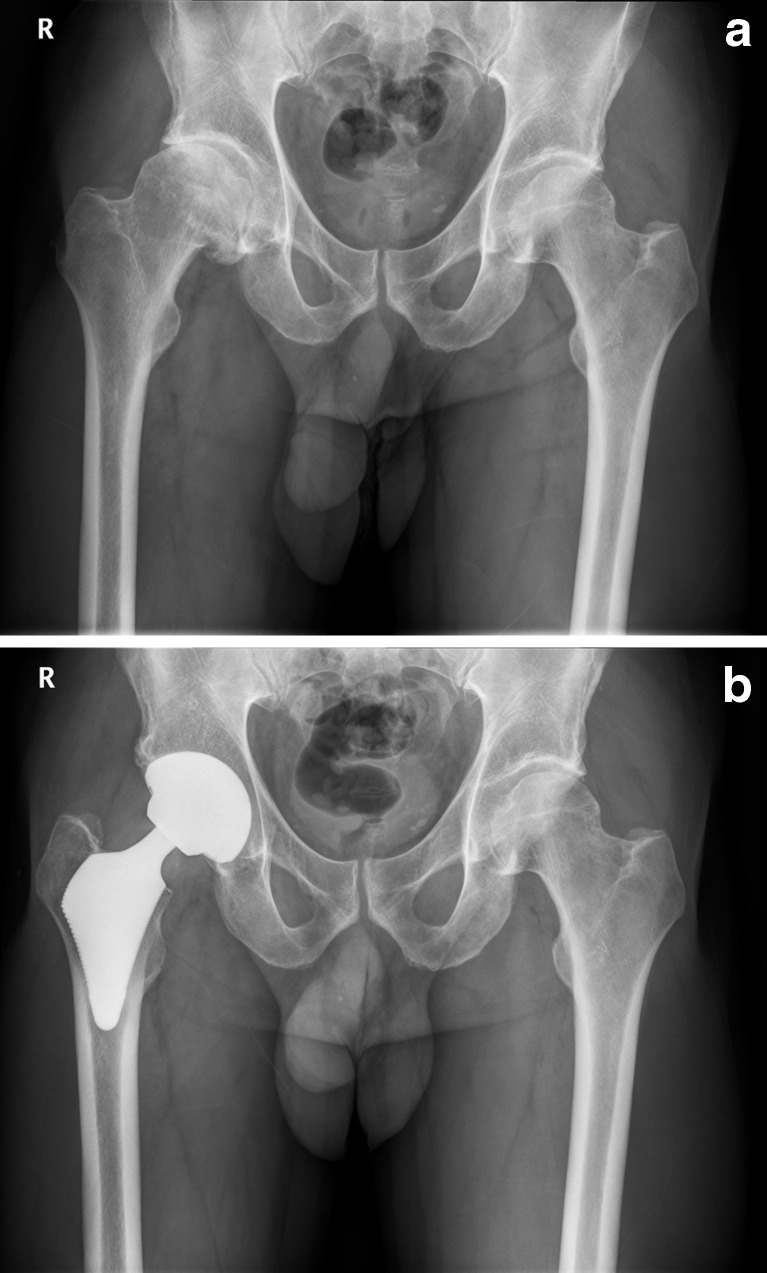
All patients in both groups received an ultra-short, anatomic metaphyseal-fitting cementless femoral component (Proxima; DePuy, Leeds, United Kingdom) with a 36-mm Biolox delta ceramic modular head (Ceram Tec). This ultra-short stem is made of titanium alloy and is entirely porous-coated with sintered titanium beads having a mean pore size of 250 μm, to which a 30-μm thick hydioxyapatite coating is applied, except for the distal tip. The design features are a longer proximomedial portion of the stem, a highly pronounced lateral flare and preservation of the femoral neck (Fig. 1).
Fig. 1.
Radiographs of a 49-year-old man with osteoarthritis of the right hip joint and Dorr type A bone. a Preoperative radiograph of both hips reveals complete loss of cartilaginous space of right hip joint. b Postoperative radiograph of both hips obtained nine years after surgery shows that Proxima stem is solidly fixed in a satisfactory position in the right hip
The femoral neck was cut horizontally at the cervicocapital juncture, because preservation of the femoral neck is required for axial and torsional stability of the stem [18, 20]. A “round-the-corner” technique [17, 18] was used for femoral broaching and insertion of the implant. The broaches and implants were inserted in a slight varus position and then rotated into the correct alignment. Adequate cancellous bone (2–3 mm) for osseointegration was left in the proximal femur. The size of the femoral component which was selected matched the size of the largest broach used. The dimension of the real component was 0.5 mm larger than that of the prepared metaphysis.
Patients in both groups were allowed to stand on the second postoperative day and then progressed to full-weight-bearing activity with crutches as tolerated. They were advised to use crutches for six weeks and to use a cane thereafter as needed.
The patients in both groups were reviewed at three months, one year, and yearly thereafter. Radiographs were taken one week after surgery and at each follow-up evaluation. The Harris hip score [21] was determined before surgery and at each follow-up, as was the Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) score [22]. Thigh pain was scored on a 10-point visual analog scale [23] where 0 = no pain and 10 = severe pain, and activity was assessed using the University of California, Los Angles (UCLA) score [24] at each follow-up. All the data were obtained by one observer who was not part of the surgical team. The mean follow-up was 7.5 years (range, six to nine years) in the younger patient group and 7.6 years (range, six to nine years) in the elderly patient group.
The occurrence of any clicking or squeaking sound emanating from the ceramic-on-ceramic bearing was recorded.
A supine anteroposterior radiograph of the pelvis with both hips in 15° internal rotation and no abduction, and a cross-table lateral radiograph of each, were obtained immediately after operation and at each follow-up visit. The femoral morphology was determined pre-operatively using Dorr’s system of classification [25]. The position of the femoral component in the anteroposterior and lateral planes was assessed.
The radiographs were analysed by a research associate for stability of the components. They were classified as osseointegrated, fibrous stable, or unstable [3]. Components that showed spot welds were considered osseointegrated. Those that lacked definite ingrowth, but had no progressive lucency or change in position, were designated as fibrous stable, and those with clear signs of loosening, including axial or angular migration, were classified as unstable. Subsidence of the femoral component was evaluated by measuring the distance between the tip of the greater trochanter and the upper margin of the lateral flare of the stem, as well as the distance between the most proximomedial part of the porous-coated surface of the stem and the upper border of the lesser trochanter. These values in the anteroposterior radiographs taken one week after the operation were compared with those taken at the final follow-up to define the subsidence of the stem. The intraobserver error for this measurement was determined by the intraclass correlation coefficient after the measurements were repeated three times at intervals of three days. This result was 0.95 (0.94–1.0), indicating excellent reproducibility. A linear change of 2 mm or an angular change of 5°, bead-shedding and increased circumferential lucency were considered to be signs of loosening of the acetabular component. A vertical change in its position was measured between its inferior margin and the inferior margin of the ipsilateral teardrop, and a horizontal change was measured between the Köhler line and the center of the outer shell. The intraclass correlation coefficient was 0.96 (0.95–1.0).
Stress-shielding was graded on the radiographs at the final follow-up according to the classification of Engh et al. [3]. The size and location of osteolytic lesions were assessed using the technique described by Zicat et al. [26].
All of the patients in both groups underwent dual-energy X-ray absorptiometry (DEXA) scanning of the pelvis and proximal femur (zones 1 and 7) using a Hologic QDR 4500A densitometer (Hologic Inc., Waltham, Massachusetts) in the metal-removal hip-scanning mode preoperatively and at final follow up. [16].
Based on power analysis, we estimated a sample size of 95 patients in each group. We detected a three-point difference in the mean Harris hip score between the two groups, with a standard deviation of 3.5 points, a two-sided p value of 0.05, and an approximate power of 80 %. We calculated the descriptive statistics (mean, standard deviation and proportions) for the continuous study variables. The Harris hip score was the primary outcome variable. This variable was analysed with Student’s independent t-test. Radiographic and bone mineral density data were compared between the two groups using Student’s independent t-test. Complication rates were compared between the two groups with a chi-square test. All statistical analyses were performed with the Statistical Package for the Social Sciences (version 14.0, SPSS Inc., Chicago, Illinois) and statistical significance was set at P < 0.05.
Results
Comparison of mean pre-operative and postoperative Harris hip scores, pain scores, function scores, WOMAC scores, patient activity score and level of thigh pain revealed no significant differences between the two groups (Table 2). The mean preoperative Harris hip scores were 43 points (range, 17–51 points) in the younger patient group and 36 points (range, 10–55 points) in the elderly group. The mean postoperative Harris hip scores were 95 points (range, 85–100 points) in the younger patient group and 91 points (range, 71–100 points) in the elderly patient group. The mean postoperative WOMAC scores were 11 ± 5.3 points (range, 6–18 points) in the younger patient group and 15 ± 6.5 points (range, 6–31 points) in the elderly patient group. The mean UCLA activity scores at the final follow-up were 6.5 points (range, 5–8 points) in the younger patient group and 4.5 points (range, 3–6 points) in the elderly patient group. All patients in both groups reported improved function and satisfaction with the outcome. No hip exhibited evident clicking or squeaking (Table 2). Dependence on walking aids had decreased substantially by the final follow-up. Preoperative function score, the ability to use stairs and public transportation, to put on footwear and to cut toenails were improved markedly after the operation in both groups. No patient had thigh pain at each follow-up.
Table 2.
Clinical results
| Parameter | Younger group (< 65 yrs) | Elderly group (> 66 yrs) | P value (Student’s t-test) | |||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | |
| Harris hip score (points)a | 43 (17−51) | 95 (85−100) | 36 (10–55) | 91 (61–100) | 0.131 | 0.078 |
| Pain score (points)a | 11.5 (0–31) | 43.5 (40−44) | 11.8 (8−30) | 42.8 (40−44) | 0.731 | 0.135 |
| Function score (points)a | 25.8 (0–40) | 51.5 (30−56) | 29.1 (10−40) | 48.2 (25−56) | 0.112 | 0.991 |
| WOMAC score (points)a | 61 ± 12.31 (45–86) | 11 ± 5.3 (6−18) | 63 ± 13.21 (48–78) | 15 ± 6.5 (6–31) | 0.110 | 0.131 |
| Thigh pain | – | None | – | None | ||
| UCLA activity score (points)a | – | 6.5 (5–8) | – | 4.5 (3–6) | – | 0.0001 |
| Clicking or squeaking sound | – | None | None | |||
a The values are given as the mean and the standard deviation, with the range in parentheses
WOMAC Western Ontario and McMaster Universities Osteoarthritis, UCLA University of California, Los Angles
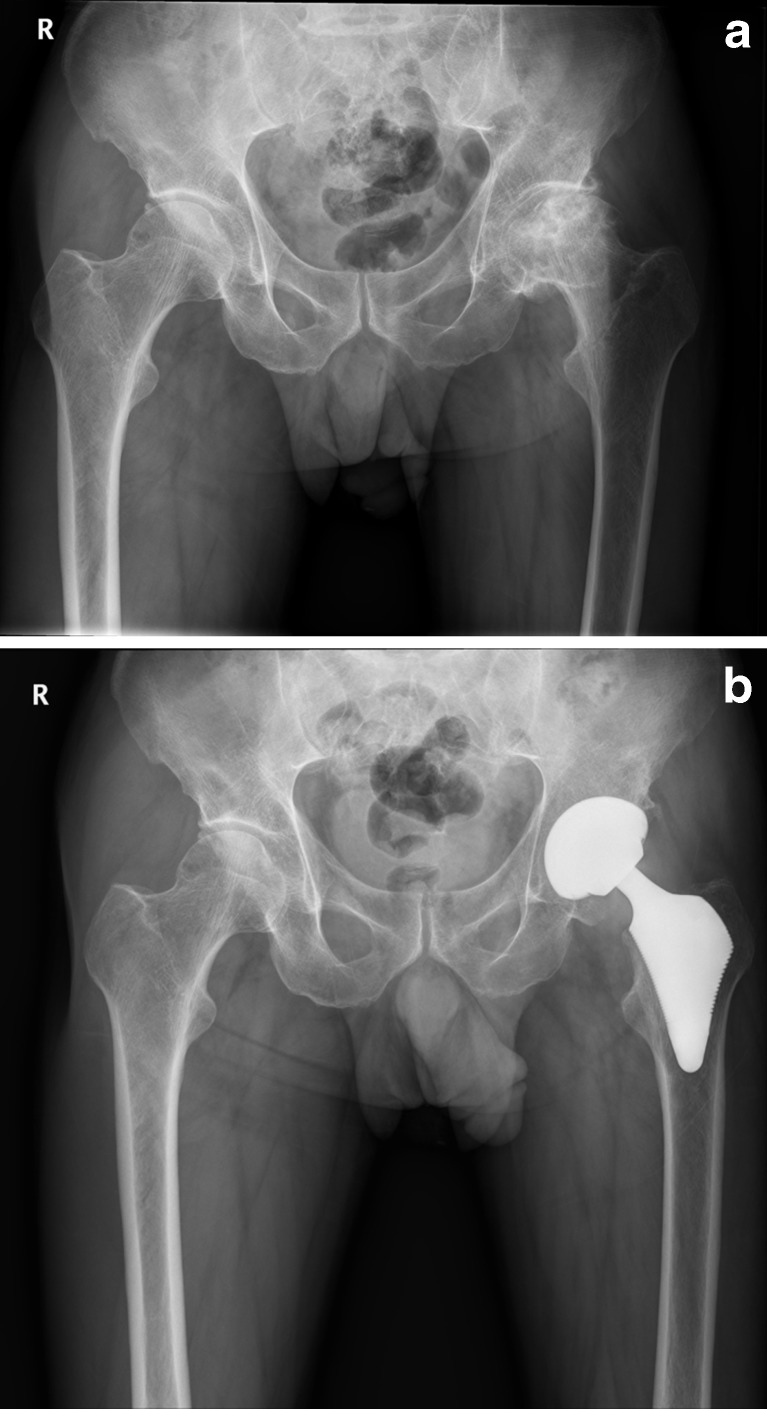
The morphology of the proximal femur in the younger patient group was Dorr type A in 108 hips (95 %) and type B in six hips (5 %). The morphology of the proximal femur in the elderly patient group was Dorr type A in 14 hips (12.5 %), type B in 28 hips (25 %) and type C in 70 hips (62.5 %). In the anteroposterior view 107 femoral components (94 %) were in a neutral position, five (4 %) were in a varus position, and two (2 %) were in a valgus position, and in the lateral view all were in an anatomic position in the young patient group. In the elderly patient group, 106 hips (95 %) were in a neutral position and six (5 %) were in a varus position in the anteroposterior view and all were in an anatomic position in the lateral view. There was no significant difference between the two groups in terms of the center of rotation, femoral offset, abductor moment arm, femoral neck length, limb length discrepancy, incidence of the radiolucent line or prevalence of the migration of the femoral component (Table 3). Osseointegration was seen in all of the acetabular and femoral components in both groups (Figs. 1 and 2). All of the hips in both groups exhibited grade 1 stress shielding in the calcar region [3]. No acetabular or femoral osteolysis was identified.
Table 3.
Radiographic results
| Parameters | Younger group (< 65 yrs) | Elderly group (> 66 yrs) | P value (Student’s t-test) |
|---|---|---|---|
| Dorr bone type [25] | |||
| A | 108 hips (95 %) | 14 hips (12.5 %) | <0.0001 |
| B | 6 hips (5 %) | 28 hips (25 %) | |
| C | – | 70 hips (62.5 %) | |
| Femoral component position | |||
| Neutral position | 107 hips (94 %) | 106 hips (95 %) | 0.912 |
| Varus position | 5 hips (4 %) | 6 hips (5 %) | |
| Valgus position | 2 hips (2 %) | – | |
| Sagittal plane | |||
| Anatomical | 114 hips (100 %) | 111 hips (100 %) | 1.000 |
| Center of rotation | |||
| Horizontal (mm) | 40.8 (34–47) | 39.8 (35–49) | 0.259 |
| Vertical (mm) | 14.9 (12–22) | 15.7 (11–25) | 0.192 |
| Femoral offset (mm) | 41.7 (34–49) | 41.3 (35–51) | 0.818 |
| Abductor moment arm (mm) | 45.1 (39−84) | 44.2 (37 −83) | 0.914 |
| Femoral neck length (mm) | 34.5 (29−42) | 35.1 (31−39) | 0.782 |
| Limb-length discrepancy (cm) | 0.3 ± 0.5 (−1.3–1.2) | 0.5 ± 0.6 (−1.3–1.3) | 0.705 |
| Radiolucent line (> 1 mm) | 0 hip (0 %) | 0 hip (0 %) | – |
| Migration of femoral Component (< 1 mm) but stabilized | 1 hip (1 %) | 1 hip (1 %) | – |
Fig. 2.
Radiographs of 75-year-old man with osteonecrosis of left femoral head. a Preoperative radiograph of left hip demonstrates collapse of left femoral head (Ficat stage IV) and Dorr type C bone. b Postoperative radiograph of left hip obtained nine years after surgery demonstrates that Proxima stem is rigidly fixed in a satisfactory position in left hip
Although bone mineral density indicated a significant variation in the manner in which the bone remodels around stem, overall bone mineral density was not significantly different between the two groups. In both groups, the bone mineral density at final follow-up was significantly increased in zone 1 but slightly decreased in zone 7 (Table 4).
Table 4.
Bone mineral density around Proxima stem in young and elderly patient groups
| Period | Younger group (< 65 yrs) | Elderly group (> 66 yrs) | ||
|---|---|---|---|---|
| Zone 1 | Zone 7 | Zone 1 | Zone 7 | |
| One week after surgery (g/cm2) | 3.128 ± 0.321 | 3.431 ± 0.328 | 2.893 ± 0.918 | 3.125 ± 0.219 |
| Six years after surgery (g/cm2) | 3.429 ± 0.387 | 3.108 ± 0.285 | 3.125 ± 0.112 | 2.830 ± 0.851 |
| Difference (%) | 0.301 ± 0.66 (9.6) | −0.323 ± 0.043 (−9.4) | 0.232 ± 0.806 (8.0) | −0.295 ± 0.632(−9.4) |
| P-value (paired t-test) | <0.001 | 0.165 | <0.001 | 0.168 |
No hip in either group displayed squeaking or clicking sounds, or ceramic fracture. One hip in each group had a fracture of the calcar. Each hip in both groups underwent open reduction and internal fixation with three Dall-Miles cables (Howmedica, Rutherford, New Jersey). The period of protected weight-bearing was extended by three months, with no additional precaution. These cases healed satisfactorily with osseointegration at the final follow-up. Two hips (1.8 %) with a femoral neck fracture in the elderly patient group exhibited recurrent dislocation. The acetabular components were revised to constrained polyethylene bearing, after which there was no further dislocation. One hip in the elderly group had calcar fracture extending to proximal femur after a fall five days after the operation. This hip was revised to an anatomical medullary locking (AML) stem (DePuy, Warsaw, Indiana).
Discussion
The question arises as to whether it is possible to obtain rigid fixation of the ultra-short metaphyseal fitting cementless anatomic stem without diaphyseal fixation in the elderly as well as in younger patients. We investigated whether an ultra-short anatomic metaphyseal-fitting cementless femoral stem would provide similar functional improvements in the young and elderly patients; radiographically secure implant fixation would be achieved with this ultra-short stem in both young and elderly patients; the bone content would be preserved at the baseline level or above at the final follow-up in both groups; and complication rate including periprosthetic fracture, dislocation, and/or squeaking or clicking sounds would be similar in both groups.
This study has certain limitations. First, we prospectively collected all of the data, but the study was not randomized and there was no control group in which a different component or different surgical technique was used to compare and contrast outcomes. Second, the duration of follow-up was short and was thus insufficient to allow conclusions to be drawn, because most prostheses exhibit good results at five years after the operation. However, the findings from these two studies [3, 23] clearly indicate that a femoral stem which is stable at five years after the operation is likely to maintain a long-term stable fixation of the femoral component.
We obtained rigid fixation of this cementless ultra-short, metaphyseal-fitting anatomic cementless femoral stem without any diaphyseal fixation in all of the hips in a younger patient group and all but one patient in the elderly patient group. These results are similar to those reported for conventional cementless femoral stems [3–5, 7, 10, 27] and other short stems [18, 28]. We found that poor bone quality was not a contraindication and that stable fixation of this short, femoral stem was achievable in osteoporotic bone, as was also reported by McAuley et al. [7] with their extensively porous-coated diaphyseal fixation femoral stem. We believe that the satisfactory results using this ultra-short, metaphyseal-fitting cementless femoral component in both groups of patients can be attributed to several factors, i.e. the optimal preparation of the proximal femur along with preservation of the femoral neck, the lateral flare of the femoral components, osseointegration in both younger and elderly patients, the improved quality of the ceramic-on-ceramic bearing capacity, no comorbidities (medically simple), and patients in both groups mobilized faster.
A potential concern with the use of cementless short metaphyseal-fitting anatomic femoral components, particularly in elderly patients, is the loss of stability of the component and failure of osseous ingrowth. Walker et al. [29] suggested that extending the femoral stem beyond the lesser trochanter is unnecessary for a cementless anatomic femoral component with a later flare, and that a short, metaphyseal-fitting is sufficient. Leali and Fetto [30] found that a proximally fixed cementless femoral component with a lateral flare provided solid initial stability. Santori et al. [18, 31, 32] reported solid fixation of their custom-made ultra-short metaphyseal-fitting stem (DePuy, Leeds, United Kingdom). Kim et al. [17, 28] also reported solid fixation of their cementless ultra-short, metaphyseal-fitting anatomic stem. These findings support the assumption that torsional loads can be controlled without disphyseal fixation by preservation of the femoral neck and lateral flare of the femoral component. In our study, the fixation was successful in both groups and stability of the femoral component had not deteriorated at mid-term follow-up. Thus the performance of the cementless ultra-short, metaphyseal-fitting anatomic femoral component in these consecutive series of young and elderly patients was comparable to that of other conventional cementless femoral components [7, 10, 27, 33–35].
Santori et al. [32] observed mild stress-shielding with a rounding off of the calcar region in seventy of 131 femora after using their custom-made ultra-short femoral component. Kim et al. [16, 28] also demonstrated that the bone content was preserved at the baseline level or above at final follow-up after using a cementless ultra-short, metapyseal-fitting anatomic femoral component. All hips in our series had mild stress shielding in the calcar region (calcar round off), as shown by radiographic and DEXA examinations at final follow-up. We believe that the absence of the distal stem avoiding contact between the distal stem and the femoral cortex minimized stress shielding-related femoral bone resorption.
The reported incidence of squeaking hips ranges from 1 % to 21 % [36–39]. The etiology of squeaking hips is still unclear. Several authors [36, 37, 39] have reported a variety of contributing factors to squeaking hips, e.g. taller, heavier and more active younger patients having a higher range of motion; high cup inclination; high femoral offset; lateralization of the hip center; and either high or low acetabular component anteversion. Contributing factors to the absence of squeaking hips in the present series may thus be shorter and lighter patients (despite they were young and active patients with high hip range of motion) and optimal cup position (between 40° and 45° inclination and between 20° and 30° anteversion). Alumina ceramic head or liner fracture is reported in the literature [40, 41]. In the present study, the absence of a ceramic head or liner fracture contrasts with the results of other studies on the use of modern designs with alumina-on-alumina ceramic bearings [1, 40–43]. The absence of a ceramic head or liner fracture in the present series is attributed to improved quality of ceramic material, optimal cup orientation, optimal interlocking of the alumina head and taper of the stem as well as alumina liner and metallic cup shell.
In conclusion, the cementless ultra-short, metaphyseal-fitting anatomic cementless femoral component provides stable fixation without any need of diaphyseal fixation in both younger and elderly patients. Despite the concern, the poor bone quality of bone in elderly patients did not compromise the stability, and osseointegration of this ultra-short, anatomic cementless femoral stem was achieved in all elderly patients.
Footnotes
The study was approved by the institutional review board, and all patients provided informed consent. All authors participated in the research for this paper. This manuscript has not been submitted elsewhere for publication.
References
- 1.Bizot P, Hannouche D, Nizard R, Witvoet J, Sedel L. Hybrid alumina total hip arthroplasty using a press-fit metal-backed socket in patients younger than 55 years. A six- to 11-year evaluation. J Bone Joint Surg Br. 2004;86(2):190–194. doi: 10.1302/0301-620X.86B2.14026. [DOI] [PubMed] [Google Scholar]
- 2.Christie J, Burnett R, Potts HR, Pell AC. Echocardiography of transatrial embolism during cemented and uncemented hemiarthroplasty of the hip. J Bone Joint Surg Br. 1994;76(3):409–412. [PubMed] [Google Scholar]
- 3.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 4.Engh CA, McGovern TF, Bobyn JD, Harris WH. A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. J Bone Joint Surg Am. 1992;74(7):1009–1020. [PubMed] [Google Scholar]
- 5.Keisu KS, Orozco F, Sharkey PF, Hozack WJ, Rothman RH, McGuigan FX. Primary cementless total hip arthroplasty in octogenarians. Two to eleven-year follow-up. J Bone Joint Surg Am. 2001;83(3):359–363. doi: 10.1302/0301-620X.83B3.11006. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y-H, Oh S-W, Kim J-S. Prevalence of fat embolism following bilateral simultaneous and unilateral total hip arthroplasty performed with or without cement: a prospective, randomized clinical study. J Bone Joint Surg Am. 2002;84(8):1372–1379. doi: 10.2106/00004623-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 7.McAuley JP, Moore KD, Culpepper WJ, 2nd, Engh CA. Total hip arthroplasty with porous-coated prostheses fixed without cement in patients who are sixty-five years of age or older. J Bone Joint Surg Am. 1998;80(11):1648–1655. doi: 10.2106/00004623-199811000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Orsini EC, Byrick RJ, Mullen JB, Kay JC, Waddell JP. Cardiopulmonary function and pulmonary microemboli during arthroplasty using cemented or non-cemented components. The role of intramedullary pressure. J Bone Joint Surg Am. 1987;69(6):822–832. [PubMed] [Google Scholar]
- 9.Patterson BM, Healey JH, Cornell CN, Sharrock NE. Cardiac arrest during hip arthroplasty with a cemented long-stem component. A report of seven cases. J Bone Joint Surg Am. 1991;73(2):271–277. [PubMed] [Google Scholar]
- 10.Pieringer H, Labek G, Auersperg V, Böhler N. Cementless total hip arthroplasty in patients older than 80 years of age. J Bone Joint Surg Br. 2003;85(5):641–645. [PubMed] [Google Scholar]
- 11.Hozack WJ, Rothman RH, Booth RE, Jr, Balderston RA, Cohn JC, Pickens GT. Survivorship analysis of 1,041 Charnley total hip arthroplasties. J Arthroplasty. 1990;5(1):41–47. doi: 10.1016/S0883-5403(06)80008-2. [DOI] [PubMed] [Google Scholar]
- 12.Sadoghi P, Janda W, Agreiter M, Rauf R, Leithner A, Labek G. Pooled outcome of total hip arthroplasty with the cementless spotorno(CLS)system: a comparative analysis of clinical studies and worldwide arthroplasty register data. Int Orthop. 2013;37(6):995–999. doi: 10.1007/s00264-013-1867-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markmiller M, Weiss T, Krew P, Rüter A, Konrad G. Partial weight bearing is not necessary after cementless total hip arthroplasty: a two-year prospective randomized study on 100 patients. Int Orthop. 2011;35(8):1139–1143. doi: 10.1007/s00264-010-1089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim Y-H, Choi Y, Kim J-S. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients young than 45 years with femoral-head osteonecrosis. Int Orthop. 2010;34(8):1123–1127. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kress AM, Schmidt R, Holzwarth U, Forst R, Mueller LA. Excellent results with cementless total hip arthropalsty and alumina-on-alumina pairing: minimum ten-year follow-up. Int Orthop. 2011;35(2):195–200. doi: 10.1007/s00264-010-1150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y-H, Choi Y-W, Kim J-S. Comparison of bone mineral density changes around short, metaphyseal-fitting and conventional cementless anatomical femoral components. J Arthroplasty. 2011;26:931–940. doi: 10.1016/j.arth.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty. 2012;27(1):88–94. doi: 10.1016/j.arth.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 18.Santori FS, Santori N. Mid-term results of a custom-made short proximal loading femoral component. J Bone Joint Surg Br. 2010;92(9):1231–1237. doi: 10.1302/0301-620X.92B9.24605. [DOI] [PubMed] [Google Scholar]
- 19.Braud P, Freeman MA (1990) The effect of retention of the femoral neck and of cement upon the stability of proximal femoral prosthesis. J Arthroplasty 5(Suppl):S5–10 [DOI] [PubMed]
- 20.Whiteside LA, White SE, McCarthy DS. Effect of neck resection on torsional stability of cementless total hip replacement. Am J Orthop. 1995;24(10):766–770. [PubMed] [Google Scholar]
- 21.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 22.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 23.Kim YH, Kim VE. Early migration of uncemented porous coated anatomic femoral component related to aseptic loosening. Clin Orthop Relat Res. 1993;295:146–155. [PubMed] [Google Scholar]
- 24.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 25.Dorr LD. Total hip replacement using APR system. Tech Orthop. 1986;1:22–34. doi: 10.1097/00013611-198610000-00007. [DOI] [Google Scholar]
- 26.Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995;77(3):432–439. doi: 10.2106/00004623-199503000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Dorr LD, Wan Z, Gruen T. Functional results in total hip replacement in patients 65 years and older. Clin Orthop Relat Res. 1997;336:143–151. doi: 10.1097/00003086-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Kim Y-H, Kim J-S, Park J-W, Joo J-H. Total hip replacement with a short metaphyseal-fitting anatomical cementless femoral component in patients aged 70 years or older. J Bone Joint Surg Br. 2011;93(5):587–592. doi: 10.1302/0301-620X.93B5.25994. [DOI] [PubMed] [Google Scholar]
- 29.Walker PS, Culligan SG, Hua J, Muirhead-Allwood SK, Bentley G. The effect of a lateral flare feature on implant stability. Hip Int. 1999;9:71–80. [Google Scholar]
- 30.Leali A, Fetto JF. Preservation of femoral bone mass after total hip replacements with a lateral flare stem. Int Orthop. 2004;28(3):151–154. doi: 10.1007/s00264-004-0554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Santori FS, Manili M, Fredella N, Tonci Ottieri M, Santori N. Ultra-short stems with proximal load transfer: clinical and radiographic results at five-year follow-up. Hip Int. 2006;16(Suppl 3):31–39. doi: 10.1177/112070000601603S06. [DOI] [PubMed] [Google Scholar]
- 32.Santori N, Albanese CV, Learmonth ID, Santori FS. Bone preservation with a conservative metaphyseal loading implant. Hip Int. 2006;16(Suppl 3):16–21. doi: 10.1177/112070000601603S04. [DOI] [PubMed] [Google Scholar]
- 33.Aldinger PR, Breusch SJ, Lukoschek M, Mau H, Ewerbeck V, Thomsen M. A Ten- to 15-year follow-up of the cementless Spotorno stem. J Bone Joint Surg Br. 2003;85(2):209–214. doi: 10.1302/0301-620X.85B2.13216. [DOI] [PubMed] [Google Scholar]
- 34.Kim Y-H, Kim VE. Uncemented porous-coated anatomic total hip replacement. Results at six years in a consecutive series. J Bone Joint Surg Br. 1993;75(1):6–13. doi: 10.1302/0301-620X.75B1.8421036. [DOI] [PubMed] [Google Scholar]
- 35.Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (Tri-Lock) inserted without cement. J Bone Joint Surg Am. 2002;84(12):2140–2144. doi: 10.2106/00004623-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91(6):1344–1349. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 37.Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466(6):1438–1443. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack WJ. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg. 2008;74(5):615–622. [PubMed] [Google Scholar]
- 39.Walter WL, Waters TS, Gillies M, Donohoo S, Kurtz SM, Ranawat AS, Hozack WJ, Tuke MA. Squeaking hips. J Bone Joint Surg Am. 2008;90(Suppl 4):102–111. doi: 10.2106/JBJS.H.00867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Callaway GH, Flynn W, Ranawat CS, Sculco TP. Fracture of the femoral head after ceramic-on-polyethylene total hip arthroplasty. J Arthroplasty. 1995;10(6):855–859. doi: 10.1016/S0883-5403(05)80087-7. [DOI] [PubMed] [Google Scholar]
- 41.Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90(2):329–336. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 42.Barrack RL, Burak C, Skinner HB. Concerns about ceramics in THA. Clin Orthop Relat Res. 2004;429:73–79. doi: 10.1097/01.blo.0000150132.11142.d2. [DOI] [PubMed] [Google Scholar]
- 43.Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty. A five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87(3):530–535. doi: 10.2106/JBJS.D.01753. [DOI] [PubMed] [Google Scholar]