Abstract
Purpose
Musculoskeletal tumours are rare in the daily practice of an orthopaedic surgeon or even a shoulder and elbow specialist. Patient complaints are often related to secondary changes to the underlying disease making the correct diagnosis challenging. The goal of this study is to identify key symptoms and findings which should give rise to suspicion of an osteoid osteoma.
Methods
This retrospective study analyses the diagnostic pathway, surgical treatment and clinical outcome of six patients who underwent resection of an osteoid osteoma of the shoulder or elbow joint.
Results
Average follow-up was 24 months (range 16–36 months). The neoplasm was often associated with synovitis mimicking a frozen joint causing marked delay in tumour identification. Misdiagnosis led to surgery without addressing the tumour in two cases, making further surgical intervention necessary. Once the tumour was identified and removed the pain resolved rapidly.
Conclusions
In cases of chronic shoulder or elbow pain without an adequate clinical history an underlying cause including rarities such as an osteoid osteoma or other musculoskeletal tumours should be taken into consideration. Particularly in young patients, a magnetic resonance imaging (MRI)-proven hot spot of unknown origin should prompt a computed tomography examination to further clarify the source of pain and stiffness.
Level of evidence
IV, case series
Keywords: Osteoid osteoma, Shoulder, Elbow, Minimally invasive surgery, Arthroscopy, Retrospective study, Benign tumour, Tumour surgery
Introduction
Osteoid osteoma is a benign bone forming tumour which predominantly affects the long bones and the spine [8]. Characteristically it causes pain due to production of prostaglandin E2 [9]. Pain at night is common and responds well to the intake of anti-inflammatory drugs or aspirin. According to its localisation, intra- and extra-articular as well as cortical, medullary or periosteal appearance can be differentiated [6]. Histologically the neoplastic tissue consists of a well vascularised nidus. The surrounding bone tends to reactive growth which might be detected on conventional radiographic or computed tomography (CT) images (Figs. 1 and 2). Clinically osteoid osteomas may mimic findings of a frozen shoulder or elbow joint due to the associated synovitis, making the correct diagnosis challenging [12]. This retrospective study focuses on the clinical presentation, the diagnostic pathway and the results of different treatment modalities of six patients suffering from osteoid osteoma of the shoulder or elbow joint. The purpose of this analysis is to identify key symptoms and findings which should give rise to suspicion of an osteoid osteoma.
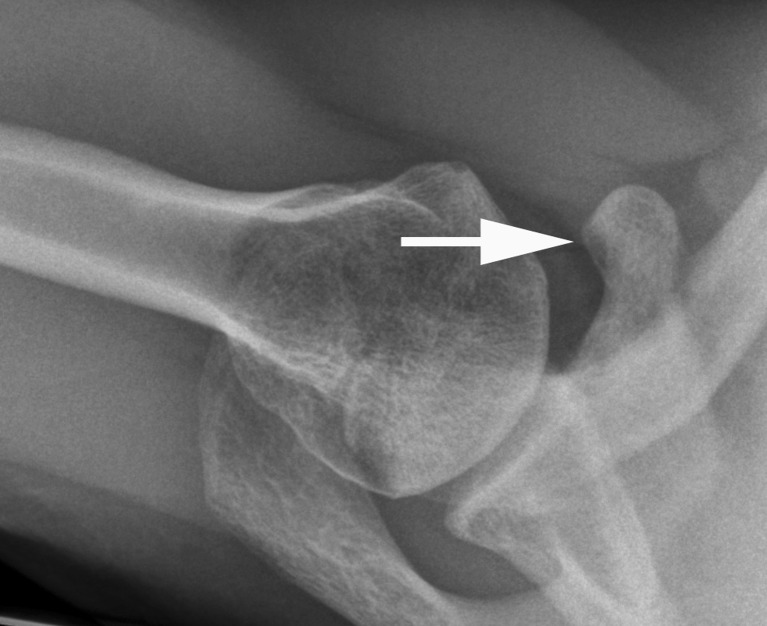
Fig. 1.
Axial radiograph of a right shoulder (case 1). With hindsight appositional bone formation can be suggested at the tip of the coracoid process. During more than 1 year the 20-year-old patient was treated for subacromial impingement syndrome with physical therapy and two corticosteroid injections without major benefit
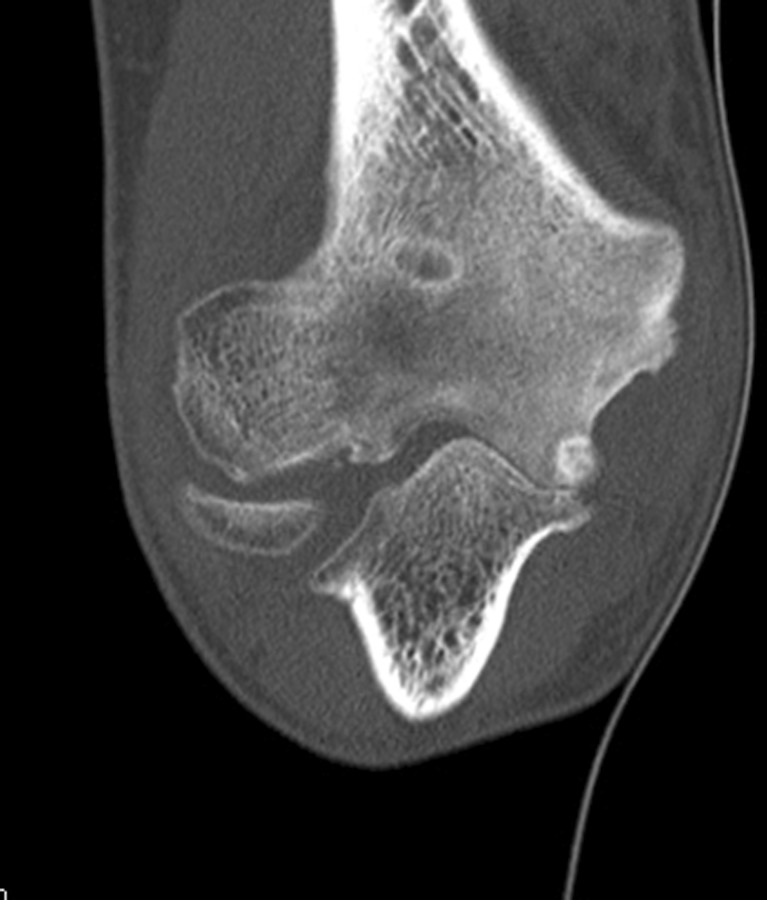
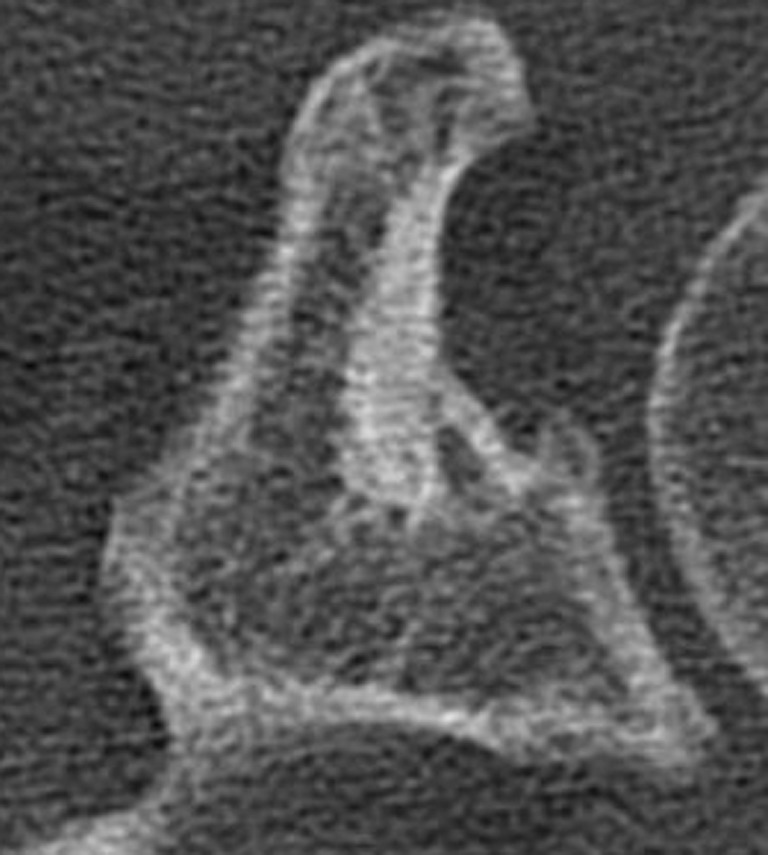
Fig. 2.
Sagittal CT scan showing reactive bone formation and sclerosis at the base of the coracoid. A feeding vessel can be assumed close to the inferior cortex
Materials and methods
This study presents a retrospective analysis of the records of six consecutive patients with an osteoid osteoma of either the shoulder or the elbow joint treated in two orthopaedic centres from 1998 through to 2011. Demographic data including age, gender, time of onset of symptoms and previous treatment, in particular surgical interventions, were recorded. Radiographic and CT as well as magnetic resonance imaging (MRI) studies were available in all cases. Every patient included had a minimum follow-up of 12 months after tumour removal. This study did not undergo an ethics review.
Results
A total of six patients with an osteoid osteoma were identified: two were localised in the coracoid process of the scapula and four tumours affected the elbow (Table 1). The mean duration between onset of the symptoms and the CT identification of an osteoid osteoma was 26 months (range six to 42 months). Four male and two female patients with an average age of 27.5 years (range 20–39 years) at the time of the index operation were affected. The dominant side was involved three times. All patients were otherwise in good health and previous discomfort of the affected joint was denied. The mean follow-up time was 24 months (16–36 months).
Table 1.
Clinical series and results
| Case | Agea (years) | Gender | Localisation | Affected joint | Diagnostic delay (months) | Type of treatment | Follow-up (months) | Range of motion |
|---|---|---|---|---|---|---|---|---|
| 1 | 22 | Male | Coracoid process | Right shoulder | 18 | CT-guided ablation | 25 | Unrestricted |
| 2 | 22 | Male | Coracoid process | Left shoulder | 42 | Arthroscopic removal and capsulotomy | 18 | Unrestricted |
| 3 | 34 | Female | Proximal ulna | Left elbow | 28 | Open resection with column procedure | 26 | 120-20-0 |
| 4 | 39 | Female | Proximal ulna | Right elbow | 25 | Open resection | 22 | Unrestricted |
| 5 | 20 | Male | Coronoid fossa | Right elbow | 42 | Arthroscopic removal | 36 | Unrestricted |
| 6 | 28 | Male | Humeral trochlea | Right elbow | 6 | CT-guided ablation | 16 | 140-35-0 |
| Median | 25 | 26.5 | 23.5 | |||||
| Average | 27.5 | 26.8 | 23.8 |
aAt time of surgery
Clinical course
Chronic pain was the chief complaint in all patients. Marked loss of active and passive range of motion was present in three cases: One individual had a stiff shoulder with complete loss of external rotation in the adducted position. This patient had undergone an unsuccessful arthroscopic capsulotomy elsewhere before referral to our department. In two patients the preoperative clinical examination demonstrated a distinct loss of elbow flexion and extension compared to the contralateral side. Pronation and supination were not affected. The characteristic pain-relieving effect of non-steroidal anti-inflammatory drugs or salicylates was recorded in two patients. The shoulder patients underwent multiple corticosteroid injections with only minor and time-limited effect.
Resection of the tumour was highly successful in terms of pain relief independent of the type of intervention (arthroscopic vs open vs CT-guided radiofrequency ablation). Up to final follow-up all patients were free of pain. Of the three patients with marked joint stiffness prior to tumour removal only one recovered full range of motion.
Imaging
In hindsight, conventional radiographs revealed signs of the underlying disease in three cases. Reactive bone formation and osteosclerosis were identifiable at the coracoid in both shoulder patients (Figs. 1 and 2). All radiographs of the elbow patients were normal except for one case with dystrophic calcification apparent on the conventional films (Figs. 3, 4 and 5). A constant finding in all patients was a marked bone marrow oedema on MRI scans (Fig. 6). The tumour-specific nidus was confirmed by CT scans in all cases (Fig. 7). The so-called feeding vessel, a distinctive finding in osteoid osteomas, was apparent in three cases on CT scans (Fig. 2).
Fig. 3.
Anteroposterior view of a right elbow (case 6) shows mild signs of joint space degeneration at the ulnar side. The construction labourer had undergone arthroscopic and open surgery prior to identification of the osteoid osteoma
Fig. 4.
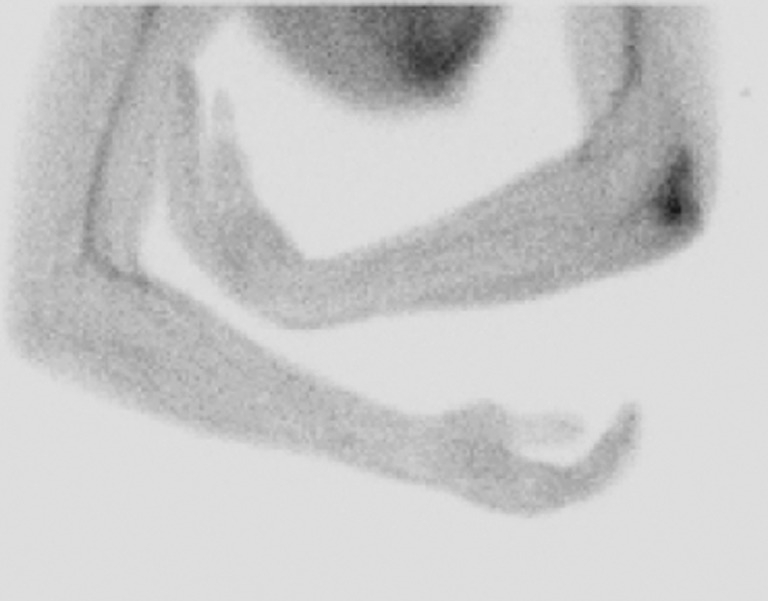
Early phase of the technetium (99mTc) bone scan showing a “hot spot” at the affected elbow
Fig. 5.
CT scan confirming the osteoid osteoma as underlying cause of ongoing elbow pain. Arthroscopic debridement and removal of a loose body and open arthrolysis were unsuccessful prior to the final diagnosis. Revision surgery did improve pain but the range of motion was not fully recovered
Fig. 6.
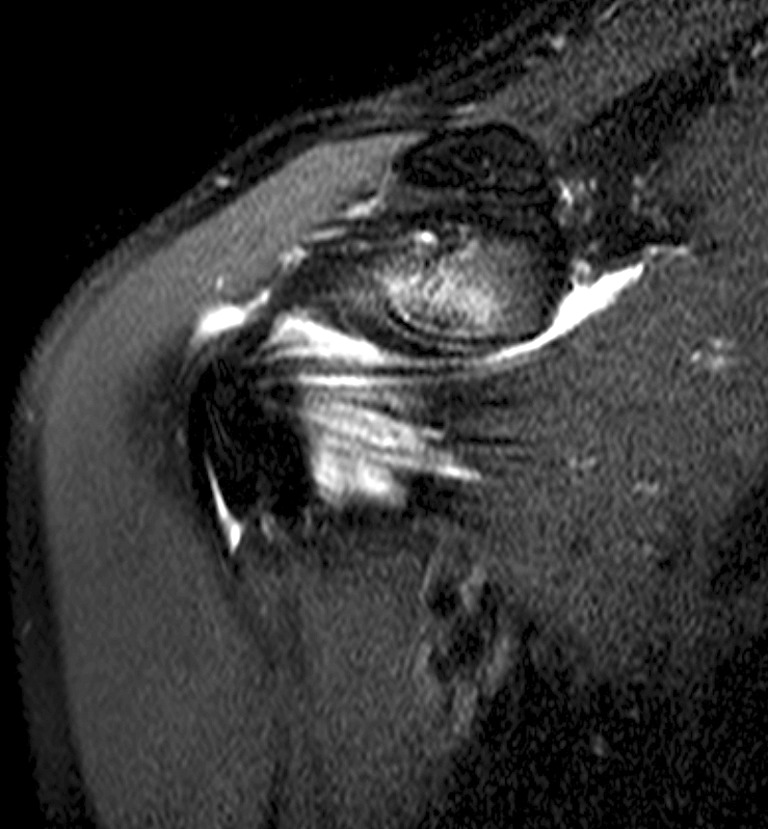
T2-weighted coronary MRI sequence of the same patient showing a marked bone marrow oedema in the coracoid process
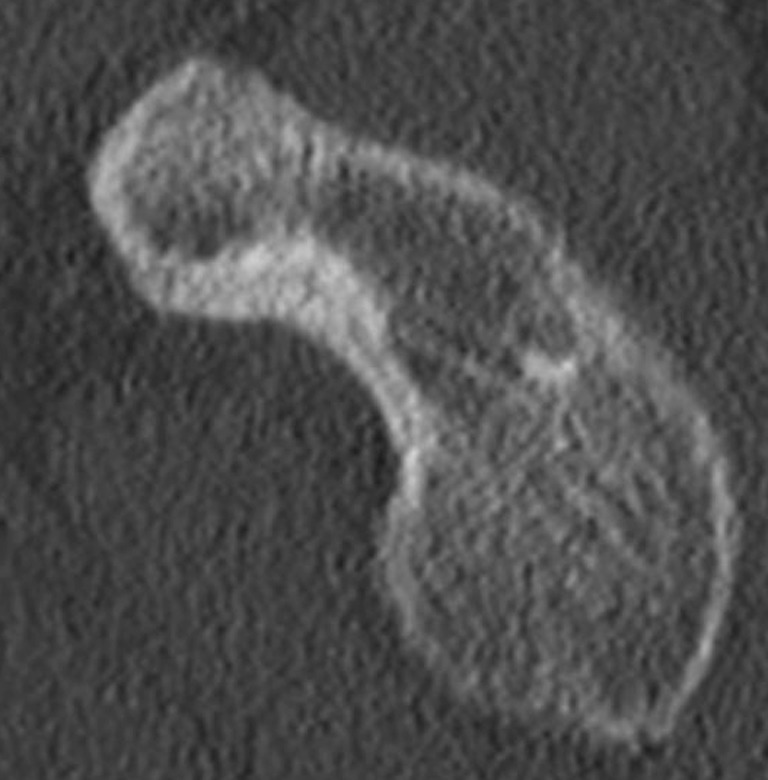
Fig. 7.

CT scan located the characteristic nidus of an osteoid osteoma. The neoplasm was removed by radiofrequency ablation due to its favourable location. The patient was pain-free and recovered a full range of motion within 1 month following the intervention
Surgical treatment
Until identification and treatment of the tumour, two patients had undergone unsuccessful operations for pain and stiffness. Once the neoplasm was detected, the osteoid osteoma was removed by CT-guided ablation in two patients (Figs. 8 and 9), by open resection in two cases and by arthroscopic resection in the remaining two cases (Figs. 10 and 11). In three patients a concomitant adhesive capsulitis was treated in the same intervention either open (two elbow joints) or arthroscopically (one shoulder joint). While the stiff shoulder regained full range of motion, both elbow patients underwent open revision for recalcitrant arthrofibrosis six and 30 months, respectively, after tumour removal. At final follow-up the range of motion of these two patients remained decreased compared to the contralateral side. A histological exam confirmed the diagnosis in all open and arthroscopically treated patients.
Fig. 8.
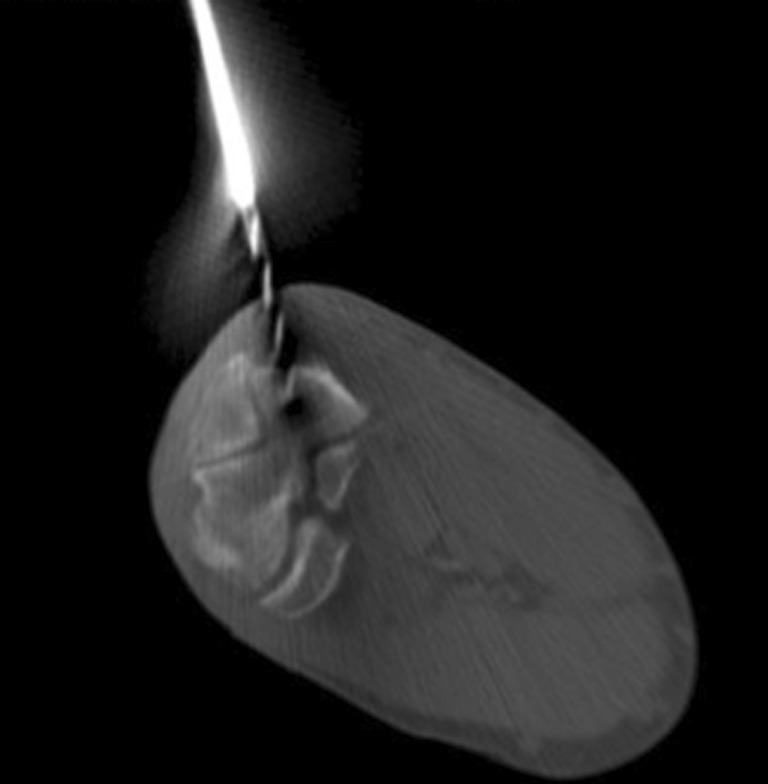
CT-guided minimally invasive resection of an osteoid osteoma of the distal humerus: as the first step of the intervention the tumour is resected by a cannulated drill followed by radiofrequency ablation of the affected area
Fig. 9.
Following overdrilling the tumour radiofrequency ablation is performed
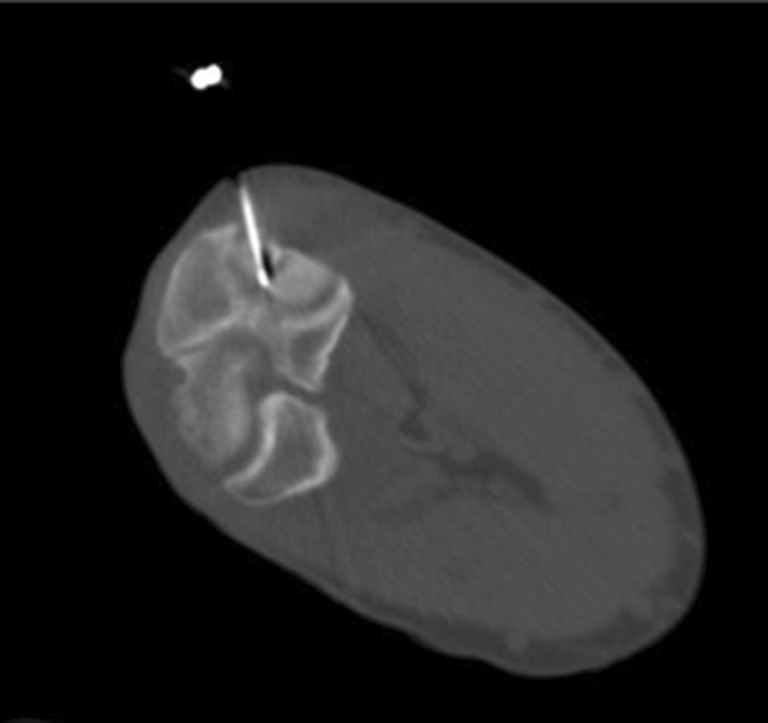
Fig. 10.
Axial CT scan of a left shoulder: the nidus of the osteoid osteoma lies superficial at the base of the coracoid favouring an arthroscopic approach for surgical removal of the tumour
Fig. 11.

Corresponding to the CT evidence (Fig. 6) the base of the coracoid is arthroscopically exposed and the tumour later removed by overdrilling with a cannulated 1.8-mm drill
Discussion
This study reports on the difficulty of identifying an osteoid osteoma as a cause of shoulder or elbow pain. A high level of suspicion is needed to detect the underlying cause of mimicking symptoms such as stiffness. In all six cases the pain was treated successfully and almost immediately through resection of the tumour.
Due to their rare appearance and unspecific symptoms musculoskeletal tumours in general and intra-articular osteoid osteomas of the shoulder and elbow joint are often diagnosed late. In a retrospective study by Sano et al. 26 % of a total of 34 patients with a malignant shoulder tumour were initially misdiagnosed with frozen shoulder syndrome [12]. In contrast, an analysis of 140 patients with primary or secondary frozen shoulder revealed an incidence of 2.1 % of tumours as the cause of the limited range of motion [5]. While primary frozen shoulder most commonly affects women in their fifth and sixth decade it is often correlated with certain co-morbidities such as diabetes. Demographically, musculoskeletal tumours of the upper extremity are more common in younger patients [4]. Bone tumours of the shoulder girdle are most frequently found in the proximal humerus followed by the scapula and the clavicle [3]. According to a study on bone tumours of the coracoid process, Ogose et al. found ten chondrosarcomas among a total of 18 patients. In two cases an osteoid osteoma was identified [11]. In a review of the literature on osteoid osteomas of the elbow 17 of 33 cases were localised in the olecranon fossa and five in the olecranon itself [1].
Concomitant synovitis causing joint stiffness is reported in a multitude of case reports of patients with an osteoid osteoma. In a study by Bednar et al. the average delay from the first medical examination to the correct diagnosis was two years [2]. In our study the average duration between the initial doctor’s visit and the confirmation of the diagnosis was 27 months. Detection of the underlying neoplastic lesion is difficult since radiological abnormalities are often absent or minimal and need a high level of suspicion in order to be detected. In a series of 48 patients Themistocleous et al. reported conventional radiographs of 32 cases as sufficient to establish the diagnosis [14]. In our cohort reactive bone formation and dystrophic calcification were present in only two patients. In hindsight secondary sclerosis at the base of the coracoid was present in two cases. As a clinical examination of skeletal neoplasms Neviaser proposed gentle tapping of bony areas in order to elicit pain which should be differentiated from symptoms provoked by firm palpation as found in rotator cuff disease [10]. A constant finding in this series was a marked bone marrow oedema on MRI scans corresponding to the highly vascularised mesenchymal tissue [13]. An otherwise unexplained bone marrow oedema can be interpreted as a red flag and should prompt further examination by CT imaging or bone scan. Furthermore, the combination of these two methods is available in current practice as single photon emission computed tomography (SPECT)/CT.
Removal of the tumour can be done surgically by open or arthroscopic resection, but also CT-guided percutaneous techniques have proven to be successful [7]. In this series the surgical approach was adapted to the localisation of the tumour and the degree of secondary stiffness (Figs. 5 and 7a, b).
Conclusions
In cases of chronic shoulder or elbow pain without an adequate clinical history an underlying cause including rarities such as an osteoid osteoma or other musculoskeletal tumours must be taken into consideration. Clinically pain elicited by gentle tapping over bony areas can be seen as a red flag. MRI-proven hot spots should prompt a CT examination to identify the pathognomonic nidus. Treatment modalities depend on localisation of the tumour and the potentially co-existing capsulitis. Pre-existing severe joint stiffness limits the success of surgical treatment.
Acknowledgments
The authors thank Laura Iskandar for her valuable assistance as a native English speaker.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Becker PL, Heywood HB 3rd, Crosby LA (2000) Osteoid osteoma of the coronoid process: case report and review of the literature. J Shoulder Elbow Surg 9(5):446–448. doi:10.1067/mse.2000.106919 [DOI] [PubMed]
- 2.Bednar MS, Weiland AJ, Light TR. Osteoid osteoma of the upper extremity. Hand Clin. 1995;11(2):211–221. [PubMed] [Google Scholar]
- 3.Cleeman E, Auerbach JD, Springfield DS (2005) Tumors of the shoulder girdle: a review of 194 cases. J Shoulder Elbow Surg 14(5):460–465. doi:10.1016/j.jse.2005.02.003 [DOI] [PubMed]
- 4.Craig EV, Thompson RC. Management of tumors of the shoulder girdle. Clin Orthop Relat Res. 1987;223:94–112. [PubMed] [Google Scholar]
- 5.Demazière A, Wiley AM. Primary chest wall tumor appearing as frozen shoulder. Review and case presentations. J Rheumatol. 1991;18(6):911–914. [PubMed] [Google Scholar]
- 6.Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. (Roentgenographic emphasis) Clin Orthop Relat Res. 1966;49:201–206. doi: 10.1097/00003086-196611000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Gangi A, Dietemann JL, Gasser B, Mortazavi R, Brunner P, Mourou MY, Dosch JC, Durckel J, Marescaux J, Roy C. Interstitial laser photocoagulation of osteoid osteomas with use of CT guidance. Radiology. 1997;203(3):843–848. doi: 10.1148/radiology.203.3.9169714. [DOI] [PubMed] [Google Scholar]
- 8.Letson GD, McEwen GD, Choy JY. A technique for excision of an osteoid osteoma. Orthopedics. 1997;20(3):266–268. doi: 10.3928/0147-7447-19970301-13. [DOI] [PubMed] [Google Scholar]
- 9.Mungo DV, Zhang X, O’Keefe RJ, Rosier RN, Puzas JE, Schwarz EM. COX-1 and COX-2 expression in osteoid osteomas. J Orthop Res. 2002;20(1):159–162. doi: 10.1016/S0736-0266(01)00065-1. [DOI] [PubMed] [Google Scholar]
- 10.Neviaser TJ. Adhesive capsulitis. Orthop Clin North Am. 1987;18(3):439–443. [PubMed] [Google Scholar]
- 11.Ogose A, Sim FH, O’Connor MI, Unni KK. Bone tumors of the coracoid process of the scapula. Clin Orthop Relat Res. 1999;358:205–214. doi: 10.1097/00003086-199901000-00025. [DOI] [PubMed] [Google Scholar]
- 12.Sano H, Hatori M, Mineta M, Hosaka M, Itoi E (2010) Tumors masked as frozen shoulders: a retrospective analysis. J Shoulder Elbow Surg 19(2):262–266. doi:10.1016/j.jse.2009.05.010 [DOI] [PubMed]
- 13.Spouge AR, Thain LM. Osteoid osteoma: MR imaging revisited. Clin Imaging. 2000;24(1):19–27. doi: 10.1016/S0899-7071(00)00157-1. [DOI] [PubMed] [Google Scholar]
- 14.Themistocleous GS, Chloros GD, Benetos IS, Efstathopoulos DG, Gerostathopoulos NE, Soucacos PN. Osteoid osteoma of the upper extremity. A diagnostic challenge. Chir Main. 2006;25(2):69–76. doi: 10.1016/j.main.2006.02.001. [DOI] [PubMed] [Google Scholar]