Abstract
Purpose
The purpose of this study was to assess the MRI features of the all-inside repaired meniscus in the long-term.
Methods
Among 27 consecutive all-inside arthroscopic meniscal repairs, 23 patients aged 25 ± 5 years at the time of surgery were reviewed at a median follow-up of 10 ± 1 years. Retrospective clinical examinations and imaging assessments using a 1.5-T MRI after all-inside arthroscopic meniscal repair were conducted.
Results
At follow-up, Lysholm and IKDC averaged 89 ± 11 and 95 ± 8, respectively. MRI examinations revealed no meniscal signal alteration in three patients (13 %), a vertical signal located in the previously torn area in seven (30 %), a horizontal grade 3 in nine (39 %), and a complex tear (grade 4) in four (17.5 %). There were no differences between medial and lateral menisci (p = 0.15), stable and stabilised knees (p = 0.56).
Conclusions
Several abnormal vertical and/or horizontal hypersignals are still present on MRI examination ten years after arthroscopic all-inside meniscal repair. The appearance of early signs of osteoarthritis is rare, suggesting a chondroprotective effect of the repaired meniscus.
Keywords: Meniscus, Meniscus repair, Arthroscopic meniscus repair, All inside meniscus repairs, MRI examinations, Meniscus tears
Introduction
Arthroscopic repair of meniscal tears is commonly performed whenever possible. Short- and long-term results are good when compared to a subtotal meniscectomy [1–3]. Therefore, meniscal repair has become the treatment of choice for traumatic meniscal lesions located in the vascularised area [4, 5].
Arthroscopically-assisted meniscal repair has been described using a variety of techniques, including inside-out [6], outside-in [7], and all-inside repairs [8].
While pre-operative imaging of the meniscus has received ample consideration in the literature, data on postoperative imaging are less abundant.
Conventional MRI is an accurate method for diagnosing meniscal derangements but it is less reliable in the postoperative assessment of meniscal repairs in the short to mid-term [9, 10], particularly as a scar in a properly healed meniscus can mimic the signal seen in meniscal tears [11, 12]. Hoffelner and al. concluded at four years of follow-up that even a 3-Tesla MRI was not suitable to distinguish scar from meniscus healing after arthroscopic meniscal repair. This signal alteration may still persist in the long-term [10]. However, the literature has rarely focused on long-term imaging assessment of a repaired meniscus, except by single radiographs.
The purpose of this study was to analyse MRI signals within the repaired site ten years after arthroscopic all-inside meniscal repair. Our hypothesis was that a persisting hypersignal was still present at that time.
Materials and methods
Between November 2000 and November 2002, 50 arthroscopic meniscal repairs were performed using all-inside devices by one experienced surgeon. In this retrospective study, patients were asked to come in for follow-up in 2012 in order to have an MRI of the knee that was operated on.
A complete follow-up visit after ten years, which included clinical and MRI assessment, was available for 27 patients who returned completed Lysholm and IKDC (International Knee Documentation Committee) forms to determine their current function and any symptoms or interventions of which we were unaware.
There were 20 men and seven women, comprising 17 right and ten left knees that had been operated upon. The mean patient age at surgery was 25 years (range, ten to 36).
The presence of a repairable meniscal lesion was confirmed by arthroscopy. Meniscal lesions located in the red-red zone and unstable to probing were all judged suitable for repair. All were vertical and longitudinal. Operative data are listed in Table 1.
Table 1.
Operative data
| Medial/lateral meniscus | 19/8 | |
|---|---|---|
| Stable knee/reconstructed ACL | 9/18 | |
| Location of the tears | Medial meniscus | Posterior: 8 |
| Middle, posterior: 9 | ||
| Anterior, middle, posterior: 2 | ||
| Lateral meniscus | Posterior: 3 | |
| Anterior, middle: 2 | ||
| Anterior, middle, posterior: 3 | ||
Nineteen patients underwent repair of the medial meniscus, and eight lateral repairs were performed using Fastfix® devices (Smith & Nephew, Andover, MA). The median length of the meniscal tear evaluated during arthroscopy with a probe was 20 ± 14 mm. The median number of all-inside devices used for repair was 2 ± 1. There was no significant chondral damage seen at the time of arthroscopy.
MRI was performed with a 1.5-T MR system, using a dedicated send–receive extremity coil. Five diagnostic serials were examined, including sagittal T1-weighted spin echo, sagittal proton density fast spin echo, sagittal T2-weighted fast spin echo, coronal proton density fast spin echo with fat saturation, and coronal T2-weighted fast spin echo with fat saturation. Sagittal scans were placed vertical to the line connecting the posterior medial and lateral femoral condyles, while the coronal scans were parallel. Slice thickness was set at 2 mm.
Signal intensity, extrusion, and tears of the repaired meniscus were identified. Extrusion of the meniscus body was evaluated on the coronal sections as none (0), partial (less than 3 mm, type 1), or complete (more than 3 mm, type 2) [13]. If a tear was identified, the location (red, red on white, white zone) was recorded. The presence of subchondral oedema around the repaired site on the tibial or femoral side was also recorded.
The MRI signal grade at the repaired site was assessed using the criteria outlined by Raunest et al. [14]: grade 0 was defined as a normal meniscus; grade 1 was defined as an irregular intrameniscal signal; horizontal grade 2 was defined as a linear signal that did not communicate with an articular surface; horizontal grade 3 was defined as a linear horizontal signal intensity that communicated with an articular surface. The presence of both horizontal grade 3 and vertical signals was defined as "a complex tear" (grade 4). Cartilage degeneration of the femoral condyle and tibial plateau of the involved compartment was graded separately, as described by Yulish [15], such that, grade 1 was a normal contour, abnormal signal; grade 2 a superficial fraying, erosion or ulceration of less than 50 %; grade 3 a partial-thickness defect of more than 50 % but less than 100 %; and grade 4 a full-thickness cartilage loss.
MRI images were interpreted by a musculoskeletal radiologist and an experienced orthopaedic surgeon who had no previous knowledge of the clinical result.
Statistical analysis was performed using SPSS 13.0 software (SPSS Inc, Chicago, Illinois). The chi-square test was used. A p-value less than 0.05 was regarded as statistically significant.
Results
Four patients were excluded from the study due to failures requiring a secondary meniscectomy (four medial menisci repaired at the time of ACL reconstruction) at a mean of 30 months after the procedure).
At a median follow-up of 10 ± 1 years, the mean subjective IKDC and Lysholm scores of the 23 remaining patients were 89 ± 11 and 95 ± 8, respectively.
The MRI features of the repaired menisci are summarised in Table 2. MRI of the postoperative repaired menisci showed hypersignals within the suture site in 20 patients (87 %). Among these abnormal signals, nine were horizontal cleavages (grade 3 extending to at least one surface, Fig. 1), seven were vertical longitudinal (Fig. 2), and four were complex with both vertical and horizontal hypersignals. Three patients showed no signal alteration (three lateral menisci) of the repaired meniscus (Fig. 3). All the horizontal signals were not present pre-operatively on MRI so they are new. There were no differences between medial and lateral menisci (p = 0.15), or between stable and stabilised knees (p = 0.56). The signal alteration was always of intermediate intensity and could not allow differentiation between scar or new meniscal tear. There were no correlations between tear size and MRI appearance after ten years (p = 0.23). A slight joint effusion of the knee was detected in the MRI of ten patients. Two of the repaired menisci presented a complete extrusion (type 2, more than 3 mm) from the tibial plateau. The repaired meniscus appeared shortened in 11 cases (48 %). One patient had a subchondral edema in the medial femoral condyle, without any clinical complaint. There were no subchondral edemas on the tibial side. Two patients had grade 2 chondral degeneration of the femoral condyle, four patients had grade 3, and two patients had grade 4. Chondral degeneration signs were absent in 15 patients (65 % of cases).
Table 2.
Summary of the MRI features of the meniscus ten years after repair
| Meniscus | No hypersignal | Hypersignal | Bone marrow oedema | Extrusion | ||
|---|---|---|---|---|---|---|
| Horizontal | Vertical | Complex | ||||
| Lateral meniscus, n = 8 | 3 (37.5 %) | 4 (50 %) | 1 (12.5 %) | 0 | 0 | 0 |
| Medial meniscus, n = 15 | 0 | 5 (33 %) | 6 (40 %) | 4 (27 %) | 1 (femoral side) | 2 |
| Total, N = 23 | 3 (13 %) | 9 (39 %) | 7 (30 %) | 4 (17.5 %) | 1 (4.3 %) | 2 (8.7 %) |
Fig. 1.
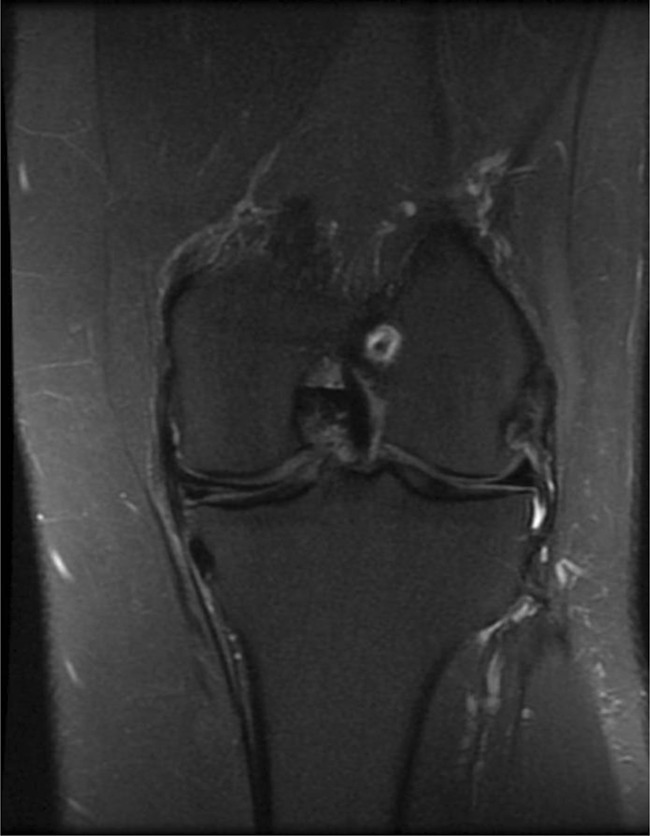
Horizontal cleavage on the repaired site of the meniscus at 10.5 years, medial meniscus, right knee
Fig. 2.

Persisting vertical hypersignal on the repaired suture site 10 years after repair, medial meniscus, right knee
Fig. 3.

Healed posterior segment, lateral meniscus, sutures still visible, no chondral lesions
The mean subjective IKDC and Lysholm scores of the patients with no abnormal signal on MRI were 94.7 ± 8 and 99 ± 1, respectively. The mean subjective IKDC and Lysholm scores of the patients with vertical abnormal signals on MRI were 99 ± 12 and 100 ± 8, respectively. The mean subjective IKDC and Lysholm scores of the patients with horizontal grade 3 abnormal signals on MRI were 83.9 ± 13 and 99 ± 10, respectively. The mean subjective IKDC and Lysholm scores of the patients with complex tears (grade 4) signals on MRI were 97 ± 5 and 99.5 ± 4, respectively.
Clinical follow-up assessment was not able to differentiate between horizontal signal, vertical signal, complex signals or the absence of signal alteration in the repaired meniscus area (p = 0.25). There was no correlation between chondral degeneration seen on MRI and clinical outcome (p = 0.12). Three complications were diagnosed at the time of the MRI: two asymptomatic cysts around Fastfix® devices, and one meniscal cyst on a repaired meniscus that presented at follow-up a horizontal grade 3 cleavage.
The mean subjective IKDC and Lysholm scores of the four failed patients with a subsequent meniscectomy were 87 ± 11 and 90.3 ± 3, respectively. Clinical outcomes were statistically different between these patients and the 23 patients with repaired meniscus still present in the joint (p = 0.04).
Discussion
The most important finding of this study is that there are persisting vertical hypersignals on the repaired site of the meniscus that are visible with MRI investigations at long-term follow-up. Moreover, many horizontal signals were also present. The appearance was similar to degenerative meniscal changes occurring in patients over 50 [16].
Meniscal repair and MRI
Many studies have confirmed the limitation of conventional MRI in evaluating the healing status of the meniscus after repair, in the short-term [9, 11, 13, 17, 18]. However, the diagnostic accuracy of conventional MRI is low, because both the initial fibrovascular and the later mature fibrocartilagenous scar produced persistent increased signal intensity on MR images after six months. Hantes et al. [19] assessed the healing process of the meniscal repair by indirect MRI at three, six, and 12 months after the operation. A postoperative hypersignal was found in each of the 20 patients involved in this study at three months. A significant reduction (but not disappearance) of this hypersignal occurred from three to 12 months, which suggested that the meniscal healing process lasted for at least 12 months. Miao et al. [12] evaluated the MRI signal characteristics and MRI diagnostic accuracy in identifying completely healed repaired menisci. A second look arthroscopy confirmed complete healing. A T2 hypersignal was found in 63 % of the 38 cases at a mean follow-up of 16 months. MRI diagnostic accuracy correlated positively with the follow-up time. Farley et al. [20] compared arthrography and MRI in the assessment of the meniscal healing after repair. T2 fat-saturated MRI sequences had a sensitivity of 60 % and a specificity of 90 % for meniscal healing. Arthrography had both sensitivity and specificity of 90 %. Further comparative studies are needed to assess the accuracy of arthro-MRI in the management of the repaired meniscus [18], but the accuracy may be comparable to arthro-CT imaging [21].
Muellner et al. [22] performed MRI among 19 patients 12.9 years after open meniscal repair. In ten patients, grade 3 signal alterations were observed on the side of the meniscal repair. In five patients, grade 2 signals were recorded, and in four patients no signal alterations were observed. Eggli [23] et al. performed 25 MRI scans at an average follow-up of 7.5 years after meniscal repair on stable knees with an outside-in technique. They found a persisting grade 3 or 4 lesion in 96 % of the successfully repaired menisci. Steenbrugge et al. [24] reported an hyperintense area within the site of the meniscal repair in 46 % of the patients, with MRI performed 13 years after meniscal repair using an inside-out technique. They suggested that these hypersignals corresponded to mucoid degeneration or scar tissue.
Although the surgical technique was different between series, this is consistent with our results. MRI is not suitable for sensing meniscal healing after repair, even at long-term follow-up. Such abnormal signals may reflect either immature fibrovascular granulation tissue or mature fibrocartilaginous scar tissue at the repair site.
Concerning horizontal hypersignals, these would not correspond to a persisting lesion (the initial lesions were all vertical), but rather a new one, like a degenerative change of the repaired meniscus with time.
Correlation between symptoms and MRI
A cohort study of 100 patients referred for suspected degenerative meniscal tear assessed the prevalence of meniscal abnormalities on MRI performed on symptomatic and contralateral asymptomatic knees [16]. Meniscal tears were found in 57 symptomatic and 36 asymptomatic knees. Horizontal medial meniscal tears were found in 32 symptomatic knees and 29 asymptomatic knees. In this study, bone marrow oedema and pericapsular soft tissue abnormality had the highest prevalence in symptomatic knees. Radial, complex displaced meniscal tears were mostly symptomatic. In our study, we found no correlation between MRI signals within the repaired site of the meniscus and clinical outcomes. Most of the knees were asymptomatic. We believe that, in patients without symptoms, the meniscus is either histologically healed or acts as an autograft and fulfils the mechanical tasks of a "nearly normal" meniscus.
Meniscal extrusion
Meniscal extrusion is defined as a significant (>3 mm) medial displacement of the medial meniscus with respect to the central margin of the medial tibial plateau. There is a significant association between the presence of pathologic meniscal extrusion and moderate to large osteophytes or cartilage loss [25–27]. Meniscal extrusion may be related to a loss of meniscal function, and may be one of the first signs of OA, due to a loss of meniscal function, appearing before cartilage thinning.
In our study, the small number of patients with a meniscal extrusion correlated with the low rate of degenerative cartilage changes. This corroborates the suggestion that the mechanical function of a repaired meniscus is still present in the long-term.
Bone marrow oedema
A cross-sectional study was performed on 410 patients (mean age 67 years) with radiographic evidence of knee osteoarthritis, either associated with pain or not [28]. On MRI, bone marrow lesions were found in 272 of the 351 painful knees compared to 15 of the 50 asymptomatic knees (p < 0.001). Large lesions were present almost exclusively in patients with knee pain. Although bone marrow oedema may be one of the first signs of osteoarthritis, it was absent in all except one of our cases.
The limitations of this study include the retrospective study design, the small number of patients reviewed, and the use of 1.5-T MRI. But, to our knowledge, this is the first study reporting long-term MRI results of the all-inside meniscal repair technique.
Imaging with a 3-Tesla MRI after meniscal suture surgery provided good but no definitive reliability regarding the assessment of meniscus healing and, therefore, gives no definite advantage compared to 1.5-T MRI [10]. Moreover, it would be much more valuable to compare the appearance of the non-operated knee on MRI in order to determine if the described changes were just natural aging progression rather than due to meniscus surgery.
Conclusion
Several abnormal vertical and/or horizontal hypersignals are present on MRI ten years after arthroscopic all-inside meniscal repair, without any subjective or objective clinical significance. Progression of cartilage degeneration according to MRI criteria was low, indicating a potential chondroprotective effect of these repaired menisci with abnormal signals.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.McGinty JB. The importance of the meniscus. Am J Knee Surg. 1996;9:109. [PubMed] [Google Scholar]
- 2.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 3.Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 4.Beaufils P, Hulet C, Dhenain M, Nizard R, Nourissat G, Pujol N. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437–442. doi: 10.1016/j.otsr.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22:347–357. doi: 10.1055/s-0030-1247773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosso C, Kovtun K, Dow W, McKenzie B, Nazarian A, DeAngelis JP, et al. Comparison of all-inside meniscal repair devices with matched inside-out suture repair. Am J Sports Med. 2011;39:2634–2639. doi: 10.1177/0363546511424723. [DOI] [PubMed] [Google Scholar]
- 7.Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206. [PubMed] [Google Scholar]
- 8.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40:459–468. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 9.Vance K, Meredick R, Schweitzer ME, Lubowitz JH. Magnetic resonance imaging of the postoperative meniscus. Arthroscopy. 2009;25:522–530. doi: 10.1016/j.arthro.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Hoffelner T, Resch H, Forstner R, Michael M, Minnich B, Tauber M. Arthroscopic all-inside meniscal repair—Does the meniscus heal? A clinical and radiological follow-up examination to verify meniscal healing using a 3-T MRI. Skeletal Radiol. 2011;40:181–187. doi: 10.1007/s00256-010-0965-6. [DOI] [PubMed] [Google Scholar]
- 11.Arnoczky SP, Cooper TG, Stadelmaier DM, Hannafin JA. Magnetic resonance signals in healing menisci: an experimental study in dogs. Arthroscopy. 1994;10:552–557. doi: 10.1016/S0749-8063(05)80013-1. [DOI] [PubMed] [Google Scholar]
- 12.Miao Y, Yu JK, Zheng ZZ, Yu CL, Ao YF, Gong X, et al. MRI signal changes in completely healed meniscus confirmed by second-look arthroscopy after meniscal repair with bioabsorbable arrows. Knee Surg Sports Traumatol Arthrosc. 2009;17:622–630. doi: 10.1007/s00167-009-0728-x. [DOI] [PubMed] [Google Scholar]
- 13.Breitenseher MJ, Trattnig S, Dobrocky I, Kukla C, Nehrer S, Steiner E, et al. MR imaging of meniscal subluxation in the knee. Acta Radiol. 1997;38:876–879. doi: 10.1080/02841859709172428. [DOI] [PubMed] [Google Scholar]
- 14.Raunest J, Hotzinger H, Burrig KF. Magnetic resonance imaging (MRI) and arthroscopy in the detection of meniscal degenerations: correlation of arthroscopy and MRI with histology findings. Arthroscopy. 1994;10:634–640. doi: 10.1016/S0749-8063(05)80061-1. [DOI] [PubMed] [Google Scholar]
- 15.Yulish BS, Montanez J, Goodfellow DB, Bryan PJ, Mulopulos GP, Modic MT. Chondromalacia patellae: assessment with MR imaging. Radiology. 1987;164:763–766. doi: 10.1148/radiology.164.3.3615877. [DOI] [PubMed] [Google Scholar]
- 16.Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B, Hodler J. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol. 2003;181:635–641. doi: 10.2214/ajr.181.3.1810635. [DOI] [PubMed] [Google Scholar]
- 17.Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011;39:735–742. doi: 10.1177/0363546510388930. [DOI] [PubMed] [Google Scholar]
- 18.Vives MJ, Homesley D, Ciccotti MG, Schweitzer ME. Evaluation of recurring meniscal tears with gadolinium-enhanced magnetic resonance imaging: a randomized, prospective study. Am J Sports Med. 2003;31:868–873. doi: 10.1177/03635465030310062301. [DOI] [PubMed] [Google Scholar]
- 19.Hantes ME, Zachos VC, Zibis AH, Papanagiotou P, Karachalios T, Malizos KN, et al. Evaluation of meniscal repair with serial magnetic resonance imaging: a comparative study between conventional MRI and indirect MR arthrography. Eur J Radiol. 2004;50:231–237. doi: 10.1016/j.ejrad.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Farley TE, Howell SM, Love KF, Wolfe RD, Neumann CH. Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology. 1991;180:517–522. doi: 10.1148/radiology.180.2.2068321. [DOI] [PubMed] [Google Scholar]
- 21.Pujol N, Panarella L, Selmi TA, Neyret P, Fithian D, Beaufils P. Meniscal healing after meniscal repair: a CT arthrography assessment. Am J Sports Med. 2008;36:1489–1495. doi: 10.1177/0363546508316771. [DOI] [PubMed] [Google Scholar]
- 22.Muellner T, Egkher A, Nikolic A, Funovics M, Metz V. Open meniscal repair: clinical and magnetic resonance imaging findings after twelve years. Am J Sports Med. 1999;27:16–20. doi: 10.1177/03635465990270011001. [DOI] [PubMed] [Google Scholar]
- 23.Eggli S, Wegmuller H, Kosina J, Huckell C, Jakob RP. Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. Am J Sports Med. 1995;23:715–720. doi: 10.1177/036354659502300614. [DOI] [PubMed] [Google Scholar]
- 24.Steenbrugge F, Verdonk R, Verstraete K. Long-term assessment of arthroscopic meniscus repair: a 13-year follow-up study. Knee. 2002;9:181–187. doi: 10.1016/S0968-0160(02)00017-0. [DOI] [PubMed] [Google Scholar]
- 25.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 26.Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthr Cartil. 1999;7:526–532. doi: 10.1053/joca.1999.0256. [DOI] [PubMed] [Google Scholar]
- 27.Kenny C (1997) Radial displacement of the medial meniscus and Fairbank’s signs. Clin Orthop Relat Res 339:163–173 [DOI] [PubMed]
- 28.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–549. doi: 10.7326/0003-4819-134-7-200104030-00007. [DOI] [PubMed] [Google Scholar]


