Abstract
Background
Inorganic arsenic, a carcinogen at high exposure levels, is a major global health problem. Prospective studies on carcinogenic effects at low-moderate arsenic levels are lacking.
Methods
We evaluated the association between baseline arsenic exposure and cancer mortality in 3,932 American Indians 45–74 years from Arizona, Oklahoma and North/South Dakota who participated in the Strong Heart Study in 1989–1991 and were followed through 2008. We estimated inorganic arsenic exposure as the sum of inorganic and methylated species in urine. Cancer deaths (386 overall, 78 lung, 34 liver, 18 prostate, 26 kidney, 24 esophagus/stomach, 25 pancreas, 32 colon/rectal, 26 breast, 40 lymphatic/hematopoietic) were assessed by mortality surveillance reviews. We hypothesized an association with lung, liver, prostate and kidney cancer.
Results
Median (interquartile range) urine concentration for inorganic plus methylated arsenic species was 9.7 (5.8–15.6) μg/g creatinine. The adjusted hazard ratios (95% CI) comparing the 80th versus 20th percentiles of arsenic were 1.14 (0.92–1.41) for overall cancer, 1.56 (1.02–2.39) for lung cancer, 1.34 (0.66, 2.72) for liver cancer, 3.30 (1.28–8.48) for prostate cancer, and 0.44 (0.14, 1.14) for kidney cancer. The corresponding hazard ratios were 2.46 (1.09–5.58) for pancreatic cancer, and 0.46 (0.22–0.96) for lymphatic and hematopoietic cancers. Arsenic was not associated with cancers of the esophagus and stomach, colon and rectum, and breast.
Conclusions
Low to moderate exposure to inorganic arsenic was prospectively associated with increased mortality for cancers of the lung, prostate and pancreas.
Impact
These findings support the role of low-moderate arsenic exposure in lung, prostate and pancreas cancer development and can inform arsenic risk assessment.
Keywords: American Indians, arsenic, cancer, mortality
INTRODUCTION
Inorganic arsenic is a major public health problem worldwide. The International Agency for Research on Cancer (IARC) has established a causal role for arsenic on skin, lung and bladder cancers, and has shown suggestive but limited human evidence for liver, kidney and prostate cancers (1). Key epidemiologic evidence came from populations chronically exposed to high arsenic levels in drinking water (>150 μg/L) in Southwestern Taiwan (2), Bangladesh (3), Northern Chile (4) and Argentina (5). Recent experimental studies have shown that inorganic arsenic and its methylated metabolites can induce lung (6, 7), liver (8) and bladder (7, 9) cancers in animal models and malignant transformation of human prostate epithelium in cellular model systems (10).
Main sources of arsenic exposure include drinking water and certain foods (e.g. rice, grains or juices) (11, 12). The current safety standard for arsenic in drinking water established by the World Health Organization, the US Environmental Protection Agency (USEPA) and the European Union is 10 μg/L (13, 14). There are concerns that this limit is too high to protect human populations from excess cancer risk (15). For food, there are no current safety standards, despite widespread low-moderate inorganic arsenic exposure through the diet. Few epidemiologic studies have evaluated the carcinogenic effects of arsenic at low-moderate arsenic levels in drinking water and food, most of them ecological or retrospective (16). We evaluated the association of low-moderate exposure to inorganic arsenic with overall and site-specific cancer mortality in American Indian men and women from Arizona, Oklahoma, and North/South Dakota who participated in the Strong Heart Study (SHS) in 1989–91 and were followed through 2008. For cancers of the lung, liver, prostate and kidney we hypothesized a positive association based on human studies at high arsenic levels (1). For other cancers we had no a priori hypothesis, although arsenic has been associated with pancreas cancer in an ecological study from Japan (17) and a case-control study from Spain (18). Our prospective cohort study can inform about cancer mortality risk at low-moderate arsenic exposure in US populations.
MATERIALS AND METHODS
Study Population
The SHS recruited 4,549 men and women 45–75 years of age from 13 tribes and communities during 1989–1991. In Arizona and Oklahoma every eligible person was invited; in North/South Dakota a cluster sampling technique was used (19). The baseline participation rate was 62%. We excluded 576 participants due to insufficient urine for arsenic analysis, and 38 participants because of missing information in other variables, leaving 3,935 participants for this study. The SHS protocol was approved by local institutional review boards, the Indian Health Service and the study communities. All participants provided oral and written informed consent.
Baseline data collection
Study visits were performed by trained and certified examiners following a standard protocol (19), and included a questionnaire (sociodemographic factors, smoking status, alcohol use and medical history), a physical examination (height, weight, blood pressure) and biospecimen collection (blood, urine). Hypertension was defined as mean systolic blood pressure ≥140 mm Hg, mean diastolic blood pressure ≥90 mm Hg, or antihypertensive medication. Diabetes was defined as fasting plasma glucose ≥126 mg/dL, 2-h post-load plasma glucose ≥200 mg/dL, hemoglobin A1c ≥6.5%, or use of insulin or oral hypoglycemic agents. Plasma creatinine was measured by an alkaline-picrate rate method to estimate glomerular filtration rate (eGFR). Urine creatinine was measured by an automated alkaline picrate methodology (19).
Urine arsenic and creatinine determinations
The analytical methods to determine arsenic species for this study have been described in detail (20). Inorganic arsenic (arsenite, arsenate), monomethylarsonate (MMA), dimethylarsinate (DMA), and arsenobetaine plus other arsenic cations were measured using anion-exchange high-performance liquid chromatography (Agilent 1100 HPLC, Agilent Technologies, Waldbronn, Germany) coupled with inductively coupled plasma mass spectrometry (Agilent 7700x ICPMS). The limits of detection were 0.1μg/L for inorganic arsenic, MMA, DMA and arsenobetaine plus other cationic arsenic species. The percentages of participants with concentrations below the limit of detection were 5.3% for inorganic arsenic, 0.7 % for MMA, 0.03 % for DMA and 2.1% for arsenobetaine plus other cations. For undetectable concentrations, we divided the limit of detection by √2. The interassay coefficients of variation were 6.0% for inorganic arsenic, 6.5% for MMA, 5.9% for DMA and 6.5% for arsenobetaine plus other cations. Arsenobetaine concentrations were low (median 0.76 μg/L, interquartile range 0.47–1.70 μg/L) confirming that seafood intake is rare in the SHS population.
Cancer mortality follow-up
Follow-up for mortality was complete for 99.8% of the study population. Death certificates were obtained from the State Departments of Health. If the death certificate indicated that an autopsy had been performed, the medical examiner’s report was obtained. Death certificate codes were recorded according to the International Classification of Diseases, 9th Revision (ICD-9) by a single nosologist. In addition to overall cancer deaths, we evaluated the following cancers: esophagus and stomach (ICD-9 150–151), colon and rectum (ICD-9 153–154), liver and intrahepatic bile ducts (ICD-9 155) and gallbladder and extrahepatic bile ducts (ICD-9 156) (ICD-9 155 and 156 were combined due to small sample size and similar results in separate analyses), pancreas (ICD-9 157), trachea, bronchus and lung (ICD-9 162) (referred from now on as lung cancer), breast (ICD-9 174), prostate (ICD-9 185), kidney (ICD-9 189.0) and lymphatic and hematopoietic tissue (ICD-9 200–208). Skin and bladder cancers were not evaluated as the corresponding number of deaths was very small (2 and 1, respectively).
Time to event was calculated from the date of baseline examination to the date of death or to December 31, 2008 whichever occurred first. The mean follow-up time among participants who did not have a cancer death was 14.6 years.
Statistical methods
We used the sum of inorganic (arsenite and arsenate) and methylated (MMA and DMA) arsenic as the biomarker of exposure to inorganic arsenic. To account for urine dilution in spot urine samples, we divided urine arsenic by urine creatinine. Urine arsenic concentrations were markedly right-skewed and log-transformed for statistical analyses. Statistical analyses were conducted using Stata 11.2 (StataCorp, College Station, Texas).
The prospective association between the creatinine-corrected sum of inorganic and methylated arsenic and cancer mortality (overall and site-specific) was assessed using Cox-proportional hazards models with age as time scale and individual starting follow-up times (age at baseline) treated as staggered entries. The assumption of hazards proportionality was evaluated based on the smoothed association between age and scaled Schoenfeld residuals, with no major departures from proportionality. The non-parametric underlying baseline hazards were allowed to differ by study region. We modeled arsenic in 3 ways: (1) tertiles; (2) 80th vs. 20th percentiles of log-transformed arsenic; and (3) restricted cubic splines with knots at the 10th (3.80 μg/g creatinine), 50th (9.68 μg/g) and 90th (24.0 μg/g) percentiles to evaluate potential non-linear relationships. P-values for linear trend were obtained from Wald tests by introducing log-arsenic concentrations as a continuous variable. Departures from linearity in the restricted cubic spline models were evaluated using the Wald test.
All Cox-proportional hazards models initially accounted for region (stratification factor) and age (model 1). In addition, we further adjusted for sex, education, smoking status, drinking status and BMI (model 2). Model 2 was further adjusted for menopausal status and parity for breast cancer, for hypertension and reduced eGFR for kidney cancer, and for diabetes for prostate cancer. We conducted exploratory interaction analyses (multiplicative scale) for overall cancer mortality including interaction terms for log-transformed arsenic concentrations with indicator variables for subgroups defined by age, sex, smoking status, diabetes, %DMA and %MMA in separate models. Interaction analyses were not conducted for specific cancers because the number of deaths across subgroups was too small.
We performed several sensitivity analyses. First, we further adjusted for cigarette pack-years (N=3,789). Second, we estimated proportional hazard regression models accounting for competing risks according to the method of Fine and Gray (21). Third, to minimize the possibility that prevalent cancers at baseline modified urine arsenic excretion, we repeated the analyses excluding participants during the first 2 or 5 years of follow-up. Fourth, to evaluate potential differences in latency, we conducted separate analyses for the first and second decades of follow-up. Fifth, we repeated the analyses for overall cancer excluding cancer deaths coded as “malignant neoplasms of other and unspecified sites” The results of these sensitivity analyses were similar to the main analyses (not shown). Finally, we used two alternative strategies to account for urine dilution: 1- adjusting for log-transformed urine creatinine in the regression models instead of dividing urine arsenic by urine creatinine concentrations (22); and 2-adjusting urine arsenic concentrations to the overall mean specific gravity (SG) in the study population (1.019 g/mL) (arsenic (μg/L)*(mean SG (g/mL) −1)/(SG (g/mL) −1)) (23). This last analysis was restricted to participants without albuminuria and diabetes because specific gravity is inadequate to adjust for dilution if albumin or glucose are present in urine (24).
RESULTS
A total of 225 women and 160 men died from cancer during the studied period. The most common cancer sites were lung (N=34) and breast (N=26) in women, and lung (N=44) and prostate (N=18) in men. A total of 46 cancer deaths were unspecified (ICD-9 190–199 and 239). Older participants, participants living in North and South Dakota, participants with lower education, current smokers and never drinkers at baseline had higher cancer mortality (Table 1).
Table 1.
Baseline characteristics of study participants overall and by cancer mortality status
| All participants (N=3,935) | Cancer death | ||
|---|---|---|---|
| Yes (N=386) | No (N=3,549) | ||
| Age, years | 56.2 (8.0) | 59.8 (8.1) | 55.9 (7.9) |
| Men, % | 40.7 | 41.5 | 40.7 |
| Post-menopausal women, %† | 77.0 | 87.6 | 75.8 |
| Arizona, % | 33.4 | 28.2 | 34.0 |
| Oklahoma, % | 33.5 | 32.4 | 33.6 |
| Dakota, % | 33.1 | 39.4 | 32.4 |
| < High school, % | 47.3 | 53.4 | 46.6 |
| Current smoking, % | 33.3 | 42.8 | 32.4 |
| Former Smoking, % | 34.0 | 31.1 | 34.3 |
| Current drinking, % | 41.9 | 35.5 | 42.6 |
| BMI, kg/m2 | 30.9 (6.3) | 30.4 (6.6) | 30.9 (6.3) |
| Diabetes, % | 49.4 | 50.4 | 49.3 |
Data in the table are percentages for categorical variables or means (SD) for continuous variables.
Subsample of women (N=2,332)
The median (IQR) concentration for inorganic plus methylated arsenic at baseline was 9.7 (5.8–15.6) μg/g creatinine [10.4 (6.12–18.4) μg/L]. Participants living in Arizona and North and South Dakota, participants who had a lower education, current drinkers, and those with lower body mass index and diabetes had higher urine arsenic concentrations (Table 2).
Table 2.
Median (IQR) for the sum of inorganic and methylated arsenic concentrations by participant characteristics
| All participants | Participants without diabetes and albuminuria | ||||||
|---|---|---|---|---|---|---|---|
| Arsenic (μg/g creatinine) | Arsenic (μg/L)* | ||||||
|
| |||||||
| N | Median (IQR) | p-value** | N | Median (IQR) | p-value** | ||
| Overall | 3,935 | 9.7 (5.8–15.6) | 1,765 | 11.1 (6.9–17.7) | |||
|
| |||||||
| Age | <55 years | 1,947 | 9.7 (5.9–15.7) | 959 | 11.1 (7.1–17.9) | ||
| 55–64 | 1,292 | 9.6 (5.7–15.4) | 0.28 | 548 | 11.3 (6.7–17.6) | ||
| >65 | 696 | 9.7 (5.6–15.8) | 258 | 10.9 (6.4–18.0) | 0.53 | ||
|
| |||||||
| Sex | Male | 1,603 | 8.8 (5.1–14.3) | <0.001 | 784 | 11.3 (6.8–17.6) | |
| Female | 2,332 | 10.4 (6.2–16.6) | 981 | 11.0 (6.9–17.9) | 0.57 | ||
|
| |||||||
| Region | Arizona | 1,314 | 14.3 (9.9–20.8) | 329 | 15.6 (10.3–23.6) | ||
| Oklahoma | 1,318 | 5.6 (3.8–8.2) | <0.001 | 702 | 7.5 (5.1–11.7) | ||
| Dakota | 1,303 | 10.6 (6.9–15.8) | 734 | 13.0 (8.7–20.9) | <0.001 | ||
|
| |||||||
| Education | No high school | 868 | 13.1 (8.9–20.3) | 302 | 15.5 (10.3–22.5) | ||
| Some high school | 992 | 10.1 (5.9–16.6) | <0.001 | 398 | 11.2 (6.8–18.6) | ||
| Completed high school | 2,075 | 8.0 (5.0–13.2) | 1,065 | 10.0 (6.3–16.1) | <0.001 | ||
|
| |||||||
| Smoking status | Never | 1,284 | 10.1 (6.0–16.5) | 511 | 10.5 (6.6–17.5) | ||
| Former | 1,338 | 9.2 (5.6–15.0) | 0.01 | 553 | 10.4 (6.5–16.1) | ||
| Current | 1,313 | 9.7 (5.8–15.4) | 791 | 12.4 (7.5–19.8) | 0.008 | ||
|
| |||||||
| Alcohol status | Never | 636 | 9.2 (5.5–15.5) | 241 | 9.7 (6.2–16.0) | ||
| Former | 1,650 | 8.7 (5.3–14.4) | <0.001 | 699 | 10.0 (6.5–15.4) | ||
| Current | 1,649 | 10.8 (6.4–17.1) | 825 | 12.5 (7.9–21.2) | <0.001 | ||
|
| |||||||
| BMI | <25 kg/m2 | 610 | 10.7 (5.8–17.6) | 364 | 12.3 (7.2–21.0) | ||
| 25–30 | 1,324 | 9.6 (5.6–15.7) | 0.02 | 683 | 10.8 (6.7–17.4) | ||
| >30 | 2,001 | 9.5 (5.9–15.0) | 718 | 10.9 (6.9–16.8) | 0.002 | ||
|
| |||||||
| Diabetes | No | 1,986 | 8.4 (5.1–13.6) | <0.001 | 1,765 | 11.1 (6.9–17.7) | |
| Yes | 1,939 | 11.0 (6.6–18.0) | - | ||||
|
| |||||||
| Glomerular Filtration Rate | ≤60 mL/min/1.73 m2 | 395 | 8.9 (5.3–14.6) | 0.03 | 105 | 11.1 (6.9–17.9) | |
| >60 | 3,468 | 9.8 (5.8–15.7) | 1,628 | 11.5 (6.9–18.3) | 0.67 | ||
Adjusted to mean specific gravity in the study population of 1.019 using the following formula: arsenic (μg/L)*(1.019 (g/mL) −1)/(SG (g/mL) −1)
p-value from Kruskall-Wallis exact test
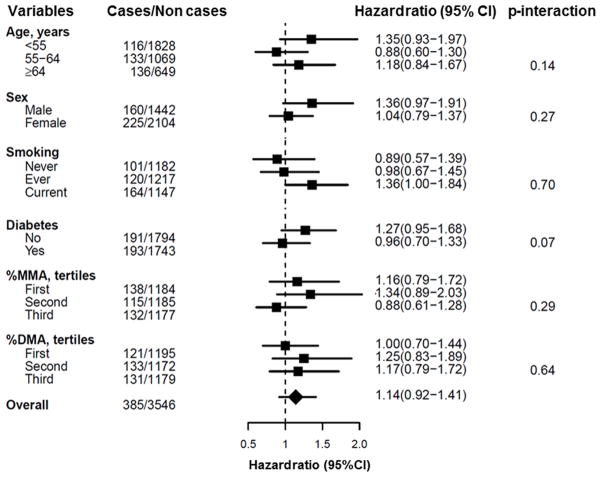
After multivariate adjustment, the hazard ratio (95% CI) for overall cancer mortality comparing the 80th vs. 20th percentile of urine arsenic concentrations was 1.14 (0.92–1.41) (Table 3). The corresponding hazard ratios for cancers of the lung, liver, prostate and kidney were 1.56 (1.02–2.39), 1.34 (0.66–2.72), 3.30 (1.28–8.48) and 0.44 (0.14–1.14), respectively. For pancreas cancer, the corresponding hazard ratio was 2.46 (1.09–5.58) and for lymphatic and hematopoietic cancers it was 0.46 (0.22–0.96). Arsenic was not associated with other cancers. The linear trend for increased mortality with increasing arsenic levels was statistically significant for lung (p=0.04), prostate (p=0.01) and pancreatic (p=0.03) cancers. When modeling the dose-response relationship using restricted cubic splines, we observed no significant departures from linearity for those cancers (figure 1).
Table 3.
Hazard ratios (95% confidence interval) for cancer mortality by urine arsenic concentrations
| Sum inorganic and methylated arsenic tertiles | 80th vs 20th percentiles* | p-trend** | |||
|---|---|---|---|---|---|
| <6.91 μg/g | 6.91–13.32μg/g | >13.32 μg/g | |||
| Overall cancer (ICD-9 140 to 208) | |||||
| Cases/Non Cases | 121/1,198 | 135/1,181 | 130/1,170 | 386/3,549 | |
| Model 1 | 1 (Referent) | 1.17 (0.90–1.52) | 1.27 (0.96–1.70) | 1.16 (0.94–1.42) | 0.16 |
| Model 2 | 1 (Referent) | 1.17 (0.90–1.53) | 1.23 (0.92–1.65) | 1.14 (0.92–1.41) | 0.24 |
| Trachea, bronchus, and lung (ICD-9 162) | |||||
| Cases/Non Cases | 27/1,292 | 20/1,296 | 31/1,269 | 78/3,857 | |
| Model 1 | 1 (Referent) | 0.89 (0.49–1.62) | 1.95 (1.09–3.49) | 1.59 (1.05–2.42) | 0.03 |
| Model 2 | 1 (Referent) | 0.94 (0.51–1.72) | 1.82 (1.00–3.32) | 1.56 (1.02–2.39) | 0.04 |
| Liver, gallbladder and bile ducts (ICD-9 155–156) | |||||
| Cases/Non Cases | 8/1311 | 13/1303 | 13/1287 | 34/3901 | |
| Model 1 | 1 (Referent) | 1.51 (0.59–3.88) | 1.56 (0.56–4.32) | 1.50 (0.76–2.97) | 0.24 |
| Model 2 | 1 (Referent) | 1.38 (0.53–3.62) | 1.36 (0.47–3.95) | 1.34 (0.66–2.72) | 0.41 |
| Prostate (ICD-9 185) | |||||
| Cases/Non Cases | 6/605 | 5/526 | 7/454 | 18/1,585 | |
| Model 1 | 1 (Referent) | 1.25 (0.37–4.26) | 2.90 (0.85–9.92) | 1.91 (0.82–4.41) | 0.13 |
| Model 2 | 1 (Referent) | 1.55 (0.45–5.33) | 4.58 (1.31–16.6) | 3.30 (1.28–8.48) | 0.01 |
| Kidney (ICD-9 189.0)†† | |||||
| Cases/Non Cases | 9/1,310 | 9/1,307 | 8/1,292 | 26/3,909 | |
| Model 1 | 1 (Referent) | 0.68 (0.25–1.86) | 0.50 (0.15–1.42) | 0.69 (0.25–1.90) | 0.28 |
| Model 2 | 1 (Referent) | 0.69 (0.25–1.90) | 0.44 (0.14–1.40) | 0.44 (0.14–1.40) | 0.36 |
| Esophagus and Stomach Cancer (ICD-9 150–151) | |||||
| Cases/Non Cases | 8/1,311 | 8/1,308 | 8/1,292 | 24/3,911 | |
| Model 1 | 1 (Referent) | 1.19 (0.42–3.39) | 1.33 (0.41–4.29) | 0.94 (0.40–2.24) | 0.89 |
| Model 2 | 1 (Referent) | 1.33 (0.46–3.84) | 1.57 (0.47–5.26) | 1.09 (0.45–2.66) | 0.85 |
| Pancreas (ICD-9 157) | |||||
| Cases/Non Cases | 7/1,312 | 7/1,309 | 11/1,289 | 25/3,910 | |
| Model 1 | 1 (Referent) | 1.04 (0.34–3.19) | 2.14 (0.67–6.82) | 2.26 (1.04–4.88) | 0.04 |
| Model 2 | 1 (Referent) | 1.04 (0.33–3.29) | 2.14 (0.67–6.82) | 2.46 (1.09–5.58) | 0.03 |
| Colon and rectal cancer (ICD-9 153–154) | |||||
| Cases/Non Cases | 12/1,307 | 14/1,302 | 6/1,294 | 32/3,903 | |
| Model 1 | 1 (Referent) | 1.46 (0.65–3.29) | 0.87 (0.30–2.57) | 0.83 (0.40–2.24) | 0.62 |
| Model 2 | 1 (Referent) | 1.41 (0.62–3.21) | 0.82 (0.27–2.48) | 0.78 (0.36–1.67) | 0.52 |
| Breast (ICD-9 174)† | |||||
| Cases/Non Cases | 7/701 | 13/772 | 6/833 | 26/2,306 | |
| Model 1 | 1 (Referent) | 1.79 (0.67–4.74) | 0.90 (0.27–3.07) | 0.84 (0.37–1.93) | 0.99 |
| Model 2 | 1 (Referent) | 1.92 (0.71–5.15) | 0.96 (0.28–3.22) | 1.00 (0.44–2.28) | 0.69 |
| Lymphatic and hematopoietic tissue (ICD-9 200–208) | |||||
| Cases/Non Cases | 11/1,308 | 20/1,296 | 9/1,291 | 40/3,895 | |
| Model 1 | 1 (Referent) | 1.63 (0.74–3.61) | 0.69(0.26–1.87) | 0.59 (0.29–1.17) | 0.13 |
| Model 2 | 1 (Referent) | 1.44 (0.64–3.25) | 0.57 (0.21–1.58) | 0.46 (0.22–0.96) | 0.04 |
Model 1: Unadjusted, stratified by center.
Model 2: Adjusted for, sex, age, education (no high school/some high school/completed high school), smoking status (never, former, current), drinking status (never, former, current), and BMI (kg/m2).
Model 2 for breast cancer was further adjusted for menopausal status and parity.
Model 2 for kidney cancer was further adjusted for estimated glomerular filtration rate (<60, ≥60 ml/min/1.72m2) and hypertension status (yes/no)
Models comparing the 80th vs 20th percentiles of urine arsenic distributions and associated p-trend were obtained from Cox proportional hazards models with log-transformed arsenic as a continuous variable.
p trend calculated modeling log-arsenic as continuous
Figure 1. Hazard ratios for cancer mortality by urine arsenic concentrations.
Lines represent the hazard ratio (thick line) and 95% confidence intervals (thin line) for overall and specific cancer mortality based on restricted cubic splines for log-transformed sum of inorganic and methylated species with knots at the 10th (3.8 μg/g creatinine), 50th (9.7 μg/g) and 90th (24.0 μg/g) percentiles. The reference was set at the 10th percentile of arsenic distribution. Models were adjusted for age, sex, education (no high school/some high school/completed high school), smoking status (never, former, current), drinking status (never, former, current) and BMI (kg/m2). Vertical bars represent the histogram of arsenic distribution in the study population.
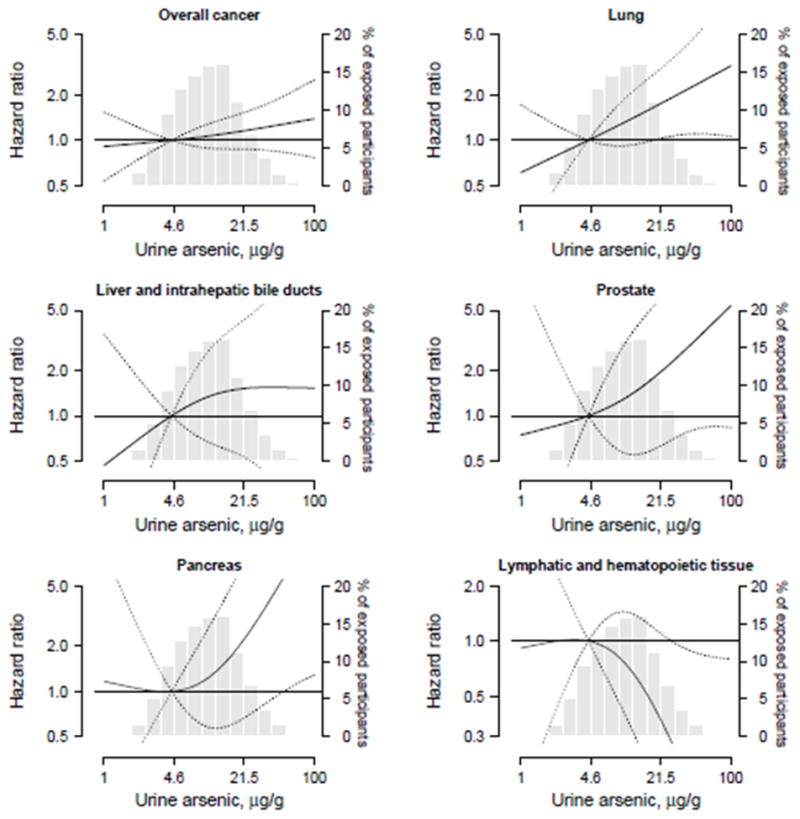
In subgroup analyses by participant characteristics (figure 2), the fully-adjusted hazard ratio for overall cancer mortality comparing the 80th vs. 20th percentile of inorganic plus methylated arsenic was consistent for most participant subgroups except diabetes at baseline (p for interaction=0.07).
Figure 2.
Hazard ratios (95% confidence interval) for overall cancer mortality comparing the 80th to the 20th percentiles of the sum of inorganic and methylated arsenic species (μg/g creatinine) by participant characteristics at baseline.
In sensitivity analyses adjusting for log-transformed urine creatinine, the results were similar compared to analyses dividing by urine creatinine (hazard ratio (95% CI) for overall cancer mortality comparing the 80th vs. 20th percentile of arsenic was 1.12 (0.88–1.42) and for lung cancer mortality it was 1.53 (0.94–2.48)). Among participants without diabetes or albuminuria (N=1,765, 166 overall cancers, 48 lung cancers), the corresponding hazard ratios adjusting for overall specific gravity were also consistent, although not significant, for overall (1.29 (0.96–1.73)) and lung cancer mortality (1.35 (0.80–2.27)). Finally, when excluding deaths coded as “malignant neoplasms of other and unspecified sites” (N=26) from the analysis for overall cancer mortality the results remained similar, and the observed hazard ratio (95%CI) comparing the 80th vs 20th percentiles of arsenic was 1.16 (95% 0.93–1.44).
DISCUSSION
Summary of the findings
In this US-based prospective cohort study, low to moderate inorganic arsenic exposure, as measured in urine, was associated with increased mortality from lung, prostate and pancreas cancer over almost 20 years of follow-up. The associations persisted after adjustment for sociodemographic and behavioral cancer risk factors. Unexpectedly, arsenic exposure was associated with decreased mortality from lymphatic and hematopoietic cancers. Arsenic was not associated with kidney cancer, and for liver cancer the increased risk was small and statistically non-significant. Both tumors have been associated with high arsenic exposure in other populations (17, 25). Overall, increasing urine arsenic concentrations showed a positive but non-significant association with total cancer mortality. Our results extend the associations of arsenic with lung and prostate cancer, observed previously only at high levels of exposure (17, 26–28). We also found supportive evidence for pancreas cancer, a cancer with limited epidemiological evidence available.
Sources of arsenic exposure in the Strong Heart Study
Participants in the Strong Heart Study rely either on small public water systems or on private wells. At the time of the study, arsenic concentrations in public drinking water systems for the study communities ranged from <10 up to 61 μg/L in Arizona and from <10 up to 21 μg/L in North and South Dakota. Levels in private wells are not known but given arsenic concentrations in groundwater in those regions (29), it is likely that arsenic levels exceeded 10 and even 50 μg/L. In Oklahoma, arsenic levels in public water systems were <10 μg/L, and similar to other populations with low arsenic levels in drinking water (30), we expect diet to be the main source of arsenic exposure in Oklahoma.
Epidemiologic evidence at high levels of exposure
Several studies have evaluated the association between lung cancer and high levels of arsenic exposure. In 10,591 participants from Southwestern Taiwan (27), the hazard ratios for lung cancer incidence were 1.09, 2.28, 3.03 and 3.29 for arsenic concentrations in drinking water of 10–99, 100–299, 300–699 and ≥700 μg/L, respectively, compared to <10 μg/L. In a case-control study from Antofagasta (Chile) (31), the odds ratio for lung cancer comparing the highest (200–400 μg/L) to the lowest (<10 μg/L) categories of arsenic in drinking water was 8.9 (95%CI: 4.0–19.6). Lung cancer mortality was also increased among young adults in Northern Chile who were exposed to high doses of arsenic in utero (32).
Regarding prostate cancer, ecological evidence from Southwestern Taiwan showed increased prostate cancer mortality compared to the overall Taiwanese population (2). Based on the Taiwanese evidence, the IARC concluded there was evidence for a dose-response relationship (1). In a population from Utah exposed to moderate arsenic levels in drinking water, the SMR for prostate cancer compared to the overall US population was 1.48 (95%CI: 1.07–1.91) (33).
Epidemiologic evidence for an association between arsenic and pancreas cancer is scarce. Japanese individuals exposed during infancy to high arsenic levels through contaminated milk showed an SMR for pancreatic cancer of 1.79 (95%CI: 1.23–2.61) compared to unexposed (17). In a case-control study from Spain (18), at low-moderate arsenic in drinking water (34), the odds ratio for exocrine pancreatic cancer comparing the highest (≥0.11 μg/g) to the lowest (≤0.05 μg/g) toenail arsenic quartiles was 2.02 (1.08–3.78).
Few studies have evaluated the association between arsenic and overall cancer mortality. In a prospective cohort including 115,903 participants in Bangladesh, the hazard ratios (95%CI) for cancer mortality were 1.10 (0.77–1.59), 1.44 (1.06–1.95), 1.75 (1.28–2.40) and 1.56 (1.06–2.30) comparing arsenic concentrations in drinking water of 10–49, 50–149, 150–299 and ≥300 to <10 μg/L, respectively (35).
Epidemiologic evidence at low-moderate levels of exposure
Evidence at low-moderate arsenic levels remains limited for most cancers. Bladder cancer has been the most frequently studied cancer, with inconsistent findings (33, 36, 37). For lung cancer, a case-control study conducted in New Hampshire and Vermont counties found an odds ratio for small-cell and squamous-cell carcinoma of 2.75 (95% CI 1.39–5.91) comparing toenail arsenic concentrations ≥0.114 vs. <0.05 μg/g (38). In our study, histological information was not available and we cannot evaluate if the association found with lung cancer mortality was also related to those cancer types. At very low levels of exposure, a Danish cohort of 57,053 participants found no association between arsenic in drinking water (mean 1.2 μg/L) with lung, liver, bladder, kidney or prostate cancer incidence over 10 years of follow-up (36). Our study, conducted in a population exposed to low-moderate arsenic levels, extends previous evidence for mortality associated with several cancer types but included too few cases to evaluate some cancers of interest, including bladder and skin cancers.
Mechanistic evidence
Despite the extensive epidemiologic evidence, the mechanisms for arsenic carcinogenicity remain unclear. A major challenge has been to develop animal models, with transplacental models being essential to advance our understanding of arsenic carcinogenesis (39). Some of the accepted mechanisms involve genetic and epigenetic changes, oxidative stress, enhanced cell proliferation, mitochondrial damage and modulation of gene expression (40–42). For prostate cancer, arsenic accelerates prostate cancer cell progression by inducing androgen independence (10). Little is known about mechanisms for arsenic related pancreatic cancer, although arsenic induces oxidative stress and apoptosis of pancreatic β-cells (43) and acinar cells (44), as well as changes in the pancreatic vasculature (45).
Lymphatic and hematopoietic cancers
In occupational settings (46, 47), and in infants exposed through milk powder (17), arsenic exposure has been associated with increased blood cancer mortality. Arsenic trioxide is used in the treatment of some leukemias such as acute promyelocytic leukemia (48), and is under investigation for multiple myeloma (49). Arsenic trioxide pharmacotherapy has been related to cytotoxicity and apoptosis in cancer cells (50). Since we could not specifically evaluate the association between arsenic and specific lymphatic or hematopoietic cancers due to the small number of cases, this finding requires replication in other populations and needs to be interpreted with caution.
Strengths and limitations
The prospective design and long follow-up, the low rate of follow-up losses, the careful standardization and quality control of data collection and laboratory analyses, and the high sensitivity of our assay for urine arsenic species are major strengths of this study (19, 20). Urine arsenic, an integrated biomarker of ongoing exposure, has a relatively short half-life. Previous evidence in the SHS, however, showed relatively constant concentrations over a 10 year-period (51), indicating that a single measure reflects long-term arsenic exposure in this population. Moreover, the Strong Heart Study is a very stable population and most of the participants were born on the communities and have lived there all their lives. The estimated migration rates during the study period are 0.5% in Arizona, 1.5% in Oklahoma, and 2.7% in North and South Dakota. Finally, this study provides information on environmental cancer determinants in American Indian communities, a population understudied for cancer risk that is disproportionately exposed to arsenic in drinking water compared to the general US population (51).
Our study has some limitations. First, cancer mortality is an imperfect outcome to study tumors with relatively good prognosis, such as bladder and skin cancer. Second, we relied on death certificates, which may lack accuracy compared to clinical or pathology records (52). Cancer deaths, however, are considered to be better coded than other causes of death. Third, the number of deaths and statistical power was limited for some cancers, for subgroup analyses, and to detect a potential small increase in overall cancer mortality. For instance, we could not evaluate the association with some cancer deaths separately such as colon and rectal cancer, or esophagus and stomach cancer. Fourth, we did not account for multiple comparisons, although the number of statistically significant associations expected to happen by chance for a total of 9 cancer-specific associations is less than one. Fifth, we could not account for family history of cancer or for clustering of arsenic exposure. Finally, arsenic levels in drinking water were only available at the community level. Arsenic in urine, however, correlates well with levels in drinking water (53) and integrates multiple sources of exposure including food (54).
Conclusions
Low to moderate inorganic arsenic exposure, as measured in urine, was prospectively associated with increased mortality for lung, prostate and pancreas cancer in the SHS. This study provides novel evidence regarding cancer mortality at low-moderate arsenic exposure in drinking water in rural communities from the US. Future studies at low-moderate arsenic levels need to evaluate the association with cancer incidence and the role of arsenic metabolism in cancer development. The current US EPA maximum contaminant level of 10 μg/L was established based on lung and bladder cancer risk in highly exposed populations from Southwestern Taiwan, and the risk of arsenic exposure at lower doses was derived using linear low-dose extrapolation. Our findings provide direct evidence at low-moderate arsenic levels and support a linear dose-response relationship with lung, prostate and pancreas cancers with no evidence of a threshold.
Acknowledgments
Financial support: This work was supported by the National Heart Lung and Blood Institute (grant HL090863 and by SHS grants HL41642, HL41652, HL41654 and HL65521). Dr. Esther Garcia-Esquinas was supported by a Río Hortega (CM10/00332) research training grant from the Spanish Ministry of Economy and Competitiveness (Carlos III Institute of Health). Dr. Navas-Acien had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Author contributions:
Navas-Acien, Umans, Francesconi, Goessler, Guallar, Howard, Farley, Yeh and Best conceptualized and designed the study, reviewed and revised the manuscript and approved the final manuscript as submitted.
Drs García-Esquinas, Navas-Acien and Pollán conducted statistical analyses, interpreted the data, drafted the initial manuscript, and approved the final manuscript as submitted.
Conflict of interest: The authors have no conflict of interest to declare.
References
- 1.International Agency for Research on Cancer (IARC) Monographs on the Evaluation of Carcinogenic Risks to Humans. Some drinking-water disinfectants and contaminants, including Arsenic. 2004;84 Available at: http://monographs.iarc.fr/ENG/Monographs/vol84/mono84.pdf. [PMC free article] [PubMed] [Google Scholar]
- 2.Chen CJ, Kuo TL, Wu MM. Arsenic and cancers. Lancet. 1988;1(8582):414–5. doi: 10.1016/s0140-6736(88)91207-x. [DOI] [PubMed] [Google Scholar]
- 3.Kurokawa M, Ogata K, Idemori M, Tsumori S, Miyaguni H, Inoue S, et al. Investigation of skin manifestations of arsenicism due to intake of arsenic-contaminated groundwater in residents of Samta, Jessore, Bangladesh. Arch Dermatol. 2001;137(1):102–3. [PubMed] [Google Scholar]
- 4.Smith AH, Goycolea M, Haque R, Biggs ML. Marked increase in bladder and lung cancer mortality in a region of Northern Chile due to arsenic in drinking water. Am J Epidemiol. 1998;147(7):660–9. doi: 10.1093/oxfordjournals.aje.a009507. [DOI] [PubMed] [Google Scholar]
- 5.Hopenhayn-Rich C, Biggs ML, Smith AH. Lung and kidney cancer mortality associated with arsenic in drinking water in Cordoba, Argentina. Int J Epidemiol. 1998;27(4):561–9. doi: 10.1093/ije/27.4.561. [DOI] [PubMed] [Google Scholar]
- 6.Stueckle TA, Lu Y, Davis ME, Wang L, Jiang BH, Holskova I, et al. Chronic occupational exposure to arsenic induces carcinogenic gene signaling networks and neoplastic transformation in human lung epithelial cells. Toxicol Appl Pharmacol. 2012;261(2):204–16. doi: 10.1016/j.taap.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tokar EJ, Benbrahim-Tallaa L, Ward JM, Lunn R, Sams RL, Waalkes MP, et al. Cancer in experimental animals exposed to arsenic and arsenic compounds. Crit Rev Toxicol. 2010;40(10):912–27. doi: 10.3109/10408444.2010.506641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J, Waalkes MP. Liver is a target of arsenic carcinogenesis. Toxicol Sci. 2008;105(1):24–32. doi: 10.1093/toxsci/kfn120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bredfeldt TG, Jagadish B, Eblin KE, Mash EA, Gandolfi AJ. Monomethylarsonous acid induces transformation of human bladder cells. Toxicol Appl Pharmacol. 2006;216(1):69–79. doi: 10.1016/j.taap.2006.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benbrahim-Tallaa L, Waalkes MP. Inorganic arsenic and human prostate cancer. Environ Health Perspect. 2008;116(2):158–64. doi: 10.1289/ehp.10423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson BP, Taylor VF, Karagas MR, Punshon T, Cottingham KL. Arsenic, organic foods, and brown rice syrup. Environ Health Perspect. 2012;120(5):623–6. doi: 10.1289/ehp.1104619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Food Safety Authority (EFSA) and EFSA Panel on Contaminants in the Food Chain (CONTAM) Arsenic in food. EFSA Journal. 2009;7(10):1351. doi: 10.2903/j.efsa.2008.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Environmental Protection Agency (EPA) Arsenic compounds. 1992 Available at: http://www.epa.gov/ttn/atw/hlthef/arsenic.html.
- 14.World Health Organization (WHO) Guidelines for drinking water quality 1993. 2012;1 Available at: http://www.who.int/water_sanitation_health/dwq/fulltext.pdf. [Google Scholar]
- 15.Smith AH. Arsenic Health Effects Research Program. Is the proposed new arsenic water standard of 10 ug/L sufficiently protective of public health? Available at: http://wwwbrr.cr.usgs.gov/projects/GWC_chemtherm/FinalAbsPDF/smith.pdf.
- 16.Cantor KP, Lubin JH. Arsenic, internal cancers, and issues in inference from studies of low-level exposures in human populations. Toxicol Appl Pharmacol. 2007;222(3):252–7. doi: 10.1016/j.taap.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yorifuji T, Tsuda T, Doi H, Grandjean P. Cancer excess after arsenic exposure from contaminated milk powder. Environ Health Prev Med. 2011;16(3):164–70. doi: 10.1007/s12199-010-0182-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaral AF, Porta M, Silverman DT, Milne RL, Kogevinas M, Rothman N, et al. Pancreatic cancer risk and levels of trace elements. Gut. 2012;61(11):1583–8. doi: 10.1136/gutjnl-2011-301086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, et al. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol. 1990;132(6):1141–55. doi: 10.1093/oxfordjournals.aje.a115757. [DOI] [PubMed] [Google Scholar]
- 20.Scheer J, Findenig S, Goessler W, Francesconi KA, Howard B, Umans JG, et al. Arsenic species and selected metals in human urine: validation of HPLC/ICPMS and ICPMS procedures for a long-term population-based epidemiological study. Anal Methods. 2012;4(2):406–13. doi: 10.1039/C2AY05638K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 2012;94:496–509. 1999. [Google Scholar]
- 22.Gamble MV, Hall MN. Relationship of creatinine and nutrition with arsenic metabolism. Environ Health Perspect. 2012;120(4):A145–A146. doi: 10.1289/ehp.1104807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nermell B, Lindberg AL, Rahman M, Berglund M, Persson LA, El-Arifeen S, et al. Urinary arsenic concentration adjustment factors and malnutrition. Environ Res. 2008;106(2):212–8. doi: 10.1016/j.envres.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Voinescu GC, Shoemaker M, Moore H, Khanna R, Nolph KD. The relationship between urine osmolality and specific gravity. Am J Med Sci. 2002;323(1):39–42. doi: 10.1097/00000441-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Chen CJ, Chuang YC, Lin TM, Wu HY. Malignant neoplasms among residents of a blackfoot disease-endemic area in Taiwan: high-arsenic artesian well water and cancers. Cancer Res. 1985;45(11 Pt 2):5895–9. [PubMed] [Google Scholar]
- 26.Wu MM, Kuo TL, Hwang YH, Chen CJ. Dose-response relation between arsenic concentration in well water and mortality from cancers and vascular diseases. Am J Epidemiol. 1989;130(6):1123–32. doi: 10.1093/oxfordjournals.aje.a115439. [DOI] [PubMed] [Google Scholar]
- 27.Chen CL, Hsu LI, Chiou HY, Hsueh YM, Chen SY, Wu MM, et al. Ingested arsenic, cigarette smoking, and lung cancer risk: a follow-up study in arseniasis-endemic areas in Taiwan. JAMA. 2004;292(24):2984–90. doi: 10.1001/jama.292.24.2984. [DOI] [PubMed] [Google Scholar]
- 28.Wadhwa SK, Kazi TG, Chandio AA, Afridi HI, Kolachi NF, Kandhro GA, et al. Comparative study of liver cancer patients in arsenic exposed and non-exposed areas of Pakistan. Biol Trace Elem Res. 2011;144(1–3):86–96. doi: 10.1007/s12011-011-9036-7. [DOI] [PubMed] [Google Scholar]
- 29.Ryker SJ. Mapping arsenic in groundwater. Geotimes. 2001;46:34–6. [Google Scholar]
- 30.Kurzius-Spencer M, O’Rourke MK, Hsu CH, Artz H, Arris VH, Burgess RB, JL, et al. Measured versus modeled dietary arsenic and relation to urinary arsenic excretion and total exposure. J Expo Sci Environ Epidemiol. 2013 doi: 10.1038/jes.2012.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferreccio C, Gonzalez PC, Milosavjlevic SV, Marshall GG, Sancha AM. Lung cancer and arsenic exposure in drinking water: a case-control study in northern Chile. Cad Saude Publica. 1998;14 (Suppl 3):193–8. doi: 10.1590/s0102-311x1998000700021. [DOI] [PubMed] [Google Scholar]
- 32.Smith AH, Marshall G, Liaw J, Yuan Y, Ferreccio C, Steinmaus C, et al. Mortality in Young Adults following in Utero and Childhood Exposure to Arsenic in Drinking Water. Environ Health Perspect. 2012;120(11):1527–31. doi: 10.1289/ehp.1104867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewis DR, Southwick JW, Ouellet-Hellstrom R, Rench J, Calderon RL. Drinking water arsenic in Utah: A cohort mortality study. Environ Health Perspect. 1999;107(5):359–65. doi: 10.1289/ehp.99107359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medrano MA, Boix R, Pastor-Barriuso R, Palau M, Damián J, Ramis R, et al. Arsenic in public water supplies and cardiovascular mortality in Spain. Environ Res. 2010;110(5):448–54. doi: 10.1016/j.envres.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Sohel N, Persson LA, Rahman M, Streatfield PK, Yunus M, Ekstrom EC, et al. Arsenic in drinking water and adult mortality: a population-based cohort study in rural Bangladesh. Epidemiology. 2009;20(6):824–30. doi: 10.1097/EDE.0b013e3181bb56ec. [DOI] [PubMed] [Google Scholar]
- 36.Baastrup R, Sorensen M, Balstrom T, Frederiksen K, Larsen CL, Tjonneland A, et al. Arsenic in drinking-water and risk for cancer in Denmark. Environ Health Perspect. 2008;116(2):231–7. doi: 10.1289/ehp.10623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mink PJ, Alexander DD, Barraj LM, Kelsh MA, Tsuji JS. Low-level arsenic exposure in drinking water and bladder cancer: a review and meta-analysis. Regul Toxicol Pharmacol. 2008;52(3):299–310. doi: 10.1016/j.yrtph.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 38.Heck JE, Andrew AS, Onega T, Rigas JR, Jackson BP, Karagas MR, et al. Lung cancer in a U.S. population with low to moderate arsenic exposure. Environ Health Perspect. 2009;117(11):1718–23. doi: 10.1289/ehp.0900566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Waalkes MP, Liu J, Ward JM, Diwan BA. Animal models for arsenic carcinogenesis: inorganic arsenic is a transplacental carcinogen in mice. Toxicol Appl Pharmacol. 2004;198(3):377–84. doi: 10.1016/j.taap.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 40.Hughes MF. Arsenic toxicity and potential mechanisms of action. Toxicol Lett. 2002;133(1):1–16. doi: 10.1016/s0378-4274(02)00084-x. [DOI] [PubMed] [Google Scholar]
- 41.Rossman TG. Mechanism of arsenic carcinogenesis: an integrated approach. Mutat Res. 2003;533(1–2):37–65. doi: 10.1016/j.mrfmmm.2003.07.009. [DOI] [PubMed] [Google Scholar]
- 42.Martinez VD, Vucic EA, Adonis M, Gil L, Lam WL. Arsenic biotransformation as a cancer promoting factor by inducing DNA damage and disruption of repair mechanisms. Mol Biol Int. 2011;2011:718974. doi: 10.4061/2011/718974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lu TH, Su CC, Chen YW, Yang CY, Wu CC, Hung DZ, et al. Arsenic induces pancreatic beta-cell apoptosis via the oxidative stress-regulated mitochondria-dependent and endoplasmic reticulum stress-triggered signaling pathways. Toxicol Lett. 2011;201(1):15–26. doi: 10.1016/j.toxlet.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Xue DB, Zhang WH, Yun XG, Song C, Zheng B, Shi XY, et al. Regulating effects of arsenic trioxide on cell death pathways and inflammatory reactions of pancreatic acinar cells in rats. Chin Med J (Engl) 2007;120(8):690–5. [PubMed] [Google Scholar]
- 45.Davila-Esqueda ME, Morales JM, Jimenez-Capdeville ME, De la Cruz E, Falcon-Escobedo R, Chi-Ahumada E, et al. Low-level subchronic arsenic exposure from prenatal developmental stages to adult life results in an impaired glucose homeostasis. Exp Clin Endocrinol Diabetes. 2011;119(10):613–7. doi: 10.1055/s-0031-1287782. [DOI] [PubMed] [Google Scholar]
- 46.Axelson O, Dahlgren E, Jansson CD, Rehnlund SO. Arsenic exposure and mortality: a case-referent study from a Swedish copper smelter. Br J Ind Med. 1978;35(1):8–15. doi: 10.1136/oem.35.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ott MG, Holder BB, Gordon HL. Respiratory cancer and occupational exposure to arsenicals. Arch Environ Health. 1974;29(5):250–5. doi: 10.1080/00039896.1974.10666582. [DOI] [PubMed] [Google Scholar]
- 48.Rehman K, Naranmandura H. Arsenic metabolism and thioarsenicals. Metallomics. 2012 doi: 10.1039/c2mt00181k. [DOI] [PubMed] [Google Scholar]
- 49.Chanan-Khan AA, Borrello I, Lee KP, Reece DE. Development of target-specific treatments in multiple myeloma. Br J Haematol. 2010;151(1):3–15. doi: 10.1111/j.1365-2141.2010.08262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yedjou C, Tchounwou P, Jenkins J, McMurray R. Basic mechanisms of arsenic trioxide (ATO)-induced apoptosis in human leukemia (HL-60) cells. J Hematol Oncol. 2010;3:28. doi: 10.1186/1756-8722-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Navas-Acien A, Umans JG, Howard BV, Goessler W, Francesconi KA, Crainiceanu CM, et al. Urine arsenic concentrations and species excretion patterns in American Indian communities over a 10-year period: the Strong Heart Study. Environ Health Perspect. 2009;117(9):1428–33. doi: 10.1289/ehp.0800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45(5):747–55. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 53.Calderon RL, Hudgens E, Le XC, Schreinemachers D, Thomas DJ. Excretion of arsenic in urine as a function of exposure to arsenic in drinking water. Environ Health Perspect. 1999;107(8):663–7. doi: 10.1289/ehp.99107663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rivera-Nunez Z, Meliker JR, Meeker JD, Slotnick MJ, Nriagu JO. Urinary arsenic species, toenail arsenic, and arsenic intake estimates in a Michigan population with low levels of arsenic in drinking water. J Expo Sci Environ Epidemiol. 2012;22(2):182–90. doi: 10.1038/jes.2011.27. [DOI] [PMC free article] [PubMed] [Google Scholar]