Abstract
Various types of diseases can involve the nasal vestibule. Diagnosis and treatment of a nasal vestibular mass is often challenging due to the anatomical features of the nasal vestibule. Here, we present four cases with nasal vestibular masses. Two cases were diagnosed as squamous papillomas. The others were a trichofolliculoma and pseudoepitheliomatous hyperplasia with hyperkeratosis. Our aim was to discuss the characteristics of each disease and the considerations thought to be necessary for diagnosis and treatment of nasal vestibular tumors from these cases and the related literature.
Keywords: Benign tumor, vestibule of nose, papilloma, trichofolliculoma, pseudoepitheliomatous hyperplasia, verruca vulgaris
Introduction
The nasal vestibule, the most anterior part of the nasal cavity, is lined with keratinizing squamous epithelium and contains different components from the nasal cavity proper such as vibrissae, sebaceous glands, and sweat glands. Pathologic lesions occurring in the nasal vestibule are different from those in the nasal cavity proper, partially due to these histologic differences. Various pathologic forms, including benign and malignant tumors and infectious diseases, can occur in the vestibule. Here, we present four cases with masses in the nasal vestibule; these were diagnosed as squamous papillomas in two cases, trichofolliculoma, and pseudoepitheliomatous hyperplasia with hyperkeratosis.
Methods
We retrospectively reviewed medical records, images, and pathologic findings of four patients with masses in the nasal vestibule; these patients were consecutively treated at our hospital from December, 2006 to February, 2013. Three patients were males and one was female. The ages of the patients ranged from 15 to 68 years.
Results
Case 1
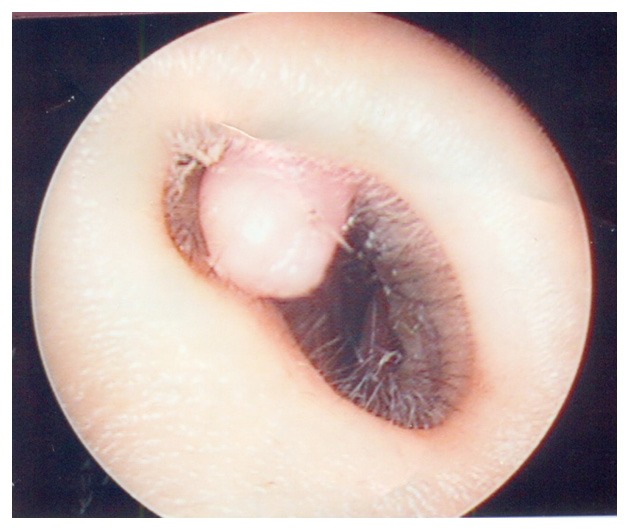
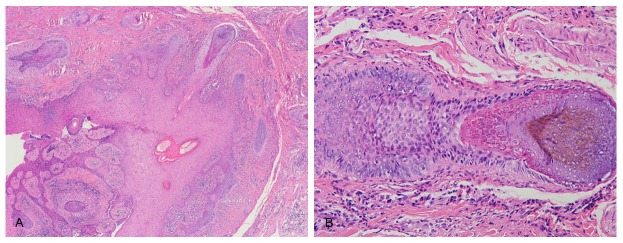
A 47-year-old man who had complained of mild discomfort in the right nasal cavity for 5 months was referred to our department. An endoscopic examination revealed a 1.0 × 1.0 cm sized, brownish, irregular shaped, multinodular mass in the right nasal vestibule (Figure 1). He was an HBV carrier. An excisional biopsy was performed under local anesthesia; the lesion was excised in a full thickness manner with an elliptical incision and narrow margins of normal tissue. Histopathologic sections showed branching exophytic proliferations of well-differentiated stratified squamous epithelium with vascular cores (Figure 2). No invasion into the dermis or mitosis was noted. The histopathologic diagnosis was squamous papilloma. The lesion rec-urred 11 weeks after the excision. Surgical excision was performed again, but the lesion was recurred repeatedly. Surgical excision was performed 4 times in total, over 23 weeks, resulting in recurrence with a six-week interval. We referred the patient to the dermatology department to undergo cryotherapy. He underwent cryotherapy 4 times, once a week. Although the size of the mass was decreased, it still remained. A 5th surgical excision was performed after the 4 cryotherapy treatments. The disease showed no recurrence during a subsequent 10-month follow-up period.
Figure 1.
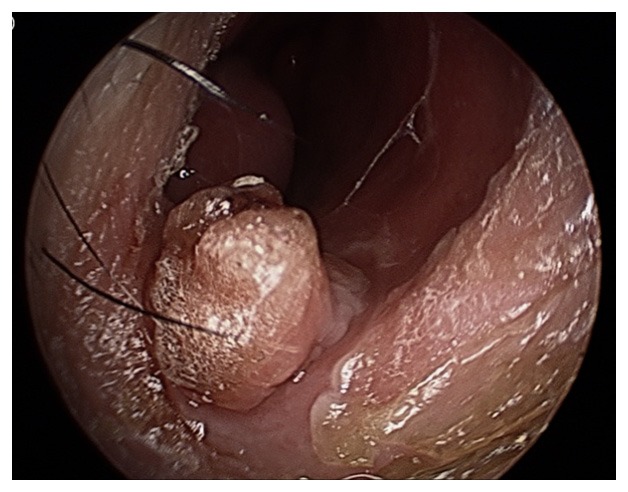
Preoperative endoscopic view of the right nasal cavity of case 1. It shows a 1.0 × 1.0 cm sized, multinodular mass attached to the floor ofthe nasal vestibule.
Figure 2.
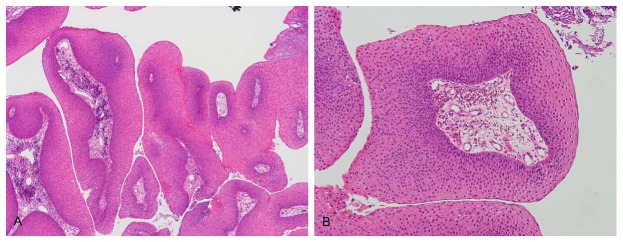
Histopathologic findings of case 1. They showexophytic proliferation of well-differentiated stratified squamous epithelium with vascular cores (H & E; A × 40, B × 100).
Case 2
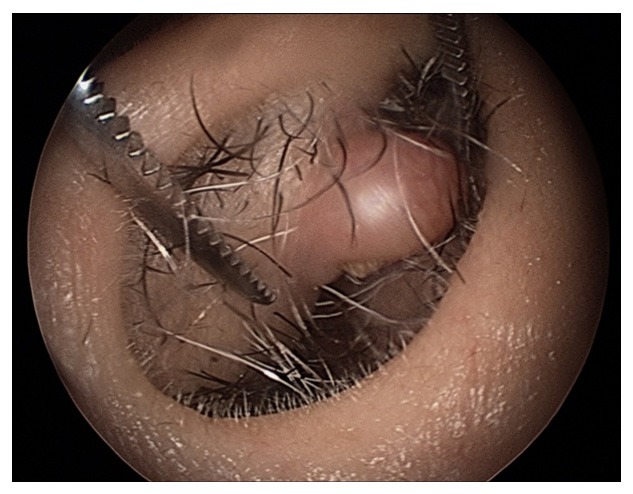
A 15-year-old male was referred to our department with a two-week history of a mass in the left nasal vestibule. He had undergone tonsillectomy and adenoidectomy at our department 10 years previously without any further particular history of illness. Endoscopic examination revealed multiple verrucous-surfaced papules of various sizes in the right nasal vestibule (Figure 3). The wide spreading lesion made surgical excision difficult to consider. A CO2 laser treatment was selected as an appropriate treatment. The patient was referred to the dermatology department. The patient underwent CO2 laser treatment using a topical anesthetic cream three times over a seven week period. At the last follow up, no residual lesions were evident. No recurrence of the disease was noted during a six-month follow-up period. Histop-athologic study was not performed due to lack of surgical specimens. The patient was diagnosed clinically with verruca vulgaris.
Figure 3.

Preoperative endoscopic view of the left nasal cavity of case 2. It shows multiple, verrucous-surfaced papule attached circumferentially to the caudal surface of the nasal vestibule.
Case 3
A 68-year-old man was referred to our department with a two-week history of a mass in the right nasal vestibule. He had no particular history of illness. Endoscopic examination reve-aled a 0.5 × 0.8 cm sized, skin-colored, smooth-surfaced, firm, polypoid mass in the right nasal vestibule (Figure 4). An excisional biopsy was performed under local anesthesia. The lesion was excised in a full thickness with narrow margins of normal tissue. No recurrence of the disease was noted during a 12-month follow-up period. Histopathologic sections showed str-ands of thin, markedly elongated, anastomosing epithelium and a heavy infiltration of inflammatory cells in the dermis, as well as varying degrees of hyperkeratosis (Figure 5). The histopathologic diagnosis was pseudoepitheliomatous hyperplasia with hyperkeratosis.
Figure 4.
Preoperative endoscopic view of the right nasal cavity of case 3. It shows a 0.5 × 0.8 cm sized, round, smooth-surfaced, protrudingmass attached to the lateral nasal vestibule.
Figure 5.
Histopathologic findings of case 3. Prominent epidermal hyperplasia is apparent, with strands of thin, markedly elongated, anastomosing epithelium diving into the dermis, and heavy infiltration of inflammatory cells in dermis, as well as varying degrees of hyperkeratosis. Nuclear atypia and mitotic figures are absent (H & E; A × 40, B × 200).
Case 4
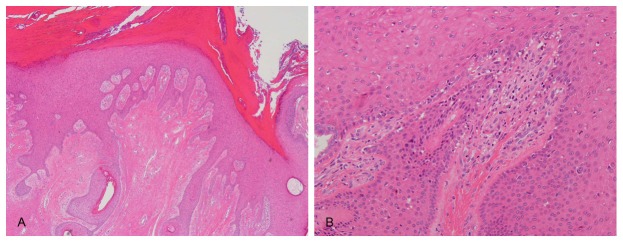
A 45-year-old woman was referred to our department with a one-year history of a growing mass in the left nasal vestibule. She had a past history of allergic rhinitis without any other particular history of illness. An endoscopic examination revealed a 0.8 × 0.5 cm sized, skin-colored, smooth-surfaced, firm, polypoid mass in the right nasal vestibule (Figure 6). Excisional biopsy was performed under local anesthesia. The lesion was excised in a full thickness with narrow margins of normal tissue. No recurrence of the disease was noted during a six-month follow-up period. Histopathologic sections showed a dilated follicular lesion containing hairs. A very incomplete follicular structure branched out from the central cavity (Figure 7). The histopathologic diagnosis was trichofolliculoma.
Figure 6.
Preoperative endoscopic view of the left nasal cavity of case 4. It shows a 0.5 × 0.8 cm sized, round, smooth-surfaced, protrudingmass attached to the superior surface of the nasal vestibule.
Figure 7.
Histopathologicfindings of case 4. A dilated follicular lesion containing hairs is apparent. A very incomplete follicular structure branches out from the central cavity (H & E; A × 40, B × 200).
Discussion
The nasal vestibule contains hair follicles, sebaceous glands, and sweat glands. The internal nasal lining of the vestibule consists of squamous epithelium and changes to pseudostratified ciliated columnar respiratory epithelium with abundant seromucinous glands within the proper nasal cavity. Disease entities occurring in the nasal vestibule and the sinonasal cavity differ, partly due to the differences in the lining epithelium and the adnexa. Various types of diseases, including inflammatory and infectious diseases and benign and malignant tumors, can arise in the nasal vestibule. These vestibular lesions can cause various symptoms such as unilateral nasal obstruction, pain, crusting, and epistaxis; usually these symptoms are nonspecific. This lack of specific signs and/or symptoms means that laboratory and pathologic studies are almost always mandatory for the diagnosis. Complete surgical excision is even more important for some benign tumors, which may have malignant potential.
In the present study, 3 different types of benign tumor were confirmed pathologically: squamous papilloma, trichofolliculoma, and pseudoepitheliomatous hyperplasia. In one case, the lesion attachment area was so wide that CO2 laser evaporation was done without obtaining a pathologic specimen; this case was clinically diagnosed as verruca vulgaris.
The squamous papilloma depicted here is identical to verruca vulgaris. Verruca vulgaris, commonly known as a common wart, is one of the most recognizable skin growths and is a benign squamoproliferative lesion caused by human papilloma virus types 1, 2, and 4 [1,2]. It can occur on any epidermal surface of the body but is seen most frequently on the hands and knees. Most have a benign clinical course and are likely to resolve spontaneously in immunocompetent patients. Warts are widespread in the worldwide population. Although the frequency is unknown, warts are estimated to affect approximately 7-12% of the population [3]. In school-aged children, the prevalence is 10-20% [4]. Warts can occur at any age but generally occur during childhood and adolescence. An increased frequency is also seen among immunosuppressed patients and meat handlers. Common warts are usually asymptomatic, but they may cause cosmetic disfigurement or tenderness depending on the site. Multiple modalities are available for the treatment of warts, but none is uniformly effective [5-7]. Various types of warts at various sites may need different treatments. Topical agents, intralesional injections, photodynamic therapy, and systemic agents are possible medical treatment options. Surgical treatment options are cryosurgery, lasers, and electrodesiccation/ curettage. According to guidelines of the British Association of Dermatologists, the recommended treatments for cutaneous facial warts are salicylic acid ointment, cryotherapy, curettage with light cautery, and CO2 laser [8]. The use of salicylic acid and surgical excision on facial warts should be considered carefully because of the risk of severe irritation and possible scarring. The use of cryotherapy also has restrictions because it can cause hypo- and hyperpigmentation. When choosing the proper surgical option, we considered the area and the site to which the mass attached. We chose surgical excision and cryotherapy for the first case, where the area was relatively small, and CO2 laser for the second case although it could also cause scarring. Transformation from a common wart to a squamous cell carcinoma is very exceptional but has been reported in a renal transplant recipient [9].
Squamous papilloma or verruca vulgaris in the nasal vestibule must be distinguished from Schneiderian papilloma, which occurs in the ciliated respiratory mucosa that lines the sinonasal tract, the so-called Schneiderian membrane. Schneiderian papillomas are classified into three morphologically distinct papillomas: fungiform, inverted, and oncocytic [10]. In contrast to squamous papilloma, where the squamous epithelium proliferates, a Schneiderian papilloma is a tumor of the respiratory epithelium although squamous metaplasia is common. In contrast to a squamous papilloma, the fungiform and inverted papillomas have malignant potential [10]. The fungiform papilloma tends to arise on the nasal septum and is exophytic. The inverted papilloma tends to occur on the lateral nasal wall. Complete surgical excision is the treatment of choice.
Pseudoepitheliomatous hyperplasia (PEH) is a benign condition that is characterized by reactive proliferation of the epidermal and adnexal epithelium. On physical examination, PEH app-ears as a well-demarcated plaque or nodule with variable degrees of scarring and crusting. Ulceration may be present. Microscopically, PEH consists of elongated, thick downward projections of the epidermis into the dermis. These findings make complicate the differentiation of PEH from squamous cell carcinoma (SCC) [11]. This reactive disease has been known to occur in response to various underlying diseases including infectious, neoplastic, and inflammatory entities. The lack of nuclear atypia and mitotic figures, and identifying the associated conditions, is usually helpful in establishing the diagnosis of PEH [11]. Histologically, we diagnosed the present case as PEH due to the lack of findings such as nuclear atypia and mitosis even though no associated infectious, neoplastic, or inflammatory conditions were present.
Trichofolliculoma is one of a few hair follicle tumors that usually feature hair follicle tissue; this typically occurs on the faces of adults [12]. Epidemiologically, trichofolliculoma is associated with minimal clinical morbidity; no confirmed cases of malignant transformation or clinical mortality are reported in the literature. The typical lesion is a single, flesh-colored, firm nodule or papule on the face of an adult, with a wisp of white hair emerging from a central pit. Micro-scopically, the lesion contains a dilated follicle or cystic lesion lined by infundibular, stratified squamous epithelium and opening to the skin surface, and the lesion contains hairs [13]. Branching out from the central cavity are many incomplete follicular structures. When many sebaceous glands are present, one can diagnose folliculosebaceous cystic hamartoma. The treatment of choice is surgical excision [13]. To the best of our knowledge, trichofolliculoma has not been previously reported in the nasal vestibule.
Correct diagnosis is important for optimal treatment. Benign lesions in particular must be differentiated from malignancies. Because the depth of epithelial infiltration, in addition to nuclear atypia and mitosis, is important for distinguishing between benign and malignant lesions, obtaining an adequate specimen is necessary. In addition, immunohistochemistry and clinicopathological communication are of paramount importance.
The nasal vestibule is structurally supported by only cartilage (septal and lower lateral cartilages) and fibrous tissue. Therefore, it is vulnerable to scarring, although maintaining the integrity of the nasal vestibule is important both functionally and cosmetically. When deciding on a treatment option for a nasal vestibular mass, this feature of the nasal vestibule as well as the disease entity should be considered. When the excision is difficult to perform anatomically, the CO2 laser is a preferred method if it is not contraindicated. Laser therapy can protect the adjacent areas, and guarantee optimal reepithelialization; therefore, less scar tissue forms than with surgical excision. One of the present cases showed recurrence despite repeated surgical excision. According to past research, no single treatment is 100% effective. Different strategies can be combined for complete treatment of the lesion. We suggest that a combination of surgical excision and cryotherapy is a possible treatment option for a recurrent mass in the nasal cavity.
A multidisciplinary approach that combines otolaryngology, dermatology, and plastic surgery in a case of reconstruction can provide optimal care for the patient with a nasal vestibular mass.
Conclusion
The nasal vestibule is lined with squamous epithelium; consequently, the pathologic entities occurring in it are quite different from those found in the remainder of the sinonasal cavity. The treatment modality for a nasal vestibular mass should be tailored to the area and site of the lesion as well as to the disease per se. For the correct diagnosis and corresponding optimal treatment of a vestibular mass, an interdisciplinary approach can be of paramount importance.
Disclosure of conflict of interest
All authors have no conflict of interest.
References
- 1.Cardoso JC, Calonje E. Cutaneous manifestations of human papillomaviruses: a review. Acta Dermatovenerol Alp Panonica Adriat. 2011;20:145–154. [PubMed] [Google Scholar]
- 2.Evans DA. Squamous papilloma of the nasal vestibule. Otolaryngol Head Neck Surg. 1994;110:605–606. doi: 10.1177/019459989411000625. [DOI] [PubMed] [Google Scholar]
- 3.Beutner KR, Becker TM, Stone KM. Epidemiology of human papillomavirus infections. Dermatol Clin. 1991;9:211–218. [PubMed] [Google Scholar]
- 4.van Haalen FM, Bruggink SC, Gussekloo J, Assendelft WJ, Eekhof JA. Warts in primary schoolchildren: prevalence and relation with environmental factors. Br J Dermatol. 2009;161:148–152. doi: 10.1111/j.1365-2133.2009.09160.x. [DOI] [PubMed] [Google Scholar]
- 5.Dall’oglio F, D’Amico V, Nasca MR, Micali G. Treatment of cutaneous warts: an evidence-based review. Am J Clin Dermatol. 2012;13:73–96. doi: 10.2165/11594610-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Goldfarb MT, Gupta AK, Gupta MA, Sawchuk WS. Office therapy for human papillomavirus infection in nongenital sites. Dermatol Clin. 1991;9:287–296. [PubMed] [Google Scholar]
- 7.Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;9:CD001781. doi: 10.1002/14651858.CD001781.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sterling JC, Handfield-Jones S, Hudson PM. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001;144:4–11. doi: 10.1046/j.1365-2133.2001.04066.x. [DOI] [PubMed] [Google Scholar]
- 9.Noel JC, Detremmerie O, Peny MO, Candaele M, Verhest A, Heenen M, De Dobbeleer G. Transformation of common warts into squamous cell carcinoma on sun-exposed areas in an immunosuppressed patient. Dermatology. 1994;189:308–311. doi: 10.1159/000246869. [DOI] [PubMed] [Google Scholar]
- 10.Vorasubin N, Vira D, Suh JD, Bhuta S, Wang MB. Schneiderian papillomas: Comparative review of exophytic, oncocytic, and inverted types. Am J Rhinol Allergy. 2013;27:287–292. doi: 10.2500/ajra.2013.27.3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165–175. doi: 10.1097/DAD.0b013e31821816ab. [DOI] [PubMed] [Google Scholar]
- 12.Kligman AM, Pinkus H. The histogenesis of nevoid tumors of the skin. The folliculoma–a hair-follicle tumor. Arch Dermatol. 1960;81:922–930. doi: 10.1001/archderm.1960.03730060038007. [DOI] [PubMed] [Google Scholar]
- 13.Misago N, Kimura T, Toda S, Mori T, Narisawa Y. A revaluation of trichofolliculoma: the histopathological and immunohistochemical features. Am J Dermatopathol. 2010;32:35–43. doi: 10.1097/DAD.0b013e3181a77414. [DOI] [PubMed] [Google Scholar]


