Abstract
Aims: To evaluate the expression of αv-series integrins in brain metastases. Inhibitors targeting these integrins are being tested for their therapeutic potential. Material and Method: The extracellular regions of the αvβ3, αvβ5, αvβ6, αvβ8, the cytoplasmic domain of β3, the αv-chain, and the ECM molecules fibronectin and fibrinogen were studied immunohistochemically in a series of 122 carcinoma and 60 melanomas metastatic to the central nervous system. In addition, 38 matched primary and metastatic tumors to the brain were compared directly. Results: The αv-subunit was generally moderately to highly expressed in most tumors. αvβ3 and cytoplasmic β3 were weakly to moderately detectable in metastatic renal cell carcinomas and melanomas, αvβ5 was prominently expressed in metastatic renal and colorectal carcinomas, αvβ6 was most abundantly detectable in metastatic lung adenocarcinomas, but absent in melanomas. The tumor associated vessels in CNS metastases consistently expressed αvβ3, αvβ5, αv-, fibronectin and fibrinogen, however, mostly at low levels, while αvβ6, αvβ8 were lacking in vasculature. The comparative analysis of 38 matched primary tumors and brain metastases showed comparable levels of expression only for αvβ3 and αvβ8, while αvβ6 and αvβ5 were higher in primaries. Conclusion: We confirmed that integrin expression exhibits considerable heterogeneity according to tumor origin. αvβ5 is the most promising target for integrin targeted treatment in brain metastases.
Keywords: Integrins, metastases, prognosis, alphav
Introduction
Brain metastases are tumors that originate outside the central nervous system and after initial local growth spread secondarily via blood vessels (hematogenous dissemination) [1]. Metastases are the most common brain tumors, with incidence up to 11 per 100.000 population per year. Some 25% of cancer victims present brain metastases at autopsy [2]. The most common tumor origin of the brain metastases is lung, followed by carcinomas of the breast and genitourinary tract. Treatment for brain metastases is primarily palliative, with the goals of therapy being reduction of symptoms and prolongation of life. Prognosis is usually very poor [3]. Patients with brain metastases survive 2.3-7.1 months on average, depending on tumor location, and the patients’ age and Karnofsky status [4].
Extracellular matrix (ECM) proteins are involved in tissue morphogenesis and tumor metastasis [5]. In coordination with the integrin family of ECM receptor present as heterodimers on the cell surface, they regulate adhesion, growth, cell movement, and survival. Alterations in integrin expression accompany and may contribute to the ability of cancer cells to cross physiological barriers in their tissue of origin and allow them to invade other structures [6]. Of interest here are the αv integrin subfamily, which has five members αvβ1, αvβ3, αvβ5, αvβ6 and αvβ8. The αv family binds ECM components of the provisional ECM containing Arginine-Glycine-Aspartic Acid attachment sites (eg. vitronectin, fibronectin, osteopontin and fibrinogen) [7] and αvβ6 and αvβ8 have also been associated with the local activation of pre TGFbeta [8]. Especial-ly αvβ3 and αvβ5 integrins, which are frequently expressed in tumor endothelia and in some tumor cells, may affect tumor initiation and progression [9], while in lung cancer αvβ3 and αvβ6 can bind ligands such as osteopontin and fibronectin [9]. Tumor progression in colorectal cancer can apparently be promoted through αvβ6-mediated activation of TGF-beta [10]. In pancreatic ductal adenocarcinoma αvβ6 is upregulated compared to normal ducts [11].
New treatment modalities against integrin subunits are being developed and integrin ligands are also being exploited as diagnostic probes [12,13], however, the analysis of integrins in tissues has been hampered by lack of antibodies suitable for use in paraffin embedded material. Recently one of us (SLG) has generated monoclonal antibodies against alpha-v integrin complexed to beta3, beta5, beta6 and beta8 in paraffin embedded archival tissue [14] and these have been successfully used to analyze brain tumors [15]. We used these antibodies to investigate integrin expression in a series of formalin-fixed, paraffin-embedded brain metastases from lung, breast, kidney and prostate, from melanomas and from some other rare carcinomas. In a subset we compared this expression profile to that in the primary tumors of origin.
Materials and methods
Antibody generation
Matched recombinant rabbit monoclonal antibodies (RabMabs) directed against intact extracellular domains of human αvβ3, αvβ5, αvβ6, αvβ8, complexes, of the common αv and the β3-cytoplasmic domain (detailed overview: Table 1) were generated and characterized as described previously [14]. Antibodies for the ligands fibronectin and fibrinogen were obtained commercially (for supplier see Table 1).
Table 1.
Overview of antibodies used in this study
| Antibody | Clone, species | Dilution (concentration) | Pretreatment, Primary antibody incubation time (Duration) | Source |
|---|---|---|---|---|
| αvβ3 | EM227-03, rabbit | 1:500 (2 μg/ml) | Protease 12 min (0.1 U/ml), 32 min | Research reagent, [14] |
| Cytoβ3 | EM002-12, rabbit | 1:500 (2 μg/ml) | SCC1, 32 min + amplification | Research reagent, [14] |
| αvβ5 | EM099-02, rabbit | 1:800 (1.25 μg/ml) | Protease 12 min (0.1 U/ml), 32 min | Research reagent, [14] |
| αvβ6 | EM052-01, rabbit | 1:1000 (1 μg/ml) | Protease 12 min (0.1 U/ml), 32 min | Research reagent, [14] |
| αvβ8 | EM133-09, rabbit | 1:1000 (1 μg/ml) | Protease 12 min (0.1 U/ml), 32 min | Research reagent, [14] |
| αv- | EM013-09, rabbit | 1:1000 (1 μg/ml) | SCC1, 32 min | Research reagent, [14] |
| Fibronectin | 568, mouse | 1:100 (not supplied) | Trypsin 30 min, (0.2 g), 32 min | Novocastra, Newcastle UK |
| Fibrinogen | 1F2, mouse | 1:1000 (10 μg/ml) | SCC1, 32 min | AbD Serotec, Düsseldorf |
| IgG | IgG1 isotype control | 1:500 (2 μg/ml) | Pretreatment, Primary antibody incubation time (Duration) | Genetex, San Antonio, TX, USA |
Tissue samples
Tumor samples were retrieved from the archives of Neuropathology at the Department of Path-ology and Neuropathology Tübingen and consisted of 182 tumors of which 175 were brain metastases and 7 intramedullary spinal cord metastases. In 38 cases, the matched primary tumor of origin was available (see Table 2). Tissue selection was performed according to the ethical guidelines of the University of Tuebingen using a protocol approved by the ethics committee (Permission number: 249/2010BO1). Histopathological designation and grading were done by at least two pathologists. Cases with divergent diagnoses and extradural location were not included. Details on these cases are shown in Table 2. Tumors were available as tissue microarrays (in 98 cases, two 1000 μm-diameter representative tissue punches from each tumor) and as full slides (in 84 cases, including all tumor primaries). The blocks were cut with a microtome (4 mM thick sections) and placed on SuperFrost Plus slides (Microm International, Walldorf, Germany) for histochemistry.
Table 2.
Epidemiological data on tumor samples used in this study
| Tumor | N (metastatic tumors) | N (primary tumors) | N (spinal metastases) | N (female/male) | Mean age (range) |
|---|---|---|---|---|---|
| lung | 50 | 10 | 1 | 16/34 | 59 (34-80) |
| breast | 23 | 9 | 1 | 23/0 | 55 (34-77) |
| colorectal | 13 | 4 | 2 | 7/6 | 63 (32-79) |
| prostate | 10 | 0 | 0 | 0/10 | 65 (50-79) |
| kidney | 9 | 3 | 0 | 3/6 | 61 (44-73) |
| melanoma | 60 | 0 | 0 | 17/43 | 57 (18-86) |
| Other* | 12 | 12 | 3 | 4/8 | 62 (34-80) |
| CUP** | 5 | 0 | 0 | 0/5 | 72 (67-77) |
Other tumors (N = 12): 2 thyroid gland carcinoma, 1 testicular embryonal carcinoma, 1 cholangiocellular carcinoma of the liver, 1 ovarian serous carcinoma, 2 urothelial carcinoma of urinary bladder, 1 laryngeal squamous cell carcinoma 1 esophageal and 1 gastric adenocarcinoma, and 2 sinonasal adenocarcinomas of paranasal cavity.
CUP: Cancer of unknown primary.
Immunohistochemistry
After deparaffinization stains were performed on formalin-fixed paraffin embedded full-slide tissue sections and microarrays on an automated immunohistochemistry system (Ventana Benchmark, Roche, Strasbourg, France), [14,15]. This system uses an indirect biotin-avidin system and an universal biotinylated immunoglobulin secondary antibody and diaminobenzidine as chromogen. To enhance signal strength, tissue sections were incubated with a copper enhancer (Ventana) and counterstained with haematoxylin. Protocols details are summarized in Table 1. Positive controls as previously established [14] included normal kidney for αvβ3, αvβ5 and cytoβ3, HT-29 colon carcinoma cell line for αvβ6, human CNS for αvβ8 and normal colon tissue for the αv-chain. Positive controls for fibronectin and fibrinogen included clear-cell renal carcinoma and glioblastoma samples [15]. Negative control slides were processed in parallel with each batch of staining by replacing the primary antibody with the appropriate rabbit or murine polyclonal IgG isotype control (Genetex, San Antonio, TX, USA) at the same concentrations of IgG primary antibodies.
Data analysis and statistical evaluation
Stained slides (both full slides and TMA cores) were scored manually as described previously [15]. Expression of integrins in vessels was semi-quantitatively recorded as: 0 (staining absent), 1 (staining in less than 50% of vessels) and 2 (staining in 50% or more vessels). Cytoplasmic and membranous expression in epithelial tumor cells was recorded together as staining intensity (SI): 0 (absent), 1+ (weak expression), 2+ (moderate expression) and 3+ (strong expression). In addition the number of epithelial and stromal cells with integrin staining in tumors (parenchymal positivity, PP) was evaluated using a semi-quantitative score as 0 (no staining, < 1% positive cells), 1 (1-24.9% positive cells), 2 (25-49.9%), 3 (50-74.9%), 4 (75–100%). A calculated immunoreactive (“IRS”) score was generated by multiplying staining intensity score of tumor epithelial cells by the score of positive cells (IRS = SI x PP: range 0-12). In addition to this manual evaluation, stained TMA slides were scanned with a digital camera (Sony, DFWX710, Japan) using the Mirax Scan software package (Zeiss, Goettingen, Germany) suite. Digitalized data were transferred to a workstation (Definiens Tissue Studio, Munich, Germany). After selecting randomly four tumor regions (size of the window was determined by the software) on the digitalized TMA punches to be used for software training, staining thresholds for nucleus detection and quantitative membrane and cytoplasmic intensity were adjusted on the four selected subsets at 20 x magnification of the scanned TMA punch area until the software test runs successfully recognized the nuclei and the calculated antibody staining intensity matched the pathologists’ assessment from manual analysis. The subsets were selected according to their overall staining (strong, moderate, weak or absent staining). The histoscore was calculated on the basis of the formula ([percentage weak staining cells x 1] + [percentage moderately stained cells x 2] + [percentage strongly stained cells x 3] = histoscore. Possible range: 0-300) which expresses precisely the overall expression in a weighted manner. Processed results were exported to the statistical analysis software JMP (SAS Institute, Cary, NJ, USA).
Clinical data (Patient age, sex and tumor location) were retrieved from medical files. Statistical analysis included ANOVA for staining intensity (comparing cells expressing low, moderate and high staining intensity), semiquantitative scoring of the number of parenchymal positive tumor cells, calculated immunoreactive score and vessel scoring. Logistic regression was used for comparing integrin expression with patient age and ANOVA, followed by Student’s-t test for patients’ sex and tumor location. Matched pairs analysis was used for analyzing comparative expression between metastases and primary tumors. Logistic fit was used for correlation between manual (calculated immunoreactive score) and automated evaluation (calculated histoscore). In addition multivariate regression was performed for correlation of expression of each integrin (based on calculated histoscore data).
Results
Staining patterns of integrin complexes in tumors examined
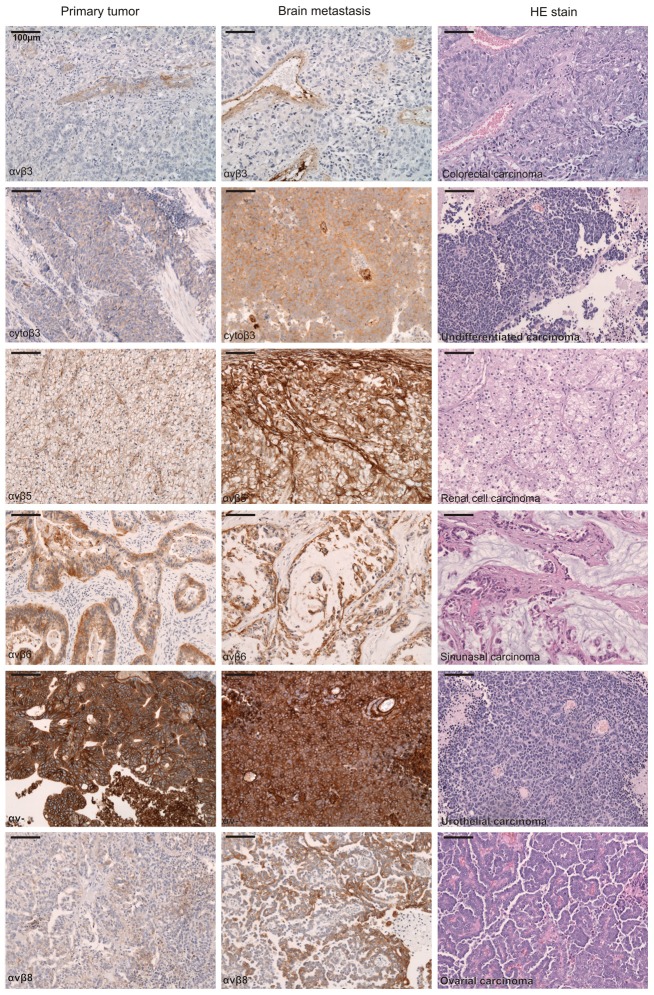
Positive integrin immunostaining in all tumors examined was both membranous and cytoplasmic (for primaries and metastases). Memb-ranous αvβ5 and αvβ6 immunoreactivity was usually more prominent than cytoplasmic staining, while for αvβ8, αv- and fibronectin membranous and cytoplasmic staining was similar (Figure 1). αvβ8 and, with very few exceptions, αvβ6 staining were not found in tumor vessels, while immunoreactivity of αvβ5, αv-, fibrinogen and fibronectin was also observed in tumor vessels. αvβ3 and cytoplasmic β3 was mainly detectable in vessels, however some tumor cells exhibited a weak additional cytoplasmic β3 staining (see Figure 1). No nuclear staining for integrins was observed. Immunoreactivity in tumor stroma was especially prominent for αvβ5 and present for αv-, while the tumor stroma was generally negative for αvβ3, αvβ6, αvβ8 and the cytoplasmic beta3. Staining intensity of tumor stroma and tumor cells was often similar for fibrinogen and fibronectin (Figure 2).
Figure 1.
Immunohistochemistry of integrin expression (brown color) in primary tumor (first column) and its metastases to the brain (middle column). The third (left) column carries tumor designation and shows a representative HE staining.
Figure 2.
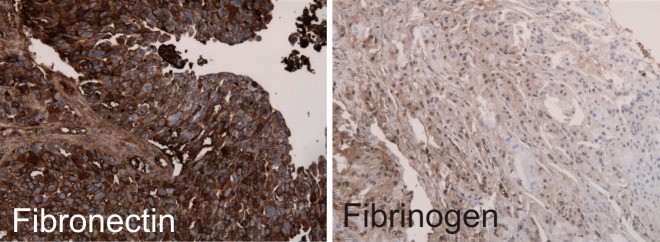
Representative Immunohistochemistry of integrin ligands in brain metastases of adenocarcinomas of unknown primary (CUP) showing a strong expression of fibronectin and focal weak expression of Fibrinogen.
Manual evaluation of integrin expression
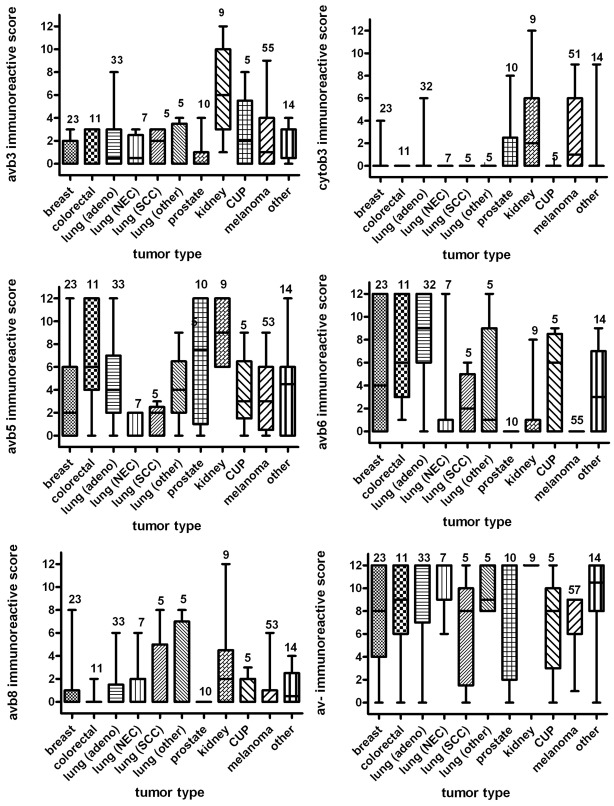
Means and standard deviations of the quantitative immunoreactivity, the staining intensity and combined IRS results for each integrin complex in 122 carcinomas and 60 melanomas metastatic to CNS grouped according to their histology are shown in Table 3. In general, the αv-subunit was most prominently stained in carcinoma and melanoma tumor cells. While αvβ5 and αvβ6 were high and αvβ3 low immunoreactive in adenocarcinomas, the opposite pattern was observed in clear cell carcinomas. Squamous cell and small cell carcinomas predominantly stained for αvβ6, while melanoma cells were immunoreactive for αvβ3 and αvβ5. αvβ8 was rarely seen in epithelial and melanocytic tumors.
Table 3.
Mean and SD values for the combined immunoreactive score (IRS), staining intensity and quantitative scoring from manual analysis of 122 brain carcinoma and 60 melanoma metastases grouped according histology
| Integrin complex/ligand | Adeno Mean IRS | Adeno SD IRS | Clear Cell Mean IRS | Clear Cell SD IRS | Squamous Cell Mean IRS | Squamous Cell SD IRS |
|
| ||||||
| αvβ3 | 1.44 | 2.12 | 5.12 | 4.08 | 1.66 | 1.33 |
| cytoβ3 | 0.60 | 1.97 | 1.87 | 2.64 | 0.0 | 0.0 |
| αvβ5 | 4.71 | 3.91 | 8.0 | 2.97 | 1.16 | 1.39 |
| αvβ6 | 5.81 | 4.73 | 0.37 | 0.51 | 3.56 | 1.45 |
| αvβ8 | 1.11 | 2.26 | 0.87 | 1.24 | 1.83 | 3.12 |
| αv | 8.44 | 4.11 | 11.62 | 1.06 | 6.66 | 4.36 |
| Fibrinogen | 0.60 | 0.92 | 0.50 | 1.06 | 1.33 | 1.03 |
| Fibronectin | 1.04 | 2.13 | 1.25 | 1.38 | 0.66 | 0.81 |
|
| ||||||
| Integrin complex/ligand | Small cell Mean IRS | Small cell SD IRS | Melanoma Mean IRS | Melamoma Cell SD IRS | Undifferentiated Mean IRS | Undifferentiated SD IRS |
|
| ||||||
| αvβ3 | 1.0 | 0.0 | 2.12 | 2.65 | 2.28 | 1.38 |
| cytoβ3 | 0.0 | 1.41 | 2.68 | 3.11 | 0.0 | 0.0 |
| αvβ5 | 0.60 | 0.89 | 3.24 | 2.86 | 2.73 | 1.03 |
| αvβ6 | 2.60 | 5.27 | 0.0 | 0.0 | 4.57 | 4.72 |
| αvβ8 | 0.40 | 0.89 | 0.81 | 1.51 | 2.42 | 2.69 |
| αv | 11.40 | 1.34 | 7.36 | 2.33 | 10.42 | 1.98 |
| Fibrinogen | 0.40 | 0.54 | 1.84 | 2.34 | 0.28 | 0.75 |
| Fibronectin | 0.80 | 1.30 | 0.64 | 1.06 | 1.14 | 1.67 |
Integrin expression profiles in CNS metastases according to tumor origin and histology
Tumors metastases in brain were grouped according to their origin and histological subtype (Table 2). Means and standard deviations of the IRS results are shown in Figure 3. αvβ3 (mean score 6.3; SD 3.9) and cytoplasmic β3 (mean score 3.2; SD 4.0) were weakly to moderately detectable in metastatic renal cell carcinomas only. αvβ5 was most prominently stained in metastatic renal (mean score 8.8; SD 2.6) and colorectal carcinomas (mean score 6.8; SD 3.9). αvβ6 was most abundant seen in metastatic pulmonary adenocarcinomas (mean score 9.0; SD 3.8) and cancer of unknown primary (mean score 7.5; SD 4.27) followed by metastatic colo-rectal (mean score 6.9; SD 3.9) and breast cancers (mean score 5.6; SD 4.9). The αv-subunit was generally highly to moderately immunoreactive in most metastases (mean values from 12 to 6.8). Fibrinogen (mean score 0.6; SD 0.9) and fibronectin (mean score 1.12; SD 2.1) were weakly stained in all CNS metastases.
Figure 3.
Mean immunoreactive scores (IRS) and standard deviation (IRS: 0-12) of αvβ integrin complex expression analyzed in CNS metastases separated for tumor origin.
Manual evaluation integrin expression in tumor vessels of brain metastases
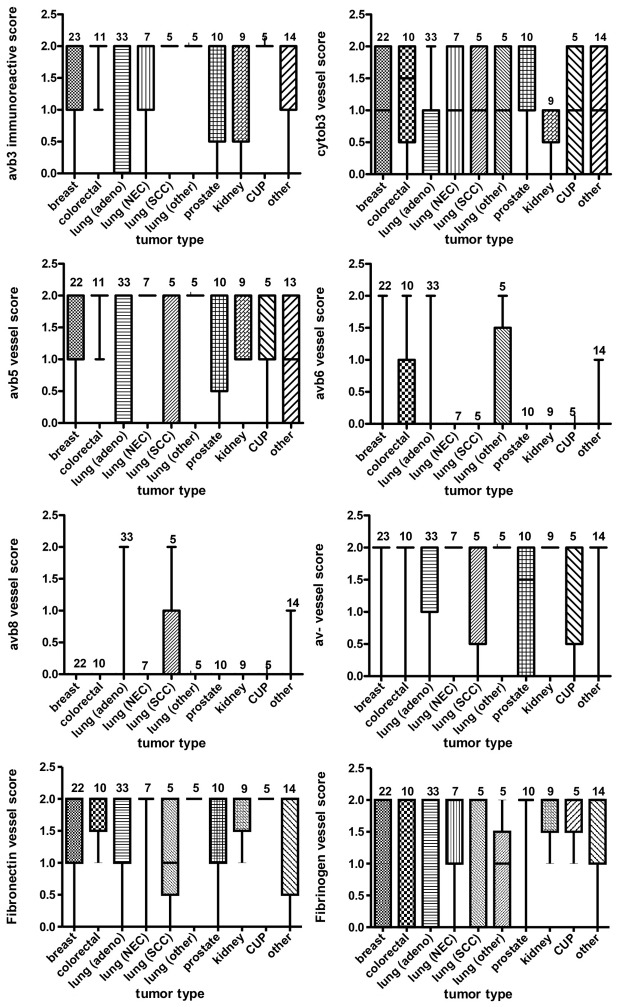
Means and standard deviations of the staining intensity scores in tumor vessels for each integrin complex are shown in Figure 4 (carcinoma n = 120, melanoma n = 39). Analysis of tumor vasculature in carcinoma metastases showed that staining in tumor vessels for αvβ3 (mean: 1.52, SD: 0.7), cytoplasmic β3 (mean: 0.92, SD: 0.8), αvβ5 (mean: 1.30, SD: 0.8), was consistently present, while αvβ8 (mean: 0.03, SD: 0.2) and αvβ6 (mean: 0.2, SD: 0.5) was almost absent in carcinoma tumor vessels. In melanoma metastases vascular αvβ3 (mean: 0.6, SD: 0.71), cytoplasmic β3 expression (mean: 0.73, SD: 0.73) and αvβ5 (mean: 0.8, SD: 0.8) was lower compared to carcinoma, while there was no immunopositivity in vessels for αvβ8 or αvβ6.
Figure 4.
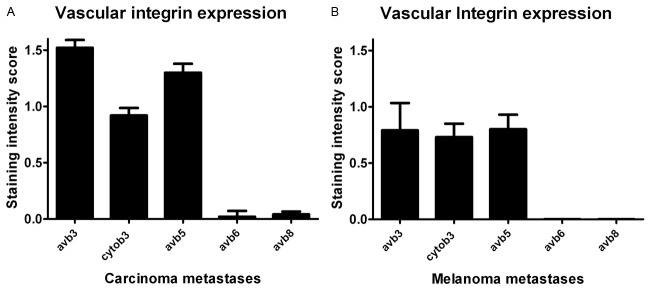
Mean staining intensity scores (manual, scores 0-2) of αvβ integrin complex and ligand expression in vasculature of (A) carcinoma and (B) melanoma metastases.
Means and standard deviations of the staining intensity scores in tumor vessels in histology subgroups are shown in Figure 5. Mean immunoreactive score of αvβ3 in vessels of tumors originating from the intestinal tract (mean: 1.9) were higher than those originating from the respiratory tract (1.3, p = 0.047, Figure 2B). Likewise cytoβ3 immunostaining in vasculature of metastatic lung tumors (mean: 0.68) was significantly lower compared to metastases of prostatic (1.6) and intestinal carcinomas (1.3). αvβ5 immunopositivity in renal (1.6), lung (1.5) and prostatic (1.4) cancer metastases was significantly higher than in metastatic breast cancer (0.7, p = 0.053 to 0.0003). Staining of αvβ6 and αvβ8 was generally weak in tumor vessels and did not differ between the groups. Fibronectin (mean score 1.5; SD 0.7) and fibrinogen (mean: 1.3; SD: 0.8) were weakly to moderately immunopositive in tumor associated vessels.
Figure 5.
Mean staining intensity scores (manual scores 0-2) of αvβ integrin complexes in vasculature of brain carcinoma metastases separated for tumor origin. For combined expression analysis, see Figure 4A.
Comparison of manual staining of primary and metastatic tumors
Matched pairs of primary and their CNS metastatic tumors were available in 38 carcinoma samples. Statis-tical analysis showed that the expression in primary tumor and corresponding metastases were significantly correlated only for αvβ3 (p = 0.0016) and αvβ8 (p = 0.048). No significant correlations were seen for cytoβ3 (p = 0.25), αvβ5 (p = 0.076), αvβ6 (p = 0.27), αv- (p = 0.31), fibrinogen (p = 0.29) or fibronectin (p = 0.78) indicating a different expression between primary tumor and metastases. No significant association was observed in vascular expression of primary and metastatic tumors for αvβ3 (p = 0.15) and αvβ5 (p = 0.61). After separation by tumor origin the matched pair analysis showed significant upregulation in αvβ3 (p = 0.04) and downregulation of αvβ6 (p = 0.0076) in kidney cancer metastases. A significant cytoβ3 upregulation was observed for breast cancer metastases (p = 0.002) and lung cancer metastases (p < 0.001).
Correlation of manual staining results with clinical data
No significant differences of immunoreactive scores (IRS) of carcinoma and melanoma metastases with patients sex was observed for the integrins examined.
In carcinomas there was a decrease of αvβ3, cytoplasmic β3, αvβ5, αvβ6, αvβ8 and αv- IRS values with a age, but results were not statistically significant. In melanoma metastases a significant increase of cytoplasmic β3 (p = 0.043) and αv- (p < 0.0001) with age was observed, while IRS for αvβ3, αvβ5, αvβ6 and αvβ8 remained constant. IRS values were independent of tumor differentiation grade (undifferentiated, moderately differentiated, well differentiated). Mean αvβ3 IRS scores were significant higher in spinal metastases (p = 0.0031, mean: 3.0, SD: 0.7) compared to brain metastases (1.62, SD 2.3), while mean αvβ8 IRS scores in spinal metastases were significant lower (p = 0.0017, mean: 0.2, SD: 0.4) compared to αvβ8 IRS in the brain metastases (mean: 1.18, SD: 2.5). Mean IRS scores for αvβ3, αvβ5 and αvβ6 were not significantly different between brain and spinal metastases.
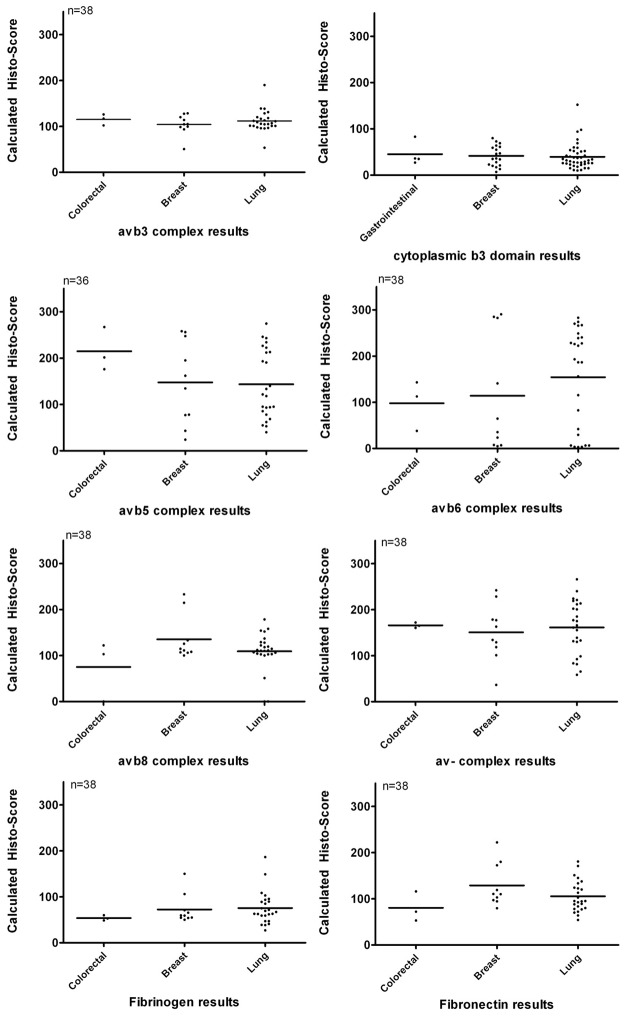
Correlation automatic analysis and manual evaluation
38 carcinoma samples were available as tissue microarray (TMA) and evaluated with the Definiens software package. Results of the calculated histoscores for the integrin complexes are displayed as scatter plots in Figure 6. Logistic fit of manual staining immunoreactive score with calculated histoscore from automated analysis showed significant correlation of manual and automatic analysis for αvβ3 (p = 0.0008), cytoplasmic β3 (p = 0.0153), αvβ8 (p < 0.0001), αvβ6 (p < 0.0001), αvβ5 (p<0.0001), αv- (p < 0.0001), fibrinogen (p = 0.0001) expression, while results for fibronectin (p = 0.285) were not significant. Possible factors influencing diverging results for fibronectin were expression in tumor vessels and necrotic areas which could not be completely excluded from the automatic analysis.
Figure 6.
Scatter plot displaying results of calculated histo-score from automated integrin αvβ analysis separated for tumor origin. N = number of tumors analyzed.
Discussion
This study aimed to characterize integrin expression profile in brain metastases, compared to the primary tumors of origin. While integrins in primary tumors have been already extensively studied, data on integrin expression in CNS metastases and its relationship to the primary tumors is very limited, and based mainly on analysis of frozen tissue samples of breast carcinoma and lung carcinoma metastases [16]. We used newly developed anti-integrin antibodies which are suitable for formalin-fixed paraffin-embedded tissues and investigated a series of carcinomas and melanomas metastatic to the brain and spinal cord. In addition we compared the expression of integrins and ligands in brain metastases and in their primaries in a smaller subset of these tumors.
All antibodies showed a robust and reproducible staining in FFPE tissue, the signal was always unambiguously interpretable. All integrin subunits were found in carcinoma tissues, but showed different expression patterns (membranous, cytoplasmic and in tumor vessels) and levels of expression dependent on tumor origin and tumor histologic type. As with our previous results in gliomas, αvβ6 expression was absent in CNS melanomas [15], while all other integrin complexes and ligands were expressed, with strongest expression of αvβ5. In CNS carcinoma metastases, the expression was strongest for αvβ5, αvβ6 and αv-, whereas expression of αvβ8, αvβ3, cytoplasmic β3, and of fibrinogen and fibronectin was rather weak. αvβ3 and cytoβ3 were restricted in many cases to tumor vessels only. This is in contrast with the overall staining results of brain tumors, where αvβ8 expression was homogeneously strong and αvβ6 was absent [15].
We found negligible expression of integrin αvβ3 in carcinoma metastases in CNS, with the exception of renal carcinoma metastases. There is only one report of αvβ3 being detectable in renal cell carcinoma tumor cells, however this was only in a small series [17]. The potential for αvβ3 integrin expression in renal cancer to promote growth or affect metastatic competence to CNS, is an interesting aspect for future study. It has been shown that αvβ3 expression in breast carcinoma can affect metastasis to brain [36]. In melanomas, tumors with increased αvβ3 expression tend to metastasize predominantly into the brain [18]. Our observation that 62% of CNS melanoma metastases had αvβ3 immunopositive tumor cells supports this notion. In general the distribution of αvβ3 in human tumors is still incompletely characterized. αvβ3 is reported to be overexpressed in glioblastomas (13/15), melanomas (17/31), ovarian cancer (23/31) and renal cell carcinomas (52/65) [16,19-21]. In metastatic tumors, αvβ3 expression has been reported to be upregulated in 47% of lymph node metastases of prostate cancers [22], in 71% of renal cell carcinoma metastases, including CNS metastases [20], in 58% of metastatic melanoma [19]. αvβ3 has been described in 60% breast cancer CNS metastases and in 56% of lung cancer CNS metastases, but we note that the majority of the samples described contained only scattered positive cells [16]. Given the fact, that αvβ3 was detectable only at low levels in most of the CNS carcinomas metastases we have examined; it may not be a general factor for promoting CNS colonization of breast, colorectal, lung and prostate cancers, while high αvβ3 expression in melanomas and renal cell carcinomas probably indicate a functional role in primary tumor parenchyma. Similarly to our results in gliomas, we observed differences in expression between αvβ3 and its cytoplasmic domain β3, that may reflect different affinity of the antibodies or total as opposed to activated / ligated integrin αvβ3 [15].
We recently observed that vascular upregulation of αvβ3 in astrocytomas is associated with shorter survival [15]. In that study we found in general a moderate αvβ3 and cytoβ3 expression in tumor associated vessels in glioblastomas, which is comparable to the vascular expression of these integrins in most brain metastases investigated by us (e.g. melanoma, breast, colorectal and lung cancer), here the upregulation of vascular αvβ3 seems to be a common event in highly malignant primary and secondary CNS neoplasms.
Integrin αvβ5 may influence adhesion of circulating tumor cells to vessel walls [23]. Our findings of high αvβ5 expression in CNS metastases of melanomas, colorectal, prostate, renal and in some lung carcinomas, points to a possible role in extravasation, outgrowth or even vascular cooption of metastatic tumor cells, a phenomenon known in brain metastases [24]. αvβ5 seems to be more widely expressed in human tumors than αvβ3. Expression of αvβ5 has been reported for 69% lymph node metastases of squamous cell carcinomas of the lung, compared to only 10% cases having such immunopositivity for αvβ3 [25]. In oral head and neck squamous cell carcinomas, αvβ5 was more frequently observed than αvβ3 [26]. αvβ5 was reported in colon carcinoma in 50% of the cases [27]. In renal cell carcinoma αvβ5 was found in 4/5 cases and αvβ3 in 4/7 cases [18]. αvβ5 was detected in frozen specimens of 6/7 lung tumors and 3/10 breast tumors metastatic to CNS [16]. There is evidence that αvβ5 has a significant role in tumor progression, which can be blocked by specific inhibitors, e.g. in lung cancer models [29,30]. Blockade inhibits not only angiogenesis, but also inhibited transforming growth factor-β-controlled malignant growth in a glioblastoma model [30]. The αvβ3 and αvβ5 inhibitor cilengitide reduced tumor progression of experimental breast cancer metastases [31].
Vascular αvβ5 has also been reported in previous studies on brain tumors [15,30]. In our CNS metastases, vascular αvβ5 was detectable at similar prevalence as vascular αvβ3.
αvβ6 is an epithelial-specific integrin in cancer, with highest expression levels reported in carcinoma of the liver, pancreas and ovary [32]. In carcinomas, αvβ6 may influence the activation of TGFb1 and 3 [33]. The CNS metastases in our study exhibited considerable heterogeneity of αvβ6 expression. Metastatic lung adenocarcinomas, colorectal carcinomas and some breast carcinomas showed high expression, while αvβ6 was hardly detectable in neuroendocrine lung carcinomas, prostate or renal carcinomas, and was absent in melanomas.
To our knowledge αvβ6 expression in primary kidney and prostate neoplasms has not been previously reported. In primary colorectal carcinomas Yang et al reported αvβ6 in 34% of the cases [34]. We detected αvβ6 in a higher proportion (63%) of metastatic colorectal metastases, but overall αvβ6 in CNS metastases was more weakly immunopositive in metastatic tumors compared to their primary tumors. Arihiro et al reported αvβ6 in 18% of their breast cancer cohort [35], while 69% of our CNS breast metastases were αvβ6 positive. Whether these differences in the αvβ6 expression between primaries and metastatic cancers are of biological significance, should be addressed in further comparative studies.
In most carcinomas, we did not observe expression of αvβ8. Tumors of the kidney expressed αvβ8 but at low levels compared to primary brain tumors [15]. To our knowledge there are no previous reports concerning αvβ8 in carcinomas and melanomas. Our findings indicate that αvβ8 may be an immunohistochemical marker of CNS tumors, but possibly has little significance for the biology of brain metastases.
Brain metastases are routinely operated on in high volume centers, which gather patients from a large catchment area. The primary tumors have been mostly resected in external hospitals. Thus primary tumor tissues are usually not available for research studies. Never-theless we collected 38 carcinoma primaries to our series of CNS metastases. Our results showed unexpectedly, that the expression levels of the αv integrins and some relevant ligands correlated only for αvβ3 and αvβ8 between primary tumors and brain metastases, showing a rather faint association even in these cases. All other integrins and ligands were detected at different levels in primary tumors compared to their metastases. If our still rather small sample of comparative data are representative for the regulation of the integrins in these tumor types, one has to assume that the regulation of integrin expression in metastatic tumor cells is influenced strongly by tumor microenvironment, or that specific competent cohorts disperse from the primary tumor and are selected by the metastatic sites. It remains to be established whether for a given patient, the metastases at each dispersion site will have a similar integrin profile, which would provide a molecular basis for the soil-and-seed hypothesis [37]. If we assess the changes in expression of a particular integrin by tumor origin no clear trends are visible. Some changes appear to be relevant, however, the expression levels are either too low (e.g. cytoβ3 in breast or lung cancers) or the number of cases are small. Therefore such results have to be interpreted with caution. Clearly, larger studies assessing more homogeneous cohorts and potentially, metastases to different sites are needed. Currently, several integrin inhibitors are under clinical development, and promising results have shown in some primary tumors of brain metastases such as melanoma and lung cancer [12,38,39]. As there is a relevant expression of αv- integrins in many human brain metastasis cases, clinical trials investigating the potential of integrin inhibitors for treatment of brain metastases seem warranted.
In summary, there is considerable av-integrin expression in brain metastases, where αvβ5 and αvβ6 are most prominently detectable in carcinomas and αvβ5 and αvβ3 most prominently in melanomas; whereas tumor associated vessels constantly exhibit αvβ3, αvβ5, αv, and the ligands fibrinogen and fibronectin mostly at low levels. Metastatic carcinomas of different subtypes show considerable heterogeneity in their integrin expression profiles. Because the best investigated integrins and ligands were detected at different levels in primary tumor and their CNS metastases, it seems that the tumor microenvironment influences integrin expression on tumors.
Acknowledgements
JS is supported by a grant of the Ludwig-Hiermaier foundation for Applied Cancer Research, Tübingen, Germany. Research antibodies EM227-03, EM002-12, EM099-02, EM052-01, EM133-09 and EM013-09 were kindly provided by Merck KGaA, Darmstadt, Germany. We like to thank Katrin Trautmann for help with additional immunostainings. We acknowledge support by Deutsche Forschungsgemeinschaft and Open Access Publishing Fund of Tuebingen University.
Disclosure of conflict of interest
This study was funded in part by Merck KGaA. Merck KGaA did not influence the selection of the patients, evaluation and acquisition of data, or the academic interpretation of the data set.
References
- 1.Kleinschmidt-DeMasters BK, Lillehei KO, Breeze RE. Neoplasms involving the central nervous system in the older old. Hum Pathol. 2003;34:1137–1147. doi: 10.1016/s0046-8177(03)00427-1. [DOI] [PubMed] [Google Scholar]
- 2.Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005;75:5–14. doi: 10.1007/s11060-004-8093-6. [DOI] [PubMed] [Google Scholar]
- 3.Ray S, Dacosta-Byfield S, Ganguli A, Bonthapally V, Teitelbaum A. Comparative analysis of survival, treatment, cost and resource use among patients newly diagnosed with brain metastasis by initial primary cancer. J Neurooncol. 2013;114:117–125. doi: 10.1007/s11060-013-1160-0. [DOI] [PubMed] [Google Scholar]
- 4.Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997;37:745–51. doi: 10.1016/s0360-3016(96)00619-0. [DOI] [PubMed] [Google Scholar]
- 5.Preusser M, Capper D, Ilhan-Mutlu A, Berghoff AS, Birner P, Bartsch R, Marosi C, Zielinski C, Mehta MP, Winkler F, Wick W, von Deimling A. Brain metastases: pathobiology and emerging targeted therapies. Acta Neuropathol. 2013;123:205–222. doi: 10.1007/s00401-011-0933-9. [DOI] [PubMed] [Google Scholar]
- 6.Caccavari F, Valdembri D, Sandri C, Bussolino F, Serini G. Integrin signaling and lung cancer. Cell Adh Migr. 2010;4:124–129. doi: 10.4161/cam.4.1.10976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hynes RO, Lively JC, McCarty JH, Taverna D, Francis SE, Hodivala-Dilke K, Xiao Q. The diverse roles of integrins and their ligands in angiogenesis. Cold Spring Harb Symp Quant Biol. 2002;67:143–153. doi: 10.1101/sqb.2002.67.143. [DOI] [PubMed] [Google Scholar]
- 8.Sheppard D. Roles of alphav integrins in vascular biology and pulmonary pathology. Curr Opin Cell Biol. 2004;16:552–557. doi: 10.1016/j.ceb.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 9.Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer. 2010;10:9–22. doi: 10.1038/nrc2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bates RC. Colorectal cancer progression: integrin alphavbeta6 and the epithelial-mesenchymal transition (EMT) Cell Cycle. 2005;4:1350–1352. doi: 10.4161/cc.4.10.2053. [DOI] [PubMed] [Google Scholar]
- 11.Sipos B, Hahn D, Carceller A, Piulats J, Hedderich J, Kalthoff H, Goodman SL, Kosmahl M, Klöppel G. Immunohistochemical screening for beta6-integrin subunit expression in adenocarcinomas using a novel monoclonal antibody reveals strong up-regulation in pancreatic ductal adenocarcinomas in vivo and in vitro. Histopathology. 2004;45:226–236. doi: 10.1111/j.1365-2559.2004.01919.x. [DOI] [PubMed] [Google Scholar]
- 12.Goodman SL, Picard M. Integrins as therapeutic targets. Trends Pharmacol Sci. 2012;33:405–412. doi: 10.1016/j.tips.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Gaertner FC, Schwaiger M, Beer AJ. Molecular imaging of αvβ3 expression in cancer patients. Q J Nucl Med Mol Imaging. 2010;54:309–326. [PubMed] [Google Scholar]
- 14.Goodman SL, Grote JH, Wilm C. Matched rabbit monoclonal antibodies against αv-series integrins reveal a novel αvβ3-LIBS epitope, and permit routine staining of archival paraffin samples of human tumors. Bio Open. 2012;1:329–340. doi: 10.1242/bio.2012364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schittenhelm J, Schwab EI, Sperveslage J, Tatagiba M, Meyermann R, Fend F, Goodman SL, Sipos B. Longitudinal Expression Analysis of αv Integrins in Human Gliomas Reveals Upregulation of Integrin αvβ3 as a Negative Prognostic Factor. J Neuropath Exp Neurol. 2013;72:194–210. doi: 10.1097/NEN.0b013e3182851019. [DOI] [PubMed] [Google Scholar]
- 16.Mittelbronn M, Warth A, Meyermann R, Goodman S, Weller M. Expression of integrins αvβ3 and αvβ5 and their ligands in primary and secondary central nervous system neoplasms. Histol Histopathol. 2013;28:749–758. doi: 10.14670/HH-28.749. [DOI] [PubMed] [Google Scholar]
- 17.Küsters B, Westphal JR, Smits D, Ruiter DJ, Wesseling P, Keilholz U, de Waal RM. The pattern of metastasis of human melanoma to the central nervous system is not influenced by integrin alpha(v)beta(3) expression. Int J Cancer. 2001;92:176–180. doi: 10.1002/1097-0215(200102)9999:9999<::aid-ijc1173>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 18.Rabb H, Barroso-Vicens E, Adams R, Pow-Sang J, Ramirez G. Alpha-V/beta-3 and alpha-V/beta-5 integrin distribution in neoplastic kidney. Am J Nephrol. 1996;16:402–408. doi: 10.1159/000169032. [DOI] [PubMed] [Google Scholar]
- 19.Natali PG, Hamby CV, Felding-Habermann B, Liang B, Nicotra MR, Di Filippo F, Giannarelli D, Temponi M, Ferrone S. Clinical significance of alpha(v)beta3 integrin and intercellular adhesion molecule-1 expression in cutaneous malignant melanoma lesions. Cancer Res. 1997;5:1554–1560. [PubMed] [Google Scholar]
- 20.Wechsel HW, Petri E, Feil G, Nelde HJ, Bichler KH, Loesr W. Renal cell carcinoma: immunohistological investigation of expression of the integrin alpha v beta 3. Anticancer Res. 1999;19:1529–1532. [PubMed] [Google Scholar]
- 21.Liapis H, Adler LM, Wick MR, Rader JS. Expression of alpha(v)beta3 integrin is less frequent in ovarian epithelial tumors of low malignant potential in contrast to ovarian carcinomas. Hum Pathol. 1997;28:443–449. doi: 10.1016/s0046-8177(97)90033-2. [DOI] [PubMed] [Google Scholar]
- 22.Pontes-Junior J, Reis ST, Dall’Oglio M, Neves de Oliveira LC, Cury J, Carvalho PA, Ribeiro-Filho LA, Moreira Leite KR, Srougi M. Evaluation of the expression of integrins and cell adhesion molecules through tissue microarray in lymph node metastases of prostate cancer. J Carcinog. 2009;8:3. doi: 10.4103/1477-3163.48453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Enns A, Korb T, Schlüter K, Gassmann P, Spiegel HU, Senninger N, Mitjans F, Haier J. Alphavbeta5-integrins mediate early steps of metastasis formation. Eur J Cancer. 2005;41:1065–1072. doi: 10.1016/j.ejca.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 24.Kienast Y, von Baumgarten L, Fuhrmann M, Klinkert WE, Goldbrunner R, Herms J, Winkler F. Real-time imaging reveals the single steps of brain metastasis formation. Nat Med. 2010;16:116–122. doi: 10.1038/nm.2072. [DOI] [PubMed] [Google Scholar]
- 25.Li F, Liu Y, Kan X, Li Y, Liu M, Lu JG. Elevated expression of integrin αv and β5 subunit in laryngeal squamous-cell carcinoma associated with lymphatic metastasis and angiogenesis. Pathol Res Pract. 2013;209:105–109. doi: 10.1016/j.prp.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Fabricius EM, Wildner GP, Kruse-Boitschenko U, Hoffmeister B, Goodman SL, Raguse JD. Immunohistochemical analysis of integrins αvβ3, αvβ5 and α5β1, and their ligands, fibrinogen, fibronectin, osteopontin and vitronectin, in frozen sections of human oral head and neck squamous cell carcinomas. Exp Ther Med. 2011;2:9–19. doi: 10.3892/etm.2010.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burvenich I, Schoonooghe S, Vervoort L, Dumolyn C, Coene E, Vanwalleghem L, Van Huysse J, Praet M, Cuvelier C, Mertens N, De Vos F, Slegers G. Monoclonal antibody 14C5 targets integrin alphavbeta5. Mol Cancer Ther. 2008;7:3771–3779. doi: 10.1158/1535-7163.MCT-08-0600. [DOI] [PubMed] [Google Scholar]
- 28.Ricono JM, Huang M, Barnes LA, Lau SK, Weis SM, Schlaepfer DD, Hanks SK, Cheresh DA. Specific cross-talk between epidermal growth factor receptor and integrin alphavbeta5 promotes carcinoma cell invasion and metastasis. Cancer Res. 2009;69:1383–1391. doi: 10.1158/0008-5472.CAN-08-3612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lau SK, Shields SJ, Murphy EA, Desgrosellier JS, Anand S, Huang M, Kato S, Lim ST, Weis SM, Stupack DG, Schlaepfer DD, Cheresh DA. EGFR-mediated carcinoma cell metastasis mediated by integrin αvβ5 depends on activation of c-Src and cleavage of MUC1. PLoS One. 2012;7:e36753. doi: 10.1371/journal.pone.0036753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roth P, Silginer M, Goodman SL, Hasenbach K, Thies S, Maurer G, Schraml P, Tabatabai G, Moch H, Tritschler I, Weller M. Integrin control of the transforming growth factor-β pathway in glioblastoma. Brain. 2013;136:564–576. doi: 10.1093/brain/aws351. [DOI] [PubMed] [Google Scholar]
- 31.Bäuerle T, Komljenovic D, Merz M, Berger MR, Goodman SL, Semmler W. Cilengitide inhibits progression of experimental breast cancer bone metastases as imaged noninvasively using VCT, MRI and DCE-MRI in a longitudinal in vivo study. Int J Cancer. 2011;128:2453–2462. doi: 10.1002/ijc.25563. [DOI] [PubMed] [Google Scholar]
- 32.Bandyopadhyay A, Raghavan S. Defining the role of integrin alphavbeta6 in cancer. Curr Drug Targets. 2009;10:645–652. doi: 10.2174/138945009788680374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsh D, Dickinson S, Neill GW, Marshall JF, Hart IR, Thomas GJ. alpha vbeta 6 Integrin promotes the invasion of morphoeic basal cell carcinoma through stromal modulation. Cancer Res. 2008;68:3295–3303. doi: 10.1158/0008-5472.CAN-08-0174. [DOI] [PubMed] [Google Scholar]
- 34.Yang GY, Xu KS, Pan ZQ, Zhang ZY, Mi YT, Wang JS, Chen R, Niu J. Integrin alpha v beta 6 mediates the potential for colon cancer cells to colonize in and metastasize to the liver. Cancer Sci. 2008;99:879–887. doi: 10.1111/j.1349-7006.2008.00762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arihiro K, Kaneko M, Fujii S, Inai K, Yokosaki Y. Significance of alpha 9 beta 1 and alpha v beta 6 integrin expression in breast carcinoma. Breast Cancer. 2000;7:19–26. doi: 10.1007/BF02967183. [DOI] [PubMed] [Google Scholar]
- 36.Felding-Habermann B. Integrin adhesion receptors in tumor metastasis. Clin Exp Metastasis. 2003;20:203–213. doi: 10.1023/a:1022983000355. [DOI] [PubMed] [Google Scholar]
- 37.Paget S. The distribution of secondary growths in cancer of the breast. Lancet 1889; 133:571–573. [PubMed] [Google Scholar]
- 38.Manegold C, Vansteenkiste J, Cardenal F, Schuette W, Woll PJ, Ulsperger E, Kerber A, Eckmayr J, von Pawel J. Randomized phase II study of three doses of the integrin inhibitor cilengitide versus docetaxel as second-line treatment for patients with advanced non-small-cell lung cancer. Invest New Drugs. 2013;31:175–182. doi: 10.1007/s10637-012-9842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Day S, Pavlick A, Loquai C, Lawson D, Gutzmer R, Richards J, Schadendorf D, Thompson JA, Gonzalez R, Trefzer U, Mohr P, Ottensmeier C, Chao D, Zhong B, de Boer CJ, Uhlar C, Marshall D, Gore ME, Lang Z, Hait W, Ho P CNTO 95 Investigators. A randomised, phase II study of intetumumab, an anti-alphav-integrin mAb, alone and with dacarbazine in stage IV melanoma. Br J Cancer. 2011;105:346–352. doi: 10.1038/bjc.2011.183. [DOI] [PMC free article] [PubMed] [Google Scholar]