Abstract
Objective
This study was conducted to determine whether residents are receiving enough hepatopancreatobiliary (HPB) training during general surgery residencies to exclude the necessity of pursuing formal fellowships in HPB surgery.
Methods
Trends in HPB surgery training were examined using Accreditation Council for Graduate Medical Education (ACGME) operative log data for the academic years 1999/2000 to 2009/2010.
Results
Of 800 000 HPB operations performed annually in the USA, the proportion of HPB procedures performed by general surgery residents increased from 15% (122 007) to 18% (143 000) between the periods under study. Numbers of pancreatic, liver and biliary procedures performed by graduating general surgery residents increased by 47% (from 8185 to 12 006), 31% (from 7468 to 9765), and 14% (from 106 354 to 121 239), respectively. The mean number of operations undertaken by a graduating resident increased from 8.3 to 11.5 (38% increase) for pancreatic surgeries, from 7.6 to 9.4 (24% increase) for liver surgeries, and from 107.5 to 116.6 (8% increase) for biliary surgeries. Total numbers of complex pancreatic, liver and biliary procedures increased by 91% (from 4768 to 9129) and 24% (from 6649 to 8233), and decreased by 29% (from 6581 to 4648), respectively.
Conclusions
The overall trend shows an increase in the number of HPB procedures undertaken by graduating general surgery residents. The mean number of procedures exceeds ACGME requirements, but falls short of association guidelines. However, certain residents exceed International Hepato-Pancreato-Biliary Association (IHPBA) fellowship requirements for total and complex procedures during residency. Consideration should be given to those residents to allow them to bypass fellowship training provided that they meet other IHPBA standards.
Introduction
In the USA, general surgery residents are required to undertake four liver resections, three pancreatic procedures and 10 biliary operations, in addition to 50 laparoscopic cholecystectomies, by the Accreditation Council for Graduate Medical Education (ACGME) over the course of their training. This experience can be acquired by the resident as surgeon chief or surgeon junior; there are no set ACGME requirements in these categories for general surgery training.
Complex pancreatic procedures are defined as Whipple and pancreatic resection subtypes (total and subtotal) and pancreatic transplant. Complex liver operations include formal hepatic resection, segmentectomy and liver transplantation. Complex biliary interventions include common bile duct exploration and choledochoenteric anastomosis. These operations are usually performed by a wide variety of surgeons, including general surgeons [both with and without hepatopancreatobiliary (HPB) fellowship training], transplant surgeons and surgical oncologists.
Training in HPB-related surgery is a fellowship requirement for the societies covering these specialties. According to the International Hepato-Pancreato-Biliary Association (IHPBA), an HPB fellowship provides general surgeons with a focused exposure to HPB diseases. To graduate with an HPB fellowship, the trainee must complete at least 100 major HPB cases, and the fellow must act as primary surgeon in 75 of those procedures. A minimum of 25 major liver procedures is required, of which 15 must be liver resections. A minimum of 20 complex biliary operations is required, which cannot include cholecystectomy. A minimum of 30 major pancreatic operations are required, which cannot include biopsy.1 In comparison, the American Society of Transplant Surgeons (ASTS) requires a fellow to complete a 24-month programme during which he or she must complete 45 liver and 15 pancreatic transplant procedures.2 The Society of Surgical Oncology (SSO) requires oncology fellows to complete a minimum of 15 complex upper gastrointestinal procedures, including liver- and pancreas-related surgeries.3 Thus, all the curricula for fellowship training with these various societies include HPB operations.
These numbers are much higher than the numbers of procedures the ACGME requires residents to complete during their training. However, it is suspected that some residents, especially those at high-volume centres, may easily exceed ACGME requirements for total and complex HPB surgeries. Therefore, the objective of this study was to determine whether or not some general surgery residents perform enough HPB procedures during general surgery residencies to exclude them from the necessity of pursuing a fellowship in HPB surgery, with particular regard to those residents who complete the number of complex HPB operations required by the IHPBA Education Council.
Materials and methods
Trends in HPB training during general surgery residency were evaluated using ACGME General Surgery operative log programme data for the academic years 1999/2000 to 2009/2010. Total numbers of complex cases were defined for pancreatic (subtotal and total numbers of Whipple procedures and resection subtypes), liver (hepatectomy, segmentectomy and wedge resection biopsy) and biliary (common bile duct exploration, choledochoenteric anastomosis and other major biliary procedures) surgeries. Data maintained by the ACGME were examined for the mean number of HPB procedures undertaken by each resident; these data are reported according to the resident's academic year of graduation. Similarly, the average numbers of HPB operations performed as surgeon junior (residency years 1–3) and surgeon chief (residency years 4–5) were examined. Finally, the distribution of operations in all these categories were compared across both levels and further compared with the requirements of the ACGME and the IHPBA Education Council.4 Student's t-test was used to compare the means of average yearly totals of graduating residents for the 3-year periods of 2000–2002 and 2008–2010. A P-value of <0.05 was considered to indicate statistical significance.
Results
In the 1999/2000 academic year, a total of 252 programmes in general surgical training were available and the number of general surgery residents was 989. By contrast, in the 2009/2010 academic year, there were 242 programmes in general surgery and 1040 general surgery residents.
According to the 2005 annual summary of the National Hospital Discharge Survey, surgeons in the USA performed 800 000 HPB procedures, and institutions with general surgery residents completed 16% of those interventions in that year.5 Similarly, the overall proportion of HPB operations completed by general surgery graduating residents at surgical teaching institutions increased from 15% (n = 122 007) in 2000 to 18% (n = 143 000) in 2010, resulting in a relative increase of 20%.
Liver surgeries
General surgery residents graduating in 2010 completed 31% more procedures than residents graduating in 2000 (Table 1). These yearly increases (Fig. 1) were reflected in the average number of operations performed per graduating resident: a 24% increase was seen between 2000 graduates (7.6 procedures) and 2010 graduates (9.4 procedures). The maximum number of hepatic operations completed by general surgery residents graduating in 2010 was 33 (Table 2). As Fig. 2 shows, when the data are further evaluated according to the surgeon's years of experience, 2000 graduates are found to have performed 4044 of all liver operations as surgeon chiefs and 3424 of all liver procedures as surgeon juniors. The 2010 graduates performed 4947 procedures as surgeon chiefs (22% increase; P = 0.013) and 4818 interventions as surgeon juniors (41% increase; P < 0.001).
Table 1.
Increases in numbers of all and complex surgeries performed by general surgery residents graduating in 2000 and 2010
| Surgery type | General surgery resident case log data | |||||
|---|---|---|---|---|---|---|
| All surgeries | Complex surgeries | |||||
| 2000 | 2010 | Change | 2000 | 2010 | Change | |
| Liver | 7 468 | 9 765 | ↑31%a | 6 649 | 8 233 | ↑24%a |
| Pancreas | 8 185 | 12 006 | ↑47%a | 4 768 | 9 129 | ↑91%b |
| Biliary | 106 354 | 121 239 | ↑14% | 6 581 | 4 648 | ↓29%b |
Statistical analysis was performed for the mean yearly number of all surgeries performed by graduating residents in the 3-year periods encompassing 2000 (2000–2002) and 2010 (2008–2010).
P = 0.002.
P < 0.001.
Figure 1.
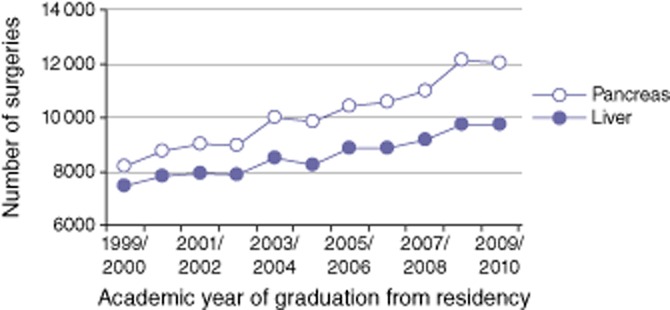
Numbers of all pancreatic and hepatic surgeries completed by general surgery residents graduating in 2000 to 2010
Table 2.
Case log totals for 2010 general surgery residents graduating in 2010 compared with Accreditation Council for Graduate Medical Education (ACGME) residency and International Hepato-Pancreato-Biliary Association (IHPBA) fellowship requirements
| Total case logs for graduates of 2010 | Surgeries required by ACGME, n | Surgeries required by IHPBA, n | ||
|---|---|---|---|---|
| Mean | Maximum | |||
| Liver | 9.4 | 33 | 4 | 25 |
| Pancreas | 11.5 | 49 | 3 | 30 |
| Biliary | 116.4 | 316 | NS | 20 |
NS, not specified as a separate category.
Figure 2.
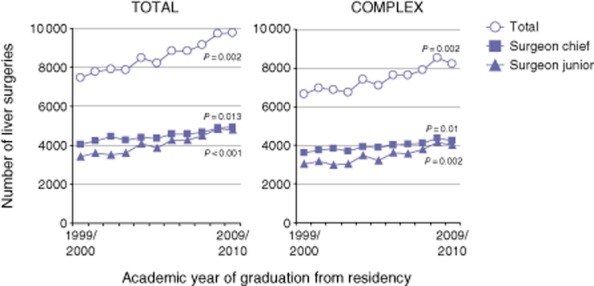
Numbers of all and complex hepatic surgeries completed by general surgery residents graduating in 2000 to 2010. Statistical values were derived by comparing the mean of the average yearly totals of graduating residents for the 3-year periods 2000–2002 and 2008–2010, respectively
The number of complex liver operations performed by general surgery residents graduating in 2010 was 24% higher than the number performed by residents graduating in 2000 (P = 0.002) (Table 1). Residents who graduated in 2000 performed 3610 complex liver interventions as surgeon chiefs and 3039 similar procedures as surgeon juniors (Fig. 2). Residents who graduated in 2010 completed 4223 procedures as surgeon chiefs (17% increase; P = 0.01) and 4010 procedures as surgeon juniors (32% increase; P = 0.002).
Pancreas surgeries
General surgery residents graduating in 2010 completed 47% more pancreatic operations than residents graduating in 2000 (Table 1). These yearly increases (Fig. 1) were reflected in the average number of procedures performed per graduating resident: residents graduating in 2010 performed an average of 11.5 procedures per graduate, whereas residents graduating in 2000 performed 8.3 procedures per graduate, indicating a 38% increase in the number of procedures performed per graduate over the decade. The maximum number of all pancreatic operations performed by general surgery residents graduating in 2010 was 49 (Table 2). Residents who graduated in 2000 performed a total of 5538 pancreatic operations as surgeon chiefs and 2647 as surgeon juniors (Fig. 3). Residents who graduated in 2010 completed 7737 procedures as surgeon chiefs (40% increase; P = 0.002) and 4269 as surgeon juniors (61% increase; P = 0.003).
Figure 3.
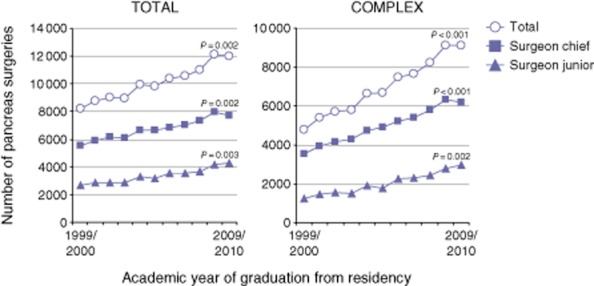
Numbers of all and complex pancreatic surgeries completed by general surgery residents graduating in 2000 to 2010. Statistical values were derived by comparing the mean of the average yearly totals of graduating residents for the 3-year periods 2000–2002 and 2008–2010, respectively
The number of complex pancreatic procedures performed by 2010 graduates was 91% higher than that completed by 2000 graduates (P < 0.001) (Table 1). Residents who graduated in 2000 logged a total of 3530 complex procedures as surgeon chiefs and 1238 as surgeon juniors (Fig. 3). Residents who graduated in 2010 completed 6174 procedures as surgeon chiefs (75% increase; P < 0.001) and 2955 as surgeon juniors (139% increase; P = 0.002).
Biliary surgeries
The ACGME does not make specific requirements for biliary operations as a separately defined category because these are included in the basic and advanced laparoscopic, alimentary and abdominal sections. However, a separate section for biliary procedures completed by graduating residents is maintained in the ACGME data system. General surgery residents graduating in 2010 completed 14% more interventions than residents graduating in 2000 (Table 1). These yearly increases (Fig. 4) were also reflected in the average number of procedures performed per graduating resident as the number of procedures performed by graduating residents in 2010 increased by 8% over that performed by equivalent residents in 2000 (116.6 versus 107.5 procedures per resident). The maximum number of all biliary procedures reported by general surgery residents graduating in 2010 was 316 (Table 2). Residents who graduated in 2000 completed 28 405 operations as surgeon chiefs and 77 949 as surgeon juniors (Fig. 5). Residents who graduated in 2010 completed 31 838 procedures as surgeon chiefs (12% increase; P = 0.097) and 89 391 as surgeon juniors (15% increase; P = 0.164).
Figure 4.
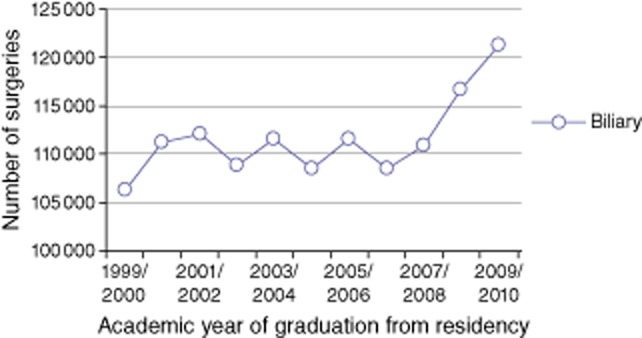
Numbers of all biliary surgeries completed by general surgery residents graduating in 2000 to 2010
Figure 5.
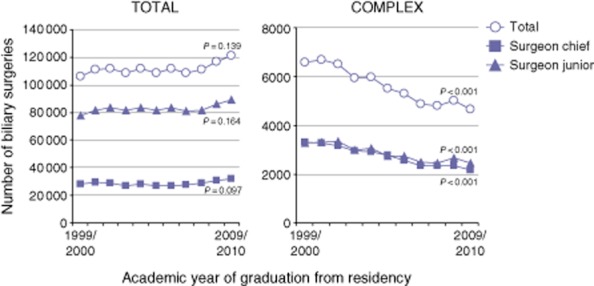
Numbers of all and complex biliary surgeries completed by general surgery residents graduating in 2000 to 2010. Statistical values were derived by comparing the mean of the average yearly totals of graduating residents for the 3-year periods 2000–2002 and 2008–2010, respectively
Complex biliary operations by general surgery residents graduating in 2010 decreased by 29% compared with the number performed by residents graduating in 2000 (P < 0.001) (Table 1). Residents graduating in 2000 performed 3297 complex biliary procedures as surgeon chiefs and 3284 as surgeon juniors (Fig. 5). Residents graduating in 2010 completed 2186 operations as surgeon chiefs (34% decrease; P < 0.001) and 2462 as surgeon juniors (25% decrease; P < 0.001).
Discussion
Hepatopancreatobiliary surgery is considered an essential part of general surgery training, and residents in this field need guidance to learn the complex operative skills necessary to successfully perform and manage HPB operations. Historically, most HPB procedures were performed by HPB, transplant and oncology surgeons. However, general surgery residents completed 16% of all HPB operations in the USA in 2005.5 The present study was able to establish that similar percentages of HPB operations were performed by residents in 2000 (15%) and 2010 (18%) using ACGME data, which showed a 20% relative increase in the number of HPB interventions performed, but only a 5% relative increase in the number of residents.
It is estimated that the US population will have increased by 18% to 325 million by 2020 and it is expected that the baby boomer generation will live longer than earlier generations.6 Moreover, the general surgery workload is predicted to increase by 31.5% and the HPB workload by 29.5% to 2020.6 However, a yearly survey covering eight of the last 10 years predicts the occurrence of ‘severe’ shortages in the general surgery workforce by 2020.7
To satisfy the need for competent HPB surgeons, an HPB fellowship registry was established on the IHPBA website in 2006. Additionally, the IHPBA Education and Training Committee was created to establish standards for HPB training and to ensure additional training during an HPB fellowship.8
Zyromski et al.9 performed a study that assessed whether including an HPB fellowship at a high-volume training centre would detract from general surgery resident HPB training. Using resident and fellow operative case logs for 3 years prior to and after incorporating the fellowship into their programme, they found no significant differences in volumes of liver or pancreatic resections between residents and fellows. Complex biliary operations declined in 2006 at the institution described by Zyromski et al.,9 which is consistent with the present data and most probably reflects the greater use of endoscopic procedures. Despite these decreases, the ACGME data in the present study show that the maximum number of complex biliary procedures reported by general surgery residents exceeds that required to complete an HPB fellowship according to IHPBA guidelines.
Additionally, according to Raptis and Clavien,10 a survey of 40 of the 71 fellowship directors registered on the IHPBA website identified the necessary steps that would ensure adequate HPB training as defined by IHPBA requirements. It is interesting to note that fewer than a third of the programme directors surveyed offered a programme that was compatible with IHPBA standards. Furthermore, 19 of 35 centres reported that only 54% of fellows actually completed the programme's objectives during the course of their training. The study also indicated that the main complaint of HPB fellowship programme directors was that the IHPBA curriculum was too extensive and should be shortened, and 33 of 40 centres either partially (n = 22, 55%) or fully (n = 11, 28%) implemented IHPBA standards as a method of ensuring adequate training in HPB surgeries.
Furthermore, the data showed that only half of hepatic (52%), pancreatic (48%) and biliary procedures (46%) were performed by programme fellows, whereas 24% of non-HPB cases involved the HPB fellow as the first surgeon. In fact, ‘the proportion of cases in which fellows were involved that represented HPB procedures and the proportion of cases in which fellows performed as first surgeons varied greatly among centres, ranging from none to 80%, and none to 100%, respectively’.10 Although Raptis and Clavien10 found the median number of operations performed by HPB fellows to be higher than that achieved by general surgery residents, analysis of ACGME data for general surgery residents reporting the maximum number of cases indicates that the number of complex HPB procedures performed per resident totalled 157. Therefore, the number of HPB procedures performed by general surgery residents is increasing over time and, in some cases, exceeds the number required by the IHPBA for the completion of a fellowship in HPB surgery.11
It is acknowledged that general surgery residents who report an average or below average number of HPB procedures require further HPB training in order to be able to successfully manage the complexity involved in HPB surgery.12 However, if selected residents who have performed complex HPB surgeries at high-volume centres meet the minimum requirements of the IHPBA, they should be considered to be working on a par with HPB fellows.
In conclusion, some general surgery residents receive more than enough HPB training to complete general surgery training as defined by the ACGME. Hence, we suggest that it is possible to exclude a graduating general surgery resident from requirements for additional training when the resident graduates with a completion portfolio greater than that required by the IHPBA and when the resident is evaluated according to a standardized protocol and appropriately meets IHPBA standards.13,14
Conflicts of interest
None declared.
References
- 1.Education and Training Committee for the International Hepato-Pancreato-Biliary Association. Standards for hepato-pancreato-biliary training. 2008. Available at http://www.ihpba.org/assets/documents/hpb_training_standards.pdf (last accessed 11 March 2013)
- 2.American Society of Transplant Surgeons. 2012. ASTS accreditation of abdominal transplant surgery fellowship programs. Available at http://www.asts.org/fellowshiptraining/accreditation.aspx (last accessed 11 March 2013)
- 3.Training Committee of the Society of Surgical Oncology. 2001. Training in surgical oncology. Available at http://www.surgonc.org/training-education/surgical-oncology/program-requirements (last accessed 11 March 2013)
- 4.Surgical Council on Resident Education. 2011. General surgery residency curriculum outline: patient care and medical knowledge 2011–2012. Available at http://www.surgicalcore.org/curriculumoutline2011-12.pdf (last accessed 11 March 2013)
- 5.DeFrances CJ, Cullen KA, Kozak LJ. 2007. National Hospital Discharge Summary: 2005 Annual Summary With Detailed Diagnosis and Procedure Data. Available at http://www.cdc.gov/nchs/data/series/sr_13/sr13_165.pdf (last accessed 20 December 2012) [PubMed]
- 6.Liu JH, Etzioni DA, O'Connell JB, Maggard MA, Ko CY. The increasing workload of general surgery. Arch Surg. 2004;139:423–428. doi: 10.1001/archsurg.139.4.423. [DOI] [PubMed] [Google Scholar]
- 7.Massachusetts Medical Society. 2012. 2012 Massachusetts Medical Society Physician Workforce Study. Available at http://www.massmed.org/workforce (last accessed 22 October 2012)
- 8.Rassadi R, Dickerman RM, Dunn EL, Tarnasky PR, Linder JD, Mejia A, et al. Hepatopancreaticobiliary (HPB) surgery: what is the right fellowship for the right training? J Surg Educ. 2008;65:186–190. doi: 10.1016/j.jsurg.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Zyromski N, Torbeck L, Canal DF, Lillemoe KD, Pitt HA. Incorporating an HPB fellowship does not diminish surgical residents' HPB experience in a high-volume training centre. HPB. 2010;12:123–128. doi: 10.1111/j.1477-2574.2009.00146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raptis DA, Clavien P-A. Evaluation of Hepato-Pancreato-Biliary (HPB) fellowships: an international survey of programme directors. HPB. 2011;13:279–285. doi: 10.1111/j.1477-2574.2010.00283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Subhas G, Mittal VK. Training minimal invasive approaches in hepatopancreatobiliary fellowship: the current status. HPB. 2011;13:149–152. doi: 10.1111/j.1477-2574.2010.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12:153–158. doi: 10.1007/s11605-007-0378-6. [DOI] [PubMed] [Google Scholar]
- 13.Bell RH., Jr Graduate education in general surgery and its related specialties and subspecialties in the United States. World J Surg. 2008;32:2178–2184. doi: 10.1007/s00268-008-9658-x. [DOI] [PubMed] [Google Scholar]
- 14.Sachdeva AK, Bell RH, Jr, Britt LD, Tarpley JL, Blair PG, Tarpley MJ. National efforts to reform residency education in surgery. Acad Med. 2007;82:1200–1210. doi: 10.1097/ACM.0b013e318159e052. [DOI] [PubMed] [Google Scholar]


