Abstract
Purpose
Supporters of minimally invasive approaches for transforaminal lumbar interbody fusion (TLIF) have reported short-term advantages associated with a reduced soft tissue trauma. Nevertheless, mid- and long-term outcomes and specifically those involving physical activities have not been adequately studied. The aim of this study was to compare the clinical outcomes of mini-open versus classic open surgery for one-level TLIF, with an individualized evaluation of the variables used for the clinical assessment.
Methods
A prospective cohort study was conducted of 41 individuals with degenerative disc disease who underwent a one-level TLIF from January 2007 to June 2008. Patients were randomized into two groups depending on the type of surgery performed: classic open (CL-TLIF) group and mini-open approach (MO-TLIF) group. The visual analog scale (VAS), North American Spine Society (NASS) Low Back Pain Outcome instrument, Oswestry Disability Index (ODI) and the Short Form 36 Health Survey (SF-36) were used for clinical assessment in a minimum 3-year follow-up (36–54 months).
Results
Patients of the MO-TLIF group presented lower rates of lumbar (p = 0.194) and sciatic pain (p = 0.427) and performed better in daily life activities, especially in those requiring mild efforts: lifting slight weights (p = 0.081), standing (p = 0.097), carrying groceries (p = 0.033), walking (p = 0.069) and dressing (p = 0.074). Nevertheless, the global scores of the clinical questionnaires showed no statistical differences between the CL-TLIF and the MO-TLIF groups.
Conclusions
Despite an improved functional status of MO-TLIF patients in the short term, the clinical outcomes of mini-open TLIF at the 3- to 4-year follow-up showed no clinically relevant differences to those obtained with open TLIF.
Keywords: Minimally invasive, TLIF, Lumbar fusion, Degenerative disc disease, Prospective
Introduction
The transforaminal lumbar interbody fusion (TLIF) was first described by Harms et al. [1, 2]. TLIF offers several advantages including the reduction of dural sac retraction or postoperative radiculitis [2, 3]. A unilateral TLIF procedure provides an access to the disc space through a far-lateral approach, after removal of all or part of the facet preserving the contralateral joint, with similar outcomes to those obtained with the posterolateral lumbar interbody fusion (PLIF) [4].
In the later years, some surgeons have supported the use of minimally invasive approaches to preserve muscular and vascular structures of the lumbar spine [5, 15]. The potential benefits include: smaller incisions, decreased soft tissue damage, shorter hospital stay, decreased time to return to work and lower costs [5–7].
The advantages of the mini-open approach applied to unilateral TLIF with transpedicular screws were published by Foley [8], Schwender [9] and Holly [10]. These authors reported good perioperative outcomes, such as lower rates of blood loss, severe pain or hospital stay. Recent papers have confirmed the advantages of mini-open approaches when compared with classic approaches [6, 11–16]. These surveys also showed lower rates of analgesic requirements during the first few months and a faster recovery of daily life activities [15, 16].
In contrast, the disadvantages of these techniques have been found to be the following: long learning curve, long operative time and a technically demanding insertion of the pedicle screws [13, 14]. Heterogeneous complication rates have been published [11, 12, 14, 17], being consistently more prevalent during the learning curve [18].
Union rates with the use of mini-open TLIF (80–100 %) have been reported to be higher than with open classic approaches (80–91 %) [3, 11, 14, 16]. Clinical outcomes in the 1-year follow-up have been found to be similar in both techniques [11–14, 17], but the evaluation of the minimally invasive approaches by the surgeons was positive due to the inclusion in all of these surveys of the cases treated during the learning curve, when most of the complications occur [13, 18]. Nevertheless, an individualized analysis of the parameters used in the clinical interviews has not been carried out in any of these works.
The aim of this study was to compare the clinical outcomes of minimally invasive versus open approaches for one-level transforaminal lumbar interbody fusion in a minimum 3-year follow-up. Particular attention has been paid to an individualized evaluation of the variables used for the clinical assessment in the standardized interviews.
Methods
Methods and patients
A prospective cohort study was conducted of 50 patients without previous medical conditions, who underwent a one-level TLIF from January 2007 to June 2008.
In all cases the indication for surgery was a degenerative disc disease. The surgery was performed after 6 months of failed nonoperative treatment or neurologic deficit progression.
Exclusion criteria were: patients with lumbar stenosis or isthmic spondylolisthesis, previous lumbar spine surgery (except single discectomy) or presence of MRI degenerative changes in other lumbar levels.
Patients fulfilling inclusion criteria were randomized into two groups, depending on their position in the waiting list for surgery: the classic approach (CL-TLIF) group, in which patients underwent a 360º circumferential arthrodesis through a classic posterior approach; and the mini-open group (MO-TLIF), in which the same instrumented arthrodesis was performed through a minimally invasive approach. In this group, all the interventions were carried out by the same principal surgeon.
In the CL-TLIF group, the standard technique was: medial approach, 12 cm length incision, one side subtotal facetectomy, discectomy made from the symptomatic side and mono-portal TLIF. Decortication of facets and transverse processes, autologous bone grafting (from the laminectomy and facetectomy) and pedicle screw fixation were also performed.
In the MO-TLIF group, two paramedian incisions of 2.5–3 cm were made for the tubular retractors (QUADRANT®. Medtronic Sofamor Danec, Memphis, TN). Subtotal facetectomy, discectomy, mono-portal TLIF (symptomatic side), pedicle screws placement, lateral facets and transverse processes decortication and bilateral autologous bone grafting were performed. The surgery was carried out with binocular loupes or under direct visualization through the retractors, with two surgeons working simultaneously from both sides of the patient.
The intersomatic device used was a 25 mm CIO® (Stryker Spine, South Allendale, NJ) / 28 mm CAPSTONE® (Medtronic Sofamor Danec, Memphis, TN), filled with autologous bone from the resected laminae and facet joints. In all cases, bilateral fixation with pedicle screws (Legacy®. Medtronic Sofamor Danec, Memphis, TN) was performed.
Assessment of results
Patients’ epidemiological information was collected from medical records. The following standardized interviews were used for the clinical assessment: visual analogic scale (VAS), North American Spine Society (NASS) Low Back Pain Outcome instrument [19, 20], Oswestry Disability Index (ODI) [21] and the Short Form 36 Health Survey (SF-36) [22, 23]. All these questionnaires have been found to be valid instruments for the assessment of clinical outcomes in spine surgery [24].
From the NASS Low Back Pain Outcome instrument several items were selected: low back and/or buttock pain, leg pain, numbness/tingling in leg and/or foot and weakness in leg and/or foot (38–45 questions—Lumbar Questionnaire). All these items were evaluated regarding frequency and intensity as follows.
Frequency: none of the time (1), a little bit of the time (2), some of the time (3), a good bit of the time (4), most of the time (5) and all the time (6).
Intensity: not at all bothersome (1), slightly bothersome (2), somewhat bothersome (3), mildly bothersome (4), very bothersome (5) and extremely bothersome (6).
The results were calculated as the average value of the two figures (frequency and intensity).
All the standardized interviews, Lumbar Questionnaire of the NASS, VAT, ODI and SF-36, were self-completed by all the patients in a minimum 3-year follow-up, from March to June 2011 (36–54 months). None of the surgeons involved in the treatment provided any information to the patients for filling the questionnaires.
No statistical differences were found between the two groups in age, gender, spinal level affected or preoperative clinical status (VAS, NASS, ODI and SF-36). The groups were considered clinically comparable, as was demonstrated in a previous study [15] (Table 1).
Table 1.
Comparison of preoperative variables between the mini-open transforaminal lumbar interbody fusion (MO-TLIF) and the classic open (CL-TLIF) groups
| Group | N | Mean ± SD | p |
|---|---|---|---|
| Age (years) | |||
| CL-TLIF | 20 | 43.15 ± 7.3 | 0.597 |
| MO-TLIF | 21 | 41.81 ± 8.7 | |
| Gender (M/F) (% male) | |||
| CL-TLIF | 20 | 13/7 (65 %) | 0.585 |
| MO-TLIF | 21 | 14/7 (66.7 %) | |
| VAT preop (low back pain) | |||
| CL-TLIF | 20 | 7.19 ± 2.21 | 0.787 |
| MO-TLIF | 21 | 7.04 ± 1.12 | |
| VAT preop (leg pain) | |||
| CL-TLIF | 20 | 7.53 ± 1.23 | 0.678 |
| MO-TLIF | 21 | 7.31 ± 2.05 | |
| Oswestry Disability Index (ODI) | |||
| CL-TLIF | 20 | 27.19 ± 8.19 | 0.449 |
| MO-TLIF | 21 | 28.85 ± 5.52 | |
| SF-36 Physical Scale | |||
| CL-TLIF | 20 | 33.5 ± 19.2 | 0.761 |
| MO-TLIF | 21 | 35.29 ± 18.32 | |
| SF-36 | |||
| CL-TLIF | 20 | 34.3 ± 9.8 | 0.647 |
| MO-TLIF | 21 | 36.1 ± 14.6 | |
The postoperative complications were the following: one case of dural tear in each group and one malposition of a pedicle screw in the MO-TLIF group that had to be replaced. All these cases were included in the study.
Statistical assessment
A standard descriptive analysis expressed as mean ± standard deviation was performed. For the comparative study, when the ordinal and quantitative variables had no standard normal distribution, the non-parametric Mann–Whitney U test was used. When the distribution of the variables was normal, the parametric Student’s t test was used. All the statistical analyses were performed with the program SPSS 16.0.
Results
From a total of 50 subjects included in the study, 21 patients of the MO-TLIF group and 20 patients of the CL-TLIF group completed the clinical interviews with reliability (N = 41). Two patients in each group did not answer the interview in time (4 %), three patients of the CL-TLIF (6 %) and two of the MO-TLIF group (4 %) answered the interviews without the required reliability and were excluded.
NASS-Lumbar Questionnaire
No significant differences were found between the two groups in the following variables studied: low back and/or buttock pain, leg pain, numbness/tingling in leg and/or foot and weakness in leg and/or foot.
The mean value of the variable “low back and/or buttock pain” was lower than 3 in both groups, being scored as follows “A little of the time/Slightly bothersome” = 2 points; and “Some of the time/Somewhat bothersome” = 3 points.
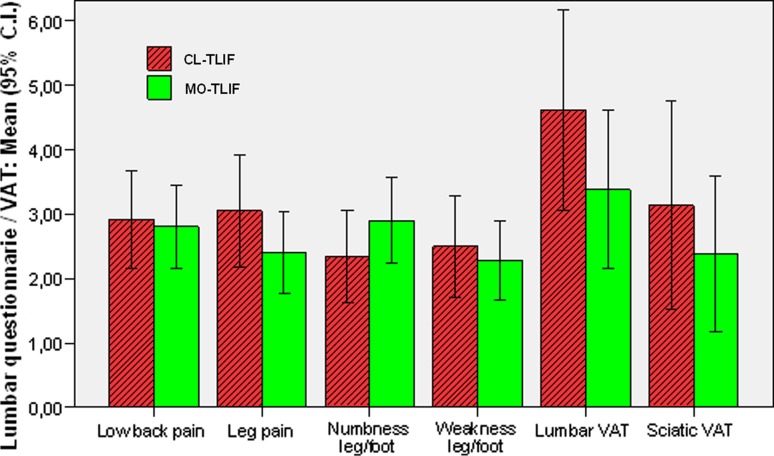
The differences found between groups in sciatic pain (more frequent and severe in the CL-TLIF group) and neurologic symptoms (more frequent and severe in the MO-TLIF group) were not statistically significant (Table 2; Fig. 1).
Table 2.
Comparison of the “Lumbar Questionnaire” of the North American Spine Society (NASS) instrument between the mini-open transforaminal lumbar interbody fusion (MO-TLIF) and the classic open (CL-TLIF) groups
| Lumbar questionnaire (NASS) | CL-TLIF group | MO-TLIF group | Mann–Whitney U (p) |
|---|---|---|---|
| Low back pain (frequency) | 2.894 ± 1.76 | 2.904 ± 1.54 | 0.936 |
| Low back pain (intensity) | 2.947 ± 1.61 | 2.714 ± 1.42 | 0.688 |
| Leg pain (frequency) | 3.052 ± 1.84 | 2.571 ± 1.56 | 0.503 |
| Leg pain (intensity) | 3.052 ± 1.84 | 2.238 ± 1.30 | 0.236 |
| Numbness of leg/foot (frequency) | 2.500 ± 1.57 | 3.142 ± 1.59 | 0.157 |
| Numbness of leg/foot (intensity) | 2.315 ± 1.56 | 2.666 ± 1.46 | 0.347 |
| Weakness in leg/foot (frequency) | 2.555 ± 1.54 | 2.381 ± 1.56 | 0.791 |
| Weakness in leg/foot (intensity) | 2.650 ± 1.72 | 2.190 ± 1.25 | 0.683 |
| VAT low back pain | 4.611 ± 3.12 | 3.381 ± 2.69 | 0.194 |
| VAT leg pain | 3.138 ± 3.24 | 2.381 ± 2.65 | 0.427 |
Fig. 1.
Comparison of variables included in the “Lumbar Questionnaire” of the North American Spine Society (NASS) instrument between the MO-TLIF and the CL-TLIF groups (mean values of each item have been represented as follows: intensity value + frequency value / 2)
VAT (lumbar and sciatic pain)
No significant differences were found in the VAT interview scores, with the mean values of lumbar pain and sciatic pain 12.5 and 7.5 %, respectively, higher in the CL-TLIF group than in the MO-TLIF group (Table 2; Fig. 1).
Oswestry Disability Index (ODI)
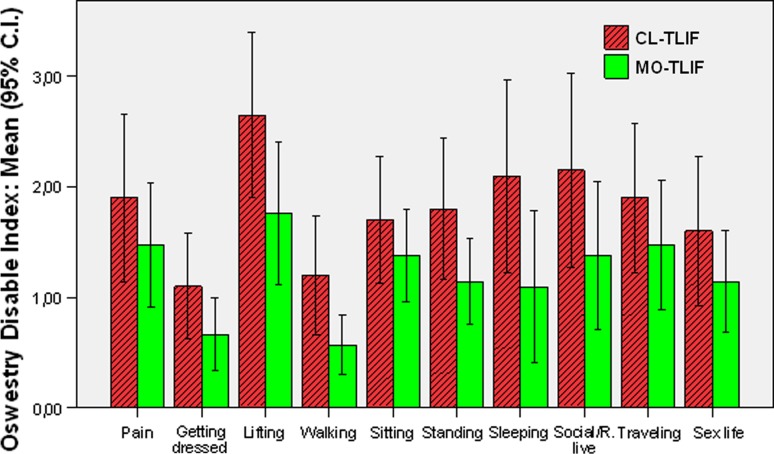
The global scores of the ODI were 6 points lower in the MO-TLIF than in the CL-TLIF group (12.09 vs 18.1), but this difference (12 %) did not reach statistical significance (p = 0.073). The main differences in favor of the MO-TLIF group were found in the following variables: lifting slight weights (p = 0.081), walking (p = 0.069), standing (p = 0.097) and sleeping (p = 0.067) (Table 3; Fig. 2).
Table 3.
Comparison of the Oswestry Disability Index (ODI) between the mini-open (MO-TLIF) and the classic open (CL-TLIF) groups
| Oswestry Disability Index (ODI) | CL-TLIF group | MO-TLIF group | Mann–Whitney U (p) |
|---|---|---|---|
| Pain | 1.90 ± 1.62 | 1.47 ± 1.23 | 0.536 |
| Getting dressed | 1.10 ± 1.02 | 0.66 ± 0.73 | 0.178 |
| Lifting slight weights | 2.65 ± 1.59 | 1.76 ± 1.41 | 0.081 |
| Walking | 1.20 ± 1.15 | 0.57 ± 0.59 | 0.069 |
| Sitting | 1.70 ± 1.21 | 1.38 ± 0.92 | 0.356 |
| Standing | 1.80 ± 1.36 | 1.14 ± 0.85 | 0.097 |
| Sleeping | 2.10 ± 1.86 | 1.09 ± 1.51 | 0.067 |
| Social–recreational life | 2.15 ± 1.87 | 1.38 ± 1.46 | 0.123 |
| Traveling | 1.90 ± 1.44 | 1.47 ± 1.28 | 0.352 |
| Sex life | 1.60 ± 1.43 | 1.14 ± 1.01 | 0.349 |
| OD Index | 18.10 ± 12.45 | 12.09 ± 7.59 | 0.073 |
Fig. 2.
Comparison of the variables of the Oswestry Disability Index (ODI) between the MO-TLIF and the CL-TLIF groups
SF-36
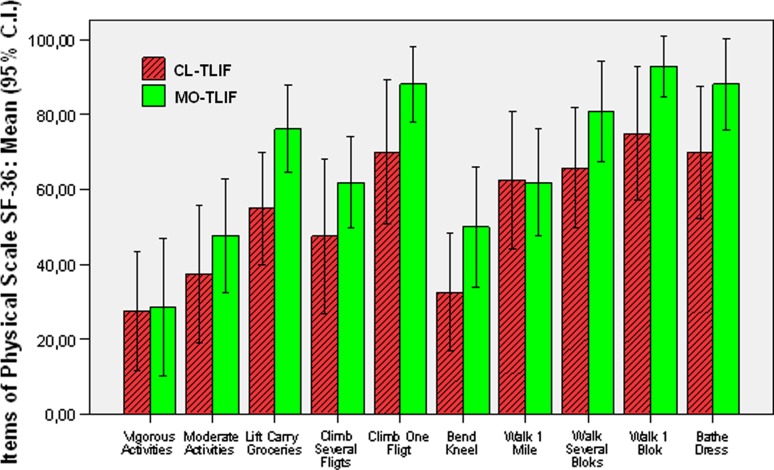
No significant differences were found between groups in any of the eight scales of the SF-36. The biggest differences (12 % in favor of the MO-TLIF group) were found in the Physical Functioning Scale (p = 0.114). Relatively high scores were found in both groups in some of the physical functioning items (climbing one floor, walking one block and having a bath). When comparing daily life activities, some variables showed statistically significant differences (lift, carry groceries, p = 0.033) or almost significant (walk one block, p = 0.095; bathe–dress, p = 0.074) in favor of the MO-TLIF group (Table 4; Fig. 3). Lesser differences (5–10 %) were shown in the Vitality, Social Functioning, Role-Emotional and Mental Health scales.
Table 4.
Comparison of the SF-36 Physical Scale between the mini-open (MO-TLIF) and the classic open (CL-TLIF) groups
| Physical Functioning SF-36 | CL-TLIF group | CL-MO group | Mann–Whitney U (p) |
|---|---|---|---|
| Vigorous activities | 27.500 ± 39.32 | 28.809 ± 33.98 | 0.841 |
| Moderate activities | 37.500 ± 39.32 | 47.619 ± 33.45 | 0.330 |
| Lift, carry groceries | 55.000 ± 32.03 | 76.190 ± 25.59 | 0.033 |
| Climb several flights | 47.500 ± 44.35 | 61.904 ± 26.95 | 0.260 |
| Climb one flight | 70.000 ± 41.04 | 88.095 ± 21.82 | 0.161 |
| Bend–kneel | 32.500 ± 33.54 | 50.000 ± 35.35 | 0.111 |
| Walk 1 mile | 62.500 ± 39.32 | 61.905 ± 31.24 | 0.831 |
| Walk several blocks | 65.789 ± 33.55 | 80.952 ± 29.48 | 0.122 |
| Walk one block | 75.000 ± 38.04 | 92.857 ± 17.93 | 0.095 |
| Bathe, dress | 70.000 ± 37.69 | 88.095 ± 26.95 | 0.074 |
| Mean SF-36 physical scale | 55.333 ± 27.44 | 67.142 ± 18.68 | 0.114 |
Fig. 3.
Comparison of the variables included in the Physical Scale of the SF-36 between the MO-TLIF and the CL-TLIF groups
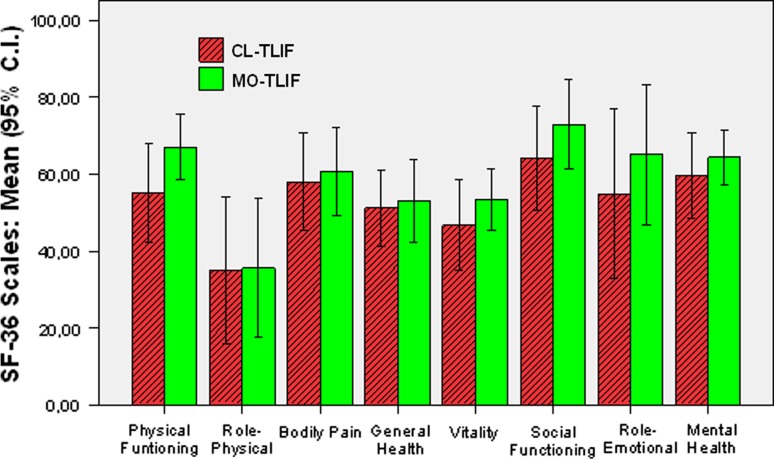
In the rest of the scales of the SF-36 (Role-Physical, Bodily Pain, General Health) the differences were scarce (< 5 %) (Table 5; Fig. 4).
Table 5.
Comparison of the scales included in the SF-36 between the mini-open (MO-TLIF) and the classic open (CL-TLIF) groups
| SF-36 | CL-TLIF group | MO-TLIF group | Mann–Whitney U (p) |
|---|---|---|---|
| Physical Functioning mean | 55.333 ± 27.44 | 67.142 ± 18.67 | 0.114 |
| Role-Physical mean | 35.000 ± 40.87 | 35.714 ± 39.97 | 0.804 |
| Bodily Pain mean | 58.125 ± 27.14 | 60.714 ± 25.07 | 0.753 |
| General Health mean | 51.315 ± 20.60 | 53.095 ± 24.01 | 0.804 |
| Vitality mean | 46.750 ± 25.14 | 53.333 ± 17.41 | 0.334 |
| Social Functioning mean | 64.250 ± 29.01 | 72.976 ± 25.35 | 0.347 |
| Role-Emotional mean | 55.000 ± 47.48 | 65.079 ± 40.10 | 0.520 |
| Mental Status mean | 59.650 ± 23.96 | 64.381 ± 15.99 | 0.460 |
| Physical Health mean | 50.599 ± 24.70 | 57.199 ± 20.80 | 0.360 |
| Mental Health mean | 55.464 ± 20.80 | 62.602 ± 19.66 | 0.317 |
| SF-36 mean | 52.513 ± 22.91 | 59.431 ± 19.34 | 0.302 |
Fig. 4.
Comparison of the scores obtained in the scales included in the SF-36 between the MO-TLIF and the CL-TLIF groups
The low scores found in both groups were remarkable in the items of General Health, Vitality and particularly in the Physical Role that evaluates the performance at work and the difficulties in some daily life activities. Both groups had similar scores in these variables.
Discussion
Minimally invasive TLIF might provide some benefits in the approach-related morbidity of conventional open surgery in the short term. The first results of pedicle fixation through a mini-open TLIF approach were published by Foley et al. [8]. Schwender et al. [9] have previously reported in a meeting in Rome satisfactory clinical outcomes in a series of 49 patients, confirmed in a later publication. Recently, better outcomes regarding blood loss, postoperative pain and hospital stay have been reported with mini-open when compared with open TLIF approaches [5–7, 11–15]. These data also support the reduced costs of the minimally invasive TLIF techniques.
In opposition, some disadvantages have been described with the use of this technique such as a long learning curve, longer operative time, high exposition to radiation and difficulty in the insertion of the pedicle screws. Nevertheless, all of them have been found to decrease with practice [9, 13].
Once the advantages of the mini-open surgery in the perioperative term have been described, other potential benefits such as a faster recovery, quicker return to work and the outcomes in the long term have to be tested.
In 2009, our group published a comparative study showing lower analgesic requirements and better recovery of daily life activities (ODI and Physical Scale of the SF-36) in the 3-month follow-up in a series of 15 patients treated with minimally invasive surgery [15].
It was remarkable that the activities requiring “moderate” efforts (walking more than 1 mile, standing, social life activities, traveling, having sex) had a significantly better recovery in the short term in patients treated with minimally invasive surgery when compared with those treated with traditional open surgery [15].
In recently published studies, no statistical differences regarding clinical outcomes have been found between mini-open and standard approaches in follow-up periods from 1 to 4 years [11–14, 17, 25]. Nevertheless, the majority of authors recommended mini-open approaches based on the aforementioned advantages even with the inclusion, in all their series, of the patients treated during the learning curve.
Different techniques for pedicle screw fixation have been used through the mini-open TLIF approach: percutaneous insertion [13], bilateral mini-open approaches [15, 22] or combined techniques, percutaneously in one side and through a mini-open approach in the contralateral one [8, 9, 11].
Two reasons explain the use of a bilateral mini-open approach in our survey: the possibility for two surgeons to work at the same time and the adequate exposure for a bilateral facet decortication to perform arthrodesis.
For the clinical assessment, several standardized interviews adapted to the Spanish language were used in our study (VAS, NASS [19, 20], ODI [21] and SF-36 [22, 23]). Clinical symptoms such as pain or neurologic deficit were evaluated with the VAS and the NASS Lumbar Questionnaire. The ODI and the Physical Scale of the SF-36 were used for the assessment of subjective symptoms and daily life activities performance; and the SF-36, a general health test, included not only information concerning physical status but also general mental and somatic health [24].
As noted before, when a detailed study of the items of these interviews was made, some results seemed remarkable in support of the mini-open approach:
(A) MO-TLIF patients showed an improvement of clinical symptoms (lumbar (p = 0.194) and sciatic pain (p = 0.427)) when compared with CL-TLIF patients. (B) MO-TLIF patients showed a better performance in daily life activities (p = 0.073). These differences were close to statistical significance in some of the variables studied: lifting slight weights (p = 0.081), walking (p = 0.069), standing (p = 0.097), sleeping (p = 0.067), carrying groceries (p = 0.033), walking one block (p = 0.095), bathing and dressing (p = 0.074). (C) Patients of the MO-TLIF group had better scores in the Role-Emotional (7.3 %) (p = 0.520) and Mental Health (8 %) (p = 0.460) scales, which might be related to a better physical status of this group of patients.
Nevertheless in this prospective comparative study, we have not found statistically significant differences between the MO-TLIF and CL-TLIF groups in the global mean scores of the VAS, NASS (Lumbar Questionnaire), ODI or SF-36. Only in the ODI the clinical differences between groups were close to statistical significance (p = 0.073). Other papers have reported similar results using the same clinical interviews [7–9, 11, 13–17].
Limitations
It might be argued that the sample size is short and therefore statistical significance could be hampered. The few surveys published in this area have been conducted on similar samples [12, 15–17]. For this purpose, the appropriate statistical corrections for short samples in the analysis were carefully selected. When the variables had no standard normal distribution, the non-parametric Mann–Whitney U test was used for the comparative study. In all other cases with normal distribution, the Student’s t test was performed.
In conclusion, mini-open approach patients tended to perform better in some daily life activities, especially in those requiring mild efforts in the first postoperative months. These results might be related to a decreased approach-related morbidity [5, 12, 15, 16] and with an improved mental health status in these group of patients. Nevertheless, the global clinical outcomes of the one-level mini-open TLIF showed no clinically relevant differences when compared with the classic open TLIF at the 3- to 4-year follow-up. Further studies in the long term are needed to evaluate if the benefits of the initial soft tissue preservation of the mini-open approach persist over time or tend to equalize with the classic open surgery outcomes.
Acknowledgments
The authors acknowledge the contribution of the members of the Spine Surgery Unit: Enrique Suñen, Diego Peña, Antonio Loste and Antonio Tabuenca, for their collaboration in this study.
Conflict of interest
None of the authors received any financial support or funding from any organization for this study. There are no conflicts of interest in this manuscript. The authors also state that they have full control of all primary data and that they allow the journal to review these data.
Contributor Information
Javier Rodríguez-Vela, Email: jrodriguezvela@hotmail.com.
Antonio Lobo-Escolar, Phone: +34-97-6765664, FAX: +34-97-6765632, Email: aloboescolar@yahoo.es.
Eduardo Joven, Email: ejovenaliaga@yahoo.es.
Javier Muñoz-Marín, Email: jmunozma@gmail.com.
Antonio Herrera, Email: aherrera@salud.aragon.es.
José Velilla, Email: jvelilla@salud.aragon.es.
References
- 1.Harms JG, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Oper Orthop Traumatol. 1998;10:90–102. doi: 10.1007/s00064-006-0112-7. [DOI] [PubMed] [Google Scholar]
- 2.Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl) Z Orthop Ihre Grenzgeb. 1982;120:343–347. doi: 10.1055/s-2008-1051624. [DOI] [PubMed] [Google Scholar]
- 3.Rouben D, Casnellie M, Ferguson M. Long-term durability of minimal invasive posterior transforaminal lumbar interbody fusion: a clinical and radiographic follow-up. J Spinal Disord Tech. 2011;24:288–296. doi: 10.1097/BSD.0b013e3181f9a60a. [DOI] [PubMed] [Google Scholar]
- 4.Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A, Wolinsky JP, Gokaslan ZL, Witham TF. Trans-foraminal versus posterior lumbar interbody fusion: comparison of surgical morbidity. Neurol Res. 2011;33:38–42. doi: 10.1179/016164110X12681290831289. [DOI] [PubMed] [Google Scholar]
- 5.Tsutsumimoto T, Shimogata M, Ohta H, Misawa H. Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis: comparison of paraspinal muscle damage and slip reduction. Spine. 2009;34:1923–1928. doi: 10.1097/BRS.0b013e3181a9d28e. [DOI] [PubMed] [Google Scholar]
- 6.Wang MY, Cummock MD, Yu Y, Trivedi RA. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine. 2010;12:694–699. doi: 10.3171/2009.12.SPINE09621. [DOI] [PubMed] [Google Scholar]
- 7.Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24:479–484. doi: 10.1097/BSD.0b013e3182055cac. [DOI] [PubMed] [Google Scholar]
- 8.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003;28:S26–S35. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 9.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18:S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 10.Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006;20:E6. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 11.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007;32:537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 12.Shunwu F, Xing Z, Fengdong Z, Xianggian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine. 2010;35:1615–1620. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 13.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780–1784. doi: 10.1007/s00586-010-1404-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010;1:12. doi: 10.4103/2152-7806.63905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodríguez-Vela J, Lobo-Escolar A, Joven-Aliaga E, Herrera A, Vicente J, Suñen E, Loste A, Tabuenca A. Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur Spine J. 2009;18:1194–1201. doi: 10.1007/s00586-009-1010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Logroscino CA, Proietti L, Pola E, Scaramuzzo L, Tamburrelli FC. A minimally invasive posterior lumbar interbody fusion for degenerative lumbar spine instabilities. Eur Spine J. 2011;20:S41–S45. doi: 10.1007/s00586-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 18.Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine. 2010;35:S281–S286. doi: 10.1097/BRS.0b013e3182022d32. [DOI] [PubMed] [Google Scholar]
- 19.Sarasqueta C, Gabaldon O, Iza I, Béland F, Paz PM. Cross-cultural adaptation and validation of the NASS outcomes instrument in Spanish patients with low back pain. Eur Spine J. 2005;14:586–594. doi: 10.1007/s00586-004-0871-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine. 1996;21:741–749. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 21.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 22.Brazier JE, Harper R, Jones NMB, O’Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alonso J, Prieto L, Anto JM. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Med Clin (Barc) 1995;104:771–776. [PubMed] [Google Scholar]
- 24.Haro H, Maekawa S, Hamada Y. Prospective analysis of clinical evaluation and self-assessment by patients after decompression surgery for degenerative lumbar canal stenosis. Spine J. 2008;8:380–384. doi: 10.1016/j.spinee.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 25.Ozgur BM, Yoo K, Rodriguez G, Taylor WR. Minimally invasive technique for transforaminal lumbar interbody fusion (TLIF) Eur Spine J. 2005;14:887–894. doi: 10.1007/s00586-005-0941-3. [DOI] [PubMed] [Google Scholar]