Abstract
Purpose
Chronic musculoskeletal pain is often associated with psychological distress and maladaptive beliefs and these are sometimes reported to have a negative impact on surgical outcome. The influence of a surgical intervention, and in particular its outcome, on the course of change in psychological status is poorly documented. In this prospective study, we sought to examine the dynamic interplay between psychological factors and outcome in patients undergoing decompression surgery for spinal stenosis/herniated disc.
Methods
Before and 12 months after surgery, 159 patients (100 men, 59 women; 65 ± 11 years) completed a questionnaire booklet containing questions on socio-demographics, medical history, pain characteristics (intensity, frequency, use of medication), psychological disturbance [ZUNG Depression Scale and Modified Somatic Perception Questionnaire (MSPQ)], catastrophising (sub-scale of the Coping Strategies Questionnaire) and disability (Roland and Morris questionnaire) and the Fear Avoidance Beliefs Questionnaire about physical activity (FABQ-PA). The global outcome of surgery was assessed at 12 months using a five-point Likert scale and dichotomised as “good” (operation helped/helped a lot; coded 1) and “poor” (operation helped only little/did not help/made things worse; coded 0).
Results
Valid questionnaire data were available for 148 patients at 12 months’ follow-up: 113 (76.4 %) reported a good outcome and 35 (23.6 %) a poor outcome. In univariate analyses, the following baseline variables each significantly (p < 0.05) predicted a good 12-month global outcome: no involvement in a disability claim, and lower LBP frequency, average LBP in the last week, average score on all pain scales, FABQ-PA and catastrophising. In multiple logistic regression, only lower FABQ-PA scores [OR 0.877 (95 %CI 0.809–0.949), p = 0.001] and lower LBP frequency at baseline [OR 0.340 (1.249–1.783), p < 0.0001] significantly predicted a good outcome at 12 months. A second “explanatory” logistic regression model revealed that a good outcome at 12 months was significantly associated with improvements (from baseline to 12 months) in average score on all the pain intensity scales [OR 1.6879 (1.187–2.398)], general health [OR 1.246 (1.004–1.545)], psychological disturbance [OR 1.073 (1.006–1.144)] and Roland Morris Disability [OR 1.243 (1.074–1.439)].
Conclusion
In a multivariable prospective (predictive) model, FABQ-PA was the only baseline psychological factor that significantly predicted outcome. Future studies should assess whether pre-operative cognitive–behavioural therapy in patients with maladaptive beliefs improves treatment outcome. Psychological disturbance did not significantly predict outcome, but it improved post-operatively in patients with a good outcome and worsened in those with a poor outcome. Rather than being a risk factor for poor outcome, in this group it appeared to be more a consequence of long-standing, unremitting pain that improved when symptoms resolved after successful surgery.
Keywords: Surgical outcome, Predictors, Fear-avoidance beliefs, Catastrophising, Psychological disturbance
Introduction
Low back pain (LBP) is one of the most common musculoskeletal disorders and is a major and costly problem in industrialised countries [1, 2]. In only 5–15 % of all back-related disorders is there a clear concept of the pain pathogenesis [3]. One such pathology concerns degenerative diseases of the lumbar spine associated with compression of the neural elements. These are common in the ageing population and are being encountered with greater frequency as the average life-expectancy increases [4]. In all but the most moderate of cases, the problem is difficult to treat without recourse to surgery [5–8]. The results for a given procedure can vary widely in different patients, despite apparently similar baseline symptoms, function, indications for surgery and surgical techniques used [9]. Unfortunately, performing a technically successful decompression surgery does not necessarily guarantee a good long-term patient outcome in patients suffering from degenerative spinal disorders [10].
Certain individual characteristics and psychological factors are believed to influence the self-rated outcome of surgery in many orthopaedic conditions: factors such as smoking, long duration of LBP, long-term sick leave, comorbidity, depression and work satisfaction have all been identified as predictors of a poor outcome after spine surgery [9, 11]. In recent years, the influence of cognitive–behavioural factors on the outcome of surgery has attracted increasing attention [12–15]. Pain-related fear and catastrophic pain beliefs, the resulting task interruptions and avoidance of painful activity, negative affect and loss of self-esteem can seriously delay recovery from chronic pain [16]. It might therefore be expected that these same factors would be important in influencing the perceptions of pain and disability in post-operative patients. Pain catastrophising is characterised by patients magnifying their feelings about painful situations and constantly thinking about these situations [17, 18]. It also involves feelings of helplessness and incorporates rumination about pain. It has been described as a cognitive style that involves the tendency to misinterpret and exaggerate the threat value of situations [17] or as an exaggerated negative mental set brought to bear during an actual or anticipated painful experience [19]. Pain catastrophising plays an important role in theoretical models of pain chronicity, showing a consistent correlation with both pain intensity and disability [18, 20–22]. It has been shown to be a significant predictor of outcome after knee replacement surgery [12, 23] and treatment for other rheumatologic disorders [21], even after controlling for other well-known psychological risk factors such as depression. Several studies have shown that kinesiophobia/fear-avoidance beliefs also play an important role in the development [24], persistence [25] and response to treatment [26] of chronic low back pain and, like pain catastrophising, show a significant correlation with pain intensity and disability [16, 22]. Although many predictor studies have been carried out to examine the influence of psychological factors such as depression and anxiety on surgical outcome [27], only few have investigated the predictive value of fear-avoidance beliefs [11, 15, 26, 28] and mostly in groups of younger patients in relation to disc surgery. To the authors’ knowledge, the importance of pre-operative pain catastrophising in relation to the outcome of spine surgery has not been investigated to date. Further, no studies have systematically evaluated the changes in these psychological and cognitive–behavioural risk factors after surgery, to assess whether a good outcome is associated with a return to a more favourable psychological profile.
The aim of this study was to investigate the predictive value of cognitive and behavioural factors including pain catastrophising and fear-avoidance beliefs on the 12-month outcome of decompression surgery for degenerative spinal disorders in a group of patients who were otherwise participating in a randomised controlled trial (RCT) of post-operative physical therapy [29]. A further aim was to identify the changes in psychological factors (from before surgery to 12 months later) that were associated with the achievement of a good global outcome at 12 months’ follow-up.
Methods
Study admission criteria
The inclusion criteria for the study were: age over 45 years; diagnosis of degenerative spinal disease with compression of the neural elements (in association with either hard tissue (osteophytes, calcification, etc.) or soft tissue (herniated disc material)) as ascertained from the medical history, clinical examination, conventional radiography and MRI/CT of the lumbar spine, with an indication for decompression surgery without fusion; failed conservative therapy; willingness to complete questionnaire follow-ups; a good understanding of written and spoken German.
The exclusion criteria were: previous spinal fusion (although other types of spinal surgery carried out more than 6 months ago were acceptable) and disorders preventing active rehabilitation (an exclusion criterion related to the original RCT [29]).
Recruitment of patients
Patients were recruited from the spine centre of the authors’ hospital (a not-for-profit orthopaedic clinic with university affiliations). The operation list for the forthcoming 2 months was examined on a weekly basis, and consecutive patients who appeared to satisfy the main admission criteria were sent a letter inviting them to participate, along with an information sheet about the study and a questionnaire booklet (see later). All patients were contacted by phone a week later to enquire about their interest in participating, check the inclusion/exclusion criteria and address any queries in connection with the study. Those who agreed to participate were invited to sign the informed consent form and bring their completed questionnaire to the research department on the day of admission. The study was approved by the local university ethics committee.
Surgical and post-operative procedures
Decompression surgery was carried out using a minimally destructive approach. Briefly, using a posterior midline approach to the laminae, the spinal canal was entered by removal of the ligamentum flavum. Undercutting laminotomy of the caudal and rostral laminae and, where necessary, partial medial facetectomy and removal of disc fragments were performed. No specific rehabilitation was carried out in the first 6–8 weeks, but the patients were encouraged to keep mobile. Between 2 and 5 months post-operatively, the patients completed a rehabilitation programme comprising either self-management (instructed to “keep active”), physiotherapeutic spine segmental stabilisation exercises or traditional mixed physiotherapy techniques. There were no significant differences between rehabilitation groups at follow-up [29], which justified an analysis of all patients together in the present report.
Assessments
Administration of questionnaires
Before and at 12 months after surgery, patients completed the questionnaires sent to them by mail. Non-responders were contacted by study personnel until the questionnaire was returned or the patient explicitly stated that no questionnaire would be returned. All the questionnaires were available in German or had been adapted for the German language prior to the study [30].
Questionnaire
The questionnaire enquired about the following variables, considered to represent potential predictors of outcome (i.e. independent variables):
Socio-demographic and medical history characteristics: age, gender, work status, involvement (past, current or intended) in a disability claim, smoking habit (non-smoker, ex-smoker, smoker), other joint problems (hip, knee, foot, shoulder, elbow, hand or “other”), general health (0–10 graphic rating scale), sleep disturbances (yes, no), number of levels to be operated and previous spine surgery [30]
LBP-related disability measured with the Roland and Morris questionnaire [31, 32]. This is a 24-item questionnaire, used to assess disability due to LBP in relation to various daily functions
Pain characteristics: intensity of the average low back pain (LBP), average leg pain (LP), highest back-related pain and lowest back-related pain in the last week, and back-related pain today, each on a 0–10 graphic rating scale [33]; duration (in months) of back problem; frequency of back-related pain in the last 6 months (never, sometimes, often, constant); use of painkillers in the last 6 months due to back-related pain (none, sometimes (few times/month), often (few times/week), always (daily) [30]
Psychological disturbance [34] determined using the combined scores from the Modified Somatic Perception Questionnaire, MSPQ [35] (enquires about the frequency of somatic symptoms experienced in the last week) and the modified ZUNG Depression Questionnaire [36]
Fear-avoidance beliefs: beliefs about physical activity/work being a cause of the patient’s back trouble and fears about the dangers of such activities when experiencing an episode of low back pain (Fear-Avoidance Beliefs Questionnaire, FABQ [26, 37] (due to the average age of the group, only the FABQ-physical activity (FABQ-PA) scores were used for further analysis)
Catastrophising, using the six items on the catastrophising sub-scale of the Coping Strategies Questionnaire, CSQ [38].
Twelve months after surgery, patients answered a question enquiring about the global outcome of surgery: “How much did the operation help your back problem?,” with five response categories: (1) helped a lot, (2) helped, (3) helped only little, (4) did not help, and (5) made things worse. The global outcome was dichotomised into “good” (responses 1 and 2) and “poor” (responses 3, 4 and 5) for the purpose of subsequent analyses. Global outcome comprised the primary outcome for the study (i.e. the dependent variable in the predictor analyses). This was chosen in preference to, e.g. the change in pain or disability scores at follow-up compared with baseline, since it circumvents the two methodological concerns “mathematical coupling” and “regression to the mean” associated with the relation between change and initial value [39] and avoids potential confounding due to baseline scores of pain/disability, themselves being related to baseline beliefs/psychological variables; further, global outcome has been shown to give a valid and responsive descriptor of overall treatment effect, representing an aggregate of all aspects of outcome that are of most importance to the patient [40].
Statistics
Descriptive statistics were firstly computed for the data. Relative frequencies were calculated for discrete (categorical) variables such as sex, smoking status, etc., and means and standard deviations for continuous variables such as age and the various questionnaire scores (pain catastrophising, fear-avoidance beliefs, etc.). Stem and leaf plots were computed to visually examine the distribution of the data, determine whether any data needed to be transformed and identify missing data.
For some of the variables, the response categories were collapsed for the later analyses to avoid having very small subgroups. For smoking habit, the response categories of 1 = no, 2 = given up and 3 = yes were collapsed into “no” (no and given up; coded as 0) and “yes” (coded as 1). For current employment, response options were (1) yes, full time; (2) yes, part time; (3) yes, part time and part retired; (4) no, out of work; (5) no, housewife; (6) no, retired on age grounds; (7) no, retired due to back pain; (8) no, retired early for reasons other than back pain; (9) no, other reasons. These were dichotomised as 1–3 = yes (coded as 1) and 4–9 = no (coded as 0). For claim for disability, response options were: (1) not applicable (not working); (2) no claim; (3) considering claim; (4) claim submitted; (5) claim granted; (6) claim turned down. These were dichotomised as 1–2 = no (coded as 0) and 3–6 = yes (coded as 1).
Two multiple logistic models were built: one was a true, prospective predictive model, in which baseline variables measured pre-operatively (“predictors”) were examined in relation to the global outcome at the 12-month follow-up; the second was an “explanatory model”, in which changes in a number of different variables (from pre-op to 12 months’ post-op; positive = improvement) were examined in relation to the global outcome, to see what factors or change scores were associated with, or statistically “explained”, a good global outcome.
Univariate logistic regression analyses were firstly applied to all variables of interest to reveal any associations with global outcome (coded as 0 = poor, 1 = good). Variables with a p value <0.10 were considered for inclusion in the subsequent multiple regression model. In the final multiple logistic regression model, odds ratios (OR) for each variable and their 95 % confidence intervals were computed. A backward (likelihood-ratio) model was used to identify the variables that best predicted/explained the global outcome at 12 months after surgery.
Data analysis was performed with SPSS (PASW statistics 18, IBM statistics SPSS18). p values <0.05 were considered to be statistically significant.
Results
Patients
A total of 159 patients were included in the original trial [29]. Details concerning the baseline characteristics of the study group, the proportion of patients completing questionnaires at the 12-month follow-up (96 %) and the methods for dealing with missing questionnaire data/imputation have all been described previously [29]. Eleven patients were re-operated within the first year and their data were excluded from the present analysis, since their ratings of outcome in the questionnaire sent 12 months after the index surgery would clearly have been influenced by the intervening procedure. Hence, questionnaire data from 148 patients were used in the present study. Their mean ± SD age was 64 ± 11 years and 92/143 (64 %) were men.
Global outcome at 12 months
At the 12-month follow-up, the numbers (%) of patients reporting a good and poor outcome, respectively, were 113 (76.4 %) and 35 (23.6 %).
Prospective evaluation of baseline predictors of outcome
The baseline predictors that showed a significant association with global outcome in the univariate logistic regression analyses are shown in Table 1. Briefly, a poor outcome (coded 0 as the dependent variable) was associated (p < 0.10) with: involvement in a disability claim, a higher frequency of LBP, higher LBP intensity in the last week, higher leg pain intensity in the last week, higher value for the average from all pain scales, higher intake of painkillers, having other joint problems, being a smoker, having greater psychological disturbance, having a higher Roland Morris Disability score, a higher FABQ-physical activity score and a higher pain-catastrophising score. Odds ratios for these variables ranged from 0.333 to 0.970 (Table 1).
Table 1.
Baseline factors predicting global outcome (0 = poor, 1 = good) at 12 months’ follow-up
| Variable | 12 Months postop | |||||
|---|---|---|---|---|---|---|
| Individual indicators | Multiple regression | |||||
| OR | 95 % CI | p value | OR | 95 % CI | p value | |
| Age (years) | 1.000 | 0.965; 1.035 | 0.979 | |||
| Gender (0 = F, 1 = M) | 1.127 | 0.518; 2.450 | 0.763 | |||
| Number of levels to be operated (1–5) | 1.043 | 0.681; 1.598 | 0.846 | |||
| Currently employed (0 = N, 1 = Y part or full time) | 2.073 | 0.864; 4.976 | 0.103 | |||
| Claim for disability (0 = N, 1 = Y considering, applied or received) | 0.333 | 0.126; 0.878 | 0.026 | |||
| Time in treatment for back problem (months, log transformed) | 0.905 | 0.704; 1.162 | 0.434 | |||
| Previous spine surgery (0 = N, 1 = Y) | 0.745 | 0.264; 2.100 | 0.577 | |||
| LBP frequency in the past 6 months | 0.341 | 0.146; 0.792 | 0.012 | 0.340 | 0.141; 0.818 | 0.016 |
| Use of painkillers in the previous 6 months | 0.811 | 0.579; 1.135 | 0.222 | |||
| LBP intensity, in the last week | 0.818 | 0.704; 0.950 | 0.009 | |||
| Leg pain intensity, in the last week | 0.850 | 0.716; 1.009 | 0.063 | |||
| Average of all pain scales | 0.728 | 0.585; 0.906 | 0.005 | |||
| Painkillers today | 0.462 | 0.212; 1.003 | 0.051 | |||
| Other joint problems (0 = N, 1 = Y) | 0.448 | 0.192; 1.048 | 0.064 | |||
| Systemic diseases/co-morbidity | 0.974 | 0.446; 2.127 | 0.947 | |||
| General medication for systemic diseases | 1.028 | 0.450; 2.348 | 0.948 | |||
| Sleep disturbance | 0.884 | 0.520; 1.505 | 0.651 | |||
| General health | 1.100 | 0.920; 1.314 | 0.295 | |||
| Smoker (0 = N, 1 = Y) | 0.403 | 0.162; 1.006 | 0.051 | |||
| Psychological distress, sum of MSPQ + ZUNG | 0.970 | 0.938; 1.003 | 0.078 | |||
| Roland Morris Disability (range 0–24) | 0.923 | 0.851; 1.001 | 0.054 | |||
| FABQ-physical activity (range 0–28) | 0.879 | 0.815; 0.949 | 0.001 | 0.877 | 0.809; 0.949 | 0.001 |
| Pain catastrophising (range 0–36) | 0.949 | 0.901; 0.999 | 0.046 | |||
LBP low back pain, MSPQ Modified Somatic Perception Questionnaire (enquires about the frequency of somatic symptoms experienced in the last week), ZUNG ZUNG self-rated depression, FABQ-physical activity Fear-Avoidance Beliefs about physical activity
p values marked in bold are p < 0.10 for the individual indicators (selected for multivariable model) and p < 0.05 for the multivariable model
Multivariable logistic regression analysis revealed that, of the baseline psychological factors, only FABQ-physical activity was a significant predictor of outcome at the 12-month follow-up; frequency of LBP was the only other unique predictor in the model (Table 1).
Association between outcome and change scores from before to 12 months after surgery
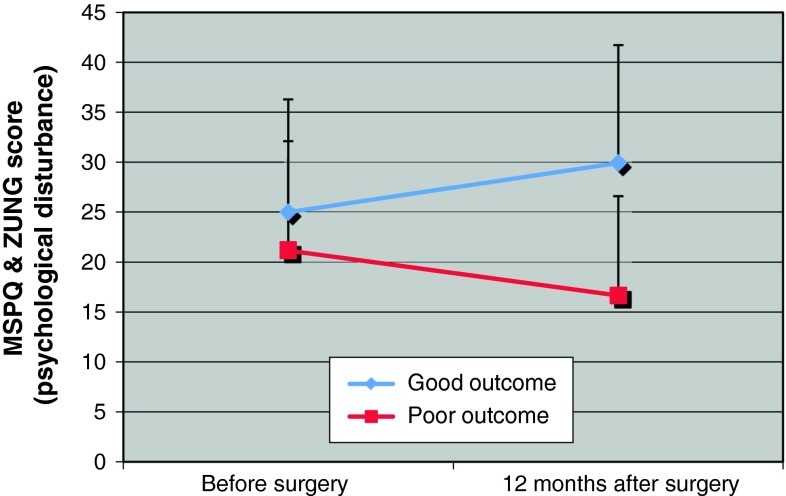
The association between change scores (i.e. the difference between pre-operative and 12 months’ post-operative scores, where positive values = improvement) and the global outcome are shown in Table 2 for both univariable and multivariable analyses. In multiple logistic regression, improvement in each of the following variables was significantly associated with a good outcome: average LBP in the last week, average of all pain scales, general health, psychological disturbance (sum of MSPQ and ZUNG) and Roland Morris disability score. The association between outcome and the change scores is exemplified in Fig. 1, which shows the change in “psychological disturbance” (sum of MSPQ and ZUNG scores) from baseline (pre-operatively) to the 12-month follow-up in the “good outcome” and “poor outcome” groups. The baseline scores did not differ markedly between the outcome groups (confirming the lack of predictive power for pre-operative psychological disturbance), but there was a marked separation (and significant difference; p < 0.0001) in scores indicating improvement and deterioration for “good” and “poor” groups, respectively, at the 12-month follow-up.
Table 2.
Association between improvement in scores (from preop to 12 months’ follow-up) and global outcome (0 = poor, 1 = good) at 12 months’ follow-up
| Variable | 12 Months postoperatively | |||||
|---|---|---|---|---|---|---|
| Individual indicators | Multiple regression | |||||
| Change scorea preop to 12 mo postop in | OR | 95 % CI | p value | OR | 95 % CI | p value |
| Average LBP in the last week | 1.346 | 1.151; 1.574 | <0.0001 | |||
| Average leg pain in the last week | 1.577 | 1.309; 1.900 | <0.0001 | |||
| Average of all pain scales | 2.073 | 1.564; 2.746 | <0.0001 | 1.687 | 1.187; 2.398 | 0.004 |
| General health | 1.303 | 1.108; 1.532 | 0.001 | 1.246 | 1.004; 1.545 | 0.045 |
| MSPQ + ZUNG (psychological disturbance) | 1.127 | 1.070; 1.187 | <0.0001 | 1.073 | 1.006; 1.144 | 0.033 |
| Roland Morris Disability | 1.396 | 1.225; 1.591 | <0.0001 | 1.243 | 1.074; 1.439 | 0.004 |
| FABQ-physical activity | 1.087 | 1.030; 1.148 | 0.002 | |||
| Catastrophising | 1.151 | 1.069; 1.241 | <0.0001 | |||
FABQ-physical activity Fear-avoidance beliefs about physical activity, LBP low back pain, MSPQ Modified Somatic Perception Questionnaire (enquires about the frequency of somatic symptoms experienced in the last week), ZUNG ZUNG self-rated depression
aThe change scores (preop to 12 months postop) were calculated such that a positive value indicated an improved status (i.e. reduced pain, better general health, reduced catastrophising, etc.)
Fig. 1.
The change in “psychological disturbance” (sum of MSPQ and ZUNG scores) from baseline (preoperatively) to 1-year follow-up in the “good outcome” and “poor outcome” groups (p = 0.0001 for the difference in change scores between the groups)
Discussion
The present study sought to examine the role of cognitive–behavioural factors in identifying patients at higher risk of a poor outcome after decompression surgery for lumbar spine degenerative disorders. Higher levels of fear-avoidance beliefs about physical activity (FABQ-PA) were shown to have significant predictive value for a poor 12-month outcome after surgery. The findings concur with many (but not all [41]) previous studies on patients with chronic back problems who have reported a significant negative influence of pre-treatment fear-avoidance beliefs (about work or physical activity) on outcome after conservative [42] or surgical [13, 15, 26, 28] treatment, with outcome being measured using different variables (disability/function [13, 42], a multidimensional index [28], return to work [26] or quality of life [15]). In the present study, FABQ-PA was the only statistically significant and also clinically useful predictor variable identified, i.e. factor that is potentially modifiable prior to surgery (see later).
We hypothesised that one or more of the specific psychological variables or health-related beliefs that we studied would predict a poor surgical outcome. As also reported previously in the literature [22], there were a number of significant inter-correlations between the various psychological variables. Conceivably, had fear-avoidance beliefs not been measured, then a closely related variable such as pain catastrophising, which was significant in the univariate analysis and has been identified as a predictor of outcome of orthopaedic surgery in previous studies [12, 23], may instead have acquired significance in the multivariable model. However, the close relationship between these variables meant that ultimately only one was selected for inclusion in the final model.
The results suggest that pre-operative screening for psychosocial risk factors such as fear-avoidance beliefs that predict poor outcome may be useful to identify individuals who would benefit from adjunctive treatments [21]. It would be interesting to examine whether the introduction of educational and psychological treatments to address negative beliefs pre-operatively in those who exhibit high levels of fear avoidance—as a type of “prehabilitation”—might improve the ultimate outcome of surgery. Rather than excluding psychologically disturbed, distressed or fear-avoidant patients from surgery, prehabilitation would be seen as part of the preparation procedure for surgery, just as for example giving up smoking or losing weight is sometimes advised. This might serve to maximise the overall number of successes. Studies in other fields of orthopaedics, such as knee surgery, have already shown the effectiveness of pre-operative pain-coping skills training for patients with pain catastrophising [43]. Pain catastrophising was shown in earlier studies to represent a significant predictor of outcome after knee arthroplasty [23] and patients that received coping skills training reported significantly greater reductions in pain severity and catastrophising and greater improvements in function post-operatively, when compared with a standard care cohort [43].
In the present study, the multivariable “change score model” indicated that improvements in the average pain score from all pain scales, general health, psychological disturbance and Roland Morris Disability scores were each statistically associated with a good global outcome after surgery (i.e. each made a unique significant contribution to explaining the variance in global outcome). That improvements in these variables explained (statistically) a good global outcome is completely logical. Pain, function, general well-being and positive mental health represent some of the key domains considered by many to be of greatest importance as condition-specific outcomes in spinal disorders/back pain [44]. Hence, changes in these variables would be expected to be the most relevant indicators of successful surgery, as judged by the global outcome rating. If these variables had not changed, it would be unlikely that the global outcome would have been rated as “good” by the patient. In other words, reducing the amount of pain, facilitating functioning in everyday life and achieving a feeling of well-being represent the main aims of surgery and consequently define a good outcome. This provides further evidence to support the validity of the “global treatment outcome” item in representing an aggregate measure of all aspects of outcome of importance to the patient [40].
Psychological distress has long been known to be associated with pain chronicity [45, 46]. Our own finding of elevated pre-operative levels of psychological disturbance in our highly symptomatic patients with chronic pain also supports this (see Fig. 1). Many studies [27], but by no means all [47], have shown that pre-operative psychological distress predisposes to a poor outcome of surgery. Our data failed to support the notion of pre-operative psychological disturbance being a significant negative predictor of surgical outcome: as illustrated in Fig. 1, the scores for psychological disturbance (MSPQ + ZUNG scores) did not differ markedly between the outcome groups at baseline. Possibly, the relevance of depression or psychological disturbance as a predictor of outcome depends on the severity of the pathology, the clarity and certainty of the indication for surgery, the appropriateness of surgery for the given “pathology” and other factors [37]. It would appear to have a greater predictive role in patients with less marked pathological changes and less certain indications [9, 37, 46]. In the present study, given that the scores improved in patients who had a good outcome of surgery (and worsened in those with a poor outcome), we interpreted psychological disturbance as being the natural response to long-standing pain/disability that subsided once the pain was diminished post-operatively and the patient was able to function more normally again.
To the author’s knowledge, few studies in the literature have investigated the dynamic interplay between psychological factors and outcome in patients undergoing surgery for degenerative diseases of the lumbar spine. As mentioned earlier, a number of studies have examined psychological distress and/or fear-avoidance beliefs pre-operatively, but few have reported the changes that occur in response to successful (or otherwise) surgery. To our knowledge, just one other study [41] has examined the association between treatment outcome (measured as pain intensity, pain interference, disability or physical health) and post-operative changes in depression/fear of movement, and the findings were similar to those reported here, namely that depression and maladaptive beliefs were increased in patients with a poorer outcome and decreased in those with a good outcome.
Our study had a number of limitations. First, patients had been assigned to three different types of post-operative rehabilitation, which could potentially have influenced the surgical outcome recorded at the 12-month follow-up. However, our previous studies had already confirmed that the type of rehabilitation had no influence on global outcome at any stage up to 2 years post-operatively [29] and we therefore considered it unlikely that this would represent a confounder in the current study and pooled the data accordingly. A 12-month follow-up was chosen as the end point for prediction for the present study because the longer the time elapsed before the baseline measure and the event being predicted (status at 12 months), the greater the likelihood that other factors will serve to influence the outcome (e.g., development of further degenerative problems, other joint problems and so on). It was not possible to account for all potential predictors that might have explained surgical outcome (e.g., medication, baseline medical/clinical status, imaging, etc.), as there would have been far too many to consider, thereby reducing the power of the study to quantify the role of the variables it particularly sought to investigate (psychological/beliefs). We had a rather high threshold for classifying the outcome as “good”, when dichotomising the global outcome responses. We only considered the outcome of surgery to be “good” if the patient reported that the operation helped a lot or helped; “helped only little”, although still a positive response, was not considered a good outcome for this elective procedure, as previously recommended [48]. Other studies have considered, e.g. “somewhat better than 1 year ago” [49] as a good outcome. It has been shown that the proportion of patients that can be considered a success after surgery as well as the factors that might predict a good outcome depend on how success is defined [9, 50].
Conclusion
In a prospective model, baseline fear-avoidance beliefs about physical activity was the only statistically significant psychological factor predicting surgical outcome. Increasing frequency of LBP at baseline was an additional unique predictor of outcome, but is not a modifiable entity and cannot therefore be manipulated in an attempt to improve outcomes. A knowledge of its negative influence on outcome might, however, be used to guide the patient’s informed consent process prior to surgery. Future studies should focus on educational and psychological treatments to address maladaptive beliefs in those patients who exhibit high levels pre-operatively. This kind of prehabilitation could potentially improve the global outcome of surgery and would be preferable to an approach where patients with an “inappropriate” psychological profile are deterred from having what would otherwise be considered as appropriate surgery.
Baseline psychological disturbance had no predictive power regarding the future surgical outcome. However, at 12 months’ follow-up, patients with a good outcome showed a marked improvement in their psychological status, whilst those with a poor outcome showed a worsening. In the group of patients studied here, psychological disturbance thus appeared to be the consequence of a long-standing back problem, diminishing hand-in-hand with the decrease in symptoms after successful surgery, but being exacerbated by a poor surgical outcome.
Acknowledgments
This study was supported by the Swiss National Science Foundation (Grant no. 32-57123.99) and the Schulthess Klinik Research Fund. We are grateful to Renata Heusser, Gordana Balaban and Katrin Knecht (Schulthess Klinik) for their valuable assistance in collecting the questionnaire data. We also thank Astrid Junge, PhD (Schulthess Klinik) for her help in planning the original questionnaire battery, and Malgorzata Roos, PhD (Division of Biostatistics, Institute of Social and Preventive Medicine, University of Zurich) for her statistical advice and support in analysing the data.
Conflict of interest
None.
References
- 1.Deyo RA, Phillips WR. Low back pain. A primary care challenge. Spine (Phila Pa 1976) 1996;21:2826–2832. doi: 10.1097/00007632-199612150-00003. [DOI] [PubMed] [Google Scholar]
- 2.Waddell G. Low back pain: a twentieth century health care enigma. Spine (Phila Pa 1976) 1996;21:2820–2825. doi: 10.1097/00007632-199612150-00002. [DOI] [PubMed] [Google Scholar]
- 3.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–S300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathers CD, Sadana R, Salomon JA, Murray CJ, Lopez AD. Healthy life expectancy in 191 countries, 1999. Lancet. 2001;357:1685–1691. doi: 10.1016/S0140-6736(00)04824-8. [DOI] [PubMed] [Google Scholar]
- 5.Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F. Lumbar spinal stenosis: conservative or surgical management?: a prospective 10-year study. Spine (Phila Pa 1976) 2000;25:1424–1435. doi: 10.1097/00007632-200006010-00016. [DOI] [PubMed] [Google Scholar]
- 6.Lurie JD, Spratt KF, Blood EA, Tosteson TD, Tosteson AN, Weinstein JN. Effects of Viewing an Evidence-Based Video Decision Aid on Patients’ Treatment Preferences for Spine Surgery. Spine (Phila Pa 1976) 2011;36(18):1501–1504. doi: 10.1097/BRS.0b013e3182055c1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benoist M. The natural history of lumbar degenerative spinal stenosis. Jt Bone Spine. 2002;69:450–457. doi: 10.1016/S1297-319X(02)00429-3. [DOI] [PubMed] [Google Scholar]
- 8.Herno A, Airaksinen O, Saari T, Luukkonen M. Lumbar spinal stenosis: a matched-pair study of operated and non-operated patients. Br J Neurosurg. 1996;10:461–465. doi: 10.1080/02688699647087. [DOI] [PubMed] [Google Scholar]
- 9.Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15(Suppl 1):S93–S108. doi: 10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katz JN, Lipson SJ, Chang LC, Levine SA, Fossel AH, Liang MH. Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 1996;21:92–98. doi: 10.1097/00007632-199601010-00022. [DOI] [PubMed] [Google Scholar]
- 11.den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15:527–536. doi: 10.1007/s00586-005-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008;13:335–341. doi: 10.1155/2008/730951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.den Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW. Continued disability and pain after lumbar disc surgery: the role of cognitive–behavioral factors. Pain. 2006;123:45–52. doi: 10.1016/j.pain.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 14.den Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW. Reduced work capacity after lumbar disc surgery: the role of cognitive–behavioral and work-related risk factors. Pain. 2006;126:72–78. doi: 10.1016/j.pain.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Johansson AC, Linton SJ, Rosenblad A, Bergkvist L, Nilsson O. A prospective study of cognitive behavioural factors as predictors of pain, disability and quality of life one year after lumbar disc surgery. Disabil Rehabil. 2010;32:521–529. doi: 10.3109/09638280903177243. [DOI] [PubMed] [Google Scholar]
- 16.Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, Karoly P. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28:475–483. doi: 10.1097/AJP.0b013e3182385392. [DOI] [PubMed] [Google Scholar]
- 17.Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the pain catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. Pain. 2002;96:319–324. doi: 10.1016/S0304-3959(01)00463-8. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan MJ, Stanish W, Waite H, Sullivan M, Tripp DA. Catastrophizing, pain, and disability in patients with soft-tissue injuries. Pain. 1998;77:253–260. doi: 10.1016/S0304-3959(98)00097-9. [DOI] [PubMed] [Google Scholar]
- 20.Swinkels-Meewisse IE, Roelofs J, Oostendorp RA, Verbeek AL, Vlaeyen JW. Acute low back pain: pain-related fear and pain catastrophizing influence physical performance and perceived disability. Pain. 2006;120:36–43. doi: 10.1016/j.pain.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Edwards RR, Bingham CO, 3rd, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006;55:325–332. doi: 10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- 22.Meyer K, Tschopp A, Sprott H, Mannion AF. Association between catastrophizing and self-rated pain and disability in patients with chronic low back pain. J Rehabil Med. 2009;41:620–625. doi: 10.2340/16501977-0395. [DOI] [PubMed] [Google Scholar]
- 23.Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2010;468:798–806. doi: 10.1007/s11999-009-0963-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94:7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 25.Peters ML, Vlaeyen JW, Weber WE. The joint contribution of physical pathology, pain-related fear and catastrophizing to chronic back pain disability. Pain. 2005;113:45–50. doi: 10.1016/j.pain.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 26.Staerkle R, Mannion AF, Elfering A, Junge A, Semmer NK, Jacobshagen N, Grob D, Dvorak J, Boos N. Longitudinal validation of the fear-avoidance beliefs questionnaire (FABQ) in a Swiss–German sample of low back pain patients. Eur Spine J. 2004;13:332–340. doi: 10.1007/s00586-003-0663-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Celestin J, Edwards RR, Jamison RN. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: a systematic review and literature synthesis. Pain Med. 2009;10:639–653. doi: 10.1111/j.1526-4637.2009.00632.x. [DOI] [PubMed] [Google Scholar]
- 28.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Dvorak J, Jacobshagen N, Semmer NK, Boos N. Predictors of multidimensional outcome after spinal surgery. Eur Spine J. 2007;16:777–786. doi: 10.1007/s00586-006-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mannion AF, Denzler R, Dvorak J, Muntener M, Grob D. A randomised controlled trial of post-operative rehabilitation after surgical decompression of the lumbar spine. Eur Spine J. 2007;16:1101–1117. doi: 10.1007/s00586-007-0399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mannion AF, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine (Phila Pa 1976) 1999;24:2435–2448. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- 31.Roland M, Morris R. A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine (Phila Pa 1976) 1983;8:145–150. doi: 10.1097/00007632-198303000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Exner V, Keel P. Measuring disability of patients with low-back pain—validation of a German version of the Roland and Morris disability questionnaire. Schmerz. 2000;14:392–400. doi: 10.1007/s004820070004. [DOI] [PubMed] [Google Scholar]
- 33.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17–S24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greenough CG, Fraser RD. Comparison of eight psychometric instruments in unselected patients with back pain. Spine (Phila Pa 1976) 1991;16:1068–1074. doi: 10.1097/00007632-199109000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Main CJ. The Modified Somatic Perception Questionnaire (MSPQ) J Psychosom Res. 1983;27:503–514. doi: 10.1016/0022-3999(83)90040-5. [DOI] [PubMed] [Google Scholar]
- 36.Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. 1965;13:508–515. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
- 37.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 38.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 39.Tu YK, Gilthorpe MS. Revisiting the relation between change and initial value: a review and evaluation. Stat Med. 2007;26:443–457. doi: 10.1002/sim.2538. [DOI] [PubMed] [Google Scholar]
- 40.Hagg A, Fritzell P, Oden A, Nordwall A. Simplifying outcome measurement: evaluation of instruments for measuring outcome after fusion surgery for chronic low back pain. Spine. 2002;27:1213–1222. doi: 10.1097/00007632-200206010-00014. [DOI] [PubMed] [Google Scholar]
- 41.Archer KR, Wegener ST, Seebach C, Song Y, Skolasky RL, Thornton C, Khanna AJ, Riley LH., 3rd The Effect of Fear-Avoidance Beliefs on Pain and Disability after Surgery for Lumbar and Cervical Degenerative Conditions. Spine (Phila Pa 1976) 2011;36(19):1554–1562. doi: 10.1097/BRS.0b013e3181f8c6f4. [DOI] [PubMed] [Google Scholar]
- 42.Pfingsten M, Leibing E, Franz C, Bansemer D, Busch O, Hildebrandt J. Fear-avoidance-beliefs in patients with back pain. Schmerz. 1997;11:387–395. doi: 10.1007/s004820050114. [DOI] [PubMed] [Google Scholar]
- 43.Riddle DL, Keefe FJ, Nay WT, McKee D, Attarian DE, Jensen MP. Pain coping skills training for patients with elevated pain catastrophizing who are scheduled for knee arthroplasty: a quasi-experimental study. Arch Phys Med Rehabil. 2011;92:859–865. doi: 10.1016/j.apmr.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 1998;23:2003–2013. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 45.Main CJ, Waddell G. The detection of psychological abnormality in chronic low back pain using four simple scales. Curr Concepts Pain. 1984;2:10–15. [Google Scholar]
- 46.Carragee E. Indications for lumbar microdiskectomy. Instr Course Lect. 2002;51:223–228. [PubMed] [Google Scholar]
- 47.Hagg O, Fritzell P, Ekselius L, Nordwall A. Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish Lumbar Spine Study. Eur Spine J. 2003;12:22–33. doi: 10.1007/s00586-002-0465-z. [DOI] [PubMed] [Google Scholar]
- 48.Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D. The quality of spine surgery from the patient’s perspective: Part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur Spine J. 2009;18:374–379. doi: 10.1007/s00586-009-0931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Campbell H, Rivero-Arias O, Johnston K, Gray A, Fairbank J, Frost H. Responsiveness of objective, disease-specific, and generic outcome measures in patients with chronic low back pain: an assessment for improving, stable, and deteriorating patients. Spine (Phila Pa 1976) 2006;31:815–822. doi: 10.1097/01.brs.0000207257.64215.03. [DOI] [PubMed] [Google Scholar]
- 50.Schade V, Semmer N, Main CJ, Hora J, Boos N. The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain. 1999;80:239–249. doi: 10.1016/S0304-3959(98)00210-3. [DOI] [PubMed] [Google Scholar]