Abstract
Background
The [13C]-Spirulina platensis gastric emptying breath test (GEBT) with 5 samples is accurate relative to scintigraphy. This study was primarily designed to further validate this GEBT using a slightly different process for incorporating [13C] in Spirulina and to evaluate the utility of additional samples for assessing early gastric emptying.
Methods
After a 223 kcal test meal labeled with 99mTc and [13C]-Spirulina platensis, scintigraphic images and 5 breath samples (45, 90, 120, 180, and 240 minutes, GEBT5) were collected in 14 controls (Part A). In Part B, 9 breath samples were collected at 15, 30, 45, 60, 90, 120, 150, 180, and 240 minutes (GEBT9) in 30 subjects (15 controls, 15 dyspepsia). Using correlation between [13C] breath excretion and scintigraphic emptying, lag time (t10, time for 10% emptying), emptying at 30 min (GE30), and half time (t50) were estimated for GEBT5 (Parts A and B) and GEBT9 (Part B).
Key Results
t50 values for scintigraphy, GEBT5, and GEBT9 were highly concordant. t10 by GEBT9 (90% CI, 6–15 minutes) was more strongly correlated (CCC 0.80 [95% CI, 0.63–0.90]) with scintigraphy (90% CI, 5–12 minutes), than GEBT5 (10–19 minutes, CCC 0.73 [95% CI, 0.54–0.85]). The correlation between estimated values (GEBT9) and linearly interpolated values (GEBT5) was closer at 60 (CCC 0.95 [95% CI, 0.91–0.97]) than 30 minutes (CCC 0.81 [95% CI, 0.71–0.89]).
Conclusions & Inferences
The [13C]-Spirulina platensis GEBT can accurately measure GE. While 5 and 9 samples are equally accurate for measuring t50, GEBT9 provides a more comprehensive assessment of early GE (t10 and GE30).
Keywords: Breath test, Dumping, Dyspepsia, Gastric emptying, Gastroparesis
INTRODUCTION
Compared to current scintigraphic methods, the measurement of gastric emptying (GE) by stable isotope gastric emptying breath tests (GEBT) has practical and safety advantages. In contrast to scintigraphy, GEBT does not require elaborate detection equipment and can be performed at the point of care, as in the office or bedside, because the collected breath samples are collected simply with a straw and sealable container, and the excreted 13CO2 is stable. Samples can be sent to a remote site for analysis. In addition, GEBT does not entail radiation exposure, and is safer than scintigraphy, particularly if repeated assessments are required, or, when GE needs to be assessed in pregnant or breast feeding women and in children. Our group has previously focused on developing an accurate mathematical analysis (1) and reducing the number of breath samples necessary, thereby reducing the cost of the test. Using 5 breath samples over 3 hours (i.e., before as also 45, 90, 120, and 180 minutes after a meal), we showed that the intra- and inter-individual coefficients of variation for gastric emptying half time (t50) measured by [13C]-octanoate and [13C]-Spirulina platensis GEBT were comparable to corresponding values for scintigraphy (2–6). The most recent version of the [13C]-Spirulina platensis GEBT uses a standardized test meal with shelf-stable components including [13C]-Spirulina platensis (7) that was validated against scintigraphy in healthy subjects, patients with accelerated and delayed gastric emptying, and healthy subjects with atropine-induced delayed gastric emptying (6). The GEBT has been endorsed by consensus statements issued by the American and European Neurogastroenterology and Motility societies (8).
There is increasing recognition that rapid gastric emptying may occur not only in diabetes mellitus or after fundoplication but also in patients with functional diarrhea, functional dyspepsia, and autonomic dysfunction (9–17) We have observed that some patients with rapid early gastric emptying (e.g., at 30 or 60 minutes) have a normal gastric emptying t50 probably because the emptying rate slows after the initial rapid phase. It is conceivable that early (i.e., at 15, 30, and 60 minutes) and late (i.e., at 240 minutes) postprandial breath samples will increase the accuracy of the GEBT for identifying rapid and delayed gastric emptying relative to scintigraphy respectively.
By growing S. platensis in a closed hydroponics chamber charged with a pure source of 13C, the cellular content of 13C is increased to 99% (7). In comparison to a previous study validating the [13C]-Spirulina platensis GEBT (6), this study utilized a slightly modified algal growth process to enhance the yield and process efficiency. Hence, the specific aims of this study were: to 1) to estimate normal ranges for scintigraphy with this test meal; 2) to appraise the performance characteristics (inter-individual coefficients of variation (CV) of both scintigraphy and [13C]-Spirulina platensis GEBT) in healthy volunteers; 3) to assess the ability of the [13C]-Spirulina platensis GEBT breath kPCD (percent dose excreted *1000) values to predict scintigraphic GE proportions at the different times, and hence to measure GE t10, GE at 30 minutes, and t50; 4) to categorize GE as delayed, normal or accelerated, and 5) to ascertain whether additional early postprandial breath samples increase the accuracy of characterizing the early phase of gastric emptying;
METHODS
Experimental Design
This is a report of 2 prospective, open-label comparison validation studies which were approved by the Mayo Clinic Institutional Review Board. In both studies, gastric emptying was simultaneously evaluated by the [13C]-Spirulina platensis GEBT and scintigraphy. In the first study labeled, Part A, breath samples and scintigraphic images were obtained at 5 time points in 14 healthy subjects. Thereafter, we were prompted, by increasing awareness of rapid gastric emptying in our clinical practice, to assess the potential utility of collecting additional samples after the GEBT5 study was completed. Hence, breath samples and scintigraphic images were obtained at 9 specific time points in the second study, (“Part B”), in 30 participants – 15 healthy subjects and 15 patients with symptoms of dyspepsia;
Eligibility Criteria for Participants
Patients and healthy volunteers were recruited through public advertisement and a clinic. Participants (males and females) were aged 18–70 years and did not have clinically significant cardiovascular, respiratory, renal, hepatic, gastrointestinal, hematological, neurological, psychiatric or other disease that may interfere with the study. Other exclusion criteria were a history of abdominal surgery other than appendectomy, cholecystectomy, tubal ligation, or hysterectomy; use of any medications that alter GI motility within two days of the study; any allergies to eggs, wheat, or milk or unwilling to consume such products; or receipt of an investigational drug within 30 days prior to the study. While healthy subjects did not have symptoms of a functional GI disorder by questionnaire, patients had symptom criteria for functional dyspepsia (18). Participants were excluded if they had severe nausea or vomiting precluding study assessments; any history of malabsorption due to mucosal disease, pancreatic disease, liver dysfunction, or other causes.
Procedures
All participants had an interview and physical examination and completed questionnaires. (i.e, Hospital Anxiety and Depression Questionnaire and gastrointestinal symptom questionnaires based on Rome III criteria) (18, 19). Healthy subjects did not have symptom criteria for functional dyspepsia or a functional bowel disorder. Patients had Rome III symptom criteria for dyspepsia. In women of child-bearing potential, a negative urine pregnancy test was required within 48 hours of the gastric emptying test. After an overnight fast (minimum 8 hours), the dual-label GE test was performed at the study center. Patients consumed the test meal containing 13C-Spirulina and 99mTc sulfur colloid in no more than 10 minutes. Scintigraphic images and breath samples were obtained upon completion of the meal and at 45, 90, 120, 150, and 180 minutes after the meal in Part A or at 15, 30, 45, 60, 90, 120, 150, 180, and 240 minutes after the meal in Part B. In both Parts A and B, a breath sample was also collected before the test meal. Gastric images were acquired with sequential 2-minute anterior and posterior images in the standing position with a single-head camera. The breath samples were collected while the posterior image was being acquired.
Test Meal
The test meal consisted of 27 g freeze dried egg mix, 6 saltine crackers, and 180 mL of water. The caloric content of the meal is 223 kcal, and the meal has a balanced composition of 19.2 g carbohydrates, 12 g protein, and 10.9 g fat. The nature and size of the meal were selected to ensure stability at room temperature, palatability, and calorie content that would be consumed entirely, even by patients with suspected gastroparesis and upper abdominal symptoms. The meal was labeled with 0.5 mCi 99mTc-sulphur colloid and 100 mg of 13C-Spirulina platensis, with a 13C content of 43%.
Substrate for 13CO2 Breath Test (13C-Spirulina platensis)
S. platensis is a protein-rich, blue-green algae eaten as a food source in many parts of the world, and is sold as a dietary supplement in the United States (20, 21). It contains 50–60% protein, 30% starch, and 10% lipid (22). The natural level of 13C in S. platensis and in all living things is about 1% (23). The S. platensis used in this study was grown in a closed hydroponics chamber charged with pure 13C-source, raising the level of 13C in the resultant cells to 99% (7). In an attempt to enhance the yield and process efficiency, this algal growth process was slightly modified from the previous study utilizing additional culture agitation and an abbreviated harvest procedure. The 13C content and distribution of 13C-labeled protein, carbohydrate and lipids was comparable to prior lots (6). Because the contents of the algal cells are not freely diffusible, incorporation of 13C-labeled S. platensis into the egg mix provides a way to assess the emptying of the solid phase of the meal. 13C can only be released from the algal cells after the egg mix is emptied from the stomach, the cells are digested, and the 13C-labeled substrates (algal protein, fat, and carbohydrate) are absorbed and metabolized. In this way, 13C-S. platensis gives rise to respiratory CO2 that is enriched in 13C.
Measurement of Breath 13CO2 during [13C]-Spirulina platensis GEBT
Breath samples were taken at baseline before the meal and thereafter on the same time schedule as the scintigraphic procedures. End-tidal breath samples were collected while the participant’s abdomen was being imaged by the gamma camera. Breath samples were stored in duplicate in glass screwcap Exetainer® tubes (Labco Limited, High Wycombe, U.K.) using a straw to blow into the bottom of the tube to displace contained air. After re-capping the tubes, the 13CO2 breath content was determined in a centralized laboratory (AB Diagnostics, Brentwood, TN) by Gas Isotope Ratio Mass Spectrometry. The 13C enrichment was expressed as the delta per mL difference between the 13CO2/12CO2 ratio of the sample and the standard. To calculate the quantity of 13C appearing in breath per unit time, delta over baseline (DOB) was used where: 0.0112372 is the isotopic abundance of the limestone standard, Pee Dee Belemnite, and CO2 production was corrected for age, sex, height and weight using the algorithms of Schofield et al., as described by Klein et al. (24).
Analysis of GEBT and Scintigraphy Data
A. GEBT
The currently preferred GEBT metric is the percent dose (abbreviated PCD) excreted at time t after consumption of the test meal (25). To provide a more convenient scale, we multiply PCD by 1000 to produce kPCD at any time, t.
where:
DOB = The measured difference in the ratio [13CO2/12CO2] between a post-meal breath specimen at any time (t-minutes) and the baseline breath specimen.
CO2 PR = CO2 Production Rate (mmol CO2/min) calculated using Schofield equations (26) which incorporate the patient’s age, gender, height and weight.
Rs = The ratio [13CO2/12CO2] in the reference standard (Pee Dee belemnite) for these measurements, Rs = 0.0112372
13 = the atomic weight of Carbon-13
10 = A constant factor for converting units
dose = the weight (mg) of Carbon-13 in the dose of [13C]-S. platensis administered to the patient in the test meal. Since [13C]-Spirulina platensis is approximately 43% Carbon-13, a dose of 100 mg [13C]-Spirulina platensis corresponds to approximately 43 mg of Carbon-13.
B. Scintigraphy
A region of interest (ROI) was drawn around the stomach on the anterior and posterior images for each time frame. Data were corrected for decay of 99mTc. To correct for depth or tissue attenuation, the counts of each anterior and posterior ROI were multiplied together and the square root of the product was taken to obtain the geometric mean. The scintigraphic GE metric, Propt, is the proportion of tracer emptied from the stomach at time, t. A linear interpolation was used to estimate the gastric emptying t50 values for each subject (i.e. linearly interpolate between the GE proportions around 0.5 to estimate the value corresponding to emptying of 50% of the meal.
C. Statistical Methods
The individual proportions of gastric emptying at each time point and the calculated t values obtained from scintigraphic data in 30 subjects were summarized. The 10th and 90th percentile values in healthy volunteers for 5 sample and separately 9 sample data were used to define normal, delayed, and accelerated GE. Because there were only 15 healthy subjects for 9 sample data, more accurate estimates of 10th and 90th percentiles can be obtained than for 5th and 95th percentiles. The pairwise correlations between scintigraphic GE proportions and GEBT kPCD values were estimated.
Since the generalizability of discriminant models is limited by differences in study populations, a bootstrap validation approach was used to generate a multiple linear regression model predicting the scintigraphic GE proportion at each time point (dependent variable) from GEBT kPCD values; gender and BMI were covariates. A total of 200 bootstrap samples was used to obtain a final model to predict the individual scintigraphic GE proportions at each of 9 time points using the set of 9 kPCD values (i.e., Part B) and separately, at each of 5 time points (i.e., the corresponding 5 time points from Part A and the same 5 time points in Part B) (27). Including the baseline sample, a total of 6 and 10 breath samples were obtained. However, since only post baseline kPCD values were used in the models, these models are referred to as 5 sample and 9 sample models respectively. From the predicted GE proportions, a breath test estimate of the corresponding t50 values could be computed using the linear interpolation approach (as described above). The lag time which was estimated as the time required for 10% GE (t10), could also be estimated from the scintgraphic proportions remaining and the corresponding GEBT estimated proportions again using linear interpolation. The agreement between the scintigraphic and GEBT estimated t50 and t10 values was then assessed (Lin’s concordance correlation coefficient [CCC]) (28) and a Bland – Altman plot generated in order to examine whether this would be a useful method to estimate gastric emptying t50 values for use in clinical practice or research. The GEBT predicted values obtained from the 9 time-point model (Part B) were compared with breath test predicted t50 values from the 5 time-point model (Parts A and B). The SAS/STAT® software package (version 9.2, SAS Institute Inc., Cary, NC) was used for all statistical analyses.
RESULTS
Clinical Characteristics
There were 14 healthy subjects in Part A and 15 healthy subjects and 15 patients in Part B (Table 1). All patients had symptoms of dyspepsia by Rome III criteria; 6 had postprandial distress syndrome, 2 had epigastric pain syndrome, and 7 had both. In addition, 6 had diabetes mellitus (DM, 4 of whom had type 2 DM), 2 had an autonomic neuropathy, and 3 had a cholecystectomy. Seven patients, including 4 with DM, had a history of delayed gastric emptying. Malabsorption and significant liver disease were excluded by reviewing the medical history and clinical records respectively.
Table 1.
Demographic Features
| Males | Females | |
|---|---|---|
| Part A (5 breath sample GEBT) | ||
| N (Healthy subjects) | 5 | 9 |
| Median age (IQR) years | 29.0 (26.0, 30.6) | 31.9 (26.8, 41.1) |
| Median body mass index (IQR) kg/m2 | 26.0 (25.1, 26.1) | 24.2 (23.5, 27.0) |
| Part B (9 breath sample GEBT) | ||
| N (Total, healthy subjects, patients) | 10, 5, 5 | 20, 10, 10 |
| Median age (IQR) years | 41.5 (23.0, 52.0) | 46.5 (29.9, 54.0) |
| Median body mass index (IQR) kg/m2 | 24.3 (22.1, 29.5) | 25.5 (22.8, 30.4) |
The results for scintigraphy versus GEBT5 and separately for scintigraphy versus GEBT9 are presented separately and followed by a comparison of GEBT5 versus GEBT9.
Assessment of Gastric emptying from Healthy Subjects & Patients using the 5 breath sample model (Parts A and B)
In addition to all participants in Part A who had a 5 breath sample GEBT, the 5 breath sample model also incorporated the data from 5 selected breath samples (i.e., 45, 90, 120, 150, and 180 minutes) in all Part B participants, in whom 9 breath samples were obtained.
a. Performance and Correlations
Inter-individual CV% for scintigraphic GE proportions and the GEBT kPCD values were, respectively, 34.5% and 39.0% at 45 minutes; 28.5% and 34.8% at 90 minutes; 24.5% and 29.4% at 120 minutes; 20.0% and 25.9% at 150 minutes; and 17.4% and 22.9% at 180 minutes.
Tables 2 and 3 demonstrate the excellent correlation between GE parameters by scintigraphy and the corresponding GEBT values, which establishes the strong association between these variables. In each subject, equations derived from multiple linear regression models were used to predict GE proportions from breath test kPCD values at 45, 90, 120, 150, and 180 minutes, including gender and BMI as covariates (Supplementary Table 1). The corresponding proportions remaining in the stomach averaged across all subjects for the scintigraphic proportions and separately the breath test estimated proportions are shown in Figure 1.
Table 2.
Gastric emptying characteristics using 5 point model (Parts A and B)
| All subjects (N=44) | Healthy subjects only (N=29) | |||
|---|---|---|---|---|
|
| ||||
| Scintigraphy | Breath Test Estimates | Scintigraphy | Breath Test Estimates | |
|
| ||||
| T 10%, min | 15.8 ± 7.6 | 15.01 ± 5.6 | 13.3 ± 4.0 | 12.8 ± 2.7 |
| T ½, min | 82.2 ± 34.6 | 82.5 ± 33.2 | 65.9 ± 14.7 | 67.3 ± 14.0 |
| GE 45 min | 0.330 ± 0.114 | 0.329 ± 0.091 | 0.365 ± 0.090 | 0.366 ± 0.067 |
| GE 90 min | 0.587 ± 0.167 | 0.588 ± 0.154 | 0.667 ± 0.104 | 0.659 ± 0.105 |
| GE 120 min | 0.719 ± 0.176 | 0.720 ± 0.165 | 0.809 ± 0.099 | 0.798 ± 0.104 |
| GE 150 min | 0.813 ± 0.163 | 0.813 ± 0.148 | 0.894 ± 0.086 | 0.882 ± 0.086 |
| GE 180 min | 0.869 ± 0.151 | 0.868 ± 0.133 | 0.942 ± 0.072 | 0.927 ± 0.073 |
Values are Mean ± SD
Table 3.
Correlations between proportion emptied from the stomach by scintigraphy and kPCD by [13C]-Spirulina platensis GEBT at a priori chosen time points in all participants. 5-point model
| Pearson Correlation Coefficients, n=44
| |||||
|---|---|---|---|---|---|
| GE45 | GE 90 | GE120 | GE150 | GE180 | |
|
| |||||
| BT45 | 0.616 * | 0.673 * | 0.656 * | 0.638 * | 0.571 * |
|
| |||||
| BT90 | 0.649 * | 0.842 * | 0.844 * | 0.887 * | 0.782 * |
| BT120 | 0.644 * | 0.846 * | 0.885 * | 0.898 * | 0.864 * |
| BT150 | 0.524 * | 0.734 * | 0.790 * | 0.844 * | 0.841 * |
| BT180 | 0.417 † | 0.610 * | 0.656 * | 0.752 * | 0.787 * |
All correlations marked “ * ” have a p ≤ 0.0010 and correlations marked “ † ” have a p >0.0 10 and ≤ 0.0050.
BT = breath test kPCD; GE = proportion of gastric emptying at specified times
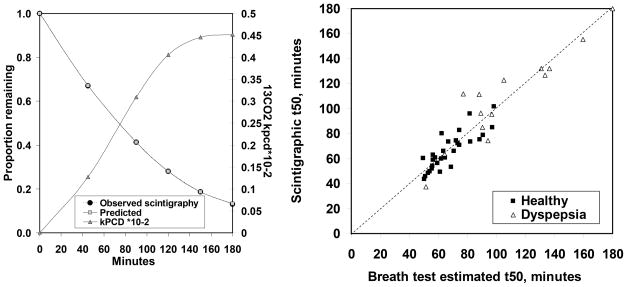
Figure 1.
Summary of gastric emptying results from the 5 time point model in 44 subjects. Left panel illustrates mean 13CO2 enrichment of breath excreted over 3 hours (right Y-axis κPCD × 10−2), as well as the mean observed proportion emptied from the stomach by scintigraphy (left Y-axis) and the mean predicted GE based on the bootstrap regression model using the measured 13CO2 excretion. The observed (scintigraphic) and predicted (GEBT) values are nearly identical; hence superimposed. Right panel illustrates scatterplot of the scintigraphic measured GE t50 values (Y-axis) versus the breath test estimated t50 values (X-axis) obtained from linear interpolation of breath test predicted GE proportions based on the 5 time points model. Only data up to 180 minutes were used in this model. Hence t50 was censored at 180 minutes in 2 subjects. The dotted line shows X=Y.
b. Estimates of Gastric Emptying in Health and Dyspepsia
The 10th and 90th percentiles for the GE t50 measured by scintigraphy in healthy volunteers were 48 and 85 minutes, respectively. The corresponding values for GEBT t50 values measured by the 5-point model were 51 and 91 minutes. The mean difference (10th, 90th %tile range) between GE t50 measured by scintigraphy and GEBT was −0.3 (−12, 14) minutes. For scintigraphy, the interindividual coefficient of variation for t50 was 42% (N=44) overall, 22% in healthy subjects, and 35% in dyspepsia. The corresponding values for GEBT estimated t50 were 40%, 21%, and 36% respectively.
Based on the scintigraphic normal values from the 5 time point data, 3 patients had normal, 11 had delayed and 1 had rapid gastric emptying. Average scintigraphic proportions emptied for these groups and for the 14 healthy subjects studied in Part A are provided in detail in Supplementary Table 2.
c. Accuracy assessed by Concordance Correlation
The (linear) concordance correlation coefficient (CCC) between the scintigraphic and GEBT estimated t50 values was 0.95 (95% CI, 0.91–0.97) for all subjects, 0.83 (95% CI, 0.67–0.92) in healthy subjects and 0.94 (95% CI, 0.83–0.98) in patients.
Assessment of Gastric emptying from Healthy Individuals & Dyspepsia using the 9 breath sample model (Part B only)
a. Performance and Correlations
Scintigraphic measurements and breath test samples were obtained at 9 time points (15, 30, 45, 60, 90, 120, 150, 180, and 240 minutes) in 30 subjects. Inter-individual CV% for scintigraphic GE proportions and the GEBT9 kPCD values respectively were 53% and 56% at 15 minutes; 45% and 44% at 30 minutes; 38% and 42% at 45 minutes; 35% and 41% at 60 minutes; 32% and 38% at 90 minutes; 27% and 34% at 120 minutes; 22% and 31% at 150 minutes; 20% and 27% at 180 minutes; and 15% and 21% at 240 minutes.
Similar to the 5-sample analysis previously published (7), a multiple linear regression model approach was used to estimate gastric emptying based on the breath test samples at all 9 time points (Supplementary Table 3). As in Table 2, which is based on the 5-point model, Table 4 demonstrates the excellent correlations at individual time points for scintigraphic gastric emptying values and the corresponding time kPCD values based on the 9 time point data.
Table 4.
Correlations between proportion emptied from the stomach by scintigraphy and kPCD by [13C]-Spirulina platensis GEBT: 9-point model
| Pearson Correlation Coefficients, n=30
| |||||||||
|---|---|---|---|---|---|---|---|---|---|
| GE15 | GE30 | GE45 | GE60 | GE 90 | GE120 | GE150 | GE180 | GE240 | |
|
| |||||||||
| BT15 | 0.432 † | 0.447 † | 0.411 † | 0.423 † | 0.375 † | 0.332 | 0.381 † | 0.317 | 0.328 |
|
| |||||||||
| BT30 | 0.437 † | 0.560 * | 0.548 * | 0.569 * | 0.5111 * | 0.494 * | 0.493 * | 0.416 † | 0.366 † |
|
| |||||||||
| BT45 | 0.392 † | 0.675 * | 0.664 * | 0.688 * | 0.639 * | 0.621 * | 0.598 * | 0.516 * | 0.455 † |
|
| |||||||||
| BT60 | 0.368 † | 0.740 * | 0.718 * | 0.746 * | 0.731 * | 0.720 * | 0.700 * | 0.623 * | 0.581 * |
|
| |||||||||
| BT90 | 0.416 † | 0.702 * | 0.690 * | 0.754 * | 0.820 * | 0.838 * | 0.838 * | 0.772 * | 0.691 * |
| BT120 | 0.481 * | 0.693 * | 0.670 * | 0.731 * | 0.842 * | 0.893 * | 0.905 * | 0.859 * | 0.776 * |
| BT150 | 0.439 † | 0.583 * | 0.541 * | 0.604 * | 0.746 * | 0.815 * | 0.868 * | 0.851 * | 0.791 * |
| BT180 | 0.456 † | 0.504 * | 0.453 † | 0.511 * | 0.663 * | 0.725 * | 0.821* | 0.835 * | 0.801 * |
| BT240 | 0.257 | 0.276 | 0.166 | 0.213 | 0.347 | 0.418 † | 0.541 * | 0.601 * | 0.743 * |
All correlations marked “* ” have a p ≤ 0.01 and correlations marked “ † ” have a p >0.01 and ≤ 0.05. All other correlations are >0.05. The canonical correlation analysis essentially jointly tests whether the correlations in the matrix below are simultaneously zero.
BT = breath test kPCD; GE = proportion of gastric emptying at specified times
b. Estimates of Gastric Emptying in Health and Dyspepsia
The 10th and 90th percentiles in healthy subjects for breath test-estimated t10 values were 6 and 15 minutes and for breath test-estimated t50 values were 50 and 97 minutes. The 10th and 90th percentiles for scintigraphic GE t50 using all 9 time points in healthy volunteers were 46 and 86 minutes, respectively (Table 5). The mean difference (10–90th percentile range) between GE t50 measured by scintigraphy and GEBT (9-point model) was −0.7 (−13, 17) minutes. The inter-individual CV(%) for the (9 time point) t50 values based on scintigraphy were: 53% overall, 25% in healthy volunteers and 47% in dyspepsia. Corresponding values for GEBT9 were 46% overall, 27% in healthy subjects, and 41% in dyspepsia. Based on the scintigraphic normal values from the 9 time point data, 3 patients had normal, 11 had delayed and 1 had rapid gastric emptying; these classifications were identical to the 5-point data.
Table 5.
Gastric emptying characteristics using 9 point model (Part B).
| All subjects (N=30) | Healthy subjects (N=15) | Dyspepsia (N=15) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Scintigraphy | Breath Test Estimates | Scintigraphy | Breath Test Estimates | Scintigraphy | Breath Test Estimates | |
|
| ||||||
| t10%, min | 13.7±10.2 | 13.4±9.1 | 8.8±2.9 | 9.7±3.6 | 18.5±12.5 | 17.1±11.3 |
| t50, min | 93.6 ± 50.0 | 91.3 ± 42.3 | 65.9 ± 16.5 | 68.3 ± 18.2 | 121.4±57.1 | 114.3±47.3 |
| GE 15 min | 0.147 ± 0.078 | 0.145 ± 0.058 | 0.190 ± 0.065 | 0.171 ± 0.049 | 0.103 ± 0.067 | 0.120 ± 0.057 |
| GE 30 min | 0.230 ± 0.104 | 0.230 ± 0.095 | 0.282 ± 0.061 | 0.271 ± 0.069 | 0.179 ± 0.114 | 0.189 ± 0.101 |
| GE 45 min | 0.324 ± 0.123 | 0.323 ± 0.116 | 0.386 ± 0.086 | 0.375 ± 0.090 | 0.262 ± 0.126 | 0.271 ± 0.118 |
| GE 60 min | 0.393 ± 0.139 | 0.391 ± 0.135 | 0.467 ± 0.096 | 0.459 ± 0.103 | 0.318 ± 0.137 | 0.324 ± 0.131 |
| GE 90 min | 0.542 ± 0.171 | 0.540 ± 0.165 | 0.652 ± 0.101 | 0.641 ± 0.114 | 0.432 ± 0.157 | 0.439 ± 0.147 |
| GE 120 min | 0.665 ± 0.181 | 0.665 ± 0.174 | 0.784 ± 0.100 | 0.775 ± 0.111 | 0.545 ± 0.164 | 0.556 ± 0.158 |
| GE 150 min | 0.765 ± 0.172 | 0.763 ± 0.163 | 0.873 ± 0.096 | 0.864 ± 0.095 | 0.656 ± 0.163 | 0.663 ± 0.156 |
| GE 180 min | 0.827 ± 0.164 | 0.824 ± 0.151 | 0.925 ± 0.085 | 0.913 ± 0.084 | 0.729 ± 0.167 | 0.735 ± 0.151 |
| GE 240 min | 0.911 ± 0.138 | 0.903 ± 0.118 | 0.978 ± 0.083 | 0.958 ± 0.047 | 0.844 ± 0.167 | 0.847 ± 0.142 |
Values are Mean ± SD
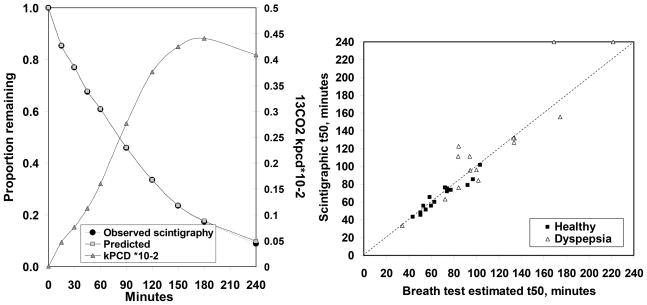
c. Accuracy assessed by Concordance Correlation
The (linear) CCC between the scintigraphic and breath test estimated t50 values was 0.93 (95% CI, 0.86–0.96) overall, 0.94 (95% CI, 0.85–0.98) in healthy subjects and 0.89 (95% CI, 0.72–0.96) in patients. Figure 2 shows the plot of observed gastric emptying (mean proportions remaining in the stomach) and corresponding mean predicted proportions remaining. Also shown in Figure 2 are the mean breath test kPCD values (*10−2 ).
Figure 2.
Summary of gastric emptying results from the 9 time point model in 30 subjects. Data illustrate mean 13CO2 enrichment of breath excreted over 4 hours (right Y-axis κPCD × 10−2), as well as the mean observed proportion emptied from the stomach by scintigraphy (left Y-axis) and the mean predicted GE based on the bootstrap regression model using the measured 13CO2 excretion. The observed (scintigraphic) and predicted (GEBT) values are nearly identical; hence superimposed. Right panel shows scatterplot of the scintigraphic measured gastric emptying t50 values (Y-axis) versus the breath test estimated t50 values (X-axis) obtained from linear interpolation of breath test predicted GE proportions in healthy subjects and patients with dyspepsia based on the 9 time points model. The dotted line shows X=Y.
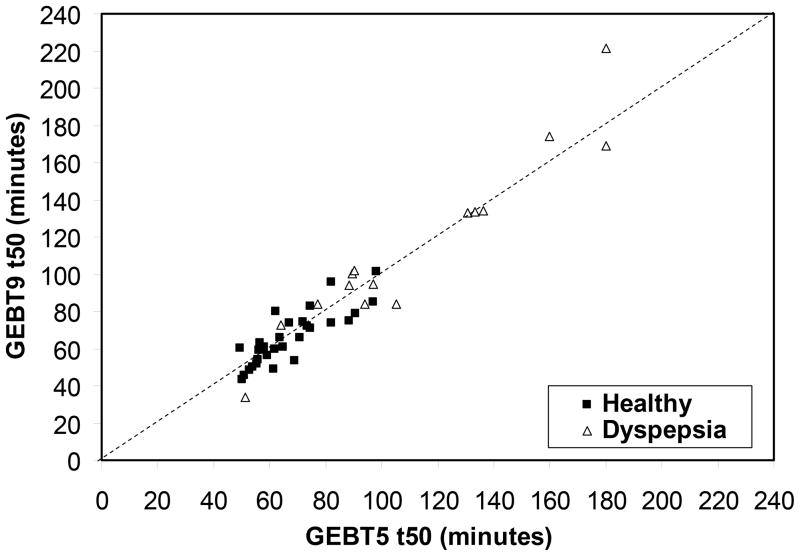
Comparison of accuracy of the 5 and 9 breath sample models
The relationship between 5 and 9 point model estimates (30 subjects in Part B) was assessed for t10, GE 30 minutes, and GE 60 minutes, which represent early gastric emptying, and t50, which summarizes the overall gastric emptying curve. Figure 3 compares GEBT estimated t50 values from all 9 and the selected 5 time point models (Part B). The concordance correlation between these two estimated t50 values was 0.96 (95% CI, 0.92–0.98). However, 2 individuals had prolonged GEBT estimated t50 values which the 5 time point model was unable to reproduce. For these two individuals, the scintigraphic proportions indicated a t50 of at least 240 minutes based on 9 time points and >180 minutes based on 5 time points. In these subjects, the estimated t50 was 169 and 222 minutes by GEBT9 and 180 by minutes GEBT5. At the other extreme, scintigraphy disclosed rapid gastric emptying, as defined by a GE t50 shorter than the 10th percentile value, in 2 healthy subjects and 1 patient. GEBT9 also demonstrated rapid emptying in this patient and in 1 of these 2 healthy subjects. However, none of these 3 subjects had rapid GE by GEBT5.
Figure 3.
Comparison of breath test estimated t50 values obtained from linear interpolation of breath test predicted GE proportions in healthy subjects and patients with dyspepsia based on the 5 time points model (X- axis) and 9 time points model (Y axis). The dotted line shows X=Y.
The Bland Altman plots demonstrate that the difference between GE t50 assessed by scintigraphy and 5 point (left panel) or 9 point (right panel) breath test models was not impacted by the average t50 for both tests in the range of GE tested in these cohorts (Figure 4).
Figure 4.
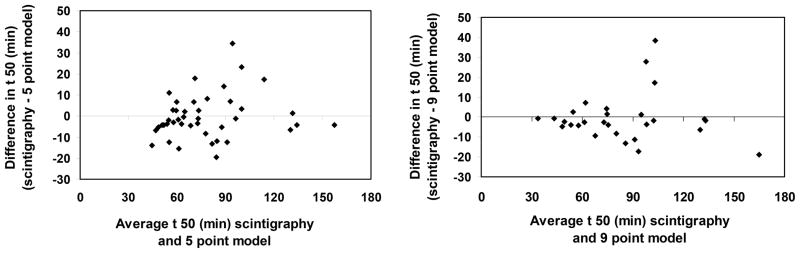
Bland Altman Plots for 5 point (left panel) and 9 point (right panel) for t50 estimated by GEBT versus scintigraphy.
The 10th and 90th percentiles for t10 in healthy subjects were respectively 5 and 12 minutes by scintigraphy (9 time points), 6 and 15 minutes for GEBT 9-point model and 10 and 19 minutes for GEBT 5-point model. For t10, the CCC for scintigraphy versus GEBT 5-point and 9-point models were 0.73 (95% CI, 0.54–0.85) and 0.80 (95% CI, 0.63–0.90) respectively.
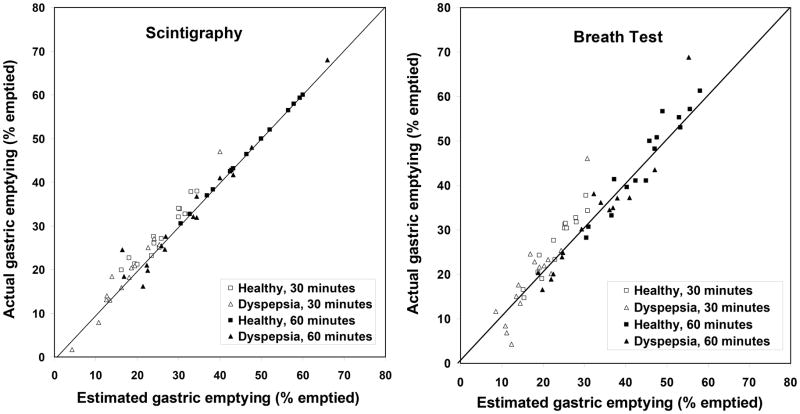
Gastric emptying at 30 and 60 minutes were estimated by linear interpolation between 0 and 45 minutes and 45 and 90 minutes respectively. Actual (i.e., GEBT 9-point model) and estimated values (i.e., from GEBT 5-point model) were more closely correlated at 60 minutes (CCC 0.95 [95% CI, 0.91–0.97]) than at 30 minutes (CCC 0.81 [95% CI, 0.71–0.89]).
DISCUSSION
The primary goals of this study were to validate a different version of a standardized, shelf-stable breath test meal labeled with [13C]-Spirulina platensis to measure GE of solids in clinical practice, to appraise the performance characteristics of GEBT5 and GEBT9 versus scintigraphy, and to assess the accuracy of 9 compared to 5 breath samples, particularly for characterizing the early phase of GE. The study confirms previous observations obtained with a whole, fresh egg meal and with 13C GEBT in our prior studies (2–6, 29). There was excellent concordance between breath excretion of 13CO2 and the proportion of isotope-labeled meal emptied from the stomach at specified time points for the 5 and separately for the 9 time point assessments. The results confirm that the breath test provides a very valid estimate of the GE t50, which is widely used to make clinical decisions and in pharmacodynamic studies. This is supported by the observation that the concordance correlation coefficient for the GE t50 measured by scintigraphy and GEBT5 and 9 point models averaged 0.9 and the average difference between the GE t50 calculated by scintigraphy and GEBT was less than 1 minute, with a 10–90th percentile range of approximately ± 15 minutes. Likewise, actual and linearly interpolated GE at 60 minutes was very similar probably because emptying is generally approximately linear between 45 and 90 minutes.
However, these data suggest that a GEBT with 9 time points may be preferable to a GEBT with 5 points for identifying rapid GE and for characterizing early GE (i.e., t10 and GE 30 minutes). For example, 2 of 3 subjects (1 healthy subject, 2 patients) with rapid GE by scintigraphy also had rapid GE by GEBT9 but none had rapid GE by GEBT5. The correlation between actual (i.e., GEBT 9-point model) and estimated values (i.e., from GEBT 5-point model) for GE at 30 minutes was modest (CCC 0.81 [95% CI, 0.71–0.89]). Likewise, for t10, the CCC for scintigraphy versus GEBT 5-point model was 0.73 (95% CI, 0.54–0.85) and lower than scintigraphy versus the GEBT 9-point model (0.80 [95% CI, 0.63–0.90]). In our previous study, breath samples at 45 and 180 minutes had 93% sensitivity at 80% specificity for identifying rapid GE as defined by the scintigraphic t50 (6). However, it is conceivable that an assessment of GE at 30 minutes may be more useful for identifying some patients with accelerated GE, i.e. those in whom GE is accelerated at 30 minutes but plateaus later, resulting in a normal t50. Because few patients had rapid GE in this study, further studies are necessary to evaluate the utility of measuring t10, and GE at 30 minutes by the 9 time point model in patients with rapid GE.
Moreover, although the vast majority of asymptomatic individuals emptied the meal from the stomach before 80 minutes, the 240 minute observation may be useful, particularly when GE is delayed. For example, when the 5 time point model suggests a t50 > 180 minutes, the 240 minute sample is necessary to clarify whether the t50 is closer to 180 minutes or even > 240 minutes, as was observed in 2 patients.
In summary, the current data confirm that the stable isotope technology developed in earlier studies is also applicable with a meal in which a slightly modified process was used to enrich Spirulina platensis with 13C. The [13C]-Spirulina platensis GEBT has high reproducibility, external validity and excellent performance characteristics. The statistical models previously proposed, based on linear regression, continue to demonstrate they are robust to estimate GE in health and disease, and offer further support for the use of this GEBT in clinical practice, epidemiological studies, or clinical research studies. A 5-sample test is as accurate as a 9-point test for identifying normal GE in symptomatic patients. The 9-breath sample test is more accurate for evaluating early GE (e.g., t10 and GE at 30 minutes), which is accelerated in patients with rapid GE, and provides a more comprehensive assessment in some patients with delayed GE. Further studies need to fully address the relative accuracy of the 5 and 9 point models in patients with rapid GE.
Supplementary Material
Figure 5.
Comparison of actual (9 time point data) and linearly interpolated (5 time point data) gastric emptying at 30 and 60 minutes by scintigraphy (left panel) and GEBT estimated proportions (right panel). The linear interpolation estimates were obtained by linear interpolation between 0 and 45 minutes for gastric emptying at 30 minutes and between 45 and 90 minutes for gastric emptying at 60 minutes.
Acknowledgments
This study was supported by PO1 DK 68055 from National Institutes of Health. The studies were conducted in the Mayo Clinic Clinical Research Unit which is supported by grant RR024150 from National Institutes of Health.
AB Diagnostics provided breath test kits at cost price and analyzed breath samples without charge but did not support the study in any other manner.
Abbreviations used
- BT
Breath test
- [13C]
13-carbon
- CCC
concordance correlation coefficient
- CV
coefficient of variation
- DOB
delta over baseline
- GE
gastric emptying
- GEBT
gastric emptying breath test
- GEBT5
gastric emptying breath test with 5 breath samples
- GEBT9
gastric emptying breath test with 9 breath samples
- PCD
percent dose
- kPCD
percent dose multiplied by 1000
- ROI
region of interest
- [99mTc]
99m- technetium
- t10
time for 10% emptying
- GE30
gastric emptying in 30 min
- t50
gastric emptying half time
Footnotes
No conflicts of interest exist for all of the authors.
Funding, and Disclosures
Author contributions: Adil E. Bharucha was principal investigator for the study and contributed to study design and concept, data analysis and interpretation, and manuscript preparation, critical revision, and final approval. Michael Camilleri contributed to study design and concept and critical revision of manuscript. Erica Veil and Duane Burton contributed to study conduct. Alan R. Zinsmeister conducted data analysis and critically revised the manuscript. All authors approved the final version of the manuscript.
References
- 1.Odunsi ST, Camilleri M, Szarka LA, Zinsmeister AR. Optimizing analysis of stable isotope breath tests to estimate gastric emptying of solids. Neurogastroenterol Motil. 2009;21:706–e738. doi: 10.1111/j.1365-2982.2009.01283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi MG, Camilleri M, Burton DD, Zinsmeister AR, Forstrom LA, Nair KS. [13C]octanoic acid breath test for gastric emptying of solids: accuracy, reproducibility, and comparison with scintigraphy. Gastroenterology. 1997;112:1155–1162. doi: 10.1016/s0016-5085(97)70126-4. [DOI] [PubMed] [Google Scholar]
- 3.Choi MG, Camilleri M, Burton DD, Zinsmeister AR, Forstrom LA, Nair KS. Reproducibility and simplification of c-13-octanoic acid breath test for gastric emptying of solids. Am J Gastroenterol. 1998;93:92–98. doi: 10.1111/j.1572-0241.1998.092_c.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee JS, Camilleri M, Zinsmeister AR, et al. Toward office-based measurement of gastric emptying in symptomatic diabetics using [13C]octanoic acid breath test. Am J Gastroenterol. 2000;95:2751–2761. doi: 10.1111/j.1572-0241.2000.03183.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee JS, Camilleri M, Zinsmeister AR, Burton DD, Kost LJ, Klein PD. A valid, accurate, office based non-radioactive test for gastric emptying of solids. Gut. 2000;46:768–773. doi: 10.1136/gut.46.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Szarka LA, Camilleri M, Vella A, et al. A stable isotope breath test with a standard meal for abnormal gastric emptying solids in the clinic and in research. Clinical Gastroenterology & Hepatology. 2008;6:635–643. doi: 10.1016/j.cgh.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Advanced Breath Diagnostics L. [13C]-Spirulina platensis Gastric Emptying Breath Test (GEBT)-Investigator Brochure. Brentwood, TN: 2005. [Google Scholar]
- 8.Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine.[reprint in J Nucl Med Technol. 2008 Mar;36(1):44–54; PMID: 18287197] Am J Gastroenterol. 2008;103:753–763. doi: 10.2967/jnmt.107.048116. [DOI] [PubMed] [Google Scholar]
- 9.Charles F, Phillips SF, Camilleri M, Thomforde GM. Rapid gastric emptying in patients with functional diarrhea. Mayo Clin Proc. 1997;72:323–328. doi: 10.4065/72.4.323. [DOI] [PubMed] [Google Scholar]
- 10.Weytjens C, Keymeulen B, Van Haleweyn C, Somers G, Bossuyt A. Rapid gastric emptying of a liquid meal in long-term Type 2 diabetes mellitus. Diabet Med. 1998;15:1022–1027. doi: 10.1002/(SICI)1096-9136(1998120)15:12<1022::AID-DIA720>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 11.Delgado-Aros S, Camilleri M, Cremonini F, Ferber I, Stephens D, Burton DD. Contributions of gastric volumes and gastric emptying to meal size and postmeal symptoms in functional dyspepsia [see comment] Gastroenterology. 2004;127:1685–1694. doi: 10.1053/j.gastro.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Lawal A, Barboi A, Krasnow A, Hellman R, Jaradeh S, Massey BT. Rapid gastric emptying is more common than gastroparesis in patients with autonomic dysfunction. Am J Gastroenterol. 2007;102:618–623. doi: 10.1111/j.1572-0241.2006.00946.x. [DOI] [PubMed] [Google Scholar]
- 13.Bharucha AE, Camilleri M, Forstrom L, Zinsmeister AR. Relationship between clinical features and gastric emptying disturbances in diabetes mellitus. Clin Endocrinol (Oxf) 2008;70:415–420. doi: 10.1111/j.1365-2265.2008.03351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malhotra N, Pathikonda M, Sachdeva P, Maurer AH, Fisher RS, Parkman HP. Rapid Gastric Emptying or Gastroparesis: Can One Tell the Difference in the Clinic? Gastroenterology. 2010;138:W1388. [Google Scholar]
- 15.Hejazi RA, Patil H, McCallum RW. Dumping syndrome: establishing criteria for diagnosis and identifying new etiologies. Dig Dis Sci. 2010;55:117–123. doi: 10.1007/s10620-009-0939-5. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE, Manduca A, Lake DS, et al. Gastric Motor Disturbances In Patients With Idiopathic Rapid Gastric Emptying. Neurogastroenterol Motil. 2010;23:617–e252. doi: 10.1111/j.1365-2982.2011.01710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balan K, Sonoda LI, Seshadri N, Solanki C, Middleton S. Clinical significance of scintigraphic rapid gastric emptying. Nucl Med Commun. 2011;32:1185–1189. doi: 10.1097/MNM.0b013e32834bf262. [DOI] [PubMed] [Google Scholar]
- 18.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders.[erratum appears in Gastroenterology. 2006 Jul;131(1):336] Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 19.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 20.Ciferri O. Spirulina, the edible microorganism. Microbiol Rev. 1983;47:551–578. doi: 10.1128/mr.47.4.551-578.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciferri O, Tiboni O. The biochemistry and industrial potential of Spirulina. Annu Rev Microbiol. 1985;39:503–526. doi: 10.1146/annurev.mi.39.100185.002443. [DOI] [PubMed] [Google Scholar]
- 22.Dillon JC, Phuc AP, Dubacq JP. Nutritional value of the alga Spirulina. World Rev Nutr Diet. 1995;77:32–46. doi: 10.1159/000424464. [DOI] [PubMed] [Google Scholar]
- 23.Ricci E. Determination of carbon-12, carbon-13 isotopic abundances and nitrogen-carbon ratios in biological substances by proton-reaction analysis. Anal Chem. 43:1866–1871. doi: 10.1021/ac60307a024. [DOI] [PubMed] [Google Scholar]
- 24.Klein PD. Clinical applications of 13CO2 measurements. Fed Proc. 41:2698–2701. [PubMed] [Google Scholar]
- 25.Schoeller DA, Schneider JF, Solomons NW, Watkins JB, Klein PD. Clinical diagnosis with the stable isotope 13C in CO2 breath tests: methodology and fundamental considerations. J Lab Clin Med. 90:412–421. [PubMed] [Google Scholar]
- 26.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Human Nutrition - Clinical Nutrition. 39(Suppl 1):5–41. [PubMed] [Google Scholar]
- 27.Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57:1–12. doi: 10.1016/j.annemergmed.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carrasco JL, Jover L. Estimating the generalized concordance correlation coefficient through variance components. Biometrics. 2003;59:849–858. doi: 10.1111/j.0006-341x.2003.00099.x. [DOI] [PubMed] [Google Scholar]
- 29.Viramontes BE, Kim DY, Camilleri M, et al. Validation of a stable isotope gastric emptying test for normal, accelerated or delayed gastric emptying. Neurogastroenterol Motil. 2001;13:567–574. doi: 10.1046/j.1365-2982.2001.00288.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.