Abstract
Purpose
The purpose of this study is to evaluate the effect of graft size on patient-reported outcomes and revision risk following ACL reconstruction.
Methods
A retrospective chart review of prospectively collected cohort data, 263 of 320 consecutive patients (82.2%) undergoing primary ACL reconstruction with hamstring autograft were evaluated. Graft size, femoral tunnel drilling technique, patient age, sex, and BMI at the time of ACL reconstruction, pre-operative and 2-year post-operative KOOS and IKDC scores, and whether each patient underwent revision ACL reconstruction during the 2 year follow-up period were recorded. Revision was used as a marker for graft failure. The relationship between graft size and patient-reported outcomes was determined by multiple linear regression. The relationship between graft size and risk of revision was determined by dichotomizing graft size at 8mm and stratifying by age.
Results
After controlling for age, sex, operative side, surgeon, BMI, graft choice, and femoral tunnel drilling technique, a 1 mm increased in graft size was noted to correlate with 3.3-point increase in the KOOS-pain subscale (p = 0.003), a 2.0-point increased in the KOOS activities of daily living subscale (p = 0.034), a 5.2-point increase in the KOOS-sport/recreation function subscale (p = 0.004), and a 3.4-point increase in the subjective IKDC score (p = 0.026). Revision was required in 0 of 64 patients (0.0%) with grafts greater than 8mm in diameter and 14 of 199 patients (7.0%) with 8 mm or smaller grafts (p = 0.037). Among patients age 18 and under, revision was required in 0 of 14 patients (0.0%) with grafts greater than 8mm in diameter and 13 of 71 patients (18.3 %) with 8 mm or smaller grafts.
Conclusions
Smaller hamstring autograft size is a predictor of poorer KOOS Sport and Recreation function 2 years following primary ACL reconstruction. Larger sample size is required to confirm the relationship between graft size and risk of revision ACL reconstruction.
Level of Evidence
Level 3
Introduction
Anterior cruciate ligament (ACL) ruptures have been estimated to occur in 200,000 people annually in the United States.(1) A majority of these patients eventually undergo ACL reconstruction based on continued instability symptoms or desire for future participation in cutting or pivoting sports. While bone-patellar tendon-bone autograft has traditionally been the gold standard for reconstruction, quadrupled hamstring tendon has become a popular autograft option.(2) Quadrupled hamstring tendon is biomechanically equivalent or superior in strength at time zero when compared to patellar tendon and can result in less donor site morbidity.(3, 4)
Unlike bone-patellar tendon-bone grafts, the diameter of a hamstring autograft is quite variable. Although difficult to predict accurately, hamstring autograft diameter has been shown to correlate with patient gender, height, BMI, and thigh circumference.(5–8) Previous biomechanical work has shown hamstring graft strength to increase with increasing graft diameter.(3)
Although ideal hamstring graft size remains undefined in the literature, recent retrospective studies demonstrate increased failure rates in younger patients with grafts less than or equal to 8 mm in diameter.(9, 10) The purpose of this study is to evaluate the effect of graft size on patient-reported outcomes and revision risk following ACL reconstruction. We hypothesize that decreased hamstring autograft size is associated with poorer patient reported outcome scores and increased risk of revision two year following ACL reconstruction.
Methods
Identification of patients
Patients were identified through the use of prospectively collected data from the Multicenter Orthopaedic Outcomes Network (MOON) collected at two academic medical centers. A total of 322 patients who underwent primary ACL reconstruction with hamstring autograft between the years of 2007 and 2009 were identified. The database provides demographic information, intra-operative findings (meniscus and cartilage status), surgical technique, and patient-reported outcome scores (Knee injury and Osteoarthritis Outcome Score [KOOS](11) and International Knee Documentation Committee [IKDC] subjective score(12)) pre-operatively and at two-year follow-up. The database also contains information regarding whether patients underwent repeat ipsilateral knee surgery, including revision ACL reconstruction. These data were supplemented by retrospective review of the operative records to determine the hamstring autograft size used in each patient. Two skeletally immature patients who underwent all-epiphyseal ACL reconstruction were excluded, yielding a total of 320 eligible patients.
Surgical Technique
Procedures were performed by a total of five fellowship-trained sports medicine surgeons at the two institutions. The hamstrings were harvested by standard techniques and 4 strand grafts were used in all cases (either doubled semitendinosus and gracilis or quadrupled semitendinosus). ACL reconstruction was performed with either an all-endoscopic or arthroscopic-assisted technique. The femoral tunnel was drilled through a medial portal in 38% of the cases, while a trans-tibial method was used in 62% of the cases. The femoral tunnel was consistently drilled to be the same diameter as the prepared graft. Femoral fixation was achieved with a cortical button in all cases. Tibial fixation was variable and included interference screw fixation, suture tied over a post or button, or a combination depending on surgeon preference. Graft tensioning was not standardized and was performed according to surgeon preference. A standard accelerated ACL rehabilitation protocol developed by the MOON group was used for all patients, with a goal of returning to sports at 6 months.
Statistics
Summary statistics including mean and standard deviations were calculated for normally distributed continuous variables. The relationship between graft size and patient-reported outcome scores at two year post-operative was determined by multiple linear regression analysis in a model that included graft size, graft type (quadrupled semitendinosus versus doubled gracilis and semitendinosus), age, sex, operative side, surgeon, BMI, femoral tunnel drilling technique, and pre-operative patient reported outcome score. The relationship between graft size and risk of revision was determined by comparing patients with grafts larger than 8mm with those in whom smaller grafts were used and stratifying based on patient age as has been performed in previous work. Characteristics of patients in each group were compared using t-tests for normally distributed continuous variables, Wilcoxin rank sum tests for non-normally distributed continuous variables, and Fisher’s exact test for dichotomous variables. The relatively small number of events (revision operations) in the series precluded modeling of the revision data by logistic regression analysis. The relationships between revision risk and patient sex, graft type, operative side, surgeon, and femoral tunnel drilling technique were evaluating using Fisher’s exact test.
Results
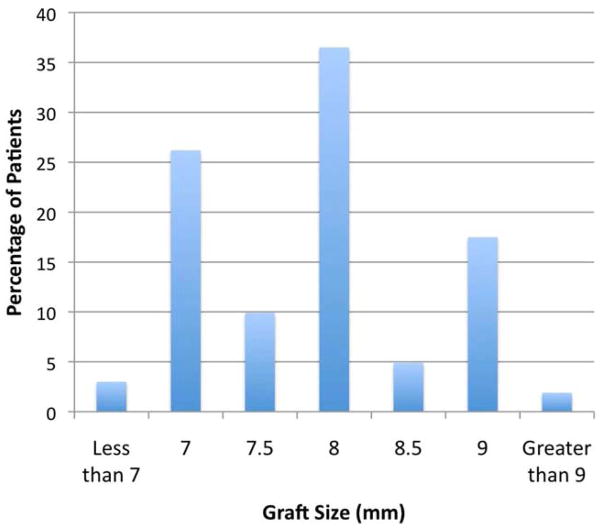
Complete data, including graft size and patient reported outcomes at two years post-operative were available in 263 patients (82.2%). There were 144 males (54.8%) and 119 females (45.2%). Mean patient age was 25.6 ± 10.3 years and ranged from 13 to 58 years. Mean graft size was 7.8 ± 0.8 mm with a range from 6 to 10 mm (Figure 1) and was significantly larger in males (8.1 ± 0.8 mm) than in females (7.6 ± 0.6 mm) (p < 0.0001).
Figure 1.
Histogram demonstrating the distribution of graft size among patients included in the study. The mean graft size was 7.8 mm.
After controlling for age, sex, operative side, surgeon, BMI, femoral tunnel drilling technique, graft choice, and pre-operative patient-reported outcome scores, graft size was noted to correlate with a number of patient reported outcome scores at two years post-operative (Table 1). A 1 mm increased in graft size was noted to correlate with 3.3-point increase in the KOOS-pain subscale (p = 0.003), a 2.0-point increased in the KOOS activities of daily living subscale (p = 0.034), a 5.2-point increase in the KOOS-sport/recreation function subscale (p = 0.004), and a 3.4-point increase in the subjective IKDC score (p = 0.026).
Table 1.
Results of multiple linear regression analyses of the correlation between graft size and patient-reported outcome scores
| Outcome Score | Regression Coefficient of Graft Size | Standard Error | Significance |
|---|---|---|---|
| KOOS-Symptoms | 1.31 | 1.20 | p = 0.28 |
| KOOS-Pain | 3.26 | 1.09 | p = 0.003 |
| KOOS-ADL’s | 1.99 | 0.93 | p = 0.034 |
| KOOS-Sport/Rec | 5.15 | 1.76 | p = 0.004 |
| KOOS-QOL | 2.82 | 1.86 | p = 0.15 |
| IKDC | 3.37 | 1.43 | p = 0.026 |
| Marx Activity | 0.47 | 0.42 | p = 0.26 |
KOOS = Knee injury and Osteoarthritis Outcome Score
IKDC = International Knee Documentation Committee 305
Graft size was also noted to correlate with the need for revision ACL reconstruction. Fourteen of the 263 patients (5.3%) underwent revision ACL reconstruction in the first two years post-operative (Table 2). The mean time from primary to revision ACL reconstruction was 12.7 ± 6.9 months (range: 6 to 25 months). Revision was required in 0 of 64 patients (0.0%) with grafts greater than 8 mm in diameter and 14 of 199 patients (7.0%)with graft 8 mm in diameter or smaller (p = 0.037). The group with grafts great than 8 mm in diameter had a higher average age and BMI and contained a higher proportion of males, patients operated with a trans-tibial technique, and patients in who a quadrupled semitendinosus was used for the graft (Table 3). There was no significant correlation between revision risk and patient sex, operative side, surgeon, graft type, or surgical technique.
Table 2.
Revision rates by graft size (total cohort)
| Graft Size | Number | Revisions | Percent Revised |
|---|---|---|---|
| Over 8 mm | 64 | 0 | 0% |
| 8 mm and under | 199 | 14 | 7.0% |
| All | 263 | 14 | 5.3% |
mm = millimeters
Table 3.
Patient Characteristics by Graft Size
| Graft Size | Significance | ||
|---|---|---|---|
| 8 mm and Under (n = 199) | Greater than 8 mm (n = 64) | ||
| Age (years) (median, IQR) | 21 (17 – 28.5) | 27 (19.8 – 35.2) | p = 0.0014 |
| Sex (Female) | 110 (55.3%) | 9 (14.1%) | p < 0.001 |
| BMI (kg/m2) (mean ± SD) | 24.4 ± 4.3 | 28.1 ± 5.1 | p < 0.001 |
| Graft type (quadrupled semitendinosus) | 31 (15.6%) | 30 (46.9%) | p < 0.001 |
| Femoral tunnel drilling technique (Trans-tibial) | 130 (65.3%) | 33 (51.6%) | p = 0.035 |
BMI = Body Mass Index
SD = Standard Deviation
IQR = Inter-quartile Range 311
Among patients age 18 and under, graft size was also noted to correlate with the need for revision ACL reconstruction. Thirteen of the 85 patients (15.3%) age 18 and under underwent revision ACL reconstruction in the first two years post-operative (Table 4). Revision was required in 0 of 14 patients (0.0%) with grafts greater than 8 mm in diameter and 13 of 71 patients (18.3%) with grafts 8mm in diameter or smaller. Overall, 13 of the 14 revisions were performed in patients age 18 and under with grafts 8 mm in diameter or less (Table 5). There was no significant difference in the incidence of revision surgery between males and females (p = 0.17).
Table 4.
Revision rates by graft size (patients age 18 and under)
| Graft Size | Number | Revisions | Percent Revised |
|---|---|---|---|
| Over 8 mm | 14 | 0 | 0% |
| 8 mm and under | 71 | 13 | 18.3% |
| Total | 85 | 13 | 15.3% |
mm = millimeters
Table 5.
ACL graft revision rates by according to patient age and graft size
| Patient Age (Years) | |||
|---|---|---|---|
| 18 and under | Over 18 | ||
| Graft Size | Greater than 8 mm | 0 / 14 (0%) | 0 / 47 (0%) |
| 8 mm and under | 13 / 71 (18.3%) | 1 / 131 (0.8%) | |
mm = millimeters
Discussion
While ACL reconstruction has demonstrated success in restoring knee stability and improving patient’s outcomes, recent have shown that ipsilateral graft failure still occurs in 1.8% to 10.4% of cases.(13, 14) Many factors contribute to the need for revision ACL surgery and the use of smaller diameter hamstring grafts may also be a contributor. The most significant findings of the current study are significant correlations between increased graft size and improved patients-reported outcome scores and decreased risk of revision surgery.
The results of the linear regression model evaluating the relationship between graft size and patient-reported outcome scores demonstrate that a 2 mm increase in graft size correlates with a 10.3 point increase in the KOOS sport and recreation function subscale, a 4.0 point increase in the KOOS activities of daily living subscale, a 6.5 point increase in the KOOS pain subscale, and a 6.7 point increase in the subjective IKDC score. These differences are close to and in some cases exceed established clinically significant differences for the KOOS subscales (8–10 points)(11, 15) and the subjective IKDC score (11.5 points).(15, 16) Smaller changes in graft size are unlikely to result in clinically significant changes in patient-reported outcome scores.
While this study is the first to evaluate the relationship between ACL graft size and patient-reported outcome scores, the findings of this study are overall in agreement with previous studies evaluating the relationship between graft size and revision risk. In a retrospective analysis of 296 patients undergoing hamstring autograft ACL reconstruction, Park et al. did not observe any failures in patients with graft diameters of 8 mm or more.(10) Among patients with a graft size of less than 8mm, they noted a revision risk of 5.2%. Magnussen et al. conducted a retrospective study of 256 patients and found that 16 of 18 revision ACL reconstructions occurred in patients with hamstrings autografts 8 mm in diameter or less, with a revision risk of 16.5% noted in patients under age 20 reconstructed with such grafts.(9) It should be noted that although the prior Magnussen et al study(9) shares one author with the current study, the studies were performed at separate institutions and involve none of the same patients. The current study was undertaken in part to address some limitations of the prior work, namely the short follow-up in the prior study and the lack of patient-reported outcome measures.
Another key finding of the current study is the interaction between age and graft size in determining ACL graft revision rate. The revision risk of ACL grafts 8mm and under in patients under age 19 was 15.3% - quite similar to that exhibited in a previous study.(9) More evidence is appearing in the literature that revision is common in this young, active population.(17–20) While much of the previous ACL literature fails to stratify ACL reconstruction outcomes based on both graft size and patient age, the high prevalence of small grafts in this population may contribute significantly to these high rates. Age itself likely serves as a surrogate marker for activity level as young patients are most likely to return to high risk cutting/pivoting sporting activities that increase their risk for traumatic graft rupture.
The reasons for poorer outcomes in patients with smaller grafts remain unclear. One could hypothesize that this differences is simply due to the decreased failure load of smaller ACL grafts; however, biomechanical studies have demonstrated strength at least equal to that of patellar tendon grafts at time zero.(3, 4) It is possible that the decreased graft strength associated with the ligamentization process may push smaller grafts below a critical strength threshold and contribute to increased risk of failure.
Limitations
There are several limitations of this study. A significant limitation entails using revision ACL as a marker for graft failure. There likely is a subset of patients that has functional instability or increased laxity ACL (i.e. a failed graft) that have not undergone revision surgery. Therefore, the number of revision surgeries may be an underestimation of the actual number of failures. We also lack information regarding the mechanism of failure of grafts that could potentially shed light on the contribution of graft size to graft failure. An additional limitation is the lack of physical examination and instrumented laxity assessment at follow-up. Such data may contribute to our understanding of the reasons for poorer patient-reported outcomes among those with smaller grafts. It is unknown, for example, if the patients with smaller graft size exhibited increased laxity at follow-up. It has; however, been demonstrated that patient-reported outcomes do correlate with specific functional assessments such as hop tests.(21) A further limitation is the relatively small sample size. The relatively small number of patients that underwent revision ACL reconstruction precluded the performance of logistic regression modeling on these data. Therefore we are unable to assess the influence of variables other than patient age (such as patient sex and size as well as surgical technique) on the findings. We did compare these variables in the patients with larger and smaller grafts and noted a number of significant differences between the groups (Table 5); however, no significant correlation between these variables and revision risk was noted. More studies with larger numbers are needed to elucidate the influence of these factors on revision risk. Further study limitations include the lack of post-operative imaging to assess tunnel position and additional uncontrolled variability in the five surgeons’ techniques, including variability in tibial fixation, graft tensioning, and other unrecorded variables. Future ACL studies involving patients reconstructed with hamstring tendons should record graft size and consider it as a factor in their analyses.
Conclusions
Smaller hamstring autograft size is a predictor of poorer KOOS Sport and Recreation function 2 years following primary ACL reconstruction. Larger sample size is required to confirm the relationship between smaller graft size and increased risk of revision ACL reconstruction.
Acknowledgments
This project was partially funded by grant number 5R01 AR053684 (K.P.S.) and K23 AR063767 (R.A.M.) from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases and by grant number 5U18-HS016075 (R.G.M.) from the Center for Education and Research on Therapeutics (Agency of Health Research and Quality). The project was also supported by the Vanderbilt Sports Medicine Research Fund. Vanderbilt Sports Medicine received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics.
We thank the following Multicenter Orthopaedic Outcomes Network (MOON) members, without whom the data utilized in this study would not exist. These members include: Kurt P. Spindler, MD, Warren R. Dunn, MD, MPH, Laura J. Huston MS (Vanderbilt University School of Medicine); Rick W. Wright, MD, Matthew J. Matava, MD, Robert H. Brophy, MD (Washington University School of Medicine at Barnes-Jewish Hospital); Eric C. McCarty, MD, Armando Vidal, MD, Michelle Wolcott, MD (University of Colorado School of Medicine); Robert G. Marx, MD, MSc (Hospital for Special Surgery); Annunziato Amendola, MD, Brian R. Wolf, MD, MS (University of Iowa)
We thank the following research coordinators, analysts and support staff from the Multicenter Orthopaedic Outcomes Network (MOON) sites, whose efforts make this consortium possible: Lynn Borzi, Julia Brasfield, Maxine Cox, Michelle Hines, Pam Koeth, Leah Schmitz (Cleveland Clinic Foundation); Kari Stammen (Ohio State University); Carla Britton, Catherine Fruehling-Wall (University of Iowa); Christine Bennett, Paula Langner (University of Colorado); Linda Burnworth, Robyn Gornati, Amanda Haas (Washington University in St. Louis); Brian Boyle, Patrick Grimm, Kaitlynn Lillemoe, Lana Verkuil (Hospital for Special Surgery); Emily Reinke, John Shaw, Suzet Galindo-Martinez, Zhouwen Liu, Thomas Dupont, Erica Scaramuzza and Lynn Cain (Vanderbilt University).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hewett TE, Schultz SJ, Griffin LY, editors. Understanding and preventing noncontact ACL injuries. Champaign, IL: Human Kinetics; 2007. [Google Scholar]
- 2.Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish national anterior cruciate ligament register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 3.Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81:549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med. 1999;27:202–207. doi: 10.1177/03635465990270021501. [DOI] [PubMed] [Google Scholar]
- 5.Ma CB, Keifa E, Dunn W, Fu FH, Harner CD. Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17:81–83. doi: 10.1016/j.knee.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Schwartzberg R, Burkhart B, Lariviere C. Prediction of hamstring autograft diameter and length for anterior cruciate reconstruction. Am J Orthop. 2008;37:157–159. [PubMed] [Google Scholar]
- 7.Treme G, Diduch DR, Billante MJ, Miller MD, Hart JM. Hamstring graft size prediction: A prospective clinical evaluation. Am J Sports Med. 2008;36:2204–2209. doi: 10.1177/0363546508319901. [DOI] [PubMed] [Google Scholar]
- 8.Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1945–1949. doi: 10.1177/0363546507304667. [DOI] [PubMed] [Google Scholar]
- 9.Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Park SY, Oh H, Park S, Lee JH, Lee SH, Yoon KH. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-2085-4. [DOI] [PubMed] [Google Scholar]
- 11.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 13.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 15.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17:31–39. doi: 10.5435/00124635-200901000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 17.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 18.Barrett AM, Craft JA, Replogle WH, Hydrick JM, Barrett GR. Anterior cruciate ligament graft failure: a comparison of graft type based on age and tegner activity level. Am J Sports Med. 2011;39:2194–2198. doi: 10.1177/0363546511415655. [DOI] [PubMed] [Google Scholar]
- 19.Kaeding CC, Aros B, Pedroza A, et al. Allograft Versus Autograft Anterior Cruciate Ligament Reconstruction: Predictors of Failure From a MOON Prospective Longitudinal Cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: A case-control study. Am J Sports Med. 2009;37:2362–2367. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 21.Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1806–1816. doi: 10.1007/s00167-011-1473-5. [DOI] [PMC free article] [PubMed] [Google Scholar]