Abstract
Objective
To examine if the suicide rate of older adults prescribed antidepressants varies with age and to assess the proportion of older adults who died by suicide that had recently been prescribed antidepressants.
Methods
A population-based cohort study using a nationwide linkage of individual-level records was conducted on all persons aged 50+ living in Denmark during 1996–2006 (1,215,524 men and 1,343,568 women). Suicide rates by treatment status were calculated using data on all antidepressant prescriptions redeemed at pharmacies.
Results
Individual-level data covered 9,354,620 and 10,720,639 person-years for men and women, respectively. Men aged 50–59 who received antidepressants had a mean suicide rate of 185 (95% confidence interval [CI]: 160–211) per 100,000, whereas for those aged 80+ the rate was 119 (95% CI: 91–146). For women, the corresponding values were 82 (95% CI: 70–94) and 28 (95% CI: 20–35). Logistic regression showed a 2% and 3% decline in the rate for men and women, respectively, considered in treatment with antidepressants, with each additional year of age. An opposite trend was found for persons not in treatment. Fewer persons aged 80+ dying by suicide had received antidepressant prescriptions during the last months of life than younger persons.
Conclusion
An age-dependent decline in suicide rate for antidepressant recipients was identified. One reason could be that older adults respond better to antidepressants than younger age groups. Still, the increasing gap with age between estimated prevalence of depression and antidepressant prescription rate in persons dying by suicide underscores the need for assessment of depression in the oldest old.
Keywords: Aged, elderly, oldest old, suicide, antidepressant
On a worldwide level, suicide rates are highest in later life.1 It has been emphasized that older adults are a diverse population, and suicidal behavior should not be examined as a unitary phenomenon among those over age 65.2 Although antidepressants are indicated treatment for major depression in mid- and late life and major depression is a strong risk factor for suicide,3–6 little is known about their impact on rate of suicide in older adults. Research indicates a complex association between antidepressants, age, and suicide. A meta-analysis of 372 double-blinded, randomized trials found a higher relative risk of suicidal ideation and behavior for participants under age 25, no effect for those aged 25–64, and reduced risk for those aged 65 and over when comparing antidepressant treatment with placebo.7 This finding is partially supported by other studies.8–11 Nevertheless, the indication of benefit with respect to suicide risk in older adults warrants further examination.
Although the rate of major depression in the general population seems to decrease with age,12 more than 7% of older adults have been found to present clinically significant symptoms of depression.13,14 In several developed countries, antidepressants are prescribed more frequently to older adults than to younger age groups.15–18 Still, depression is widely under-treated in older adults.19–21 Furthermore, the proportion of suicides with major depression seems to increase with age into later life.22 Moreover, a substantial share of older adults dying by suicide are considered to suffer from an unidentified and untreated depression.23 As a means of reducing suicide-related morbidity and mortality in older adults, detection and treatment of depression has been heavily emphasized.24,25
It is striking contrast that older adults are more likely to be treated with antidepressant medications than younger people despite their lower prevalence of affective disorder. The increasing population share of older adults underlines the importance of examining suicide risks associated with antidepressant medications, particularly when considering suicide's close association to depression and the fact that suicide rates increase with age. Also, is relevant to estimate how large a proportion of older adults dying by suicide are not in treatment with antidepressants.
Our primary objective was to examine whether the relationship between antidepressant exposure and suicide differs as a function of age. Second, we examined if the proportion of persons redeeming antidepressants during the last months before dying by suicide varied by age. Danish linkage records allowed us to address these questions using nationwide longitudinal data.
METHODS
Register records on all persons living in Denmark during January 1, 1996, through December 31, 2006, were assessed. In Denmark, a unique personal identifier enables linkage on an individual level of various administrative registers, such as the Centralized Civil Register and the Registry of Causes of Death.
An open and dynamic cohort study design was applied by including all persons aged 50 years and over. People who reached the age of 50 years after January 1, 1996, entered the study sample on the date of their 50th birthday. Persons migrating in or out of the country were left- or right-hand truncated at the date of the respective event. Similarly, persons dying by causes other than suicide were censored on the date of death. The observation period ended on December 31, 2006. The event of interest, death by suicide, was defined as deaths recorded as suicide according to the 10th revision of the International Classification of Diseases and Related Health Problems26 or where the manner of death was stated as suicide.
Measures
Information on all antidepressants handed out at pharmacies, including date, drug type, and number of pills, is available since January 1, 1995 in the Register of Medicinal Product Statistics. Antidepressants are only available on prescription in Denmark. Pharmacies, furthermore, deliver medication to the homes of people with limited mobility. Drugs were grouped into tricyclic antidepressants (N06AA), selective serotonin reuptake inhibitors (SSRI: N06AB), and other types of antidepressants (N06AF, N06AG, and N06AX).
Using these data, it is possible to follow prescription patterns over time for each individual and form consecutive treatment periods. A person was considered in treatment with antidepressants from the date when a second prescription in a consecutive series was handed in at a pharmacy. The second prescription was preferred over the first because a substantial proportion of people discontinue treatment with antidepressants after having redeemed only one prescription.27 In addition, 4 weeks of treatment is likely to show evidence of improvement in those who will respond to treatment,28 a period that in many cases is equivalent to the length of the first prescription. Based on number of pills dispensed, we calculated when a subsequent prescription was due. Unless a new prescription was redeemed within the expected time frame, the person was considered as having ended treatment on the date when the new prescription was expected. A standard minimum dosage of 0.75 pills per day was assumed to take account of occasional misses. Individuals who switched to a different type of antidepressant within the expected time frame were from that date onward considered as users of the new type of antidepressant. Data covering the calendar year before study onset (i.e., 1995) were observed to identify subjects who were in treatment at the beginning of the observation period (i.e., January 1, 1996). The details of these and similar assumptions have been described elsewhere.23 We subsequently created a time-varying covariate denoting the current treatment status of each single individual. Additionally, variables on current age (expressed as whole integers) and current calendar year were created. All variables were updated on the exact date of change.
Statistical Analyses
Average and median age-specific suicide rates were calculated for each treatment group by gender. The denominator for the rates was calculated from the exact number of person-days spent in the different strata defined by age, gender, and treatment status. A χ2 test was performed to evaluate the independence of frequencies between age groups (i.e., age group 50–59 versus 80+ years).
The relationship between age+and suicide rate by treatment status was examined using Poisson regression. The following covariates were included in the model: calendar year (1996, 1997, ...2006), age (50, 51, 52, ...95+), and treatment status (no antidepressants, antidepressants). To examine the impact by both treatment categories in the same model, an interaction term covering age and treatment status was included. The outcome of the model was number of suicides offset by the logarithm of person-years/100,000. By calculating the exponential value of the estimates from the Poisson regression, we obtained the incidence rate ratio per 100,000 person-years. Dispersion of each regression model was evaluated by assessing the deviance divided by its degrees of freedom. Data management and analyses were carried out using SAS version 9.1.3 (2003, SAS Institute, Cary, NC).
RESULTS
In all, 2,567,914 persons aged 50 years and over (1,220,941 men and 1,346,973 women) were included in the study. Of these, 772,854 men and 915,331 women entered the study on January 1, 1996, and 427,603 men and 416,406 women entered the study on the date they reached the age of 50. During the 11 years of follow-up, 3,061 men and 1,456 women died by suicide. The study sample was observed for a total of 20,075,260 person-years (person-years: 9,354,620 for men, 10,720,639 for women).
With increasing age, a larger share of the older adults was prescribed antidepressants (Tables 1 and 2). Although 110,610 person-years (3%) among men aged 50–59 years were spent in treatment with antidepressants, it was 59,832 (8%) among the oldest old men aged 80+ (χ2 (1) = 46,912, p <0.0001). Also, a smaller proportion of women aged 50–59 years were in treatment with antidepressants than among those aged 80+ (χ2 (1) = 90,434, p <0.0001). SSRIs were most commonly prescribed, and the proportion increased with age (men: χ2 (1) = 40,756, p <0.0001; women: χ2 (1) = 57,733, p <0.0001).
TABLE 1.
Distribution of Person-Years, Suicide, and Suicide Rate per 100,000 with Regard to Prescriptions of Antidepressants and Drug Type for Men Aged 50 Years and Older Living in Denmark during January 1, 1996, to December 31, 2006
| Age Group | Person-Years (% of Age Group) | Number of Suicides (% of Age Group) | Mean Suicide Rate per 100,000 [95% CI] | Median Suicide Rate per 100,000 | |
|---|---|---|---|---|---|
| No antidepressants | 50–59 | 3,982,436 (97) | 903 (81) | 23 [21–24] | 22 |
| 60–69 | 2,652,509 (97) | 565 (78) | 21 [20–23] | 19 | |
| 70–79 | 1,649,199 (95) | 555 (84) | 34 [31–36] | 35 | |
| 80+ | 728,041 (92) | 498 (88) | 68 [62–74] | 72 | |
| Antidepressants | 50–59 | 110,610 (3) | 205 (19) | 185 [160–211] | 183 |
| 60–69 | 88,810 (3) | 156 (22) | 176 [148–203] | 166 | |
| 70–79 | 83,183 (5) | 108 (16) | 130 [105–154] | 133 | |
| 80+ | 59,832 (8) | 71 (12) | 119 [91–146] | 127 | |
| TCA | 50–59 | 21,740 (1) | 37 (3) | 170 [115–225] | 156 |
| 60–69 | 20,006 (1) | 37 (5) | 185 [125–245] | 160 | |
| 70–79 | 14,928 (1) | 19 (3) | 127 [70–185] | 131 | |
| 80+ | 6,446 (1) | 3 (1) | 47 [–6–99] | 0 | |
| SSRI | 50–59 | 59,762 (1) | 84 (8) | 141 [110–171] | 156 |
| 60–69 | 47,855 (2) | 59 (8) | 123 [92–155] | 113 | |
| 70–79 | 49,081 (3) | 51 (8) | 104 [75–132] | 96 | |
| 80+ | 39,065 (5) | 37 (7) | 95 [64–125] | 106 | |
| Other | 50–59 | 29,108 (1) | 84 (8) | 289 [227–350] | 324 |
| 60–69 | 20,949 (1) | 60 (8) | 286 [214–359] | 278 | |
| 70–79 | 19,174 (1) | 38 (6) | 198 [135–261] | 173 | |
| 80+ | 14,321 (2) | 31 (5) | 216 [140–293] | 207 |
TABLE 2.
Distribution of Person-Years, Suicide, and Suicide Rate per 100,000 with Regard to Prescriptions of Antidepressants and Drug Type for Women Aged 50 Years and Older Living in Denmark during January 1, 1996, to December 31, 2006
| Age Group | Person-Years (% of Age Group) | Number of Suicides (% of Age Group) | Mean Suicide Rate per 100,000 [95% CI] | Median Suicide Rate per 100,000 | |
|---|---|---|---|---|---|
| No antidepressants | 50–59 | 3,803,697 (95) | 309 (63) | 8 [7–9] | 8 |
| 60–69 | 2,709,797 (94) | 215 (57) | 8 [7–9] | 7 | |
| 70–79 | 2,032,746 (91) | 219 (65) | 11 [9–12] | 11 | |
| 80+ | 1,371,953 (87) | 202 (78) | 15 [13–17] | 15 | |
| Antidepressants | 50–59 | 218,669 (5) | 179 (37) | 82 [70–94] | 89 |
| 60–69 | 188,079 (6) | 159 (43) | 85 [71–98] | 80 | |
| 70–79 | 192,543 (9) | 116 (35) | 60 [49–71] | 56 | |
| 80+ | 203,154 (13) | 57 (22) | 28 [21–35] | 30 | |
| TCA | 50–59 | 49,694 (1) | 38 (8) | 76 [52–101] | 70 |
| 60–69 | 52,889 (2) | 40 (11) | 76 [52–99] | 69 | |
| 70–79 | 48,727 (2) | 31 (9) | 64 [41–86] | 58 | |
| 80+ | 30,366 (2) | 8 (3) | 26 [8–45] | 0 | |
| SSRI | 50–59 | 121,684 (3) | 71 (15) | 58 [45–72] | 51 |
| 60–69 | 94,513 (3) | 60 (16) | 63 [47–80] | 57 | |
| 70–79 | 97,520 (4) | 38 (11) | 39 [27–51] | 37 | |
| 80+ | 119,947 (8) | 25 (10) | 21 [13–29] | 23 | |
| Other | 50–59 | 47,291 (1) | 70 (14) | 148 [113–183] | 140 |
| 60–69 | 40,677 (1) | 59 (16) | 145 [108–182] | 146 | |
| 70–79 | 46,296 (2) | 47 (14) | 102 [72–131] | 92 | |
| 80+ | 52,841 (3) | 24 (9) | 45 [27–64] | 42 |
Fewer oldest old were considered to be in treatment with antidepressants at the time of death by suicide than younger persons. Among men aged 50–59 versus 80+ years, 19% and 12%, respectively, of suicides were in treatment at the time of death (χ2 (1) = 9.9, p = 0.0016). Among women, the corresponding percentages were 37% and 22%, respectively (χ2 (1) = 16.9, p <0.0001).
The suicide rate of men considered to be in treatment with antidepressants declined with age. Whereas the rate was 185 (95% confidence interval [CI]: 160–211) per 100,000 for those aged 50–59, it was 119 (95% CI: 91–146) for those aged 80 and over. Among women in treatment, the suicide rate was 82 (95% CI: 70–94) per 100,000 for those aged 50–59, whereas those aged 80+ years had a rate of 28 (95% CI: 21–35) per 100,000.
In contrast, the mean suicide rate increased with age for men not considered to be in treatment, from 23 (95% CI: 21–24) per 100,000 among those aged 50–59 to 68 (95% CI: 62–74) among the oldest old. Among women not in treatment, the corresponding rates were 8 (95% CI: 7–9) and 15 (95% CI: 13–17) per 100,000 for those aged 50–59 and 80+, respectively. Although younger age groups present fairly similar suicide rates, the oldest old aged 80 years and over have markedly higher suicide rates than younger age groups among those not prescribed antidepressants. An opposite pattern was found for women in treatment with antidepressants.
The Poisson regression analyses confirmed the decreasing trend among those in treatment with antidepressants; each additional year of age was associated with an approximately 2% decline in the male suicide rate (incidence rate ratio: 0.98; 95% CI: 0.98–0.99; Wald = 17.7; df = 1; p <0.0001) (Table 3). Among women in treatment, each additional year of age was associated with a 3% decline in suicide rate (incidence rate ratio: 0.97; 95% CI: 0.96–0.98; Wald = 63.0; df = 1; p <0.0001). Both models converged and over- and under-dispersion was within acceptable limits (i.e., close to 1).
TABLE 3.
Poisson Regression of Current Age and Its Impact on the Suicide Rate of Persons Aged 50 Years and Older Living in Denmark during January 1, 1996, to December 31, 2006
| Incidence Rate Ratio (95% CI) | df | Wald | p | |
|---|---|---|---|---|
| Men | ||||
| No antidepressants | 1.03 (1.03–1.04) | 1 | 360.9 | <0.0001 |
| Antidepressants | 0.98 (0.98–0.99) | 1 | 17.7 | <0.0001 |
| Women | ||||
| No antidepressants | 1.02 (1.15–1.29) | 1 | 51.4 | <0.0001 |
| Antidepressants | 0.97 (0.96–0.98) | 1 | 63.0 | <0.0001 |
Adjusted for calendar year.
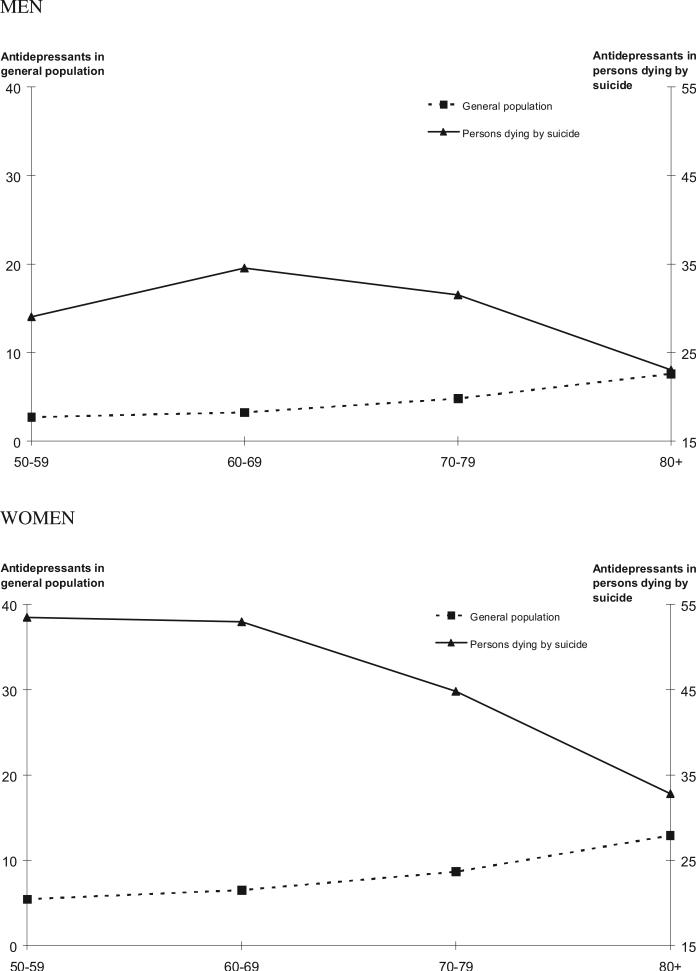
The proportion of people who died by suicide but had redeemed any antidepressant prescription (first as well as subsequent prescriptions in a treatment sequence) was found to decline with age (Tables 4 and 5). Within the last 90 days of life, fewer of those aged 80+ years had redeemed one or more antidepressant prescriptions than for those aged 50–59 (men: χ2 (1) = 6.95, p = 0.0084; women: χ2 (1) = 29.06, p <0.0001). Figure 1 display that although the proportion of people in the general population redeeming antidepressants rose steadily by age, an opposite trend was observed among those dying by suicide.
TABLE 4.
Proportion of Men Who Died by Suicide and Had Redeemed Antidepressant Prescriptions during the Last 365 Days of Life by Drug Type Among Persons Aged 50 Years and Older Living in Denmark during January 1, 1996, to December 31, 2006
| 50–59 |
60–69 |
70–79 |
80 + |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | N | Percent | pa | |
| Antidepressants during last 1 yearb | |||||||||
| Any type | 424 | (38) | 319 | (44) | 250 | (38) | 167 | (29) | 0.0003 |
| TCAc | 83 | (7) | 76 | (11) | 52 | (8) | 14 | (2) | <0.0001 |
| SSRIc | 281 | (25) | 186 | (26) | 179 | (27) | 118 | (21) | 0.0350 |
| Otherc | 176 | (16) | 129 | (18) | 85 | (13) | 67 | (12) | 0.0236 |
| Time since last prescription before suicide | |||||||||
| ≤6 mo | 368 | (33) | 283 | (39) | 226 | (34) | 150 | (26) | 0.0040 |
| ≤3 mo | 322 | (29) | 249 | (35) | 209 | (32) | 131 | (23) | 0.0084 |
| ≤1 mo | 213 | (19) | 143 | (20) | 135 | (20) | 89 | (16) | 0.0707 |
| ≤1 wk | 74 | (7) | 42 | (6) | 42 | (6) | 33 | (6) | 0.4856 |
Notes: TCA: tricyclic antidepressant.
χ2 test of differences between age groups 50–59 and 80+. Degrees of freedom = 1.
These calculations are based on any antidepressant prescription (also a first prescription).
Drug types are not mutually exclusive.
TABLE 5.
Proportion of Women Who Died by Suicide and Had Redeemed Antidepressant Prescriptions during the Last 365 Days of Life by Drug Type Among Persons Aged 50 Years and Older Living in Denmark during January 1, 1996, to December 31, 2006
| 50–59 |
60–69 |
70–79 |
80 + |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | N | Percent | pa | |
| Antidepressants during last 1 yearb | |||||||||
| Any type | 326 | (67) | 247 | (66) | 183 | (55) | 115 | (44) | <0.0001 |
| TCAc | 83 | (17) | 71 | (19) | 61 | (18) | 25 | (10) | 0.0065 |
| SSRIc | 217 | (44) | 155 | (41) | 111 | (33) | 86 | (33) | 0.0028 |
| Otherc | 134 | (27) | 103 | (28) | 78 | (23) | 41 | (16) | 0.0004 |
| Time since last prescription before suicide | |||||||||
| ≤6 mo | 294 | (60) | 224 | (60) | 171 | (51) | 107 | (41) | <0.0001 |
| ≤3 mo | 261 | (53) | 198 | (53) | 150 | (45) | 85 | (33) | <0.0001 |
| ≤1 mo | 160 | (33) | 133 | (36) | 97 | (29) | 57 | (22) | 0.0020 |
| ≤1 wk | 48 | (10) | 36 | (10) | 28 | (8) | 16 | (6) | 0.0891 |
Notes: TCA: tricyclic antidepressant.
χ2 test of differences between age groups 50–59 and 80+. Degrees of freedom = 1.
These calculations are based on any antidepressant prescription (also a first prescription).
Drug types are not mutually exclusive.
FIGURE 1.
Percentage of the general population considered to be in treatment with antidepressants and percentage of persons dying by suicide who received antidepressants within the last 3 months before death in people aged 50 years and older living in Denmark during January 1, 1996, through December 31, 2006.
DISCUSSION
We found an inverse relationship between age and suicide rate in those considered to be in treatment with antidepressants. This is, to our knowledge, the first study to document this trend using data for an entire nation of older adults and using death by suicide as outcome. Although the proportion of middle-aged and older adults in treatment with an antidepressant increased with age in the second half of life, only a small proportion of those dying by suicide were considered to be in treatment with antidepressants at the time of death, and that proportion decreased with increasing age.
Age Effect
The difference between rates of persons considered to be in treatment and not in treatment is likely to be due to psychiatric characteristics of the two groups. However, distinctly different age patterns were identified for those in treatment with antidepressants versus not in treatment. The inverse age effect of the suicide rate for people in treatment, albeit minor in magnitude, supports previous meta-analyses concerning suicidal ideation and self-harming acts.7 It could be that antidepressant administration results in lower levels of suicidal ideation and behavior in older than in middle-aged adults simply because they are a more efficient and targeted intervention for suicide in depressed elders. However, other explanations are also possible.
Depression might be disproportionally under-diagnosed, and consequently not treated, in the very high age groups.29 Such selection bias would explain the higher suicide rate among the oldest old who are not in treatment. Our finding of a lower proportion of oldest old suicides receiving antidepressants in the time before death supports this interpretation. It has been suggested that the very old with depression who die by suicide are less likely to receive treatment.30 At the same time, one would expect those older adults who did receive treatment to have more severe illness (i.e., less likely to escape detection) and to be at higher risk for suicide on that basis. If so, then the finding that rates were significantly lower among older adults than younger adults who did receive treatment supports the notion that antidepressants have a greater “protective” effect with increasing age in the second half of life.
On the other hand, given that the oldest old generally have higher levels of comorbid medical illness than younger age groups, they are likely to be in more frequent contact with general practitioners and other healthcare providers. It is thus possible that depression is more frequently identified and treated in the oldest old. A possible consequence could be that less severe depressions among older adults are treated successfully, leaving fewer but more chronic and treatment-resistant depressions unresolved. In addition, more frequent visits to healthcare providers might secure a closer follow-up with treatment and improve adherence. Furthermore, confounding by indication and selective survival are also a concern. For instance, persons with a high level of suicidal ideation might not live to reach high ages.
Investigators have argued that suicidal behavior results from a biologic predisposition or “diathesis” independent from depression.31 Such a predisposition may be exacerbated by aging-related biologic processes that in turn might be more responsive to antidepressants. For instance, SSRIs are selectively active on central serotonin systems, dysregulation of which has been implicated in the pathogenesis of impulsive and aggressive behavior, including suicide.32 Aging-related changes in indolamine function have been documented,33 potentially making antidepressants relatively more effective in buffering the risk for suicide in the brain of an older than a younger person. Also, psychopathologic expressions of depression may differ by age, for example, in depressive subtypes, natural history and severity, presence of concurrent medical and psychiatric disorders, and level of associated features, such as impulsivity.13,34 The association can, however, also be a result of spurious effects (see Strengths and Limitations, below).
Antidepressants Redeemed by Persons Dying by Suicide
With increasing age, a declining proportion of those dying by suicide received antidepressants in the time shortly before death. Consistent with prior findings,23 less than one of eight men and one of four of women aged 80+ years dying by suicide were in treatment with antidepressants at the time of death. International findings estimate that fewer than 28% of older adults aged 65 years and over are in treatment with antidepressants at the time of death by suicide.35–37 This is supported by earlier findings showing that only a marginal proportion were in mental healthcare at the time of their deaths.38 In contrast, clinically significant symptoms of major depression were identified in 54%–87% of older adults who died by suicide.4 This could suggest that as many as half of the oldest old dying by suicide are suffering from an untreated depression.
Psychological autopsy studies furthermore indicate that older adults dying by suicide present more often than younger adults with relatively uncomplicated depressions, which should respond well to treatment.22 In terms of preventing suicide in older adults, there are pathways worth exploring further. Promising results have been presented for collaborative care models where depression specialists and case managers are embedded in the primary care practice to optimize treatment outcomes.24 The potential of this approach gains in strength by the fact that as many as 50%–69% of adults aged 60 years and over who later die by suicide contact their general practitioner during the last month of life.36,39 Medical treatment of depression in older adults has also been recommended by review panels.6
Strengths and Limitations
A major strength of the study is the individual-level and nationwide data available through the Danish registers. The findings of the current study are based on register records on every single individual and are fully representative for the entire population aged 50 and over in Denmark using complete information on all prescribed antidepressants redeemed at pharmacies.
The findings reported by this study can, however, only be considered as indicative; redeemed antidepressant prescriptions are not an optimal proxy for depression. It should be taken into account that older people are more indiscriminately treated with antidepressants than younger age groups, including for conditions in which the risk of suicide is relatively lower than it is for depression (e.g., chronic pain syndromes, anxiety, irritable bowel syndrome, and sexual dysfunction).40–44 Unfortunately, the register data do not provide information on the specific diagnosis for which the medication was prescribed.
We only know when antidepressant prescriptions are redeemed at pharmacies. No information is provided on free samples handed out by general practitioners or medication distributed during hospitalizations. Likewise, we have no indication of who actually consumed the drugs. Also, due to data limitations, it was not feasible to adjust findings for other potentially relevant confounders (e.g., medical and psychiatric conditions, comorbidity, disability, and cognitive impairment). Circumstances related to cohort effects can also not be explained.
Studies suggest that the risk of suicidal behavior is particularly elevated during the first days or weeks of treatment with antidepressants, also in an elderly sample.45,46 Our treatment specification implies that persons who die by suicide while in treatment with a first prescription will not be considered as being in treatment. Additional analyses where the first prescription period was considered as active treatment obtained similar trends when assessed by Poisson regression (available upon request).
The current findings were derived using Danish data (i.e., in a setting with free public health care and subsidies available for purchasing antidepressants if needed). It is not certain that the findings apply to other settings.
In sum, the oldest old proportionally receive more antidepressants than younger age groups and also have the highest suicide rate. Nevertheless, we found a declining suicide rate with increasing age among those in treatment. Although the causal pathways of this are not clarified, it is possible that antidepressant treatment protects the oldest old from death by suicide. A remarkably small proportion of older adults who died by suicide had received these medications. This finding underscores the need for improved identification of depression in this vulnerable group.
Acknowledgments
AE received funding for the project by the Danish Ministry of Social Welfare (Fund for Prevention of Suicide and Suicide Attempts), the Danish Health Insurances Foundation, the Danielsens Foundation, the EGV Foundation, and from the Augustinus Foundation. YC is supported by the National Institute of Mental Health (grant P20 MH071897).
Contributor Information
Annette Erlangsen, The Research Unit, Mental Health Centre Copenhagen, Capital Region of Denmark, Denmark and Department of Mental Health, Johns Hopkins School of Public Health, Baltimore, Maryland
Yeates Conwell, Center for the Study and Prevention of Suicide and Department of Psychiatry, University of Rochester Medical Center, Rochester, New York.
References
- 1.World Health Organization [June 6, 2011];Distribution of suicide rates (per 100, 000) by gender and age. 2000 Available at http://www.who.int/mental_health/prevention/suicide/suicide_rates_chart/en/index.html.
- 2.Erlangsen A, Bille-Brahe U. Jeune B: Differences in suicide between the old and the oldest old. J Gerontol Psychol Sci Soc Sci. 2003;58B:314–322. doi: 10.1093/geronb/58.5.s314. [DOI] [PubMed] [Google Scholar]
- 3.Erlangsen A, Zarit SH, Tu X, et al. Suicide among older psychiatric inpatients: an evidence-based study of a high-risk group. Am J Geriatr Psychiatry. 2006;14:734–741. doi: 10.1097/01.JGP.0000225084.16636.ec. [DOI] [PubMed] [Google Scholar]
- 4.Conwell Y, Thompson C. Suicidal behavior in elders. Psychiatr Clin North Am. 2008;31:333–356. doi: 10.1016/j.psc.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arroll B, MacGillivray S, Ogston S, et al. Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ. 2003;326:1014. doi: 10.1136/bmj.326.7397.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charney DS, Reynolds CF, III, Lewis L, et al. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. 2003;60:664–672. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- 7.Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880. doi: 10.1136/bmj.b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbui C, Esposito E, Cipriani A. Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ. 2009;180:291–297. doi: 10.1503/cmaj.081514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalmar S, Szanto K, Rihmer Z, et al. Antidepressant prescription and suicide rates: effect of age and gender. Suicide Life Threat Behav. 2008;38:363–374. doi: 10.1521/suli.2008.38.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibbons RD, Brown CH, Hur K, et al. Relationship between anti-depressants and suicide attempts: an analysis of the Veterans Health Administration data sets. Am J Psychiatry. 2007;164:1044–1049. doi: 10.1176/ajp.2007.164.7.1044. [DOI] [PubMed] [Google Scholar]
- 11.Hall WD, Mant A, Mitchell PB, et al. Association between anti-depressant prescribing and suicide in Australia, 1991-2000: trend analysis. BMJ. 2003;326:1008–1011. doi: 10.1136/bmj.326.7397.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Birnbaum HG, Shahly V, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety. 2010;27:351–364. doi: 10.1002/da.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 14.Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113:372–387. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- 15.Hansen DG, Rosholm JU, Gichangi A, et al. Increased use of antidepressants at the end of life: population-based study among people aged 65 years and above. Age Ageing. 2007;36:449–454. doi: 10.1093/ageing/afm056. [DOI] [PubMed] [Google Scholar]
- 16.Blazer DG, Hybels CF, Simonsick E, et al. Marked differences in antidepressant use by race in an elderly community sample: 1986-1996. Am J Geriatr Psychiatry. 2000;157:1089–1094. doi: 10.1176/appi.ajp.157.7.1089. [DOI] [PubMed] [Google Scholar]
- 17.Hartikainen S, Klaukka T. Use of psychotropics is high among very old people. Eur J Clin Pharmacol. 2004;59:849–850. doi: 10.1007/s00228-003-0702-3. [DOI] [PubMed] [Google Scholar]
- 18.Middleton N, Gunnell D, Whitley E, et al. Secular trends in anti-depressant prescribing in the UK, 1975-1998. J Public Health Med. 2001;23:262–267. doi: 10.1093/pubmed/23.4.262. [DOI] [PubMed] [Google Scholar]
- 19.Barry LC, Abou JJ, Simen AA, et al. Under-treatment of depression in older persons. J Affect Disord. 2012;136:789–796. doi: 10.1016/j.jad.2011.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonnenberg CM, Deeg DJ, Comijs HC, et al. Trends in antidepressant use in the older population: results from the LASA-study over a period of 10 years. J Affect Disord. 2008;111:299–305. doi: 10.1016/j.jad.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Garrido MM, Kane RL, Kaas M, et al. Use of mental health care by community-dwelling older adults. J Am Geriatr Soc. 2011;59:50–56. doi: 10.1111/j.1532-5415.2010.03220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conwell Y, Duberstein PR, Cox C, et al. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153:1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 23.Erlangsen A, Canudas-Romo V, Conwell Y. Increased use of antidepressants and decreasingsuicide rates: a population-based study using Danish register data. J Epidemiol Commun Health. 2008;62:448–454. doi: 10.1136/jech.2007.061580. [DOI] [PubMed] [Google Scholar]
- 24.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. A randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 25.Erlangsen A, Nordentoft M, Conwell Y, et al. Key considerations for preventing suicide in older adults: consensus opinions of an expert panel. Crisis. 2011;32:106–109. doi: 10.1027/0227-5910/a000053. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organisation . International Statistical Classification of Diseases and Related Health Problems, 10th revision. World Health Organisation; Geneva: 2007. [Google Scholar]
- 27.Rosholm JU, Andersen M, Gram LF. Are there differences in the use of selective serotonin reuptake inhibitors and tricyclic anti-depressants? A prescription database study. Eur J Clin Pharmacol. 2001;56:923–929. doi: 10.1007/s002280000234. [DOI] [PubMed] [Google Scholar]
- 28.Beyer JL. Managing depression in geriatric populations. Ann Clin Psychiatry. 2007;19:221–238. doi: 10.1080/10401230701653245. [DOI] [PubMed] [Google Scholar]
- 29.Lebowitz BD, Pearson JL, Schneider LS, et al. Diagnosis and treatment of depression in late life. JAMA. 1997;278:1186–1190. [PubMed] [Google Scholar]
- 30.Waern M, Rubenowitz E. Wilhelmson K: Predictors of suicide in the old elderly. Gerontology. 2003;49:328–334. doi: 10.1159/000071715. [DOI] [PubMed] [Google Scholar]
- 31.Mann JJ, Waternaux C, Haas GL, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–186. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 32.Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 33.Goldberg S, Smith GS, Barnes A, et al. Serotonin modulation of cerebral glucose metabolism in normal aging. Neurobiol Aging. 2004;25:167–174. doi: 10.1016/s0197-4580(03)00088-5. [DOI] [PubMed] [Google Scholar]
- 34.Katona C, Shankar K. Depression in old age. Rev Clin Gerontol. 2004;14:283–306. [Google Scholar]
- 35.Bruvik-Ruhlmann PEG, Kristensen IB, Nielsen KR. Selvmord hos aeldre i Arhus Amt i perioden 1993-2000. Et deskriptivt studium. Ugeskr Laeger. 2004;166:4151–4154. [PubMed] [Google Scholar]
- 36.Pitkälä K, Isometsä ET, Henriksson MM, et al. Elderly suicide in Finland. Int Psychogeriatr. 2000;12:209–220. [PubMed] [Google Scholar]
- 37.Abrams RC, Leon AC, Tardiff K, et al. Antidepressant use in elderly suicide victims in New York city: an analysis of 255 cases. J Clin Psychiatry. 2009;70:312–317. doi: 10.4088/jcp.08m04243. [DOI] [PubMed] [Google Scholar]
- 38.Conwell Y, Lyness JM, Duberstein PR, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 39.Harwood D, Hawton K, Hope T, et al. Suicide in older people: mode of death, demographic factors, and medical contact before death. Int J Geriatr Psychiatry. 2000;15:736–743. doi: 10.1002/1099-1166(200008)15:8<736::aid-gps214>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 40.Sindrup SH, Bjerre U, Dejgaard A. The selective serotonin reup-take inhibitor citalopram relieves the symptoms of diabetic neuropathy. Clin Pharmacol Ther. 1992;52:547–552. doi: 10.1038/clpt.1992.183. [DOI] [PubMed] [Google Scholar]
- 41.Creed F. How do SSRIs help patients with irritable bowel syndrome? Gut. 2006;55:1065–1067. doi: 10.1136/gut.2005.086348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giuliano F. 5-Hydroxytryptamine in premature ejaculation: opportunities for therapeutic intervention. Gut. 2007;30:79–84. doi: 10.1016/j.tins.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Rahme E, Dasgupta K, Turecki G, et al. Risks of suicide and poisoning among elderly patients prescribed selective serotonin reuptake inhibitors: a retrospective cohort study. J Clin Psychiatry. 2008;69:349–357. doi: 10.4088/jcp.v69n0303. [DOI] [PubMed] [Google Scholar]
- 44.Godfrey RG. A guide to the understanding and use of tricyclic anti-depressants in the overall management of fibromyalgia and other chronic pain syndromes. Arch Intern Med. 1996;156:1047–1052. [PubMed] [Google Scholar]
- 45.Jick H, Kaye JA, Jick SS. Antidepressants and the risk of suicidal behaviors. JAMA. 2004;292:338–343. doi: 10.1001/jama.292.3.338. [DOI] [PubMed] [Google Scholar]
- 46.Rubino A, Roskell N, Tennis P, et al. Risk of suicide during treatment with venlafaxine, citalopram, fluoxetine, and dothiepin: retrospective cohort study. BMJ. 2007;334:242. doi: 10.1136/bmj.39041.445104.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]