Abstract
Background
High blood pressure is a significant risk factor for cardiovascular disease and mortality. Japan has traditionally had higher levels of measured blood pressure than many Western countries and reducing levels of hypertension has been a major focus of Japanese health policy over recent decades. In the West, hypertension is strongly associated with sociodemographic and behavioral (smoking and BMI) factors; studies of the association between sociodemographic factors and biological indicators have not been fully explored in the elderly population of Japan using nationally representative survey data.
Objective
To describe hypertension prevalence rates with increasing age and to examine the link between sociodemographic and behavioral factors (including age, gender, education, residence, smoking, and BMI) and measures of blood pressure and overall hypertension in the Japanese population aged 68 years-or-older.
Methods
Data were collected in 2006 during the fourth wave of the Nihon University Japanese Longitudinal Study of Aging (NUJLSOA), a nationally representative sample of those 68 or older. The analytic sample includes 2,634 participants. Pulse pressure (PP), Systolic (SBP), diastolic (DBP), and mean blood pressure (MBP), as well as hypertension, were regressed on sociodemographic and behavioral factors.
Results
There is no significant difference in the prevalence of overall hypertension by age for men and women from ages 68–69 to 90+. Higher BMI and older age were linked to higher blood pressure and higher chance of having hypertension. More years of education and being female were associated with a lower likelihood of measured hypertension. Smoking, rural residence, and living alone were not significantly associated with the outcome measures.
Conclusion
The increase in hypertension with higher BMI raises concerns about future health in Japan as BMI increases. The lack of a relationship between smoking and any measure of blood pressure or hypertension is an indicator that smoking may have different effects in Japan than in other countries. Because there is no effect of living alone on blood pressure, compliance with drug regimes may not enhanced by living with others in Japan.
Keywords: blood pressure, elderly, hypertension, Japan
Introduction
High blood pressure is a significant risk factor for cardiovascular disease and mortality [1]. Japan has traditionally had higher levels of measured blood pressure than many Western countries. As a result, decreasing levels of hypertension have been a major focus of Japanese health policy over recent decades [2, 3]; a combination of an increase in antihypertensive medication usage [3, 4] and population based interventions to reduce salt intake have contributed to declining levels of hypertension in recent years [5]. Despite these gains, hypertension prevalence rates still remain relatively high in Japan [6]. In the West, hypertension is strongly associated with sociodemographic factors [7, 8]; studies of the association between sociodemographic factors and biological indicators have not been fully explored in the elderly population of Japan using nationally representative survey data. Better understanding of these associations will allow us to develop more effective policies and interventions to improve health outcomes and reduce health inequalities. We hypothesize that sociodemographic factors will be associated with blood pressure levels and hypertension in Japanese elderly.
In this paper we examine four indices of blood pressure, systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP), and mean blood pressure (MBP) as well as overall hypertension. SBP tends to increase with age, although the relationship is not as clear among older age groups in Japan [9, 10], and most researchers and clinicians agree that it is important in predicting risk in older populations [11]. On the other hand, DBP decreases in the elderly populations [11]. As a result of changes in SBP and DBP, PP, which is the difference between the two, has been suggested as a better predictor of risk for cardiovascular disease and mortality in the elderly [12, 13]. Studies have suggested that both PP and MBP, which is based on DBP and PP, are better indicators of cardiovascular risk in Asian populations so we include them in our analyses [13, 14, 15].
In general, studies conducted in Western countries have shown that higher blood pressure (SBP, DBP and PP) is associated with lower socio-economic status (SES), of which education is an indicator [7, 16, 18]. One mechanism that has been proposed for the role of SES is through the associated educational advantage, particularly, the health specific knowledge and better ability to follow medical advice that comes with more education [17]. On the other hand, the literature on links between SES and health in Japan is mixed; some studies have shown that, as in other industrialized countries, people with higher SES tend to have better health outcomes [19, 20], whereas others have shown the association does not exist among the elderly and may differ by gender in Japan [21].
Urban/rural residence [22, 23] and living arrangement (i.e. living alone or with others) [24] are two other sociodemographic characteristics that have been associated with differential health outcomes in Japan, with rural residence and living alone associated with worse health outcomes. One study found that stroke mortality tended to be higher in rural areas of Japan [22] whereas the association between living alone and health outcomes is less consistent; some researchers report lower mortality [24] and others report worse self-rated health [25].
Interestingly, gender is a mediating factor in the relationship between living alone and worsened health in Japan, with elderly men who live alone having worse outcomes than women [26]. In general, gender is linked to increased levels of blood pressure and hypertension in some countries, with men having an earlier onset but women having higher prevalence at older ages [27, 28]. However, gender differences in hypertension in the elderly population of Japan are small compared to those in the West; on the other hand, gender differences in specific aspects of hypertension, such as high DBP, are larger in Japan [29]. Studies on the association of gender on blood pressure levels in Japan have focused on younger age groups; therefore it is still not known how gender influences blood pressure, and subsequently hypertension, in this elderly population.
Behavioral factors also influence blood pressure and hypertension. Higher body mass is thought to be a risk factor for hypertension, particularly when the body mass index (BMI) is in the obese range (≥30 kg/m2) [11]. However, research findings are inconsistent on the relationship between obesity and elevated blood pressure levels in Japan, particularly at older ages [30, 31]. Smoking is another well-known risk factor for cardiovascular disease [11]; researchers have shown that smoking increases blood pressure and even counters the positive effects of some antihypertensive medication [32]. However, acute and long-term effects of smoking on hypertension are still not clear among the Japanese population [33].
In order to gain a better understanding of the association between sociodemographic characteristics, behavioral factors and health outcomes, we examine the association of blood pressure and hypertension, and education, rural/urban residence, living arrangement, gender, age, smoking, BMI, and antihypertensive medication usage among the elderly Japanese population.
Methods
Data Sources
This study utilizes data collected in 2006 during the fourth wave of the Nihon University Japanese Longitudinal Study of Aging (NUJLSOA). NUJLSOA is a nationally representative sample of the Japanese population aged 65 years-or-older at baseline collected by the Nihon University Tokyo, Japan. The first wave of data was collected in 1999 and subsequent waves were conducted in 2001, 2003, and 2006. Younger participants were added at the second and third waves so as to remain nationally representative of the 65 years-or-older population at each wave. New participants were not added at the fourth wave in 2006 so that the fourth wave contains data from participants aged 68 years-or-older. The survey has included questions on hypertension and self-reports of antihypertensive medication usage. In addition, at the fourth wave of the survey, blood pressure measurement was added to the survey. Complete information on the design and methods of the study can be found on the website of the Nihon University [34].
The fourth wave of the survey includes 3,403 participants of whom 68% participated in the collection of blood pressure measurements (n=2,330); and of this sample 2,073 had a measured blood pressure recording and responded to all sociodemographic, health behavior, and medication questions included in the analysis and constitute the total analytic sample.
The sample is weighted to represent a national population and for this analysis weights were adjusted to account for having missing data on measured blood pressure. The adjustment was created by multiplying the normalized weight of the sample by the inverse of the predicted probability that each participant would have a blood pressure measurement. The predicted probability was based on age, sex, and level of education. The adjusted weight was used in all analyses.
Measurements
Blood Pressure Collection
Blood pressure in NUJLSOA was measured using the digital OMRON HEM-762 (OMRON, Kyoto, Japan), validation information for the device is provided by the manufacture [35]. For blood pressure measurement, the participant was typically in a seated position and the recording was performed on the left arm by the interviewer. Blood pressure was measured three times with approximately one minute between measurements and the average of the three readings was used for analysis. If fewer than three readings were performed, then the average of those readings was included.
Blood Pressure
The measures of blood pressure included in this study were SBP (mmHg), DBP (mmHg), PP (mmHg) and MBP (mmHg). PP was calculated by subtracting DBP from SBP. MBP was computed as DBP + (PP / 3).
Hypertension
Measured hypertension was defined as having SBP ≥ 140 mmHg or a DBP ≥ 90 mmHg [36]. Overall hypertension prevalence was indicated by either having measured hypertension or self-reported antihypertensive medication usage. The question of whether or not participants were using blood pressure medication was asked of those participants who responded affirmatively to ever having experienced hypertension. Table 1 provides descriptive measures on the blood pressure variables.
Table 1.
Descriptive statistics for NUJLSOA sample (mean, percent, and number of participants) (n=2073).
| Measure | Mean/percent | SD |
|---|---|---|
| Systolic blood pressure (mmHg) | 155.2 | 22.7 |
| Diastolic blood pressure (mmHg) | 82.1 | 12.4 |
| Pulse Pressure (mmHg) | 73.2 | 18.2 |
| Mean blood pressure (mmHg) | 106.5 | 14.2 |
| Prevalence of high systolic blood pressure (%) | 73.41 | --- |
| Prevalence of high diastolic blood pressure (%) | 24.73 | --- |
| Measured hypertension (%) | 74.15 | --- |
| Overall hypertension (measured high or medication use) (%) | 81.87 | --- |
| Education | --- | |
| ≤8 years (%) | 30.07 | --- |
| 9–11 years (%) | 39.28 | --- |
| ≥12 years (%) | 30.65 | --- |
| Rural residence (%) | 28.5 | --- |
| Living alone (%) | 14.46 | --- |
| Female (%) | 53.66 | --- |
| Age (years) | 75.8 | 7.56 |
| Use of Antihypertensive medication (%) | 35.50 | --- |
| Non-smoker (%) | 37.72 | --- |
| Former smoker (%) | 50.11 | --- |
| Current smoker (%) | 12.18 | --- |
| Body mass index (kg/m2) | 22.6 | 4.0 |
Sociodemographic
Socioeconomic status (SES), measured by years of education, was divided into three categories, less than 8 years, 9–11 years, and more than 12 years. For our analyses, we selected the middle education group (9–11 years) as the referent group. Rural residence, living alone, and gender were coded as dichotomous variables. Age was categorized into six groups (68–69, 70–74, 75–79, 80–84, 85–89, and 90 and over). In order to observe age-related differences in blood pressure and hypertension, we selected the youngest age group as the referent category for all the analyses and examined differences of the other age groups from this group.
Health Behavior and Medication
Smoking status was separated into three categories; never smoked, former smoker, and current smoker because the effect of smoking on blood pressure was not clear from existing literature. Never smokers were used as the referent group. BMI was used as a continuous measure and was calculated by dividing self-reported weight (kg) by the square of self-reported height (m) (BMI=kg/m2). Use of antihypertensive medication among those who said they had experienced hypertension was coded as a dichotomous variable, indicating medication usage or not.
Ethical Concerns
The study procedure was approved by the Ethics Committee of the School of Medicine, Nihon University.
Statistical Methods
All analyses were conducted on Statistical Analysis System (SAS) 9.1 (SAS Institute, Inc, Cary, NC). Regression analysis of blood pressure and hypertension measures on sociodemographic indicators was used in order to examine the independent effect of each of the variables while controlling for the others. Analysis of continuous measures of blood pressure was based on Ordinary Least Squares (OLS) regression (Table 2). Dichotomous indicators of measured hypertension and overall hypertension were regressed on independent variables using the logistic regression procedure (Table 3).
Table 2.
Regression coefficients from OLS-regressions of blood pressure regressed on sociodemographic characteristics and health behavior (n=2073).
| Systolic blood pressure | Diastolic blood pressure | Pulse pressure | Mean blood pressure | |
|---|---|---|---|---|
| ≤8 years of education1 | −1.96 | −1.12 | −0.84 | −1.40 |
| ≥12 years of education | −1.51 | −0.19 | −1.32 | −0.63 |
| Rural residence | 0.63 | 0.85 | −0.22 | 0.78 |
| Living alone | −1.74 | 0.25 | −1.99 | −0.42 |
| Female | −0.66 | −0.55 | −0.11 | −0.58 |
| 70–74 years old2 | 0.65 | −1.34 | 1.98 | −0.68 |
| 75–79 years old | 1.47 | −3.22** | 4.68** | −1.66 |
| 80–84 years old | 5.17* | −2.71* | 7.87*** | −0.08 |
| 85–89 years old | 5.37* | −4.42** | 9.79*** | −1.16 |
| 90+ years old | 3.11 | −4.25* | 7.36** | −1.80 |
| Antihypertensive medication | 3.17** | 0.14 | 3.03*** | 1.15 |
| Former smoker3 | −0.69 | 0.67 | −1.35 | 0.22 |
| Current smoker | 0.83 | 0.62 | 0.21 | 0.69 |
| Body mass index (kg/m2) | 0.74*** | 0.33*** | 0.41** | 0.47*** |
| R2 | 0.02 | 0.03 | 0.05 | 0.02 |
| df | 14 | 14 | 14 | 14 |
9–11 years of education was used as the referent category
68–69 was used as the referent category
Non-smokers was used as the referent category
Table 3.
Odds ratios and 95% confidence intervals from logistic regressions of hypertension regressed on sociodemographic characteristics and health behavior (n=2073).
| Measured hypertension (either high systolic or diastolic) | Overall hypertension (measured high or medication) | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| ≤8 years of education1 | 0.96 | 0.78 – 1.19 | 1.10 | 0.86 – 1.40 |
| ≥12 years of education | 0.79 | 0.65 – 0.95 | 1.03 | 0.83 – 1.28 |
| Rural residence | 1.05 | 0.88 – 1.26 | 1.11 | 0.90 – 1.37 |
| Living alone | 0.87 | 0.69 – 1.08 | 0.85 | 0.66 – 1.10 |
| Female | 0.81 | 0.67 – 0.97 | 0.95 | 0.77 – 1.17 |
| 70–74 years old2 | 1.00 | 0.78 – 1.29 | 1.20 | 0.91 – 1.58 |
| 75–79 years old | 1.21 | 0.90 – 1.64 | 1.83 | 1.31 – 2.57 |
| 80–84 years old | 1.37 | 0.98 – 1.91 | 1.76 | 1.21 – 2.55 |
| 85–89 years old | 1.22 | 0.83 – 1.82 | 2.05 | 1.30 – 3.23 |
| 90+ years old | 0.97 | 0.57 – 1.67 | 2.29 | 1.17 – 4.46 |
| Antihypertensive medication | 1.35 | 1.13 – 1.60 | ----- – ----- | |
| Former smoker3 | 1.16 | 0.94 – 1.43 | 1.05 | 0.82 – 1.33 |
| Current smoker | 1.13 | 0.84 – 1.52 | 0.96 | 0.69 – 1.34 |
| Body mass index (kg/m2) | 1.06 | 1.03 – 1.09 | 1.13 | 1.10 – 1.17 |
| Chi-square | 64.59 | 93.58 | ||
| df | 14 | 13 | ||
| BIC | −113 | −134 | ||
| pseudo-R2 | 0 | 0 | ||
Values in bold font indicate significant findings.
9–11 years of education was used as the referent category
68–69 was used as the referent category
Non-smokers was used as the referent category
Results
Descriptive Statistics
Table 1 shows the descriptive statistics for the blood pressure, hypertension, sociodemographic, health behavior, and medication measures. Average SBP for the sample (155.5 mmHg) was much higher than 140 mmHg, which is the criterion for systolic hypertension. However, DBP for the sample (82.2 mmHg) was lower than 90 mmHg, the cutoff value for hypertension. Measured hypertension was found in about three-fourths (74.15%) of the sample, whereas the prevalence of overall hypertension was 81.87%. Less than half the sample (35.50%) reported antihypertensive medication usage. These figures confirm previously reported high levels of hypertension among the older Japanese population.
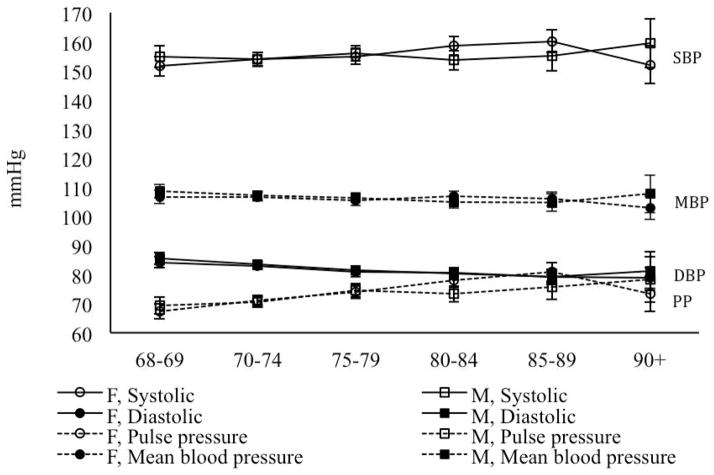
Blood Pressure by Age and Gender
Before we examine the associations of blood pressure and hypertension with sociodemographic variables using multivariate analyses, we examine levels of SBP, DBP, PP, and MBP by age and gender (Figure 1). There are no significant differences by gender at any age in these measures. There is little change with age in level of SBP and MBP in either men or women at these older ages. There is some reduction in DBP at older ages (75 years or older). Among females 68–69 years-old average DBP is 84 mmHg (95% CI: 82–86 mmHg) versus 79 mmHg (95% CI: 77–81 mmHg) for the 85–89 age group. The drop in DBP occurs at a slightly earlier age among males. As a result of the stability of SBP and this decline in DBP, PP increases slightly with age.
Figure 1.
Average blood pressure by age and sex.
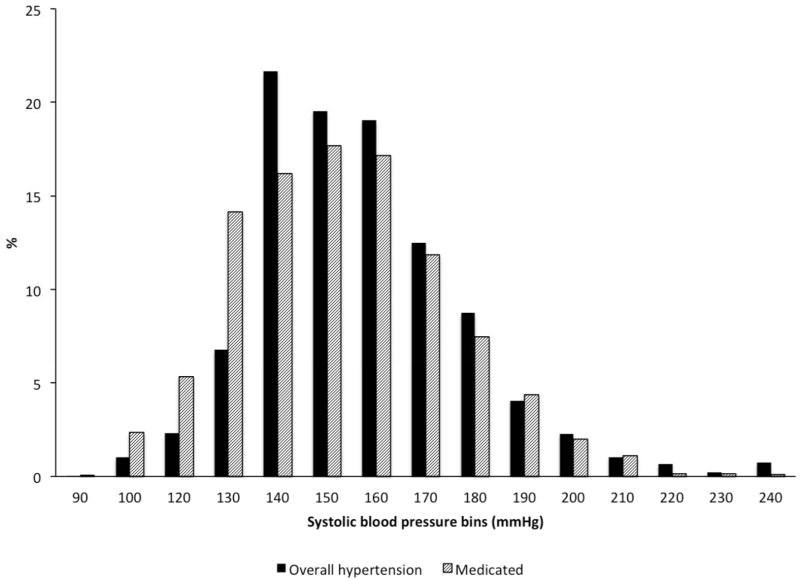
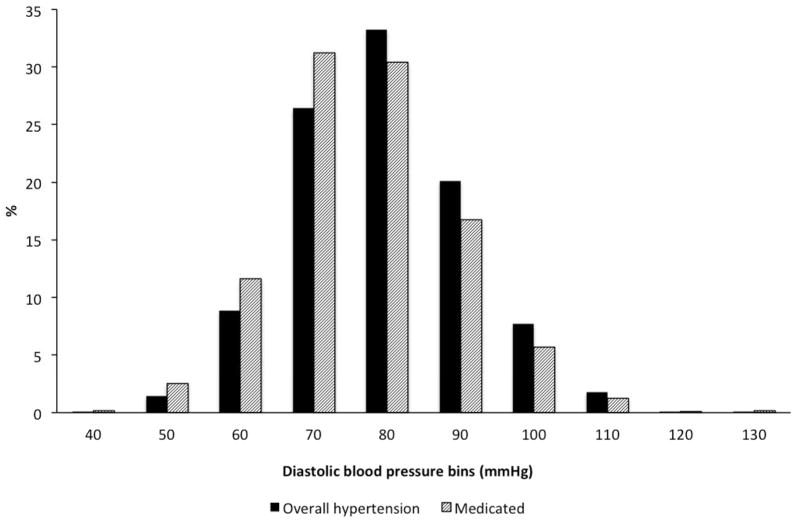
SBP and DBP among Respondents with Overall Hypertension
Figure 3 presents histograms indicating the distribution of SBP and DBP among all respondents with overall hypertension and among respondents with overall hypertension who are on medication. Slightly more than 20% of overall hypertensives on medication have SBP less than 140 mmHg, compared to only 10% of all overall hypertensions who have a SBP less than 140 mmHg. Similarly, around 75% of medicated overall hypertensives have a DBP less than 90 mmHg, compared to about 70% of all overall hypertensives. This suggests that medication interventions may be reducing blood pressure levels to some degree, but seem to work more effectively on DBP.
Figure 3.
Figure 3a–b. Distribution of systolic blood pressure (SBP) (a) and diastolic blood pressure (DBP) (b) of respondents with overall hypertension.
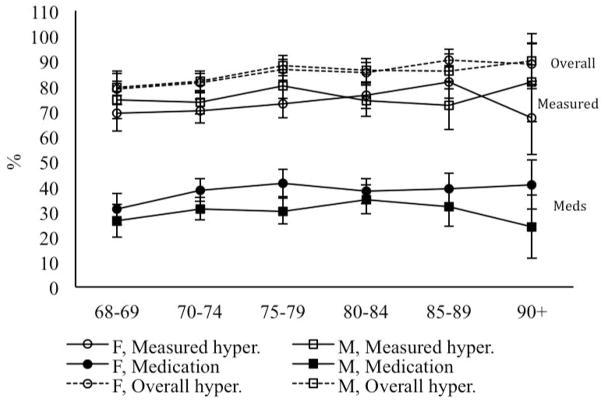
Prevalence of Hypertension and Antihypertensive Medication Usage
Figure 2 displays the prevalence of overall hypertension, measured hypertension, and antihypertensive medication usage by age and gender; there is no clear pattern of increase with age in any of these measures when differences by age group are examined. The only significant difference by gender was found in medication usage in the 75–79 age group, women had slightly higher antihypertensive medication usage, 41% (95% CI: 35.85–46.89%) versus 30% (95% CI: 24.97–35.46%) respectively.
Figure 2.
Prevalence of hypertension and medication usage by age and sex.
The only significant difference with age is seen in the prevalence of overall hypertension among women, where women under age 75 have a lower prevalence of overall hypertension compared to women aged 85–89 years old, 79% (95% CI: 73–85%) versus 90% (95% CI: 86–95%) respectively.
OLS-Regressions of Blood Pressure on Sociodemographic Characteristics and Health Behavior
Table 2 contains regression coefficients from OLS-regressions of SBP, DBP, PP, and MBP on education, rural residence, living alone, gender, age, antihypertensive medication usage, smoking, and BMI. These equations control for confounding variables so that the effect of each variable in shown with controls for the others. There were no significant associations between years of education, rural residence, living alone, and gender on any of the blood pressure measures; thus none of these sociodemographic characteristics appear to be significant predictors of blood pressure among older Japanese persons. With controls, SBP is significantly higher for those in the 80–84 (5.17, p<.05) and 85–89 (5.37, p<.05) age groups than for those 68–69 (the reference category). On the other hand, with controls, higher age was associated with lower DBP for all older age groups, except 70–74 year olds. PP was significantly higher for each age group, except 70–74, compared to the 68–69 (referent) age group. Age had no influence on MBP.
Antihypertensive medication usage was significantly associated with higher SBP (3.17, p<.01) and, since PP is calculated by subtracting DBP from SBP, PP also increased (3.03, p<.001). This positive relationship probably reflects the tendency for the use of drugs among those with the most severe hypertension as well as the inability of drugs to reduce blood pressure to low levels in many patients.
Higher BMI was significantly associated with higher SBP (0.74, p<.001), DBP (0.33, p<.001), PP (0.41, p<.01), and MBP (0.47, p<.001). Smoking was not significantly associated with blood pressure.
Logistic Regressions of Hypertension on Sociodemographic Characteristics and Health Behavior
Table 3 contains the odds ratios and 95% confidence limits from logistic regressions of hypertension on, education, urban/rural residence, living alone, gender, age, antihypertensive medication usage, smoking, and BMI. Higher education had a significant effect on measured hypertension; those with 12 years or more of schooling have 21% less chance of having measured hypertension. There was no association between education and overall hypertension. There was no significant effect of rural residence and living alone on either measured or overall hypertension. Women were 19% less likely to have measured hypertension (0.81, CI: 0.67–0.97) but there was no significant difference between men and women in overall hypertension. Age was associated with an increase in the relative likelihood of having overall hypertension. For those 90+, the likelihood of having overall hypertension was more than twice that of those 68–69. On the other hand, there was no significant difference with age in measured hypertension.
Those who were on antihypertensive medication had a higher likelihood of having measured hypertension (1.35, CI: 1.13–1.60). BMI was significantly associated with both measured and overall hypertension; one unit of increase in BMI increased chances of having measured hypertension by 6% (CI: 1.03–1.09) and overall hypertension by 13% (CI: 1.10–1.17). Smoking was not significantly associated with hypertension.
Discussion
The intent of this paper was to provide a more complete analysis of the association between blood pressure and sociodemographic characteristics and health behaviors within the older Japanese population using nationally representative survey data. We found significant links between BMI and each of our measures of blood pressure and hypertension; in each case higher BMI is linked to higher blood pressure or more hypertension. The only other variable, which was fairly consistently related to differences in blood pressure when other controls were in the equations, was age. Without the controls in the equations, most measures of blood pressure did not change much with age; only DBP was lower at higher ages and PP increased with age. However, when the controls were added, older participants had higher SBP, PP, and overall hypertension, and lower DBP.
The lack of relationships between some of the other variables and well-measured blood pressure is of interest because it again demonstrates how different the process of health determination is in Japan. Rural residence was not significantly associated with any of the outcome measures; and we should note that when we substituted rural residence in childhood into the equation, the relationship was not significant. Thus we examined the effect of both early and late life environment across Japan and found no differentials in blood pressure. The lack of relationship of hypertensive measures with living arrangements would tend to indicate that compliance with drug regimens is not enhanced by living with others. The lack of a relationship between past or current smoking and any measures is a strong indicator that smoking may have different effects in Japan, a country where heart disease is relatively low when compared to other low mortality countries [2]. In fact, some researchers have found that SBP and DBP in Japanese men who are current smokers was significantly lower than in non- and ex-smokers [37], whereas others have found that smoking is associated with the onset of systolic hypertension among Japanese men [38].
We should note that higher education was only significantly linked to lower measured hypertension when the use of antihypertensives was included as a control variable; this is also true for gender differences, where the only significant difference by gender was higher measured hypertension among males when antihypertensive use was included in the equations. The fact that the effect of education and being male disappear when antihypertensive medication use is part of the dependent variable means that differences in use of antihypertensives was what caused the significant findings. Additionally, medication seems to be more effective at reducing DBP than at reducing SBP. Reductions in DBP compared to SBP, might actually be more beneficial in reducing mortality among the oldest old; some researchers have found lower mortality rates among men 85 years-or-older with a SBP of 180 mmHg or higher and higher mortality among both genders with a DBP of 90 mmHg or higher [39].
We can offer some explanations for the lack of significant effects between hypertension in Japan for a number of variables that are associated with hypertension in other countries. Studies examining effects of education on various health outcomes in Asian countries suggest that the effects of education might be more limited in these countries than in Western countries [17, 40]. This may be related to a lack of differences by education in behaviors, lifestyle, and diet in Asian countries. Further study of the mediating variables might add to our understanding. It is also possible that the provision of universal and comparable health care in Japan might play a role in the lack of social differences in hypertension. More research needs to be conducted to understand the extent to which sociodemographic characteristics are associated, or not associated, with other biomarkers and health outcomes in Japan. Future studies on Japan should also compare the association between mortality and blood pressure with that observed in other countries, as well as the longitudinal relationship between blood pressure and other aspects of health.
The strong link between weight and hypertension adds to concern about future health in Japan as BMI increases. While BMI is low in Japan, relative to most other countries, it has been steadily increasing [23]. If we use our results to calculate the likelihood of having overall hypertension for people of different characteristics we can see the effect of increasing weight in the population. For instance, a woman 75–79 years of age with a BMI of 22.7 (the average in the sample), high education, who did not smoke and lived with someone in an urban area, would be predicted to have a 65% probability of having overall hypertension. With higher BMI at the level of overweight (BMI=25), the probability would increase to 68%, and with the onset of obesity (BMI+30), it would rise to 74%. Given that BMI is increasing in the population, these findings indicate a force toward increasing blood pressure for Japan. Similarly, the aging of the aged in Japan is another force toward increasing blood pressure and improvements need to be made in monitoring that population. As an example of the effect of age, when age is increased from 68–69 years to 90 years-or-older, the risk of overall hypertension for a woman with the same characteristics as above and average BMI (22.7 kg/m2) increases from 55% to 70%.
We used multiple measures of blood pressure and hypertension in our analyses. The results indicate that MBP does not differ with age while SBP, DBP, and PP vary with age when examined in multivariate analyses including sociodemographic and behavioral variables. Defining hypertension as either by measured blood pressure or including the use of medications in the definition of hypertension produces different links to sociodemographic measures. The different links between different measures and outcomes may partly explain the sometimes conflicting results in the literature.
Finally, we should note that our results are limited to people over 68 years of age and they would be likely to differ if younger people were included in the analysis. Our results indicate only limited differences by age in the measures of blood pressure without controls for other variables. This may be partly explained by mortality among those with higher more adverse blood pressure and by the fact that much of what we think of age-related physiological change occurs before old age.
Acknowledgments
This study was partially supported by the “Academic Frontier” Project for Private Universities: matching fund subsidy from MEXT (Ministry of Education, Culture, Sports, Science and Technology), 2006–2010 and the National Institute on Aging of the United States (P30AG017265).
References
- 1.Okayama A, Kadowaki T, Okamura T, Hayakawa T, Ueshima H. The NIPPON DATA80 Research Group: Age-specific effects of systolic and diastolic blood pressures on mortality due to cardiovascular diseases among Japanese men (NIPPON DATA80*) J Hypertens. 2006;24:459–462. doi: 10.1097/01.hjh.0000209981.43983.cf. [DOI] [PubMed] [Google Scholar]
- 2.Crimmins EM, Preston SH, Cohen B. Detailed age group contributions to e50. In: Crimmins EM, Preston SH, Cohen B, editors. International Difference in Mortality at Older Ages: Dimensions and Sources. Washington DC: The National Academies Press; 2010. pp. 64–104. [PubMed] [Google Scholar]
- 3.Ikeda N, Gakidou E, Hasegawa T, Murray CJL. Understanding the decline of mean systolic blood pressure in Japan: An analysis of pooled data from the national nutrition survey, 1986–2002. Bull World Health Organ. 2008;86:978–988. doi: 10.2471/BLT.07.050195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mori H, Ukai H, Yamamoto H, Saitou S, Hirao K, Yamauchi M, Umemura S. Current status of antihypertensive prescription and associated blood pressure control in Japan. Hypertens Res. 2006;29:143–151. doi: 10.1291/hypres.29.143. [DOI] [PubMed] [Google Scholar]
- 5.Ikeda N, Saito E, Kondo N, Inoue M, Ikeda S, Satoh T, Wada K, Stickley A, Katanoda K, Mizoue T, Noda M, Iso H, Fujino Y, Sobue T, Tsugane S, Naghavi M, Ezzati M, Shibuya K. Japan: Universial health care at 50 years 1: What has made the population of Japan healthy? Lancet. 2011;378:1094–1105. doi: 10.1016/S0140-6736(11)61055-6. [DOI] [PubMed] [Google Scholar]
- 6.Hozawa A, Ohkubo T, Kikuya M, Yamaguchi J, Ohmori K, Fujiwara T, Hashimoto J, Matsubar M, Kitaoka H, Nagai K, Tsuji I, Satoh H, Hisamichi S, Imai Y. Blood pressure control assessed by home, ambulatory and conventional blood pressure measurements in the Japanese general population: the Ohasama study. Hypertens Res. 2002;25:57–63. doi: 10.1291/hypres.25.57. [DOI] [PubMed] [Google Scholar]
- 7.Gliksman MD, Lazarus R, Wilson A, Leeder SR. Social support, marital status and living arrangement correlates of cardiovascular disease risk factors in the elderly. Soc Sci Med. 1995;40:811–814. doi: 10.1016/0277-9536(94)00149-n. [DOI] [PubMed] [Google Scholar]
- 8.van Rossum CTM, van de Mheen H, Witteman JCM, Hofman A, Mackenbach JP, Grobbee DE. Prevalence, Treatment, and Control of Hypertension by Sociodemographic Factors Among the Dutch Elderly. Hypertension. 2000;35:814–821. doi: 10.1161/01.hyp.35.3.814. [DOI] [PubMed] [Google Scholar]
- 9.Kagiyama S, Fukuhara M, Ansai T, Matsumura K, Soh I, Takata Y, Sonoki K, Awano S, Takehara T, Iida M. Association between Blood Pressure and Mortality in 80-Year-Old Subjects from a Population-Based Prospective Study in Japan. Hypertens Res. 2008;31:265–270. doi: 10.1291/hypres.31.265. [DOI] [PubMed] [Google Scholar]
- 10.Kagiyama S, Takata Y, Ansai T, Matsumura K, Soh I, Awano A, Sonoki K, Yoshida A, Torisu T, Hamasaki T, Nakamichi I, Takehara T, Iida M. Does decreased diastolic blood pressure associate with increased mortality in 80-year-old Japanese? Clin Exp Hypertens. 2009;31:639–647. doi: 10.3109/10641960903407009. [DOI] [PubMed] [Google Scholar]
- 11.DiGiovanna AG. Circulatory System. In: DiGiovanna AG, editor. Human Aging: Biological Perspectives. 2. San Francisco: McGraw-Hill; 1999. pp. 68–92. [Google Scholar]
- 12.Benetos A, Safar M, Rudnichi A, Smulyan H, Richard JL, Ducimetière P, Guize L. Pulse Pressure: A predictor of long-term cardiovascular mortality in a French male population. Hypertension. 1997;30:1410–1415. doi: 10.1161/01.hyp.30.6.1410. [DOI] [PubMed] [Google Scholar]
- 13.Okada K, Iso H, Cui R, Inoue M, Tsugane S. Pulse pressure is an independent risk factor for stroke among middle-aged Japanese with normal systolic blood pressure: the JPHC study. J Hypertens. 2011;29:319–324. doi: 10.1097/HJH.0b013e32834143d9. [DOI] [PubMed] [Google Scholar]
- 14.Asia Pacific Cohort Studies Collaboration. Blood Pressure Indices and Cardiovascular Disease in the Asia Pacific Region: A Pooled Analysis. Hypertension. 2003;42:69–75. doi: 10.1161/01.HYP.0000075083.04415.4B. [DOI] [PubMed] [Google Scholar]
- 15.Miura K, Soyama Y, Morikawa Y, Nishijo M, Nakanishi Y, Naruse Y, Yoshita K, Kagamimori S, Nakagawa H. Comparison of Four Blood Pressure Indexes for the Prediction of 10-Year Stroke Risk in Middle-Aged and Older Asians. Hypertension. 2004;44:715–720. doi: 10.1161/01.HYP.0000145108.23948.7b. [DOI] [PubMed] [Google Scholar]
- 16.Kiely DK, Gross AL, Kim DH, Lipsitz LA. The association of educational attainment and SBP among older community-living adults: the Maintenance of Balance, Independent Living, Intellect and Zest in the Elderly (MOBILIZE) Boston Study. J Hypertens. 2012;30:1518–1525. doi: 10.1097/HJH.0b013e3283550fc0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yong V, Saito Y. Are there education differentials in disability and mortality transitions and active life expectancy among Japanese older adults? Findings from a 10-year prospective cohort study. J of Gerontol B Psychol Sci Soc Sci. 2012;67:343–353. doi: 10.1093/geronb/gbs029. [DOI] [PubMed] [Google Scholar]
- 18.Colhoun HM, Hemingway H, Poulter NR. Socio-economic status and blood pressure: an overview analysis. J of Hum Hypertens. 1998;12:91–110. doi: 10.1038/sj.jhh.1000558. [DOI] [PubMed] [Google Scholar]
- 19.Fujino Y, Tamakoshi A, Iso H, Inaba Y, Kubo T, Ide R, Ikeda A, Yoshimura T. JACC study group: A nationwide cohort study of educational background and major causes of death among the elderly population in Japan. Prev Med. 2005;40:444–451. doi: 10.1016/j.ypmed.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Fukuda Y, Nakamura K, Takano T. Wide range of socioeconomic factors associated with mortality among cities in Japan. Health Promot Int. 2004;19:177–187. doi: 10.1093/heapro/dah205. [DOI] [PubMed] [Google Scholar]
- 21.Honjo K, Hiroyasu Iso H, Manami Inoue M, Shoichiro Tsugane S the JPHC Study Group. Education, social roles, and the risk of cardiovascular disease among middle-aged Japanese women: the JPHC study cohort. Stroke. 2008;39:2886–2890. doi: 10.1161/STROKEAHA.108.514067. [DOI] [PubMed] [Google Scholar]
- 22.Nishi N. Baseline Cardiovascular Risk Factors and Stroke Mortality by Municipality Population Size in a 19-year Follow-up Study-NIPPON DATA80. J Epidemiol. 2008;4:135–143. doi: 10.2188/jea.JE2008034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoshiike N, Kaneda F, Takimoto H. Epidemiology of obesity and public health strategies for its control in Japan. Asia Pc J Clin Nutr. 2002;11:S727–S731. [Google Scholar]
- 24.Saito E, Sagawa Y, Kanagawa K. Social support as a predictor of health status among older adults living alone in Japan. Nurs Health Sci. 2005;7:29–36. doi: 10.1111/j.1442-2018.2005.00220.x. [DOI] [PubMed] [Google Scholar]
- 25.Murata C, Takaaki K, Hori Y, Miyao D, Tamakoshi K, Yatsuya H, Sakakibara H, Toyoshima H. Effects of social relationships on mortality among the elderly in a Japanese rural area: an 88-months follow-up study. J Epidemiol. 2005;15(3):78–84. doi: 10.2188/jea.15.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fujino Y, Matsuda S. Prospective study of living arrangement by the ability to receive informal care and survival among Japanese elderly. Prev Med. 2009;48:79–85. doi: 10.1016/j.ypmed.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Crimmins EM, Hayward MD, Ueda H, Saito Y, Kim J. Life with and without heart disease among women and men over 50. J Women Aging. 2008;20:5–19. doi: 10.1300/j074v20n01_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim JK, Alley D, Seeman T, Karlamangla A, Crimmins E. Recent changes in cardiovascular risk factors among women and men. J Womens Health. 2006;15:734–746. doi: 10.1089/jwh.2006.15.734. [DOI] [PubMed] [Google Scholar]
- 29.Crimmins EM, Vasunilashorn S, Kim JK, Hagedorn A, Saito Y. A comparison of biological risk factors in two populations: the United States and Japan. Popul Dev Rev. 2008;34:47–482. doi: 10.1111/j.1728-4457.2008.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matsumura K, Ansai T, Awano S, Hamasaki T, Akifusa S, Takehara T, Abe I, Takata Y. Association of body mass index with blood pressure in 80-year-old subject. J Hypertens. 2001;19:2165–2169. doi: 10.1097/00004872-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Wakabayashi I. Relationships of body mass index with blood pressure and serum cholesterol concentrations at different ages. Aging Clin Exp Res. 2006;16:461–466. doi: 10.1007/BF03327402. [DOI] [PubMed] [Google Scholar]
- 32.Omvik P. How smoking affects blood pressure. Blood Press. 1996;5:71–77. doi: 10.3109/08037059609062111. [DOI] [PubMed] [Google Scholar]
- 33.Narkiewicz K, Kjeldsen SE, Hedner T. Is smoking a causative factor of hypertension? Blood Press. 2005;14:69–71. doi: 10.1080/08037050510034202. [DOI] [PubMed] [Google Scholar]
- 34.Nihon University Japanese Longitudinal Study of Aging. 2004 Home page. Retrieved December 4, 2012, from http://gero.usc.edu/CBPH/nujlsoa/ (English), http://www.nihon-u.ac.jp/affiliate_institute/information_networking/services/nujlsoa// (Japanese)
- 35.Shirasaki O, Asou Y, Takahashi Y. New clinical validation method or sutomated sphygmomanometer: a proposal by Japan ISO-WG for sphygmomanometer standard. Blood Press Monit. 2007;12:381–383. doi: 10.1097/MBP.0b013e3282495905. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Global health observatory data repository: Blood pressure. 2012 Retrieved January 28, 2013, from http://apps.who.int/gho/data/?vid=2464.
- 37.Ohkubo YT, Miyamoto Y, Suwazono E, Kobayashi E, Nogawa K. An association between smoking habits and blood pressure in normotensive Japanese men. J Hum Hypertens. 2002;16:91–96. doi: 10.1038/sj.jhh.1001303. [DOI] [PubMed] [Google Scholar]
- 38.Dochi M, Sakata K, Oishi M, Tanaka K, Kobayashi E, Suwazono Y. Smoking as an independent risk factor for hypertension: A 14-year longitudinal study in male Japanese workers. Tohoku J of Exp Med. 2009;217:37–43. doi: 10.1620/tjem.217.37. [DOI] [PubMed] [Google Scholar]
- 39.Satish S, Freeman DH, Ray L, Goodwin JS. The relationship between blood pressure and mortality in the oldest old. JAGS. 2001;49:367–374. doi: 10.1046/j.1532-5415.2001.49078.x. [DOI] [PubMed] [Google Scholar]
- 40.Kaneda T, Zimmer Z. Education, gender, and functional transitions among Indonesian elderly. JAMA. 2007;22:303–322. doi: 10.1007/s10823-007-9041-7. [DOI] [PubMed] [Google Scholar]